Abstract
While supine, fluid moves from the legs and accumulates in the chest and neck. However, patterns of rostral fluid shift are not clear. Furthermore, real-time measurement of neck fluid volume has not been investigated. The objective of this study was to investigate the dynamics of rostral fluid shift in men and women. We developed a bioelectrical impedance system to measure leg, abdominal, thoracic and neck fluid volumes (LFV, AFV, TFV, NFV) continuously. Forty healthy non-obese adults (20 men) lay supine for 90 min while fluid volumes were measured. After 90 min, a similar volume of fluid shifted out of the legs in both sexes (p = 0.079), but men accumulated more fluid in their thorax (63 ± 6 vs. 44 ± 11 ml, p = 0.016) and neck (17 ± 2 vs. 14 ± 1 ml, p = 0.029) than women. In both sexes, the increase in NFV caused a significant increase in neck circumference, which was greater in men (p = 0.009). Furthermore, 80% of rostral fluid shift would occur in the first 2 h of lying supine. These results suggest that greater fluid shift into the thorax and neck may contribute to the higher prevalence of sleep apnea in men than in women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Moving from the standing to the recumbent position is accompanied by a redistribution of body fluid due to gravitational and Starling’s forces.45,48,51 Based on Starling’s forces, the balance between capillary hydrostatic and colloid osmotic pressures influences the passive movement of fluid between the capillaries and interstitial space.40 While standing, capillary pressure in the legs greatly exceeds the pressure required for the movement into the interstitial space. As a consequence, intravascular fluid volume of the leg decreases while interstitial and total fluid volume of the leg increases3,10,45,47,51 at a filtration rate which is proportional to venous pressure.22,25,51 When lying in bed, the reverse occurs: fluid is reabsorbed from the interstitial into the intravascular compartment of the legs,3,10,45,48 which moves rostrally to the upper body through the vascular system.1,2,15,44 This is associated with a reduction in leg fluid volume (LFV) and reciprocal increases in thoracic and head blood volumes.2,15 Previous studies showed that rostral fluid shift out of the legs and its accumulation in the neck can increase neck circumference (NC)13,21,34 and pharyngeal tissue pressure leading to narrowing of the upper airway.37 However, due to technical limitations, neck fluid volume (NFV) was not measured in these studies. Furthermore, the pattern and time course of fluid redistribution out of the legs and its accumulation in the upper body when assuming the recumbent position has not been previously investigated.
Recently, we showed that rostral fluid shift out of the legs could affect the pathophysiology of the respiratory system. We showed that the amount of fluid coming out of the legs was positively correlated with increases in NC,13,21,34 narrowing of the upper airway14,37,38 and increases in its resistance5,20 and collapsibility.41,42 Furthermore in heart failure patients, nocturnal fluid shift out of the legs was associated with a low PCO2, presumably due to increases in thoracic fluid volume (TFV) which could increase pulmonary congestion, stimulate pulmonary vagal irritant receptors that provoke hyperventilation and reduce PCO2.20,53 While these studies demonstrated strong evidence for the role of rostral fluid shift on the pathophysiology of the respiratory system, they were subject to some technical limitations. TFV and NFV were not measured; but were assessed indirectly by the changes in PCO2 and NC, respectively. Also, LFV was only measured at the beginning and end of the studies; therefore, the time course and pattern of fluid redistribution out of the legs was not determined. Similarly, the time course of fluid accumulation in the chest and neck is not known. Furthermore, the effects of rostral fluid shift on the upper airway collapsibility and resistance and PCO2 were only observed in men, but not in women.21,42 Therefore, it is possible that due to physiological differences, men and women have different patterns of rostral fluid redistribution. However, differences in the pattern of rostral fluid shift between sexes have not been investigated.
The objective of this study was to develop a system to measure fluid volumes of multiple body segments in real time to determine the pattern and time-course of rostral fluid redistribution from the lower body to the upper body while supine. We hypothesized that men would have greater fluid redistribution into the thorax and neck than women over a given time period. We also hypothesized that women would have greater fluid accumulation in the abdomen than men because of greater venous capacitance in their uterine and ovarian venous plexi, absent in men,18 in which fluid displaced from the legs might collect while recumbent.
Methods
Participants
Inclusion criteria were healthy men and women between 18 and 70 years of age, with a body mass index (BMI) <30 kg/m2, and a blood pressure of ≤140/90 mmHg. Women were included who were premenopausal and not having their menstrual period at the time of experiments. Participants were instructed to refrain from consuming coffee or energy drinks on the study day. The exclusion criteria were a history of hysterectomy, cardiovascular, renal, neurological or respiratory diseases, taking any medication for them, or taking any over the counter medication that might influence fluid retention such as non-steroidal anti-inflammatory agents. Participants were recruited by advertisement.
