Abstract
The objective of this study was to develop a new high-efficiency dry powder inhaler (DPI) that can effectively aerosolize large masses (25–100 mg) of spray dried powder formulations. The DPI was designed to implement a concept similar to a fluidized bed for aerosolization using small mixing balls made of polytetrafluoroethylene along with a larger, hollow dosing sphere filled with the powder. The performance of the fluidized bed DPI was compared, based on emitted dose (ED) and aerosolization efficiency, to other recently developed capsule-based DPIs that were designed to accommodate smaller powder masses (~2–20 mg). The inhalers were tested with spray dried excipient enhanced growth (EEG) formulations that contained an antibiotic (ciprofloxacin) and hygroscopic excipient (mannitol). The new fluidized bed design produced an ED of 71% along with a mass median aerodynamic diameter of 1.53 μm and fine particle fractions <5 and 1 μm of 93 and 36%, respectively, when used to deliver a 100 mg loaded mass of EEG powder with the advantage of not requiring multiple capsules. Surprisingly, performance of the device was further improved by removing the mixing balls from the inhaler and only retaining the dose containment sphere.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dry powder inhalers (DPIs) continue to gain market share and are becoming the most prescribed devices for delivering inhaled medications to the lungs.24 Recent studies have demonstrated high efficiency performance of three dimensional (3D) rod array DPIs with aerosol fine particle fractions (FPF) <5 µm greater than 90%, mouth-throat depositional loss <5%, and little sensitivity to inhalation flow rate.1,2,26 However, these DPI development studies and high efficiency devices were tested with relatively low doses of drug. For these devices to deliver a large dose medication, like an inhalable antibiotic, multiple capsules may need to be used to administer a therapeutic dose. In the recent study by Behara et al.2 a DPI was developed that could produce an aerosol with a mass median aerodynamic diameter (MMAD) of approximately 1.50 μm, an emitted dose (ED) greater than 75%, and FPF less than 5 and 1 μm (FPF<5µm/ED and FPF<1µm/ED) of 95 and 31%, respectively, at an inhalation flow rate of 45 LPM and a pressure drop of 4 kPa using an excipient enhanced growth (EEG) powder formulation. In comparison, most commercial DPIs typically employ carrier-particle based formulations (i.e., lactose blends) that struggle to generate FPF<5µm above 40% and produce lower values at low flow making dispersion highly dependent on inhalation flow rate.14,20,31 However, spray dried formulations (e.g., Pulmosphere™ and EEG) have recently improved inhaler performance by increasing deaggregation, and thus increasing FPF<5µm values.7,23,29,30 The high efficiency performance achieved by Behara et al.2 was based on a 2 mg loaded mass, which is consistent with inhaled medications such as β2-agonists and corticosteroids. The delivery of higher dose medicines with these new high efficiency devices may require loading and actuating multiple powder capsules. Repeated loading and delivering the medications over multiple cycles is time consuming and may result in poor patient compliance24 and variability in delivery efficiency.
Potential pharmaceutical applications that require high doses of drug include most inhaled antibiotics (e.g., tobramycin), non-steroidal anti-inflammatories (e.g., disodium cromoglycate), mucus clearance agents (e.g., mannitol), and surfactants (e.g., recombinant protein-C).15,22,30 To deliver these high-dose inhaled medications, three approaches may be employed: (i) use active DPIs often requiring multiple dose loadings, (ii) implement single capsule passive devices and load multiple capsules, and (iii) develop new passive devices intended for high-dose medications. Active DPIs provide a power source to assist with aerosolizing the large powder mass. For example, the MicroDose DPI (MicroDose Therapeutx, Inc., Monmouth Junction, NJ) utilizes a vibrating piezoelectric system to form an aerosol from a foil dosing blister that can contain up to approximately 400 mg of powder.5 Aerosolization performance with active devices is typically good; however, the implementation of a power source typically increases device cost and complexity.14,26 Currently, the most widely used strategy for delivering high-doses of inhaled medications is a capsule-based device with multiple cycles of loading and actuation. For example, the Podhaler (Novartis Pharmaceuticals, San Carlos, CA) inhaler is used to effectively deliver a 112 mg dose of tobramycin to cystic fibrosis patients.7 This approach provides a significant time savings compared with nebulized delivery, which typically requires 15–20 min per treatment; however, the patient is required to load and actuate four separate capsules.7 Furthermore, mouth-throat depositional loss is reported to be >40% with the PulmoSphere formulation and Podhaler combination. For the delivery of mannitol as a mucus clearance enhancer, Bronchitol (Pharmaxis Ltd, Sydney, Australia) is currently delivered as ten separate capsules containing 40 mg each.4
High-dose devices can be classified as delivering 50 mg of powder and above. Ideally, the same device should also be capable of delivering lower masses in the range of 10 or 25 mg. The Twincer inhaler is a passive device that can be operated with a loaded mass up to approximately 50 mg; however, higher masses have not been reported.6 Recently, the Orbital multi-breath inhaler was introduced as a true high powder mass platform capable of delivering doses up to 400 mg over a series of 16 inhalations.30 With high powder mass devices, multiple inhalations with a single dose loading are considering advantageous to avoid overloading the oropharynx and upper airways with deposited powder during a single inhalation. The Orbital was found to produce aerosols with MMADs of 3, 4.2, and 4 μm using ciprofloxacin (Cipro), mannitol, and a 1:8 Cipro-mannitol co-spray-dried powder, respectively.30 Fine particle fractions were in the range of 42–67% and mouth-throat (MT) depositional loss was not reported at the tested inhalation flow rate of 60 LPM.
