Abstract
Exogenous electrical stimulation (ES) has been investigated as a therapy for chronic wounds, as the skin produces currents and electrical fields (EFs) during wound healing. ES therapies operate by applying small EFs to the skin to mimic the transepithelial potentials that occur during the granulation phase of wound healing. Here, we investigated the effect of short duration (10 min) ES on the migration of HDFs using various magnitudes of physiologically relevant EFs. We modeled cutaneous injury by culturing HDFs in custom chambers that allowed the application of ES and then performed timelapse microscopy on a standard wound model. Using MATLAB to process cell coordinate data, we determined that the cells were migrating randomly and fit mean squared displacement data to the persistent random walk equation using nonlinear least squares regression analysis. Results indicated that application of 25–100 mV/mm DC EFs to HDFs on either uncoated or FN-coated surfaces demonstrated no significant changes in viability or proliferation. Of significance is that the HDFs increased random migration behavior under some ES conditions even after 10 min, providing a mechanism to enhance wound healing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
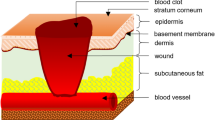
Annually, $25 billion is spent in the United States on wound healing treatments affecting 6.5 million individuals.40 These excessive costs result partly from widespread diabetic40 and other nonhealing wounds, which are defined as wounds that do not heal as expected within three months.30 Given the health and economic implications of wound healing treatments, a need exists for a wound healing therapy that can be applied to traumatic and nonhealing wounds of varying sizes, geometries, and anatomical locations. It has been well documented that the skin presents endogenous electrical fields (EFs) in the range of 30–100 mV during wound healing.5 Ions traveling across cells and tissues result in polarization of the tissue and a measurable direct current (DC) EF gradient over the span of a skin wound.26,29 This phenomenon results in what has been termed a transepithelial electric potential, and the EF values generally fall in the range of 1–100 mV/mm2 during normal wound healing processes.5,21,26,49 These endogenous EFs are thought to influence cellular division, proliferation, and migration.10
Attempts have been made to exploit the concept of transepithelial electrical potentials by using ES as a therapy to enhance wound healing.4,11,22,33,34,38 Most of these studies focus on the application of EFs with corresponding microampere (µA) currents. Most studies utilize custom electrotaxis chambers to apply EFs within the range of 50–100 mV/mm to two-dimensional cell cultures,8,21 while in three-dimensional systems, conductive membranes are often used to apply EFs.33,34,38 Several groups report increased rates of wound healing in the presence of EFs.4,29,38 Additionally, hyperphysiological EFs and ultrasound have been applied clinically and have been successful in enhancing wound healing.1,4 Based on these reports, hyperphysiological currents with associated physiological EFs may also be beneficial to wound healing.
At the foundation of cutaneous wound healing is the concept of increased cell migration into the site of injury. Human dermal fibroblasts (HDFs) have been identified as a crucial component in cutaneous wound healing,19,25,27 as wound healing prompts the arrival of inflammatory cells and fibroblasts. HDFs are particularly important for the formation of granulation tissue, a process characterized by HDF migration, proliferation, and deposition of extracellular matrix components, including fibronectin (FN).24 While the effect of ES on human keratinocytes is well documented,14,32,41 few have investigated similar responses of HDFs to ES. Unlike keratinocytes, HDFs have not been found to migrate directionally, or faster, on collagen-coated substrates in 100 mV/mm fields when exposed for an hour.21,42 The effect of ES on HDFs seeded on other extracellular matrix proteins relevant to the formation of granulation tissue, such as FN, remains largely unstudied. As FN is a critical component in wound healing,20 its contribution to wound healing in the presence of ES therapy should be identified and analyzed.
Numerous studies have reported that treatment with ES for even short periods of time are able to alter cellular functions related to wound healing. Previous studies have shown that ES treatment for 10 min is capable of enhancing nerve growth in vitro 48 and in vivo.9 Additionally, Bourguignon, et al. reported increases in protein synthesis by fibroblasts subjected to 20 min of ES6 and that 10 min of pulsed ES can increase receptor expression in human fibroblasts.7 A clinical study demonstrated that repeat treatment with short-duration pulsed ES can directly improve healing in ulcers.16 Given the variety of evidence supporting the hypothesis that short duration ES can improve cellular function and migration pertaining to wound healing, here we aim to characterize the migration behavior of HDFs on FN when exposed to physiologically relevant magnitudes of ES.