Blood Pressure, Upper Airway Cross-Sectional Area, and Neck Circumference
At the beginning of the study, heart rate, systolic and diastolic blood pressures were measured three times using an automated sphygmomanometer with 2-min intervals between successive measurements that were averaged. Then with participants supine, upper airway cross-sectional area (UA-XSA) was assessed by acoustic pharyngometry12 and NC by tape measure just above the cricothyroid cartilage. A line was drawn at this level to ensure that NC measurements at the end of experiments were made at the same level as at baseline.34,53
Fluid Measurements
Bioelectrical impedance is a non-invasive technique to estimate fluid volume of tissues. Based on Ohm’s law, the resistance of a tissue to electric current is inversely related to its fluid content and directly related to its length: R = ρL 2/V, where ρ is the resistivity of fluid, L is the segment’s length, and V is the fluid volume.6,17,23 This equation has been widely used to estimate total body water where L is replaced by the subject’s height.8,55 Bioelectrical impedance analysis was also applied to measure fluid volumes in various body segments. In most studies V = ρL 2/R was used to estimate the fluid volume with L representing the segment’s length.4,26,43,56 This equation is based on the assumption that each body segment is a cylinder, where the length is much greater than the diameter of the cylinder. While this assumption may be valid for legs or arms, it is less accurate for other body segments such as the abdomen, chest and neck. Considering each body segment as a truncated cone, its fluid volume can be estimated as:11,50
where C 1 and C 2 are the segment’s circumferences at the level of the sensing electrodes, and ρ is blood resistivity. Frequency of the injecting electrical current affects the tissue resistance; at frequencies lower than 100 kHz, the cell membrane acts as an insulator and the measured resistance mainly represents extra-cellular fluid.6 Extra-cellular resistivity, ρ, can change with age, sex, and hematocrit level.29 However, in a study of 73 healthy subjects, the extracellular resistivity was estimated to be 47 Ω cm.6
In order to measure fluid volume in various body segments, we used four impedance measurement modules (Biopac Systems, EBI100C). For each segment, two electrodes injected high frequency ([12.5–100] kHz), low amplitude (400 μA) current to the segment; and two electrodes measured voltage to estimate bioelectrical impedance (R in Eq. 1). To electrically isolate different body segments for bioelectrical impedance measurements, we used a different injecting frequency for each segment. Frequencies of 25, 12.5, 100 and 50 kHz were used to measure the bioelectrical impedance of leg, abdomen, thorax, and neck, respectively. Furthermore, the alignment and polarity of electrodes for each segment were designed to minimize the current artifact from adjacent segments. To measure LFV, voltage measuring electrodes were placed on the ankle and upper thigh of the right leg; to measure abdominal fluid volume (AFV), on the right posterior part of the trunk one inch below the xiphoid process, and on the posterior, superior part of the femur; to measure TFV, on the midline of the posterior aspect of the chest at the superior border of the scapula and at the same level as the xiphoid process; and to measure NFV, on the right side of the neck below the right ear and at the base of the neck. For each segment, the injecting electrodes were placed one inch from the sensing electrodes. The electrodes were secured to the skin with adhesive tape. At the beginning of the study, length and circumferences of each segment were measured with a measuring tape and Eq. 1 was used to estimate fluid volume of each segment. For NFV, the value of NC was used for both circumferences (C1, C2).
In a preliminary study, we simultaneously measured below-the knee LFV with the method described above and with a validated commercial device (Xitron 4200, Hydra ECF/ICF, Xitron Technologies Inc., San Diego, CA).50 The Xitron device measures multi-frequency bioelectrical impedance to estimate intra- and extra-cellular fluid volumes. Paired t test was used to compare the results of fluid measurements from our system with the extra-cellular fluid volumes measured by Xitron.
Ethics Statement
The study protocol was reviewed and approved by the Research Ethics Board of University Health Network and all participants provided written consent prior to participation.
Protocol
Participants arrived at the laboratory in the early afternoon. While seated, their heart rate and blood pressure were measured after which they were instrumented for bioelectrical impedance measurements. All experiments were performed in the same room with a temperature maintained between 22 ºC and 24 °C. To reduce possible effects of urine volume on the measurement of AFV, all subjects voided before starting the experiments. Just prior to the beginning of experiments, participants stood up motionless for 5 min. Participants then lay supine on a bed while awake with no pillow. LFV, AFV, TFV and NFV were recorded continuously during experiments (Fig. 1). To minimize any potential influence of movement artefacts on bioelectrical impedance measurements, participants were instructed to remain still during the recordings. The duration of the study was limited to 90 min for two reasons: first, it was shown that when moving from upright to supine, it takes between 60 and 90 min to reach a balance in LFV and plasma volume.3,10 Second, in preliminary studies, most participants could not remain still beyond 90 min due to discomfort. NC, blood pressure, heart rate, and UA-XSA were measured before and after each experiment.
Schematic illustration of the experimental timeline and various measurements. Participants arrived at the sleep laboratory in the early afternoon. While seated, their heart rate and blood pressure were measured by an automated sphygmomanometer after which they were instrumented for bioelectrical impedance measurements. Before beginning the experiments, participants stood up motionless for 5 min. Then, they lay supine on a bed while awake with no pillow. While supine and at the beginning and end of the experiment, neck circumference (NC) was measured by tape measure just above the cricothyroid cartilage and upper airway cross-sectional area (UA-XSA) was assessed using acoustic pharyngometry. During experiments, leg, abdominal, thoracic, and neck fluid volumes (LFV, AFV, TFV, and NFV, respectively) were recorded continuously and simultaneously using bioelectrical impedance measurements. Measurements of blood pressure and heart rate were repeated at the end of study
Data Analysis
During the study, we measured changes (Δ) in NC, blood pressure, heart rate, and UA-XSA from baseline. Within each group of men or women, we investigated variations in fluid volumes of each segment over time. Within each group, the changes in blood pressure, heart rate, NC, and UA-XSA from baseline were compared by paired t tests for normally distributed data and Wilcoxon test for non-normally distributed data. Between sexes, the changes in blood pressure, heart rate, NC, and UA-XSA from baseline were compared by Student t-tests for normally distributed data and non-parametric ranked t test for non-normally distributed data. To compare the changes in fluid volumes of each body segment between sexes, we used analysis of covariance (ANCOVA). ANCOVA is a generalized form of analysis of variance (ANOVA) which is combined with regression analysis. ANCOVA evaluates the difference between groups while controlling for the effects of covariants. In our models for either ∆LFV, ∆AFV, ∆TFV, or ∆NFV, sex was included as the independent categorical factor and age, weight, height, BMI, body segments’ lengths and circumferences were included as the covariants to take into account differing anatomical factors between the sexes.