A concept that has previously not been reported for the efficient aerosolization and delivery of pharmaceutical powders in a handheld device is that of a fluidized bed. The fluidized bed concept consists of a collection of small spheres, or other solids, that have fluid-like movement when a gas is forced through them.19 Chaotic motion of the spheres induces turbulence and collisions that can effectively deaggregate a powder as it passes through the bed. This approach was previously reported in a large scale device used to produce test aerosols for evaluating filters and aerosol characterization equipment.12 Fluidized beds have also been used to meter and fill dose containment units used in inhalers, such as blisters and capsules.32 However, a miniature fluidized bed in an inhaler has not previously been considered and may provide an effective approach for producing high efficiency aerosolization of high-dose medications.
The objective of this study is to develop a high-efficiency, high-dose DPI intended for EEG aerosol delivery using a concept similar to a classic fluidized bed aerosol generator.12,16,19 The inhaler contains the fluidized bed, which consists of small light-weight mixing balls. Designs include introduction of the powder directly to the fluidized bed and containment of the powder in a separate dosing sphere that is placed in the fluidized bed. The effect of the mixing balls is also considered by removing them from the design and only including the dose sphere. A series of in vitro experiments was conducted to select leading design conditions, optimize the design, and evaluate aerosolization characteristics compared with existing high efficiency devices at different flow conditions that reflect the inhalation capabilities of adults and children.
Materials and Methods
Overview
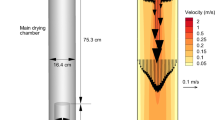
To develop and optimize the fluidized bed (FB)-DPI, a number of screening experiments were first conducted. The proposed design, shown in Fig. 1, consists of a chamber with an off-center inlet for airflow to enter from the top, approximately sixty PTFE mixing balls that are 4.76 mm in diameter (McMaster-Carr, Elmhurst, Illinois), a powder dosing sphere with an outer diameter of 12 mm, an inner diameter of 10 mm, and four 0.5 mm holes for the powder to exit, a mixing chamber, a mesh to retain the mixing balls, and a mouthpiece. The effects of different mixing ball sizes, air inlets, mixing chamber sizes, and number of holes in the powder dosing sphere were evaluated in search of an optimized design. The inlet, chamber size, and ball size were optimized to produce the maximum vibrational amplitude, as measured using a piezoelectric force sensor. Next, the powder dosing sphere was optimized based on emptying over time to produce a consistent amount of powder leaving the device during each inhalation using a readily available spray dried mannitol powder. Performance of the proposed device was then compared to a previously developed high efficiency DPI for EEG aerosol delivery (i.e., the CC90-3D inhaler).2 The FB-DPI was tested using 25 mg of an EEG ciprofloxacin (EEG-Cipro) formulation for comparison with a single 25 mg capsule used in the previously developed CC90-3D device. The FB-DPI was also tested using 100 mg of the EEG-Cipro formulation at a characteristic adult pressure drop of 4 kPa, and 50 mg using a representative pediatric pressure drop of 2 kPa. Results of aerosolization are given in terms of dosing sphere (or capsule) and device retention, ED, FPF<5µm/ED, and FPF<1µm/ED, and the MMAD of the aerosol. Based on previous studies, high efficiency performance for the delivery of EEG formulations will be defined by the production of an aerosol with the following characteristics: an MMAD of approximately 1.50 μm, FPF<5µm/ED above 90%, FPF<1µm/ED above 30%, and an ED of approximately 75% while using a relatively large mass (25–100 mg) of powder.1,2
Materials
Ciprofloxacin hydrochloride (Cipro) was purchased from Spectrum Chemicals (Gardena, CA) and Pearlitol® PF-Mannitol was donated from Roquette Pharma (Lestrem, France). Poloxamer 188 (Leutrol F68) was donated from BASF Corporation (Florham Park, NJ). l-leucine and all other reagents were purchased from Sigma Chemical Co. (St. Louis, MO). Hydroxypropyl methylcellulose (HPMC) capsules (size 3) were donated from Qualicaps (Whitsett, NC).
Inhaler Design
A fluidized bed can be created by inducing fluid motion through an array consisting of many solids, usually of similar size and material. As the fluid, which is typically air, moves through the bed of solids, the entire structure begins to behave similar to a fluid rather than a solid structure.9 For creation of the high-dose “fluidized bed” style DPI, small PTFE mixing balls are used to assist with the emptying of the device as well as the deaggregation of the powder. Inhalation air is drawn through the mixing balls from an inlet jet, causing them to move chaotically within the mixing chamber, which empties the powder dosing sphere and breaks up agglomerates of powder. The basic design of the proposed inhaler is shown in Fig. 1. The design consists of the mixing chamber, an air inlet from the top, a mesh preventing inhalation of the small mixing balls and dosing sphere, and a mouthpiece. The edges on the inside of the device were rounded to prevent powder buildup in corners that the mixing balls could not reach. The air inlet configurations to be evaluated are shown in Fig. 2 and labeled Inlets 1–6. Inlets directed from the bottom of the chamber were also considered, but were found to be ineffective in comparison to the top inlets.
Approaches to introduce the formulation into the inhaler were direct addition of the powder mass on top of the fluidized bed or containment of the powder in a dosing sphere. The initial prototyped design of the dosing sphere had inner and outer diameters of 10 and 12 mm, respectively. To release the powder, the dosing sphere had either 2, 4, 6 or 8 circular openings (holes) with diameters of 0.5 mm each. The sphere was built in two halves which were assembled after placing the powder inside. The first hole was placed at a 20° offset from the center bisection of the sphere, with a second hole opposite of this at 180°. For the four hole design there are two sets of two holes with center lines that intersect each other in the center of the sphere. For the six and eight hole spheres, the holes were placed at equal intervals around the outside of the sphere, so that for the six hole sphere, there would be three holes on both the top and bottom halves and for the eight hole sphere there would be four holes on each half. Furthermore, a fifth hole configuration, shown in Fig. 3, was considered that implemented four holes oriented in a way such that the center lines of the holes intersected in the center of the sphere, but the center lines were offset 90° when looking from the top or bottom of the sphere. The dosing sphere was intended to provide high emission from the device while uniformly releasing the powder over four inhalations.