Materials and Methods
Characterization of Electrical Stimulation System
A salt bridge system was necessary in order to eliminate the possibility of cells contacting products created by traditional electrodes, such as platinum plates, in the presence of higher applied voltages during DC stimulation.44 Current travels through the salt bridges to the culture chamber in order to apply the EF to cells in vitro. Salt bridges were constructed by filling glass tubes (4.83 mm diameter) with a 1% agarose solution dissolved in phosphate buffered saline (PBS). Fields were applied using silver–silver chloride (Ag–AgCl) electrodes, which were made by soaking 99.9% pure silver wire in Clorox for 10 min. A custom lid was made by punching holes in a Nunclon Delta treated 4-well rectangular plate lid. Salt bridges were connected to the cell chambers through these holes. The other end of each salt bridge was submerged in a reservoir of PBS, which contained the electrodes attached directly to a BioRad Power Pac 300 DC power supply (Fig. 1).
Schematic diagram showing construction and operation of ES chambers. The DC power supply is set to provide desired EF, and current flows from AgCl electrodes through the saline reservoirs in and across the agarose filled salt bridges. Two platinum wires register the current and EF transmitted to cells at the outlets of each salt bridge. A scopemeter is used to track the change in currents and EFs over time for precise monitoring.
The EF was measured by placing two platinum wires at the outlet of each salt bridge. These wires were connected to a Fluke 196 scopemeter. The accompanying FlukeView software was used to directly measure the voltage drop across the cells. The total voltage measured between these wires was divided by the distance between them, 50 mm, in order to determine the magnitude of the field seen by cells (Eq. 1).
Because the resistance of each salt bridge varied due to slight differences in geometry and construction, voltage on the power source was continually monitored and adjusted during experiments in order to provide a precise EF to the cells. The circuit for each individual well was constructed in series such that the actual current measured at the outlet of the salt bridge remained the same across the chamber. Therefore, reading current at the salt bridge represents the current seen by the cells.
Culture of HDFs
HDFs were obtained from Akron General Medical Center under an institutional review board approved protocol via deidentified tissue transfer (IRB #: 0002). Cells were cultured in L-15 medium containing 4.6 g/L d-glucose and 10% fetal bovine serum and maintained at 37 °C. HDFs were seeded at a concentration of 3 × 104 cells/cm2 and allowed to grow until confluent. For cells that were cultured on FN-containing surfaces, chambers were coated with FN for 1 h at room temperature at a concentration of 1.5 µg/cm2 prior to seeding.
Electrical Stimulation
To simulate dermal wounding, confluent cell layers were scratched perpendicular to the direction of the EF with a 10–20 µL sterile micropipette tip to create a wound of 500 µm average width.17 Immediately after, cells were washed twice with sterile PBS and stimulated for 10 min at room temperature in serum-containing culture medium at one of three EF magnitudes: 25, 50, or 100 mV/mm. Cells were then washed twice with PBS and medium was replaced. The voltage across the cells was continually monitored and recorded for the duration of the stimulation using FlukeView software and the current seen by cells during the course of the experiment was monitored.
Timelapse Microscopy
Immediately following stimulation, cells were washed and labeled for 15 min at 37 °C with Hoechst 33342 fluorescent nuclei label diluted 1:500 in sterile PBS. Cells were washed again and the chambers were each refilled with 4 mL of culture medium for timelapse microscopy. Cell migration was observed for 24 h following stimulation of cells on an Olympus inverted microscope housed in an incubation chamber maintained at 37 °C. Phase and DAPI images taken at 5× magnification were taken once every 20 min for 24 h for a total of 73 frames in the image sequence.
Migration Analysis
Cell migration was determined using ImageJ36 and the MTrackJ plugin.28 Images were divided into quadrants, with 5 cells tracked per quadrant for a total of 20 cells tracked per image. Average values are reported for each condition. Cell coordinate data from the plugin was imported into MATLAB. The trajectory of each cell was normalized to its origin and plotted. Mean squared displacement (MSD) was calculated over each time interval (Eq. 2)
where x and y are the positions at times t 0 and t + t 0. Additionally, we determined the migration direction of cells in each condition by plotting the total distance travelled over the 24-h period by the angle of displacement between each cell’s initial and final location relative to the origin. The cosine of this angle is reported to give a measure of migration direction. Cells moving a total of less than a single cell diameter were not considered motile and were excluded from analysis.