To investigate the time course of fluid redistribution over longer periods, different mathematical functions were examined to model the changes in fluid volumes. We found that a single exponential function was the best fit, thereby suggesting first-order single-time constant kinetics. For each subject, an exponential function was fitted to the variations in fluid volume of every segment as FV(t) = FVend − FVend × exp(−t/τ), where t is time, FV is either ΔLFV, ΔAFV, ΔTFV, or ΔNFV, and FVend is the expected final change in each segment’s fluid volume. Depending on whether FV of a particular segment increased or decreased, τ represented the time constant of growth or decay of FV, respectively. Mathematically, after 3τ, FV would reach 95% of FVend; which can be considered as the time required to reach the plateau point. For every individual and every segment, r 2 of the model and τ were calculated. To assess the time course of changes in segmental fluid volumes, τ for each segment was compared between sexes. For AFV, analysis of covariance was used to investigate whether patterns of fluid accumulation in the abdomen were influenced by sex or age. Statistical analyzes were performed by SAS 9.3 and a two-sided p value <0.05 was considered significant. Data are presented as mean ± SD.
Results
Characteristics of the Participants
Fifty two participants consented to participate in the study. One participant declined to continue the study before being instrumented. Eleven participants had movement artefacts in at least one of the bioelectrical impedance signals, and their data were excluded. A total of 40 participants completed the study; 20 men and 20 women whose characteristics are shown in Table 1. Age, systolic and diastolic blood pressure, heart rate, UA-XSA and abdominal length were similar for both sexes. Although weight, height, and BMI were lower in women, the percent of ideal body weight (IBW), a better means than BMI for comparing body habitus between the sexes, was similar in men and women. NC, the lengths of the leg, chest, and neck as well as the baseline values of LFV, AFV, TFV and NFV were lower in women than in men, as expected.
Fluid Redistribution in Various Body Segments Over Time
In 7 healthy non-obese adults, estimates of below the knee ∆LFV with our system were consistent with the extra-cellular ∆LFV measured with a commercial validated device.39.
Within Group Comparisons
Figure 2 depicts fluid redistribution in various body segments over time. In women, LFV decreased, and AFV, TFV, and NFV increased significantly after 90 min (ΔLFV, ΔTFV, and ΔNFV: p < 0.001, and ΔAFV: p = 0.002). The exponential functions describing variations in LFV, TFV, and NFV over time had an average r 2 of 0.99, 0.89, and 0.97 for ΔLFV, ΔTFV, and ΔNFV, respectively. The time constants of the exponential changes (τ) in LFV, TFV, and NFV were 67.2 ± 23.1, 63.9 ± 30.3, and 80.7 ± 44.4 min respectively. Based on these models, after 7 h which could resemble the sleep duration, ΔLFV, ΔTFV, ΔNFV would be (mean ± SE) −186 ± 13, 67 ± 8, and 20 ± 2 ml, respectively. However, neither an exponential nor any other model could be fitted to ΔAFV, because the patterns of fluid accumulation in the abdomen were highly variable among participants. After 90 min, NC increased 0.3 ± 0.3 cm (p < 0.001), but UA-XSA did not change significantly (Fig. 3). Also there were significant increases in systolic (7.3 ± 5.9 mmHg, p < 0.001), diastolic (2.1 ± 4.2 mmHg, p = 0.049), and mean arterial (3.9 ± 3.8 mmHg, p < 0.001) blood pressures and a decrease in heart rate (−7.4 ± 7.6 bpm, p = 0.001) after 90 min.
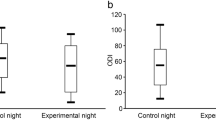
Variations in fluid volumes of different segments after lying supine for 90 min. This figure shows the absolute values of changes in segmental fluid volumes after lying supine for 90 min relative to the baseline (time 0 after lying supine): (a) leg fluid volume (ΔLFV), (b) abdominal fluid volume (ΔAFV), (c) thoracic fluid volume (ΔTFV), and (d) neck fluid volume (ΔNFV). Data are presented as mean ± SE. The average r 2 of exponential models for ΔLFV, ΔTFV, and ΔNFV were >0.90 in all subjects. The results show that for similar amount of fluid coming out of the legs in both men and women (a), men accumulate more fluid in their thorax (c) and neck (d). However, neither an exponential nor any other model could be fitted to ΔAFV, because the patterns of fluid accumulation in the abdomen were highly variable among subjects
Changes in neck circumference and upper airway cross-sectional area after lying supine for 90 min. (a) Relative to baseline, after lying supine for 90 min there was a significant increase in neck circumference (ΔNC) in both sexes, which was greater in men. (b) While after 90 min, upper airway cross-sectional area (ΔUA-XSA) decreased significantly in men, it did not change in women. However, the decrease in UA-XSA did not differ between the sexes. The p values above each bar represent the statistical significance of the changes in NC and UA-XSA from baseline
Similar to women, LFV decreased, while TFV and NFV increased significantly (p < 0.001) after 90 min in men (Fig. 2). However, in contrast to women, there was no increase in AFV after 90 min (p = 0.540). Similar to women, exponential functions were the best models to describe the pattern of ΔLFV, ΔTFV, and ΔNFV over time; the average r 2 of exponential models for ΔLFV, ΔTFV, and ΔNFV were 0.99, 0.94, and 0.97, respectively. The time constants (τ) of ΔLFV, ΔTFV, and ΔNFV were 71.5 ± 24.1, 105.3 ± 105.3, and 106.4 ± 71.9 min, respectively. Furthermore the models predicted that after 7 h, ΔLFV, ΔTFV, and ΔNFV would be (mean ± SE) −219 ± 16, 110 ± 13, and 28 ± 3 ml, respectively. Similar to women, after 90 min, there was a significant increase in NC (0.6 ± 0.3 cm, p < 0.001, Fig. 3), but in contrast to women, there was a significant decrease in UA-XSA (−0.4 ± 0.7 cm2, p = 0.003, Fig. 3). Similar to women, there were significant increases in systolic (8.1 ± 7.6 mmHg, p = 0.001), diastolic (5.3 ± 6.2 mmHg, p = 0.004), and mean arterial (6.2 ± 6.4 mmHg, p = 0.001) blood pressures and a decrease in heart rate (−8.3 ± 9.1 bpm, p = 0.002) after lying supine for 90 min.