The inhalers and dosing spheres were created using Autodesk Inventor and exported as .STL files to be prototyped. The files were then prepared using 3D Lightyear Software. The parts were built using a 3D Systems Viper SLA machine (3D Systems Inc., Rock Hill, SC) using Accura 60 stereolithography resin (3D Systems Inc.). Once the parts were prototyped, they were cleaned using a Proclean SL Part Washer (3D Systems Inc.) and dried in a 3D Systems UV-light dryer for 90 min. The parts were then sanded to provide a smooth finish.
After prototyping and cleaning, the inhaler devices (but not dosing spheres) were coated with a commercial polytetrafluoroethylene (PTFE) suspension (LU™708, Sprayon Products, Cleveland, OH), which is a high contact angle (or low surface energy) material. A suspension of PTFE was sprayed inside the entire device to form a thin coating. Compressed air was blown through the coated portions until the surface appeared dry. This coating was applied to reduce the powder buildup on the walls of the device and to reduce static charge buildup due to a difference in the material of the mixing balls and the prototyped chamber.
Evaluation of Vibrational Amplitude
To optimize the mixing chamber diameter (15, 20, or 25 mm), inlet configuration, and mixing ball size (3.18, 3.97, or 4.76 mm), a screening method was used. A polyvinylidene fluoride (PVDF) piezoelectric force sensor (LDT1-028 K; Measurement Specialties, Hampton, VA) was fixed to the outside of the devices to measure the intensity of vibration caused by the impaction of the spheres inside the DPI at a steady state flow rate of 45 LPM (4 kPa pressure drop). The positive and negative leads were then connected to an oscilloscope probe. The intensity of the vibration was measured by reading the voltage output values on the oscilloscope. Peak-to-peak voltage averages were used to measure the intensity of vibrations within the inhaler and labeled the vibrational amplitude.
Powder Formulations
Formulations employed were a commercially available spray dried mannitol powder for rapid screening of emitted dose (ED) at high-mass loadings and a spray dried EEG formulation of the antibiotic ciprofloxacin. The spray dried mannitol powder was PEARLITOL 25C (Roquette Pharma, Lestrem, France) with a reported primary particle mean diameter of 25 µm. While larger in particle size than the EEG-Cipro formulation, the PEARLITOL powder was selected for use in the screening studies as it is highly dispersible, similar to EEG formulations, and readily available for high-mass testing of the inhaler emptying characteristics without having the potential pharmacological effects of the EEG-Cipro formulation.
An EEG formulation of co-spray dried mannitol and ciprofloxacin was prepared using the approach described by Son et al.25 Briefly, a 20% ethanol in water mixture containing 0.5% w/v of solutes consisting of Cipro, mannitol, l-leucine and poloxamer 188 in a ratio of 30:48:20:2 (w/w %) was spray dried using a Büchi Nano spray dryer B-90 (Büchi Laboratory-Techniques, Flawil, Switzerland). The powder formulation was generated using an airflow rate of 120 LPM, 100% liquid flow rate using the 4 µm nozzle diameter at an air inlet temperature of 70 °C. The resulting air outlet temperature and spray dryer pressure were 40 °C and 35 mbar, respectively. Powder was collected from the electrostatic precipitator of the spray dryer and was stored in a desiccator until it was used. The powder yield was about 50–60%. Approximately 1 mg of powder was dissolved in 100 mL of deionized water and analyzed for content uniformity (n = 3) of Cipro in the formulation using the USP HPLC method for Cipro. To protect the powder formulations from the effects of ambient humidity, powders were stored in a desiccator to prevent moisture ingress and aerosolized following brief exposure to environmental RH conditions.
As previously described, the EEG approach is intended to generate an aerosol with a very small initial MMAD, typically 1.5 µm or below, and high FPF.25 Due to small size of the aerosolized particles, MT or extrathoracic deposition is minimal.25 Once inside the airways, the EEG particles take up water due to the inclusion of the hygroscopic excipient and become significantly larger droplets.10 This size increase of the droplets is used to ensure aerosol deposition within the lungs, which would be largely exhaled without size increase, and potentially control the region of drug delivery.27
Evaluation of Device Emptying
The device with the highest vibrational amplitude was selected and implemented for evaluation of ED from the five different dosing spheres. Initial screening was conducted with 100 mg of the PEARLITOL 25C formulation loaded into the dosing sphere and placed in the selected FB-DPI. A vacuum pump, flow controller and inline filter were connected in series to the mouthpiece of the inhaler and the FB-DPI was actuated using a inhalation flow rate of 60 LPM for 4 s producing an inhaled volume of 4 L. The corresponding pressure drop over the device was 4 kPa. Four inhalation cycles were used to evaluate the inhaler. The ED in these screening experiments using PEARLITOL 25C was calculated by weighing the FB-DPI before and after testing. Emptying of the inhaler after each inhalation was also tested using a 25 mg mass of spray dried EEG-Cipro powder over four inhalations and analyzed by weight. This relatively low mass was employed to provide a conservatively low estimate of emptying, as percent ED is expected to increase as loaded mass is increased.