Using a published MATLAB code,45 MSD curves for each of the paired 8 conditions were fitted using nonlinear least squares regression analysis to the model given by Eqs. (3) and (4), where the random motility coefficient µ, mean migration speed S, and mean persistence time P were determined for each of the 8 paired conditions by determining the 95% confidence intervals for both parameters. The first 25% of MSD data were used to fit the curves, and MSD data was calculated as a mean for each condition in order to get the most data possible, as in previous studies.12,46
Viability and Proliferation Experiments
Cells were seeded, the monolayer was scratched, and ES was applied as described above. Twenty-four hours after ES, cells were removed from well plates using trypsin–EDTA solution (0.5 g/L porcine trypsin and 0.2 g/L EDTA diluted in PBS). The cells were centrifuged for 10 min at 1000 rpm, resuspended in fresh medium, and counted using trypan blue exclusion in order to determine viability. Trypan blue is excluded from viable cells, therefore cells labeling blue were counted dead and viability was calculated as a percentage.
In separate experiments, cells were washed 3× with PBS 24 h after stimulation and calcein AM (4 mM), ethidium homodimer-1 (2 mM), and H33342 (1 mg/mL) were diluted into one solution at a ratio of 1:1000 into sterile PBS. The solution was applied to each well for 10 min at 37 °C. Dye solution was aspirated from each well and each well was washed 2× with PBS. L-15 medium was replaced in each well and cells were immediately imaged using Zen Blue (Zeiss) software.
In order to determine if migration differences were simply attributed to an increased number of cells, cell proliferation was quantified. Twenty-four hours following stimulation, cells were washed twice with sterile PBS and labeled with 10 µg/mL H33342 for 10 min at 37 °C. Dye solution was removed from culture surfaces and cells were washed again twice with PBS. Cells were lysed and the cell lysate was collected and stored at 4 °C. The intensity of each sample was acquired with a fluorescent plate reader at 350 nm excitation and 461 nm emission. Fluorescence intensity ratios were normalized to unstimulated cells to determine how application of DC ES affected cell proliferation on both uncoated and FN-coated surfaces.
Gene Expression
Cells were cultured and stimulated as above. After 24 h of post-stimulation culture, the cells were lysed using 1 mL TRIzol reagent according to the manufacturer’s protocol. After phase separation, the aqueous RNA layer was collected, precipitated with isopropanol and glycogen, and purified with 75% ethanol. RNA quality was evaluated using gel electrophoresis (1% agarose gel) and Nanodrop spectroscopy. For Nanodrop, a 260/280 nm absorbance ratio of 1.9–2.1 indicated high-quality RNA samples. The samples were reverse transcribed to cDNA using Quanta Biosciences qScript cDNA synthesis kit. The genes of interest (Table 1) were amplified using Amplitaq Gold 360 Mastermix in polymerase chain reaction (PCR). Our primers were designed specifically to address gene changes in human cells. Appropriate gene sequences were identified using BLAST from NIH for each gene. Two sequences for each gene were selected based on the sequences with the fewest unintended targets (highest specificity). Each primer pair was evaluated on control cells in preliminary PCR experiments to determine which primer provided the most effective quantification, and the best primer from each pair was used for reverse transcription PCR analysis. The exception was αV, for which a third primer was used after the first two failed to show consistent expression. All gene products were confirmed by DNA sequencing. The gene products were run on a 2% agarose electrophoresis gel and analyzed using ImageJ by a person who was blinded to the gene product. Insufficient evidence exists on gene expression of HDFs that respond consistently to ES, therefore, only a negative control (0 mV/mm) was utilized. All expression was normalized to GAPDH as a housekeeping gene as reported by similar studies.34,38
Statistics
MATLAB was used for all migration calculations and R Studio and Minitab were used for statistical evaluation. All data are displayed as the mean, with error bars representing standard deviation. To determine the relationship between the EF and current, a one-way ANOVA was used. For MSD, the angle of migration, proliferation, viability, and gene expression data, two-way ANOVA with post hoc Tukey comparisons was used. For measures of random cell migration, the data were fitted to a general linear model considering interactions between surface and magnitude of ES. For all tests, statistical significance is considered when p ≤ 0.05.