While in all participants, LFV decreased and TFV and NFV increased over time, the pattern of fluid accumulation in the abdomen varied among participants. Variations in the fluid content of the abdomen appeared to represent a balance between outflow of fluid from the abdomen to the chest; and the inflow of fluid to the abdomen from the legs. We found two main patterns of variation in ∆AFV (examples are shown in Fig. 4). In the first type, there was an initial reduction in AFV followed by an increase in AFV after 90 min (Fig. 4a, d2) that was greater than the initial decrease in AFV (Fig. 4a, d1). As a consequence, there was a net increase in AFV so that the abdomen had some reservoir capacity. This pattern was observed in 35 participants, 20 women aged 36.3 ± 8.9 years and 15 men aged 34.5 ± 10.1 years. In the second type, there was continuous outflow of fluid from the abdomen and as a consequence, there was a net reduction in AFV (Fig. 4b). In this case, the abdomen did not act as a reservoir, but as a conduit for fluid. This pattern was observed in five participants, all men aged 50.2 ± 7.7 years. The results of ANCOVA showed that the interaction between age and sex was significantly different between participants with different patterns of fluid accumulation in the abdomen (Age * Sex: p = 0.010). This indicated that in older men, the abdomen acted more as a conduit than as a reservoir.
Different patterns of fluid accumulation in the abdomen while lying supine. There were two patterns of variations in abdominal fluid volumes (∆AFV) after lying supine for 90 min. In the first type (a), there was a net increase in AFV so that the abdomen had some reservoir capacity. This pattern was observed in 35 participants, 20 women aged 36.3 ± 8.9 years and 15 men aged 34.5 ± 10.1 years. In the second type (b), abdomen acted as a conduit for fluid and there was continuous outflow of fluid from the abdomen. This pattern was observed in older men (n = 5, aged 50.2 ± 7.7 years)
Between Group Comparisons
After 90 min, the increases in blood pressure and the decrease in heart rate were similar in men and women. Table 2 shows the effect of different anthropometric factors on the changes in LFV, AFV, TFV, NFV, NC, and UA-XSA after 90 min. Men had a non-significant tendency for more fluid coming out of their legs than women (p = 0.079); other factors such as age, weight, height and the physical dimensions of the leg did not have a significant effect on the changes in LFV. There was a borderline significant tendency for a greater increase in AFV in women than in men after 90 min (p = 0.053). Age was the other factor that significantly affected the amount of fluid accumulation in the abdomen; older participants accumulated less fluid in their abdomen after 90 min. Compared to women, men had greater increases in TFV and NFV (p = 0.016 and p = 0.029, respectively, Table 2 and Fig. 2), as well as a greater increase in NC (p = 0.009, Fig. 3a). None of the other anthropometric factors had any significant effect on the ∆TFV or ∆NFV (Table 2). While men accumulated more fluid in their neck with a significant decrease in UA-XSA, the decrease in UA-XSA did not differ significantly between the sexes (Fig. 3b).
Mathematical modeling beyond 90 min predict that while after 7 h the decreases in LFV would be similar in men and women, men would experience greater increases in TFV and NFV than women (p = 0.030 and p = 0.018, respectively). For all segments, τ was similar between the sexes; which indicates that the time for the fluid changes to reach the plateau is independent of sex. Based on the models, ΔLFV, ΔTFV, and ΔNFV would reach 80% of their final value after 110 min, 140 min, and 120 min, respectively. Including data of all participants, the increase in NC after 90 min correlated significantly with the increase in NFV (r = 0.575, p = 0.002, Fig. 5).
Discussion
This study has given rise to important and novel findings with implications for physiological monitoring. First, we demonstrated that patterns of fluid redistribution while supine within multiple body segments can be measured in real time by using bioelectrical impedance. Second, we found that for a similar amount of fluid moving out of the legs while supine for 90 min, men accumulated significantly more fluid in their thorax and neck than women. The differences remained significant even after controlling for differences in the physical dimensions of the thorax and neck, and other anthropometric factors between the sexes. The greater increase in NFV was also associated with a greater increase in NC in men than in women as well as a reduction in UA-XSA in men that was not observed in women. Third, our data demonstrated that fluid redistribution out of the legs and its accumulation in the thorax and neck followed exponential functions. To our knowledge, this is the first study to investigate the time course of fluid redistribution in various body segments while supine. Based on the exponential models, after 7 h supine which could resemble sleep duration, there would be no difference between men and women in the amount of fluid displaced from the legs; however, men would accumulate more fluid in their thorax and neck than women. These results confirm our hypothesis that upon assuming the recumbent position, men accumulate more fluid in their thorax and neck than women.