Evaluation of Previously Developed Capsule-Based EEG DPIs at Higher Loaded Mass
The previous study of Behara et al.2 developed the CC90-3D rod array DPI for use with EEG formulations and showed high efficiency performance with a 2 mg loaded mass. In the current study, performance of the CC90-3D device is evaluated with 25 mg of the EEG-Cipro formulation, which is the approximate maximum that can be placed in a single size 3 HPMC capsule (Qualicaps, Whitsett, NC). The loaded capsules were then pierced using a 0.5 mm needle in the optimum configuration as determined by Behara et al.2 and placed in the CC90-3D inhaler. The powder was then aerosolized into a Next Generation Impactor (NGI; MSP Corp., Shoreview, MN) using a 2 or 4 kPa pressure drop across the device, which corresponded to flow rates of 32 LPM or 45 LPM, respectively. For the adult 4 kPa pressure drop, powders were aerosolized until a total air volume of 4 L was drawn through the inhaler at ambient conditions (10–45% RH and 20–24 °C). For the pediatric 2 kPa pressure drop, the powder was aerosolized until a total volume of 1.5 L was drawn through the device. Four inhalation cycles were pulled through the device for the adult and pediatric pressure drops.
Evaluation of Fluidized Bed High-Dose Device (FB-DPI)
To characterize the aerosolization performance of the FB-DPI, EEG-Cipro formulation weights of 25, 50, and 100 mg were considered. Evaluation of 25 mg was used for direct comparison with the CC90-3D inhaler whereas 50 and 100 mg were considered as high-doses for pediatric and adult applications, respectively. The appropriate mass was weighted and placed in the prototyped dosing sphere, which was then loaded into the FB-DPI. The powder was then aerosolized into the NGI at an airflow rate corresponding to both a 2 and 4 kPa pressure drop across the device. For the adult 4 kPa pressure drop, powders were aerosolized at 60 LPM until a total air volume of 4 L was drawn through the inhaler. For the pediatric 2 kPa pressure drop, the powder was aerosolized at 45 LPM until a total volume of 1.5 L was drawn through the device, which is consistent with in vivo data for an approximately 7-year-old child.13,28 As in the other cases, four inhalation cycles were implemented for each test. All measurements with the EEG-Cipro formulation were made with three replicates.
Particle Size Characterization
The stages of the impactor were coated with silicone spray to minimize particle bounce and re-entrainment. The powders were aerosolized with the DPI in a horizontal position attached to the pre-separator on the NGI using a rubber mold made specifically for the mouthpiece of this inhaler to ensure a perfect seal. To allow for horizontal positioning of the inhaler, as it would be used by a patient, and avoid the use of an induction port, the NGI was positioned on its side (oriented vertically). This positioning of the NGI is not expected to affect sizing performance due to the reliance on impaction and not sedimentation for aerosol capture. To assess the total aerosol size distribution in the absence of a lactose carrier, the USP induction port was not used in this research and development study. After aerosolization, drug retained in the dosing sphere or capsule, device, and the drug collected on the pre-separator, impaction plates and the filter were extracted by washing with deionized water for quantitative HPLC analysis. The cut-off diameters of each NGI stage at a specific airflow rate were calculated using the formula specified in USP 35 (Chapter 601, Apparatus 5).
Device Retention, Emitted Dose, and Calculation of Aerosol Metrics
When using the EEG-Cipro formulation, the loaded Cipro dose was determined from the initial weight of the powder taken for aerosolization and the percent of Cipro content in the EEG formulation as measured by content uniformity. The mass of Cipro retained in the dosing sphere, or capsule, and device was determined by HPLC and expressed as a percentage of the loaded Cipro dose. Emitted dose was calculated by subtracting the mass of Cipro retained in the dosing sphere and device from the loaded Cipro dose. FPF of the EEG formulation (FPF<5µm/ED) and submicrometer FPF (FPF<1µm/ED) were defined as the fraction less than 5 and 1 µm, respectively, expressed as a percentage of the ED. MMAD, FPF<5µm/ED, and FPF<1µm/ED were calculated from linear regression equations resulting from cumulative percentage mass vs. ln(cut-off diameter) of the respective stages on the NGI plots.
Results
Effects of Chamber Size and Inlet Configuration on Vibrational Amplitude
Results for the optimization of the chamber size, inlet configuration, and mixing ball size are shown in Table 1. These values are the peak-to-peak voltage averages output from the piezoelectric averaged over five repetitions (vibrational amplitude). The results were verified visually and indicated that the designs with the highest vibrational amplitude values produced the highest amount of ball movement. The three different mixing ball sizes, along with the 25 mm chamber and Inlet 5 (Fig. 2e) produced the most active ball movement. The different mixing ball sizes did not show any significant difference in the ball movement of the optimum system (Table 1), so the largest ball size, 4.76 mm, was selected. Based on this evaluation of maximum vibrational amplitude at a constant inhalation flow rate, the leading design used in the subsequent experiments implemented a 25 mm chamber diameter with airflow Inlet 5 and 4.76 mm mixing balls.
Effect of Powder Dose Sphere on Emitted Dose
The initial emptying results using PEARLITOL 25C are shown in Table 2 and include the total ED from the inhaler and the percentage of the powder released from the dosing sphere after a total of four inhalations at 60 LPM for 4 s. All of the designs, excluding the two hole design, performed well in terms of ED, however this test provided no information as to the emptying of the inhaler during each individual inhalation. The design goal was to produce relatively uniform release of the powder over each of the four inhalations.