Results
Characterization of Electrical Stimulation System
The EFs were characterized by recording the current required to maintain each field strength over the resistance of the salt bridge system. The DC power supply used to deliver voltage to the circuit was operated in constant voltage mode, meaning the current was allowed to fluctuate between values to maintain the specified voltage drop across the chamber. As a result, the current fluctuated depending on the resistance of the system, which changed per experiment based on the instantaneous resistance in the salt bridges. As the chambers were connected to the salt bridges and power source in series, the current reading recorded directly from the power source is equivalent to the current experienced by the cells. With increasing EF, the corresponding current increased significantly (Fig. 2). A field of 25 mV/mm results in a 2.78 mA current, 50 mV/mm fields produce currents of 7.06 mA, and 100 mV/mm fields result in current of 18.24 mA. These differences indicate that our system is capable of applying mA order currents to cells in culture while maintaining fairly consistent EF values within the range of 25–100 mV/mm.
Applying 25–100 mV/mm EFs for 10 min Does Not Direct HDF Migration
Based on previous reports,13,15,18,21,32 we first investigated if any directional components of cell migration existed after ES exposure by plotting the final migration distance of each cell versus the angle between the starting and ending position. This measure, in addition to the cosine of that angle, allows for comparison of the cells’ migration direction (Fig. 3). The application of EFs did not result in statistical difference between the cosine of the angle of stimulated samples and those that were unstimulated.
Polar plot showing the end point of each cell’s trajectory relative to its origin. Cells moving upward move toward the positive electrode, and cells moving downward on the plot are migrating toward the ground. Distance from the origin indicates total distance traveled from the origin over time. The angle of each plotted point describes the angle of the cell’s displacement between the initial and final locations. Reported are also the cosine of the angle between the starting and ending position, which were compared using a two-way ANOVA (p ≤ 0.05) to show that ES does not direct migration. Cosine values shown represent mean ± standard deviation.
HDFs Exposed to 25–100 mV/mm EFs for 10 min Increase Random Migration Behavior
As the migration was not directional, we next investigated the potential effects of ES on random migration. MSD curves were averaged from the MSD data for individual cells using overlapping intervals (Fig. 4). The MSD curves were fit to the persistent random walk model equation to determine mean cell persistence time P and motility coefficient µ in response to ES on either uncoated or FN-coated surfaces. From these values of P and µ, the average cell migration speed S was calculated (Table 2). For control samples, µ and S on uncoated surfaces was higher than FN-coated surfaces, but P was higher FN-coated surfaces. For cells treated with either 25 or 50 mV/mm ES, µ increased on both surfaces, while cells treated with 100 mV/mm ES had a lower µ compared to unstimulated cells.
MSD curves for cells on both uncoated and FN-coated surfaces over 24-h period. The displayed curves are the average of the movement of all cells migrating a minimum of two square cell diameters using overlapping time intervals. To determine motility parameters, the first 25% of these curves were fit to Eq. (3).
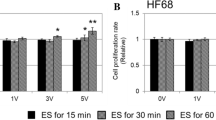
Changes in Migration Are Not Caused by Changes in Cell Viability or Proliferation
To determine if repopulation of the wound bed could be attributed to increased cell proliferation instead of cell migration, we examined the number of cells via DNA quantification. No significant differences were found with cells treated with ES compared to unstimulated controls cultured on either surface type (Fig. 5a). Images showed that cells maintain morphology and viability 24 h following ES (Fig. 5b). These results suggest that the ES did not impair cell proliferation or viability. In addition, data derived from a trypan blue exclusion assay completed 24 h following ES suggests that viability is not altered after exposure to EFs, regardless of current level, on either surface condition (Table 3). By ruling out cell death and proliferation as factors that influence repopulation of the wound, we confirm that our results are attributed to cell migration.
(a) Proliferation assay shows no differences in the quantity of DNA on either surface exposed to 25, 50, or 100 mV/mm ES compared to unstimulated controls. Error bars represent standard deviation. (b) Live-dead staining shows no reduction in viability for cells on either surface in the presence of ES compared to unstimulated controls.
HDF Gene Expression Was Not Affected by Exposure to EFs
We used PCR to determine the gene expression of potential genes responsible for increased µ. First, changes in GAPDH were measured by comparison to the ladder to assure that the housekeeping gene had consistent expression with ES. No statistical differences were found (Fig. 6a). The growth factor tested, FGF-2, showed no significant changes in expression with ES or substrate differences (Fig. 6b), which agreed with proliferation results. The four integrins that were studied, αV, β3, α5, and β5, also showed no significant changes in mRNA transcript production at 25, 50, or 100 V/m ES on either substrate (Figs. 6c–6f).