Differing effects of sex on rostral fluid shift could be one of the factors that put men at greater risk of developing sleep apnea than women. Sleep apnea is a common respiratory disorder, affects 5 and 10% of women and men, respectively, and increases the risk of cardiovascular morbidity and mortality.19,28,31 Recently, we showed that rostral fluid shift out of the legs could contribute to the severity of sleep apnea.49 Obstructive sleep apnea, the most common type of sleep apnea, occurs due to repetitive upper airway collapse during sleep. Rostral fluid shift out of the legs increases NC,13,21,34 narrows the upper airway14,37,38 and increases its resistance5,20 and collapsibility;41,42 all of which could contribute to the severity of obstructive sleep apnea.7 Central sleep apnea, rare in the general population, is common in fluid retaining states, such as heart failure.54 Central sleep apnea occurs when PCO2 during sleep falls below the apnea threshold and results in withdrawal of central drive to the respiratory muscles. In heart failure patients with central sleep apnea nocturnal fluid shift out of the legs is associated with a low PCO2, presumably due to increases in pulmonary congestion that would stimulate pulmonary vagal irritant receptors that provoke hyperventilation, reduce PCO2 and thereby predispose to central sleep apnea.20,53
Both in the general population and in patients with heart failure, obstructive sleep apnea is 2–3 times more prevalent in men than in women52,54 for reasons not fully understood. One factor appears to be that women have a shorter pharynx than men which in theory makes it less collapsible.27 On the other hand, the luminal dimension is smaller in women30 which should increase upper airway collapsibility. However, previous studies did not find any differences in upper airway collapsibility between healthy men and women during sleep or wakefulness.35,42 Sex hormones may be another factor that contributes to differences in susceptibility to obstructive sleep apnea between the sexes. However, neither androgen blockade nor administration of estrogen or progesterone alleviated obstructive sleep apnea in men.36 Therefore, none of these factors appears to fully explain the lower prevalence of obstructive sleep apnea in women than men. The present results suggest that the greater fluid accumulation in the neck in association with a greater increase in NC in men than in women, along with a reduction in UA-XSA in men but not in women, could put men at greater risk than women for upper airway obstruction during sleep.
Central sleep apnea is more common in men than in women with heart failure.54 Heart failure patients with central sleep apnea usually hyperventilate and their PCO2 is close to the apnea threshold. Therefore, slight augmentations in ventilation can lower PCO2 below the apnea threshold and trigger central apneas. We found that in both men and women, TFV increased exponentially over time. However, after 90 min, men accumulated more fluid in the thorax than women. In heart failure patients, increases in TFV could increase left ventricular filling pressure, and induce pulmonary edema that could, in turn, stimulate pulmonary vagal irritant receptors provoking hyperventilation thus predisposing to central sleep apnea.9,24,46 Hence, greater increases in TFV in men than in women over time could be one reason why men with heart failure are at greater risk for central sleep apnea than women. This possibility should be investigated in future studies.
Smaller increases in TFV and NFV in women than in men could be partially due to a larger amount of fluid sequestration in the abdomen in women. Our results show that while AFV did not increase in men after 90 min, it increased significantly in women. Gonadal veins of women are substantially larger than those of men, and women have a large venous plexus around the uterus absent in men with multiple connections between the pelvic and leg venous systems. Such anatomical venous capacitance in women could have contributed to the lower amount of fluid shifting from the legs to the thorax and neck than in men that we observed. Nevertheless, the differences between the sexes were quite small.
The pattern of fluid redistribution in the abdomen was different from those of the other segments. In women and in younger men the abdomen acted as a fluid reservoir. However in older men (aged 50.2 ± 7.7 years), AFV decreased continuously over time so that it acted more like a conduit for fluid movement from the legs to more superior segments than a reservoir. There were no differences in the amount of fluid accumulating in the thorax or neck after 90 min in participants with different patterns of abdominal fluid accumulation. Therefore, the amount of fluid accumulating in the abdomen could not account for the differing amount of fluid that accumulates in the thorax or neck.
We found that variations in LFV, TFV, and NFV could be modeled as first order dynamic systems, with exponential changes over time. The exponential models (time constants of 70–90 min when considering all participants) imply rapid initial changes in fluid redistribution followed by slower changes over time. Based on these models, after the first and second hours of recumbent position, more than 60 and 80% of fluid would be redistributed out of legs into the thorax and neck. Recently, Jafari et al. showed that in 65 patients there was no change in sleep apnea severity from the first 2 h to the last 2 h of sleep.16 They concluded that because there was no increase in sleep apnea severity, as assessed by the number of apnea and hypopneas per hour of sleep, between the first and last 2 h of sleep, fluid redistribution into the neck could not be playing a role in sleep apnea severity. However, since they did not measure fluid volumes of either leg or neck they could not make assumptions about degree and timing of overnight fluid movement. Also, they assumed a linear change in fluid volumes over time. Based on our model, the change in NFV in the first and last 2 h of sleep (for all participants) would be 17.4 ± 4.6 and 1.1 ± 2.0 ml (p < 0.001). Therefore, since the increase in NFV in the last 2 h of sleep compared to the first 2 h of sleep is negligible, one would not expect a change in sleep apnea severity from the beginning to the end of sleep in association to rostral fluid shift. In addition, two studies demonstrated that compression stockings reduced sleep apnea severity in association with reductions in overnight fluid shift out of the legs and attenuation of the overnight increase in neck circumference. Those data demonstrate that rostral fluid shift does play a role in the pathogenesis of obstructive sleep apnea.32,33
Our study is subject to some limitations. First, currently there is no device that measures both intra- and extra-cellular fluid volumes in various body segments simultaneously and continuously. The system that we used is based on single frequency measurements of bioelectrical impedance which can measure extracellular fluid. We validated our system against a commercially available device that uses multi-frequency bioimpedance analysis to measure leg fluid volume (Xitron 4200, Hydra ECF/ICF, Xitron Technologies Inc., San Diego, CA).39,50 We found that extracellular leg fluid volumes measured by our system correlated strongly with the extracellular fluid volume measure by the other device. Further work will be needed to develop devices using multi-frequency bioimpedance analysis to measure both intra- and extra-cellular fluid volumes of various body segments simultaneously and continuously.