Table 3 illustrates the cumulative dose emptying for each of the four inhalation cycles achieved by each configuration of the dosing sphere. The two hole design achieved a consistent release, but the overall ED was low at 58.8%. Without the dose sphere, nearly the entire ED was released in the first inhalation (80.5%), and only increased to 81.4% with four inhalations. The four and six hole designs outperformed the 4 Hole-90° design in terms of overall emptying in this test, but the 4 Hole-90° design produced the more consistent release of the powder that was desired. Specifically, for the four and six hole designs 61.3 and 85.4% of the powder was released in the first breath, respectively. The 4 Hole-90° design only released 36.9% of the powder in the first breath, then 63.3%, cumulatively, in the second breath. Based on both good emptying and consistent release, the 4 Hole-90° design was selected for subsequent experiments. The final design of the dosing sphere for the adult pressure drop, shown in Fig. 3, consisted of an outside diameter of 12 mm, inside diameter of 10 mm, and four 0.5 mm holes with centerlines that intersect perpendicularly through the middle of the sphere (4 Hole-90° design). The dosing sphere for the pediatric pressure drop was of the same design, but with an inside diameter of 8 mm and an outside diameter of 9.4 mm to keep the ball as light as possible. These designs were implemented in the final testing of the aerosolization performance of the device using the EEG-Cipro formulation.
Results of CC90-3D Inhaler with High-Dose
For this high-dose study, the CC90-3D inhaler was very effective at deaggregating the EEG-Cipro powder with the adult pressure drop of 4 kPa, even at its maximum fill mass of 25 mg, as shown in Table 4. As expected with the larger mass, as well as using multiple inhalations, the ED increased to 88.6% while the MMAD was found to be 1.55 μm, only a slight increase over the previous study of Behara et al.2 FPF<5µm/ED and FPF<1µm/ED values were similar to the previous study with only a slight drop in the FPF<1µm/ED value from 31.4%, as reported previously, to 28.8% with the larger mass.2 However, when the pediatric pressure drop was used with the 25 mg formulation mass, there appeared to be insufficient airflow to levitate the capsule and produce the aerosol. In contrast, the previous study of Behara et al.2 which implemented a 2 mg mass, showed consistent performance of the device across pressure drops of 2–6 kPa. As a pressure drop of 2 kPa and formulation weight of 25 mg is outside of the initial design criteria of the CC90-3D inhaler and ED performance was poor, these results are not presented. However, it is expected that the CC90-3D inhaler can be modified to perform well under these conditions by optimization of the airflow inlet size and capsule chamber dimensions to allow for levitation of the capsule at reduced flow rates.
Results of the High-Dose Fluidized Bed Device (FB-DPI)
The high-dose device was tested using 25 mg of the EEG-Cipro powder formulation for comparison with the CC90-3D inhaler and the results are displayed in Table 4. The aerosolization performance of the device at the adult pressure drop was similar to that of the CC90-3D inhaler with a MMAD of 1.53 μm and a FPF<5µm/ED and FPF<1µm/ED of 93.8 and 31.3%, respectively. However, the ED of 59.8% was significantly lower than with the CC90-3D device with 25 mg of powder. The ED of the FB-DPI increased to 71.4% when 100 mg was used while still achieving a 1.53 μm MMAD, as well as a FPF<5µm/ED of 93.3% and FPF<1µm/ED of 36.4% as shown in Table 5. The pediatric pressure drop and 25 mg loaded mass produced an ED of 57.5%, with only 12.4% retention in the dosing sphere, but 30.2% device retention. As expected with a lower flow rate, the MMAD increased to 1.81 μm and the FPF<1µm/ED decreased to 20.0%, but the FPF<5µm/ED remained similar at 93.0%. The design of the dosing sphere for the pediatric pressure drop limited the maximum mass to 50 mg instead of 100 mg with the adult model. The results for the pediatric pressure drop using 50 mg of powder are compared to the adult pressure drop at 100 mg in Table 5. At 2 kPa and 50 mg loaded mass with the pediatric dose sphere, the device produced an ED of 59.8%, a MMAD of 1.80 μm, a FPF<5µm/ED of 92.3%, and a FPF<1µm/ED of 21.8%, which is comparable to the 25 mg data.
In a final set of experiments, the mixing balls were removed from the system and the motion of the dosing sphere alone was used to deaggregate and aerosolize the powder. Results at a 4 kPa pressure drop with the adult dose delivery sphere and 25 mg loaded mass are displayed in Table 6 for the FB-DPI without the mixing balls. Results indicated an ED of 73.8% without the mixing balls, which was significantly (p < 0.05; t test) improved compared to the similar case with the balls (59.8%; Table 4, FB-DPI 4 kPa). However, there were no significant changes in the aerosol quality when the balls were removed with an MMAD of 1.53 μm, FPF<5µm/ED of 95.1%, and FPF<1µm/ED of 31.4%.
Discussion
A primary outcome of this study is the first evaluation of an inhaler based on a fluidized bed design. The design of the inhaler incorporating mixing balls caused a significant decrease in the aerosol ED compared to the inhaler without the mixing balls with more drug retention in both the dosing sphere and the device (absolute difference of 16%), but the MMAD was unaffected by the presence of the mixing balls. This is likely because of the increased surface area, provided by the mixing balls, to which the powder could adhere. The movement of the dose sphere was potentially hindered by the mixing balls, thus increasing the retention in the dosing sphere.
The previously developed CC90-3D inhaler was able to produce a very high quality aerosol with a 25 mg loaded mass at the adult pressure drop of 4 kPa. However, four capsules and four inhalations per capsule would be required to achieve the same nominal loaded formulation mass as the 100 mg FB-DPI device. The performance of the CC90-3D device became extremely limited at the pediatric pressure drop with a weight of 25 mg, which was beyond the initial design parameters of the inhaler. It is expected that the capsule chamber of the CC90-3D inhaler can be redesigned to allow for effective operation at this higher formulation weight compared with the 2 mg weight considered by Behara et al.;2 however, this optimization is beyond the scope of the current study.