Gene expression of (a) GAPDH relative to the ladder, and (b) growth factor FGF-2, (c) αV integrin, (d) α5 integrin, (e) β3 integrin, and (f) β5 integrin, with (b)–(f) normalized to GAPDH. No significant differences were found between different current levels or substrate types. Error bars represent standard deviation.
Discussion
Most published studies focus on the application of physiologically relevant EFs and currents, e.g., 25–100 mV/mm EFs with µA currents. While these conditions are often tested, questions still exist regarding the ability of exogenous ES to increase fibroblast migration. One problem in comparing studies and migration results are the inconsistent manner of reporting the EFs and in characterizing migration. In addition, studies using physiological range EFs in conjunction with mA currents, similar to our study, are difficult to find. One potential concern with mA level currents is related to reduced cell viability. However, our results indicate no statistical change in cell number between the 8 groups, no reduction in cell viability in response to any EF, and cells displayed typical fibroblast morphology for 24 h following ES treatment. Therefore, application of currents of magnitudes noted here did not impair cellular viability or proliferation.
Studies have previously explored the application of hyperphysiological ES for wound healing applications,35 however, few groups have applied mA current to cells and quantified fibroblast migration in detail. Using polar plots, we showed cells displayed no directional preference for the direction in which they migrated. The results presented here for 10 min of stimulation agree with previous literature for short duration ES, where stimulations need to be applied for at least 1 h to direct cell migration.8,21 Studies completed as early as 1994 indicated a patterned cellular locomotion in response to ES. Brown and Loew observed cathode-directed migration in murine fibroblasts stimulated via agarose salt bridges with a minimum of 100 mV/mm EFs for 1 h,8 however the current was not reported. A 2007 study used 200 and 600 mV/mm DC EFs with 0–0.30 mA currents for an hour to observe a cathode-directed effect of such fields on ligament fibroblasts.10 However, this study noted that increasing the attachment of the ligament fibroblasts through increasing the amount of collagen on the surface obliterated the directional migration.10 The results of our work demonstrate no difference in patterns of directional migration under the conditions studied, confirming random migration. The variety of results across ES studies can be attributed to the duration and magnitude of the EF and current, among other conditions such as substrate coatings and the disease state of the cells.10,23,29,47
We next considered that cell migration rates could still be increasing as a result of an applied EF, even if the migration did not present itself as directional. Therefore, we chose to analyze our migration data using a common model of random cell migration. We fit the data to the equation for the persistent random walk model and determined the parameters of μ, S, and P using nonlinear least squares regression analysis. In calculating the MSD for cells, cells on FN-coated surfaces had lower MSDs than cells on uncoated surfaces, indicating reduced migration in the presence of FN. We then found further changes due to ES, with increased values of µ in the presence of 25 and 50 mV/mm EFs for both surface conditions (r 2 > 0.970). Measures of P and S were on the expected order known for fibroblast motility. Rouabhia et al. suggested that longer exposure to DC EFs of 50 mV/mm or 200 mV/mm results in greater wound closure compared to unstimulated fibroblasts,38 which may indicate an increased random migration, as both cathodal and anodal migration are required for a closure, but the MSD was not examined. Additionally, Simpson et al. report that 3T3 fibroblasts subjected to 0, 100, 200, and 400 mV/mm EFs respond similarly in that they express some inherent randomness in their migration patterns, although these differences were determined qualitatively, and quantitative results showing directed migration were obtained using a different model.43 Otherwise, direct evidence of increased random migration via ES is difficult to find.
Interestingly, application of 100 mV/mm EFs impaired HDF motility on both surfaces by demonstrating reduced values of µ as well as the greatest reduction in values of S. For cells stimulated at 100 mV/mm, P was higher for cells on FN-coated surfaces compared to those on uncoated surfaces. These results indicated a potential relationship between ES and a cell’s interaction with FN on the culture surface that decreases random migration. Decreased motility in the presence of FN has been previously noted,37 exogenous ES has been reported to upregulate cellular FN,39 and various FN isoforms are apparent at lesion sites.31 Therefore, it is critical to examine the surface coating as a factor in the study of migration, as well as the EF and current applied.