The other limitation of making continuous real-time measurements of bioelectrical impedance is its sensitivity to motion artifact. To overcome this problem, we restricted participants from moving during the study to assure stability and validity of the impedance recordings. Accordingly, the recording period was limited to 90 min because we found, in preliminary studies, that most participants became very uncomfortable and could not remain immobile beyond this time. For the same reason, we could not investigate the influence of recumbent body positions other than supine, or the effects of sleep on the fluid redistribution patterns, since during sleep, participants will move from time to time. Future studies should investigate whether the pattern and time-course of rostral fluid shift differs between sleep and wakefulness. We also did not measure the hematocrit levels in every individual to estimate blood resistivity (ρ); but we used the previously estimated values for extracellular resistivity (ρ = 47 Ω cm for both sexes).6 However since sex could affect ρ, we repeated the measurements of fluid volume assuming different resistivity for men (ρ = 40.3 Ω cm) and women (ρ = 42.3 Ω cm).11,50 However, taking into account these potential differences in resistivity between men and women did not alter the differences between them based on our original analysis in which we assumed the same resistivity for both sexes: after 90 min, ΔLFV was similar between sexes (p = 0.210), there was a trend for larger ΔAFV in women (p = 0.067), and men accumulated more fluid in their thorax and neck than women (TFV: p = 0.024, NFV: p = 0.037).
Since urine volume could affect the measurement of AFV, we asked subjects not to drink energy drinks and caffeine on the day of experiments, and all subjects voided before starting the experiments. It is nevertheless possible that bladder volume might have had a small effect on our AFV measurements.
The main objectives of our study were to investigate the feasibility of bioelectrical impedance to measure neck fluid volume, to examine the dynamics of rostral fluid shift, and to investigate whether men and women have different patterns of rostral fluid shift due to anatomical differences in their abdomen. For feasibility purposes and to control for other factors that could affect the measurement, we limited our studies to awake subjects and those with no diagnosed history of sleep apnea. Based on these findings that even in awake healthy subjects, sex plays an important role on the amount of fluid accumulating in the chest and neck, future studies should investigate the potential roles of different patterns of segmental fluid accumulation on the severity of obstructive and central sleep apnea in men and women.
In conclusion, we found that for a similar amount of fluid moving out of the legs, men accumulate more fluid in their thorax and neck in association with a bigger increase in NC than women. In men, unlike women, this increase in neck circumference was accompanied by narrowing of the upper airway. The present findings along with those of our previous studies,25,50 suggest that differences in patterns of recumbent fluid redistribution may contribute to the higher prevalences of obstructive and central sleep apnea in men than in women. Further interventional studies will be required to determine whether fluid accumulation in the thorax and neck affects the pathophysiology of sleep apnea and whether prevention of fluid movement out of the legs and into the thorax and neck may have a greater effect on sleep apnea severity in men than in women.
Abbreviations
- AFV:
-
Abdominal fluid volume
- ANCOVA:
-
Analysis of covariance
- BMI:
-
Body mass index
- LFV:
-
Leg fluid volume
- NC:
-
Neck circumference
- NFV:
-
Neck fluid volume
- TFV:
-
Thoracic fluid volume
- UA-XSA:
-
Upper airway cross-sectional area
References
Avasthey, P., and E. H. Wood. Intrathoracic and venous pressure relationships during responses to changes in body position. J. Appl. Physiol. 37:166–175, 1974.
Baccelli, G., P. Pacenti, S. Terrani, M. Checchini, G. Riglietti, F. Prestipino, E. Omboni, F. Sardella, M. Catalano, and Z. Malacarne. Scintigraphic recording of blood volume shifts. J. Nucl. Med. 36:2022–2031, 1995.
Berg, H. E., B. Tedner, and P. A. Tesch. Changes in lower limb muscle cross-sectional area and tissue fluid volume after transition from standing to supine. Acta Physiol. Scand. 148:379–385, 1993.
Bracco, D., D. Thiebaud, R. L. Chiolero, M. Landry, P. Burckhardt, and Y. Schutz. Segmental body composition assessed by bioelectrical impedance analysis and DEXA in humans. J. Appl. Physiol. (1985) 81:2580–2587, 1996.
Chiu, K. L., C. M. Ryan, S. Shiota, P. Ruttanaumpawan, M. Arzt, J. S. Haight, C. T. Chan, J. S. Floras, and T. D. Bradley. Fluid shift by lower body positive pressure increases pharyngeal resistance in healthy subjects. Am. J. Respir. Crit. Care Med. 174:1378–1383, 2006.
De Lorenzo, A., A. Andreoli, J. Matthie, and P. Withers. Predicting body cell mass with bioimpedance by using theoretical methods: a technological review. J. Appl. Physiol. (1985) 82:1542–1558, 1997.
Dempsey, J. A., S. C. Veasey, B. J. Morgan, and C. P. O’Donnell. Pathophysiology of sleep apnea. Physiol. Rev. 90:47–112, 2010.
Demura, S., S. Sato, and T. Kitabayashi. Percentage of total body fat as estimated by three automatic bioelectrical impedance analyzers. J. Physiol. Anthropol. Appl. Hum. Sci. 23:93–99, 2004.
Drazner, M. H., A. Prasad, C. Ayers, D. W. Markham, J. Hastings, P. S. Bhella, S. Shibata, and B. D. Levine. The relationship of right- and left-sided filling pressures in patients with heart failure and a preserved ejection fraction. Circ. Heart Fail 3:202–206, 2010.
Fawcett, J. K., and V. Wynn. Effects of posture on plasma volume and some blood constituents. J. Clin. Pathol. 13:304–310, 1960.