Compared with the previously developed CC90-3D inhaler at a formulation weight of 25 mg and adult pressure drop of 4 kPa, the optimal FB-DPI device produced nearly identical aerosol characteristics but the ED was reduced from 88.6 to 59.8% (Table 4). The clear advantage of the FB-DPI is the ability to increase the loaded mass to 100 mg as considered in Table 5. Increasing the loaded mass to 100 mg at the adult pressure drop did not change the aerosolization characteristics and increased the ED to 71.4%. This increase in ED associated with increased loaded mass is due to the internal surface area of the dosing sphere, which is larger than the internal surface area of the capsules used in the CC90-3D inhaler, in order to hold more powder.
By using a combination of the fluidized bed device and the EEG powder formulation, the FB-DPI was able to produce an aerosol much smaller than that of the ORBITAL device using the co-spray-dried formulation, with an MMAD less than half the size (1.53 vs. 4.0 µm) and with much higher FPFs (93.8 vs. 42%).30 It should be noted that the primary particle size of the EEG-Cipro formulation was in the submicrometer range unlike the 2.9 µm ORBITAL formulation. The ED of the FB-DPI after four inhalations was approximately 71.4% compared with the ORBITAL device that appeared to emit approximately 75% of its dose at four inhalations. The ORBITAL was also able to deliver a formulation mass of up to 400 mg, which could offset the expected higher mouth-throat depositional loss associated with using a larger aerosol MMAD.
The optimum fluidized bed device that resulted from this study had the following characteristics: 25 mm chamber diameter, Inlet #5, 4.76 mm mixing ball diameter, and the 4 Hole-90° dose sphere. This device was able to produce a 1.53 μm MMAD aerosol with a FPF<5µm/ED of 93.3%, a FPF<1µm/ED of 36.4%, and an ED of 71.4% when used at the adult pressure drop and maximum tested formulation weight of 100 mg. When used at the pediatric pressure drop, the device was able to produce a 1.80 μm MMAD aerosol with a FPF<5µm/ED of 92.3%, a FPF<1µm/ED of 21.8%, and an ED of 59.8% using the maximum tested pediatric formulation weight of 50 mg. In both the adult and pediatric cases, the small aerosol (i.e., MMAD <2 µm) is expected to produce low MT depositional loss. For example, Son et al.25 previously demonstrated that an EEG aerosol with a MMAD of approximately 1 µm produced a MT depositional loss of <5%, compared with 80% for a commercial formulation and inhaler. Using a 3D rod array DPI and EEG formulation, MT depositional loss was reduced to <3%.26 For the adult inhalation conditions, the shortcoming of the optimized FB-DPI is the ED of 71.4%, whereas previous high efficiency DPIs have achieved ED values >75%.1,2
Testing the device without the mixing balls indicated that ED could be increased without altering the performance. This was an interesting finding considering that fluidized beds are known to contribute to powder deaggregation and are often used in industry to produce high quality fine aerosols.12 An additional test of the vibrational amplitude without the mixing balls but including the dose sphere indicated a value of 566.4, which is higher than the values reported in Table 1 for the FB-DPI designs with mixing balls and supports an association between the measured vibrational amplitude and DPI performance. In contrast, increased vibrational frequency created by the mixing balls may reduce vibrational amplitude and limit ED. Furthermore, the use of smaller mixing balls, as with the studies of Lind et al.16 and Prenni et al.19 for packed beds, may further decrease ED due to increased surface area of the spheres as a whole and likely increased vibrational frequency. As a result, the high dose device can be simplified and improved by removing the mixing balls and only retaining the dosing sphere and inhaler body. These findings motivate further study of the high dose DPI in order to maximize ED and deaggregation with the simplest possible device. However, this optimization is beyond the scope of the current study, which was intended to characterize the performance of an inhaler that was based on using the well recognized approach of a fluidized bed for aerosol deaggregation. As previously described, the use of CFD simulations together with concurrent in vitro experiments can be applied to further optimize the device design in a quantitative manner.11,17,18
Considering the pediatric delivery conditions and 50 mg formulation weight, performance of the FB-DPI appears acceptable. Shortcomings of the device at 2 kPa appear to be an ED of ~60% and a small increase in particle size with a MMAD of 1.8 µm. A recent study of commercial inhalers tested under pediatric delivery conditions produced MT deposition values of 60–80%.3 In contrast, our preliminary MT deposition results with EEG formulations and pediatric airway conditions indicate losses <10%. Based on results for the FB-DPI device at 100 mg and 4 kPa, it is expected that removing the mixing balls from the pediatric inhaler will again improve ED. Further decreases in MMAD, if needed, can likely be achieved through optimization of the dosing sphere (e.g., hole position and size) and modifying the number of required inhalations.