These changes in migration parameters when a high EF was applied led us to examine some of the potential regulators of cell-surface interactions by gene expression of HDFs. Based on our results, the presence of a FN coating did not significantly change the gene expression of αV, β3, α5, or β5 integrin subunits. We also found no difference in expression when comparing different levels of stimulation. This result matches previous results,34 where Park et al. found no difference in αV, β3, or α5 expression in HDF’s subjected to 50 mV/mm or 200 mV/mm ES on conductive membranes with heparin for 6 h. However, they found up-regulation of β5 at 200 mV/mm, which is beyond our maximum applied voltage, but this effect would highly depend on the conditions (current, duration, and substrate). Here we also noted that gene expression of FGF-2 was unchanged with surface coating or ES, as might be expected from the proliferation results, although Park et al. also found gene up-regulation and increased protein expression of FGF-2 at 200 mV/mm after 6 h of exposure.34 While our gene expression results did not lead to a mechanism for the increased random migration, it does not necessarily eliminate these molecules as a mechanism for the changes, as gene expression does not necessarily correlate with protein expression. Future work should focus on surface expression of integrin proteins and secretion of FGF after these short duration applications of ES.
The rationale for using a scratch assay, a widely used in vitro wound model,2,38 was that we wanted to disrupt a confluent cell layer similar to injury in vivo. By combining the use of HDFs with a FN surface coating and ES, we sought to model ES application during the granulation phase of wound healing. Alternative assays rely on techniques such as stamping to prevent cell infiltration into a region of interest in order to simulate a cell-free area that is to model a cutaneous wound. However, these models do not disrupt cells as we would expect from wounding in vivo, and therefore do not closely model cutaneous injury.3
In summary, our results demonstrated HDFs migrate randomly in response to 10 min ES and increase migration parameters for some EFs. While the presence of FN decreased both µ and P, EFs increased these parameters similarly on uncoated and FN coated substrates. Considering our results, we hypothesize that the observed differences in random motility on both substrates due to ES are due to a similar mechanism, as MSD increases similarly for both surface conditions at lower EFs, and may be independent of the interaction between the protein coating and the cell. Our results indicated that the culture environment, including EF magnitude, current, and surface coating are important parameters in studying wound healing, and should be measured and reported for future studies. The increase in random migration demonstrates the potential utility of ES to alter cell behavior after a 10 min application.
References
Anglen, J. The clinical use of bone stimulators. J. South. Orthop. Assoc. 12(2):46–54, 2003.
Ascione, F., A. Vasaturo, S. Caserta, V. D’Esposito, P. Formisano, and S. Guido. Comparison between fibroblast wound healing and cell random migration assays in vitro. Exp. Cell. Res. 347:123–132, 2016.
Ashby, W. J., and A. Zijlstra. Established and novel methods of interrogating two-dimensional cell migration. Integr. Biol. 11:1338–1350, 2012.
Avrahami, R., J. Rosenblum, M. Gazes, and L. Litman. The effect of combined ultrasound and electric field stimulation on wound healing in chronic ulcerations. Wounds 27:199–208, 2014.
Barker, A., L. Jaffe, and J. Vanable. The glabrous epidermis of cavies contains a powerful battery. Am. J. Physiol. 242(3):R358–R366, 1982.
Bourguignon, G. Y., and L. Y. Bourguignon. Electric stimulation of protien and DNA synthesis in human fibroblasts. FASEB J. 1(5):398–402, 1987.
Bourguignon, G. Y., W. Jy, and L. Y. Bourguignon. Electric stimulation of human fibroblasts causes an increase in Ca2+ influx and the exposure of additional insulin receptors. J. Cell Physiol. 140(2):379–385, 1989.
Brown, M. J., and L. M. Loew. Electric field-directed fibroblast locomotion involves cell surface molecular reorganization and is calcium independent. J. Cell Biol. 127:117–128, 1994.
Calvey, C., W. Zhou, K. S. Stakleff, P. Sendelbach-Sloan, A. B. Harkins, W. Lanzinger, and R. K. Willits. Short-term electrical stimulation to promote nerve repair and functional recovery in a rat model. J. Hand Surg. Am. 40(2):314–322, 2015.
Chao, P., H. Lu, C. Hung, S. Nicoll, and J. Bulinski. Effects of applied DC electric field on ligament fibroblast migration and wound healing. Connect Tissue Res. 48:188–197, 2007.
Collard, J., and M. Hinsenkamp. Cellular processes involved in human epidermal cells exposed to extremely low frequency electric fields. Cell. Signal. 27:889–898, 2015.
Dickinson, R. B., and R. T. Tranquillo. Optimal estimation of cell movement indices from the statistical analysis of cell tracking data. AlChe J. 39(12):1995–2010, 1993.