Fenech, M., and M. Y. Jaffrin. Extracellular and intracellular volume variations during postural change measured by segmental and wrist-ankle bioimpedance spectroscopy. IEEE Trans. Biomed. Eng. 51:166–175, 2004.
Fredberg, J. J., M. E. Wohl, G. M. Glass, and H. L. Dorkin. Airway area by acoustic reflections measured at the mouth. J. Appl. Physiol. 48:749–758, 1980.
Friedman, O., T. D. Bradley, C. T. Chan, R. Parkes, and A. G. Logan. Relationship between overnight rostral fluid shift and obstructive sleep apnea in drug-resistant hypertension. Hypertension 56:1077–1082, 2010.
Friedman, O., T. D. Bradley, and A. G. Logan. Influence of lower body positive pressure on upper airway cross-sectional area in drug-resistant hypertension. Hypertension 61:240–245, 2013.
Hildebrandt, W., H. C. Gunga, J. Herrmann, L. Rocker, K. Kirsch, and J. Stegemann. Enhanced slow caudad fluid shifts in orthostatic intolerance after 24-h bed-rest. Eur. J. Appl. Physiol. Occup. Physiol. 69:61–70, 1994.
Jafari, B., and V. Mohsenin. Overnight rostral fluid shift in obstructive sleep apnea: does it affect the severity of sleep-disordered breathing? Chest 140:991–997, 2011.
Jaffrin, M. Y., and H. Morel. Body fluid volumes measurements by impedance: a review of bioimpedance spectroscopy (BIS) and bioimpedance analysis (BIA) methods. Med. Eng. Phys. 30:1257–1269, 2008.
Kachlik, D., V. Pechacek, V. Musil, and V. Baca. The venous system of the pelvis: new nomenclature. Phlebology 25:162–173, 2010.
Kasai, T., J. S. Floras, and T. D. Bradley. Sleep apnea and cardiovascular disease: a bidirectional relationship. Circulation 126:1495–1510, 2012.
Kasai, T., S. S. Motwani, D. Yumino, J. M. Gabriel, L. T. Montemurro, V. Amirthalingam, J. S. Floras, and T. D. Bradley. Contrasting effects of lower body positive pressure on upper airways resistance and partial pressure of carbon dioxide in men with heart failure and obstructive or central sleep apnea. J. Am. Coll. Cardiol. 61:1157–1166, 2013.
Kasai, T., S. S. Motwani, D. Yumino, S. Mak, G. E. Newton, and T. D. Bradley. Differing relationship of nocturnal fluid shifts to sleep apnea in men and women with heart failure. Circ. Heart Fail. 5:467–474, 2012.
Krogh, A., E. M. Landis, and A. H. Turner. The movement of fluid through the human capillary wall in relation to venous pressure and to the colloid osmotic pressure of the blood. J. Clin. Invest. 11:63–95, 1932.
Kyle U. G., I. Bosaeus, A. D. De Lorenzo, P. Deurenberg, M. Elia, J. M. Gomez, B. L. Heitmann, L. Kent-Smith, J. C. Melchior, M. Pirlich, H. Scharfetter, A. M. Schols, C. Pichard and E. W. G. Composition of the. Bioelectrical impedance analysis–part I: review of principles and methods. Clin. Nutr. 23:1226–1243, 2004.
Larsen, F., L. Mogensen, and B. Tedner. Influence of furosemide and body posture on transthoracic electrical impedance in AMI. Chest 90:733–737, 1986.
Levick, J. R., and C. C. Michel. The effects of position and skin temperature on the capillary pressures in the fingers and toes. J. Physiol. 274:97–109, 1978.
Ling, C. H., A. J. de Craen, P. E. Slagboom, D. A. Gunn, M. P. Stokkel, R. G. Westendorp, and A. B. Maier. Accuracy of direct segmental multi-frequency bioimpedance analysis in the assessment of total body and segmental body composition in middle-aged adult population. Clin. Nutr. 30:610–615, 2011.
Malhotra, A., Y. Huang, R. B. Fogel, G. Pillar, J. K. Edwards, R. Kikinis, S. H. Loring, and D. P. White. The male predisposition to pharyngeal collapse: importance of airway length. Am. J. Respir. Crit. Care Med. 166:1388–1395, 2002.
Marin, J. M., S. J. Carrizo, E. Vicente, and A. G. Agusti. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365:1046–1053, 2005.
Mohapatra, S. N., and D. W. Hill. The changes in blood resistivity with haematocrit and temperature. Eur. J. Intensive Care Med. 1:153–162, 1975.
Mohsenin, V. Gender differences in the expression of sleep-disordered breathing : role of upper airway dimensions. Chest 120:1442–1447, 2001.
Punjabi, N. M., B. S. Caffo, J. L. Goodwin, D. J. Gottlieb, A. B. Newman, G. T. O’Connor, D. M. Rapoport, S. Redline, H. E. Resnick, J. A. Robbins, E. Shahar, M. L. Unruh, and J. M. Samet. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 6:e1000132, 2009.
Redolfi, S., I. Arnulf, M. Pottier, T. D. Bradley, and T. Similowski. Effects of venous compression of the legs on overnight rostral fluid shift and obstructive sleep apnea. Respir. Physiol. Neurobiol. 175:390–393, 2011.
Redolfi, S., I. Arnulf, M. Pottier, J. Lajou, I. Koskas, T. D. Bradley, and T. Similowski. Attenuation of obstructive sleep apnea by compression stockings in subjects with venous insufficiency. Am. J. Respir. Crit. Care Med. 184:1062–1066, 2011.