Limitations of the current study include use of vibrational amplitude and Pearlitol powder to screen the initial designs. Vibrational amplitude was found to be highest in the case without the mixing balls, which implies that use of this parameter as a screening tool for DPI performance may be valuable. However, vibrational frequency was not considered and could potentially reduce ED as in the study of Behara et al.1 The highly dispersive EEG formulations were expected to deaggregate like much larger Pearlitol particles; however, this association has not been proven. In the sizing experiments, neither an induction port nor a mouth-throat geometry was used in order to best quantify the size distribution of the aerosol leaving the inhaler and entering the respiratory tract. It was not our intent to perform compedial quality control experiments; however, it is expected that the preseparator captures the drug that would have deposited in the induction port (or mouth-throat) considering that it has a smaller cutoff size. As a result, it is expected that FPF calculations were not biased based on exclusion of the MT geometry. In addition, while the stages of the NGI were coated with a silicone spray, as suggested by USP, it is acknowledged that with the higher masses of powder used in this study, particle bounce may not have been completely prevented. Some small powder deposits were seen on the nozzles of the NGI after the experiments suggesting some particle bounce may be present, which may lead to small changes in the particle size distribution.8,21
Additional limitations of this study include the investigation of a single chamber design and orientation, the evaluation of the device only with an inlet at the top of the chamber, and the evaluation of a single EEG drug formulation. Other chamber designs could prove to be more effective at lowering the device retention, but could also have a negative effect on the particle size. Positioning the inlet on the side or the back of the inhaler could also have an effect on the performance of the device and needs to be studied further for confirmation. The EEG-Cipro powder was the only formulation studied, but the data from the CC90-3D device was similar to the EEG-Albuterol Sulfate (AS) formulation used in the study by Behara et al.2
Conclusions
In conclusion, the classic deaggregation method of a fluidized bed was implemented in a compact hand-held oral inhaler for the first time and optimized for the delivery of high dose dry powder aerosols. Based on previous performance of new high efficiency inhalers originally designed for lower doses, the optimized FB-DPI provided excellent deaggregation of the aerosol but decreased ED under adult and pediatric inhalation conditions.1,2 Removal of the mixing balls improved emitted dose while maintaining excellent deaggregation, such that the combination of the powder formulation with the mixing chamber and dose sphere is likely most responsible for the high quality aerosol that was produced. Still, the combination of the FB-DPI and EEG powders with or without the mixing balls achieved MMADs and FPFs that are far superior to currently available products. Compared with the newly proposed high dose Orbital inhaler, the strength of the FB-DPI is its improved aerosolization.30 However, the Orbital device is currently capable of delivering 400 mg, which may be advantageous in some applications. Our approach is to instead load 100 mg and be four times more efficient at targeted lung delivery, which is to be determined in future studies. Analysis of the fluidized bed design indicated that removal of the mixing balls and maintaining the newly designed dosing sphere and chamber increased ED to 73.8% while maintaining excellent aerosolization performance. As a result, it is concluded that the FB-DPI is highly effective but can be simplified by maintaining only the newly designed dosing sphere and inhaler chamber. Future studies will seek to optimize the simplified new design for high dose DPI delivery to both adults and children.
Abbreviations
- AS:
-
Albuterol sulfate
- Cipro:
-
Ciprofloxacin hydrochloride
- DPI:
-
Dry powder inhaler
- ED:
-
Emitted dose
- EEG:
-
Excipient enhanced growth
- FB:
-
Fluidized bed
- FPF:
-
Fine particle fraction
- HPLC:
-
High-performance liquid chromatography
- HPMC:
-
Hydroxypropyl methylcellulose
- MMAD:
-
Mass median aerodynamic diameter
- MT:
-
Mouth-throat
- PTFE:
-
Polytetraflouroethylene
- PVDF:
-
Polyvinylidene fluoride
- SD:
-
Standard deviation
References
Behara, S. R. B., D. R. Farkas, M. Hindle, and P. W. Longest. Development of a high efficiency dry powder inhaler: effects of capsule chamber design and inhaler surface modifications. Pharm. Res. 31:360–372, 2014.
Behara, S. R. B., P. W. Longest, D. R. Farkas, and M. Hindle. Development and comparison of new high-efficiency dry powder inhalers for carrier-free formulations. J. Pharm. Sci. 103:465–477, 2014.
Below, A., D. Bickmann, and J. Breitkreutz. Assessing the performance of two dry powder inhalers in preschool children using an idealized pediatric upper airway model. Int. J. Pharm. 444(1–2):169–174, 2013.
Bilton, D., P. Robinson, P. Cooper, C. G. Gallagher, J. Kolbe, H. Fox, A. Jaques, and B. Charlton. Inhaled dry powder mannitol in cystic fibrosis: an efficacy and safety study. Eur. Respir. J. 38(5):1071–1080, 2011.
Corcoran, T. E., R. Venkataramanan, R. M. Hoffman, M. P. George, A. Petrov, T. Richards, S. Zhang, J. Choi, Y. Y. Gao, C. D. Oakum, R. O. Cook, and M. Donahoe. Systemic delivery of atropine sulfate by the microdose dry-powder inhaler. J. Aerosol. Med. Pulm. Drug Deliv. 26(1):46–55, 2013.
de Boer, A. H., P. Hagedoorn, R. Woolhouse, and E. Wynn. Computational fluid dynamics (CFD) assisted performance evaluation of the Twincer™ disposable high-dose dry powder inhaler. J. Pharm. Pharmacol. 64(9):1316–1325, 2012.
Geller, D. E., J. Weers, and S. Heuerding. Development of an inhaled dry-powder formulation of tobramycin using PulmoSphere™ technology. J. Aerosol. Med. Pulm. Drug Deliv. 24(4):175–182, 2011.
Grasmeijer, F., P. Hagedoorn, H. W. Frijlink, and A. H. de Boer. Characterisation of high dose aerosols from dry powder inhalers. Int. J. Pharm. 437(1–2):242–249, 2012.
Green, D. W. Perry’s Chemical Engineers’ Handbook (7th ed.). New York: McGraw-Hill, 1997.
Hindle, M., and P. W. Longest. Condensational growth of combination drug-excipient submicrometer particles for targeted high efficiency pulmonary delivery: evaluation of formulation and delivery device. J. Pharm. Pharmacol. 64(9):1254–1263, 2012.
Hindle, M., and P. W. Longest. Quantitative analysis and design of a spray aerosol inhaler. Part 2: improvements in mouthpiece performance. J. Aerosol. Med. Pulm. Drug Deliv. 26(5):237–247, 2013.
Hinds, W. C. Aerosol Technology: Properties, Behavior, and Measurement of Airborne Particles. New York: Wiley, 1999.
ICRP. Human Respiratory Tract Model for Radiological Protection. New York: Elsevier Science Ltd., 1994.
Islam, N., and M. J. Cleary. Developing an efficient and reliable dry powder inhaler for pulmonary drug delivery—a review for multidisciplinary researchers. Med. Eng. Phys. 34:409–427, 2012.