Erickson, C. A., and R. Nuccitelli. Embryonic fibroblast motility and orientation can be influenced by physiological electric fields. J. Cell Biol. 98(1):296–307, 1984.
Fang, K. S., B. Farboud, R. Nuccitelli, and R. R. Isseroff. Migration of human keratinocytes in electric fields requires growth factors and extracellular calcium. J. Invest. Dermatol. 11:751–756, 1998.
Farboud, B., R. Nuccitelli, I. R. Schwab, and R. R. Isseroff. DC electric fields induce rapid directional migration in human corneal epithelial cells. Exp. Eye Res. 70:667–673, 2000.
Feedar, J. A., L. C. Kloth, and G. D. Gentzkow. Chronic dermal ulcer healing enhanced with monophasic pulsed electrical stimulation. Phys. Ther. 71(9):639–649, 1991.
Funari, V. A., M. Winkler, J. Brown, S. D. Dimitrijevic, A. V. Ljubimov, and M. Saghizadeh. Differentially expressed wound healing-related microRNAs in the human diabetic cornea. PLoS ONE 8(12):e84425, 2013.
George, S. P., H. Chen, J. C. Conrad, and S. Khurana. Regulation of directional cell migration by membrane-induced actin binding. J. Cell Sci. 126:312–326, 2013.
Ghosh, K., X. Ren, G. Prestwich, and R. Clark. Fibronectin functional domains coupled to hyaluronan stimulate adult human dermal fibroblast responses critical for wound healing. Tissue Eng. 12:601–613, 1006.
Grinnell, F. Fibronectin and wound healing. J. Cell. Biochem. 26(2):107–116, 1984.
Guo, A., B. Song, B. Reid, Y. Gu, J. Forrester, C. Jahoda, and M. Zhao. Effects of physiological electric fields on migration of human dermal fibroblasts. J. Invest. Dermatol. 130:2320–2327, 2010.
Kim, M., M. Lee, B. Kwon, H. Seo, M. Koo, K. You, D. Kim, and J. Park. Control of neonatal human dermal fibroblast migration on poly(lactic-co-glycolic acid)-coated surfaces by electrotaxis. J. Tissue Eng. Regener. Med. 11:11–12, 2015.
Kloth, L. C. Electrical stimulation for wound healing: a review of evidence from in vitro studies, animal experiments, and clinical trials. Adv. Wound Care 3(2):81–90, 2014.
Lenselink, E. A. Role of fibronectin in normal wound healing. Int. Wound. J. 12:313–316, 2015.
Lin, F., X. Ren, Z. Pan, L. Macri, W. Zong, M. Tonnesen, M. Rafailovich, D. Bar-Sagi, and R. Clark. Fibronectin growth factor-binding domains are required for fibroblast survival. J. Invest. Dermatol. 131:84–98, 2011.
McCaig, C., A. Rajnicek, B. Song, and M. Zhao. Controlling cell behavior electrically: current views and future potential. Physiol. Rev. 85:943–978, 2005.
McClain, S., M. Simon, E. Jones, A. Nandi, J. Gailit, M. Tonnesen, D. Newman, and R. Clark. Mesenchymal cell activation is the rate-limiting step of granulation tissue induction. Am. J. Pathol. 149:1257–1270, 1996.
Meijering, E., O. Dzyubachyk, and I. Smal. Methods for cell and particle tracking. Methods Enzymol. 504:183–200, 2012.
Messerli, M., and D. Graham. Extracellular electrical fields direct wound healing and regeneration. Biol. Bull 221(1):79–92, 2011.
Mustoe, T. A., K. O’Shaughnessy, and O. Kloeters. Chronic wound pathogenesis and current treatment strategies: a unifying hypothesis. Plast. Reconstr. Surg. 117(7 Suppl):35S–41S, 2006.
Natali, P. G., M. R. Nicotra, D. Filippo, and A. Bigotti. Expression of fibronectin, fibronectin isoforms and integrin receptors in melanocytic lesions. Br. J. Cancer 71(6):1243–1247, 1995.
Nishimura, K. Y., R. R. Isseroff, and R. Nuccitelli. Human keratinocytes migrate to the negative pole in direct current electric fields comparable to those measured in mammalian wounds. J. Cell Sci. 109:199–207, 1996.
Niu, X., M. Rouabhia, N. Chiffot, M. King, and Z. Zhang. An electrically conductive 3D scaffold based on a nonwoven web of poly(l-lactic acid) and conductive poly(3,4-ethylenedioxythiophene). J. Biomed. Mater. Res. Part A 103(8):2635–2644, 2015.