Redolfi, S., D. Yumino, P. Ruttanaumpawan, B. Yau, M. C. Su, J. Lam, and T. D. Bradley. Relationship between overnight rostral fluid shift and Obstructive Sleep Apnea in nonobese men. Am. J. Respir. Crit. Care Med. 179:241–246, 2009.
Rowley, J. A., X. Zhou, I. Vergine, M. A. Shkoukani, and M. S. Badr. Influence of gender on upper airway mechanics: upper airway resistance and Pcrit. J. Appl. Physiol. 91(2248–2254):2001, 1985.
Ryan, C. M., and T. D. Bradley. Pathogenesis of obstructive sleep apnea. J. Appl. Physiol. 99:2440–2450, 2005.
Shepard, Jr, J. W., D. A. Pevernagie, A. W. Stanson, B. K. Daniels, and P. F. Sheedy. Effects of changes in central venous pressure on upper airway size in patients with obstructive sleep apnea. Am. J. Respir Crit. Care. Med. 153:250–254, 1996.
Shiota, S., C. M. Ryan, K. L. Chiu, P. Ruttanaumpawan, J. Haight, M. Arzt, J. S. Floras, C. Chan, and T. D. Bradley. Alterations in upper airway cross-sectional area in response to lower body positive pressure in healthy subjects. Thorax 62:868–872, 2007.
Singh B., A. Yadollahi, O. D. Lyons, H. Alshaer and T. D. Bradley. Measurement of leg fluid volume using bioelectrical impedance [abstract]. In: American Physiology Society Experimental Biology Conference. San Diego, CA, pp. 1156–1114, 2014.
Starling, E. H. On the absorption of fluids from the connective tissue spaces. J. Physiol. 19:312–326, 1896.
Su, M. C., K. L. Chiu, P. Ruttanaumpawan, S. Shiota, D. Yumino, S. Redolfi, J. S. Haight, and T. D. Bradley. Lower body positive pressure increases upper airway collapsibility in healthy subjects. Respir. Physiol. Neurobiol. 161:306–312, 2008.
Su, M. C., K. L. Chiu, P. Ruttanaumpawan, S. Shiota, D. Yumino, S. Redolfi, J. S. Haight, B. Yau, J. Lam, and T. D. Bradley. Difference in upper airway collapsibility during wakefulness between men and women in response to lower-body positive pressure. Clin. Sci. (Lond.) 116:713–720, 2009.
Tagliabue, A., A. Andreoli, M. Comelli, S. Bertoli, G. Testolin, G. Oriani, and A. De Lorenzo. Prediction of lean body mass from multifrequency segmental impedance: influence of adiposity. Acta Diabetol. 38:93–97, 2001.
Terada, N., and T. Takeuchi. Postural changes in venous pressure gradients in anesthetized monkeys. Am. J. Physiol. 264:H21–H25, 1993.
Thompson, W. O., P. K. Thompson, and M. E. Dailey. The effect of posture upon the composition and volume of the blood in man. J. Clin. Invest. 5:573–604, 1928.
van Lieshout, J. J., M. P. Harms, F. Pott, M. Jenstrup, and N. H. Secher. Stroke volume of the heart and thoracic fluid content during head-up and head-down tilt in humans. Acta Anaesthesiol. Scand. 49:1287–1292, 2005.
Waterfield, R. L. The effect of posture on the volume of the leg. J. Physiol. 72:121–131, 1931.
Waterfield, R. L. The effects of posture on the circulating blood volume. J. Physiol. 72:110–120, 1931.
White, L. H., and T. D. Bradley. Role of nocturnal rostral fluid shift in the pathogenesis of obstructive and central sleep apnoea. J. Physiol. 591:1179–1193, 2013.
XITRON. HYDRA ECF/ICF (Model 4200), Bio-impedance spectrum analyzer, for measuring intracellular and extracellular fluid volumes. Operating manual San Diego, CA, USA: XITRON Technologies Inc, 2007.
Youmans, J. B., H. S. Wells, D. Donley, D. G. Miller, and H. Frank. The effect of posture (standing) on the serum protein concentration and colloid osmotic pressure of blood from the foot in relation to the formation of edema. J. Clin. Invest. 13:447–459, 1934.
Young, T., M. Palta, J. Dempsey, J. Skatrud, S. Weber, and S. Badr. The occurrence of sleep-disordered breathing among middle-aged adults. N. Engl. J. Med. 328:1230–1235, 1993.
Yumino, D., S. Redolfi, P. Ruttanaumpawan, M. C. Su, S. Smith, G. E. Newton, S. Mak, and T. D. Bradley. Nocturnal rostral fluid shift: a unifying concept for the pathogenesis of obstructive and central sleep apnea in men with heart failure. Circulation 121:1598–1605, 2010.
Yumino, D., H. Wang, J. S. Floras, G. E. Newton, S. Mak, P. Ruttanaumpawan, J. D. Parker, and T. D. Bradley. Prevalence and physiological predictors of sleep apnea in patients with heart failure and systolic dysfunction. J. Card. Fail. 15:279–285, 2009.
Zhu, F., M. K. Kuhlmann, P. Kotanko, E. Seibert, E. F. Leonard, and N. W. Levin. A method for the estimation of hydration state during hemodialysis using a calf bioimpedance technique. Physiol. Meas. 29:S503–S516, 2008.
Zhu, F., D. Schneditz, E. Wang, and N. W. Levin. Dynamics of segmental extracellular volumes during changes in body position by bioimpedance analysis. J. Appl. Physiol. 85(497–504):1998, 1985.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Zahra Moussavi oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Yadollahi, A., Singh, B. & Bradley, T.D. Investigating the Dynamics of Supine Fluid Redistribution Within Multiple Body Segments Between Men and Women. Ann Biomed Eng 43, 2131–2142 (2015). https://doi.org/10.1007/s10439-015-1264-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-015-1264-0