Keller, Manfred., and Joerg. Schierholz. Have inadequate delivery systems hampered the clinical success of inhaled disodium cromoglycate? Time for reconsideration. Expert Opin. Drug Deliv. 8(1):1–17, 2010.
Lind, T., S. Danner, and S. Guentay. Monodisoerse fine aerosol generation using fluidized bed. Powder Technol. 199(3):232–237, 2010.
Longest, P. W., and M. Hindle. Quantitative analysis and design of a spray aerosol inhaler. Part 1: effects of dilution air inlets and flow paths. J. Aerosol. Med. Pulm. Drug Deliv. 22(3):271–283, 2009.
Longest, P. W., Y.-J. Son, L. T. Holbrook, and M. Hindle. Aerodynamic factors responsible for the deaggregation of carrier-free drug powders to form micrometer and submicrometer aerosols. Pharm. Res. 30:1608–1627, 2013.
Prenni, A. J., R. L. Siefert, T. B. Onasch, M. A. Tolbert, and P. J. DeMott. Design and characterization of a fluidized bed aerosol generator: a source for dry, submicrometer aerosol. Aerosol Sci. Technol. 32(5):465–481, 2000.
Prime, D., A. C. Grant, A. L. Slater, and R. N. Woodhouse. A critical comparison of the dose delivery characteristics of four alternative inhalation devices delivering salbutamol: pressurized metered dose inhaler, Diskus inhaler, Diskhaler inhaler, and Turbuhaler inhaler. J. Aerosol Med. 12(2):75–84, 1999.
Rissler, Jenny., Lars. Asking, and Jakob. Kisbye Dreyer. A methodology to study impactor particle reentrainment and a proposed stage coating for the NGI. J. Aerosol. Med. Pulm. Drug Deliv. 22(4):309–316, 2009.
Ruppert, C., T. Kuchenbuch, M. Boensch, S. Schmidt, U. Mathes, V. Hillebrand, I. Henneke, P. Markart, I. Reiss, R. T. Schermuly, W. Seeger, and A. Gunther. Dry powder aerosolization of a recombinant surfactant protein-C-based surfactant for inhalative treatment of the acutely inflamed lung. Crit. Care Med. 38(7):1584–1591, 2010.
Sham, J. O.-H., Y. Zhang, W. H. Finlay, W. H. Roa, and R. Lobenberg. Formulation and characterization of spray-dried powders containing nanoparticles for aerosol delivery to the lung. Int. J. Pharm. 269:457–467, 2004.
Smith, I. J., J. Bell, N. Bowman, M. Everard, S. Stein, and J. G. Weers. Inhaler devices: what remains to be done? J. Aerosol. Med. Pulm. Drug Deliv. 23:S25–S37, 2010.
Son, Y.-J., P. W. Longest, and M. Hindle. Aerosolization characteristics of dry powder inhaler formulations for the excipient enhanced growth (EEG) application: effect of spray drying process conditions on aerosol performance. Int. J. Pharm. 443:137–145, 2013.
Son, Y.-J., P. W. Longest, G. Tian, and M. Hindle. Evaluation and modification of commercial dry powder inhalers for the aerosolization of submicrometer excipient enhanced growth (EEG) formulation. Eur. J. Pharm. Sci. 49:390–399, 2013.
Tian, G., P. W. Longest, X. Li, and M. Hindle. Targeting aerosol deposition to and within the lung airways using excipient enhanced growth. J. Aerosol. Med. Pulm. Drug Deliv. 26(5):248–265, 2013.
Tiddens, H. A., D. E. Geller, P. Challoner, R. J. Speirs, K. C. Kesser, S. E. Overbeek, D. Humble, S. B. Shrewsbury, and T. A. Standaert. Effect of dry powder inhaler resistance on the inspiratory flow rates and volumes of cystic fibrosis patients of six years and older. J. Aerosol Med. Depos. Clear. Eff. Lung 19(4):456–465, 2006.
Weers, J. G., R. C. Andrew, N. Rao, K. Ung, A. Haynes, S. K. Khindri, S. A. Perry, S. Machineni, and P. Colthorpe. In vitro–in vivo correlations observed with indacaterol-based formulations delivered with the breezhaler®. J. Aerosol. Med. Pulm. Drug Deliv. 2014.
Young, P. M., J. Crapper, G. Philips, K. Sharma, H.-K. Chan, and D. Traini. Overcoming dose limitaitons using the orbital multi-breath dry powder inhaler. J. Aerosol. Med. Pulm. Drug Deliv. 26:1–10, 2013.
Zhou, Qi., Patricia. Tang, Sharon. Shui. Yee. Leung, John. Gar. Yan. Chan, and Hak.-Kim. Chan. Emerging inhalation aerosol devices and strategies: where are we headed? Adv. Drug Deliv. Rev. 75:3–17, 2014.
Zhu, J., and Y. Ma. A New breath-activated, excipient-free dry powder inhaler and a rotating fluidized bed powder dispenser for pulmonary drug delivery. Respir. Drug Deliv. 925–930:2006, 2006.
Acknowledgments
The authors gratefully acknowledge financial support from the National Heart, Lung, and Blood Institute through Award R01 HL107333. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
Conflict of interest
The authors are employees of Virginia Commonwealth University. Virginia Commonwealth University is seeking patent protection with respect to the technology described, which if licensed may result in a financial interest to the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor John H. Linehan oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Farkas, D.R., Hindle, M. & Longest, P.W. Characterization of a New High-Dose Dry Powder Inhaler (DPI) Based on a Fluidized Bed Design. Ann Biomed Eng 43, 2804–2815 (2015). https://doi.org/10.1007/s10439-015-1335-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-015-1335-2