Park, H., M. Rouabhia, D. Lavertu, and Z. Zhang. Electrical stimulation modulates the expression of multiple wound healing genes in primary human dermal fibroblasts. Tissue Eng. Part A 21(13–14):1982–1990, 2015.
Peters, E. J., L. A. Lavery, D. G. Armstrong, and J. G. Fleischli. Electric stimulation as an adjunct to heal diabetic foot ulcers: a randomized clinical trial. Arch. Phys. Med. Rehabil. 82(6):721–725, 2001.
Rasband, W. S. ImageJ, 1997–2016. http://imagej.nih.gov/ij/
Rhoads, D. S., and J.-L. Guan. Analysis of directional cell migration on defined FN gradients: role of intracellular signaling molecules. Exp. Cell. Res. 313(18):3859–3867, 2007.
Rouabhia, M., H. Park, S. Meng, H. Derbali, and Z. Zhang. Electrical stimluation promotes wound healing by enhancing dermal fibroblast activity and promoting myofibroblast transdifferentiation. PLoS ONE 8(8):e71660, 2013.
Sebastian, A., F. Syeh, D. Perry, V. Balamurugan, J. Colthurst, I. Chaudhry, and A. Bayat. Acceleration of cutaneous healing by electrical stimulation: degeneral electrical waveform down-regulates inflammation, up-regulates angiogenesis and advances remodeling in temporal punch biopsies in a human volunteer study. Wound Repair Regen. 19(6):693–708, 2011.
Sen, C., G. Gordillo, S. Roy, R. Kirsner, L. Lambert, T. Hunt, F. Gottrup, G. Gurtner, and M. Longaker. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen. 17(6):763–771, 2009.
Sheridan, D. M., R. R. Isseroff, and R. Nuccitelli. Imposition of a physiologic DC electric field alters the migratory response of human keratinocytes on extracelluar matrix molecules. J Invest. Dermatol. 106(4):642–646, 1996.
Sillman, A. L., D. M. Quang, B. Farboud, K. S. Fang, R. Nuccitelli, and R. R. Isseroff. Human dermal fibroblasts do not exhibit directional migration on collagen I in direct-current electric fields of physiological strength. Exp. Dermatol. 12(4):396–402, 2003.
Simpson, M. J., K. Y. Lo, and Y. S. Sun. Quantifying the roles of random motility and directed motility using advection-diffusion theory for a 3T3 fibroblast cell migration assay stimulated with an electric field. BMC Syst. Biol. 11(1):39, 2017.
Tandon, N., C. Cannizzaro, P. H. Chao, R. Maidhof, A. Marsano, H. T. Au, M. Radisic, and G. Vunjak-Novakovic. Electrical stimulation systems for cardiac tissue engineering. Nat. Protoc. 4(2):155–173, 2009.
Tarantino, N., J. Tinevez, E. F. Crowell, B. Boisson, R. Henriques, M. Mhlanga, F. Agou, A. Israel, and E. Laplantine. TNF and IL-1 exhibit distinct ubiquitin requirements for inducing NEMO-KK supramolecular structures. J. Cell Biol. 204(2):231–245, 2014.
Ware, M. F., A. Wells, and D. A. Lauffenburger. Epidermal growth factor alters fibroblast migration speed and directional persistence reciprocally and in a matrix-dependent manner. J. Cell Sci. 111(Pt 16):2423–2432, 1998.
Weiss, D., R. Kirsner, and W. Eaglestein. Electrical stimulation and wound healing. Arch. Dermatol. 126(2):222–225, 1990.
Wood, M., and R. K. Willits. Short-duraction, DC electrical stimulation increases chick embryo DRG neurite outgrowth. Bioelectromagnetics 27(4):328–331, 2006.
Zhao, M. Electrical fields in wound healing—an overriding signal that directs cell migration. Semin. Cell Dev. Biol. 20(6):674–682, 2009.
Acknowledgments
Funding for this work was provided through the Margaret F. Donovan Endowed Chair for Women in Engineering at The University of Akron. The authors would like to thank the Cornell University Statistical Consulting Unit for assistance with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Michael Gower oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Snyder, S., DeJulius, C. & Willits, R.K. Electrical Stimulation Increases Random Migration of Human Dermal Fibroblasts. Ann Biomed Eng 45, 2049–2060 (2017). https://doi.org/10.1007/s10439-017-1849-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-017-1849-x