Abstract
The ability to measure and quantify the properties of skeletal muscle in vivo as a method for understanding its complex physiological and pathophysiological behavior is important in numerous clinical settings, including rehabilitation. However, this remains a challenge to date due to the lack of a “gold standard” technique. Instead, there are a myriad of measuring techniques each with its own set of pros and cons. This review discusses the current state-of-the-art in elastography imaging techniques, i.e., ultrasound and magnetic resonance elastography, as applied to skeletal muscle, and briefly reviews other methods of measuring muscle mechanical behavior in vivo. While in vivo muscle viscoelastic properties can be measured, these techniques are largely limited to static or quasistatic measurements. Emerging elastography techniques are able to quantify muscle anisotropy and large deformation effects on stiffness, but, validation and optimization of these newer techniques is required. The development of reliable values for the mechanical properties of muscle across the population using these techniques are required to enable them to become more useful in rehabilitation and other clinical settings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Skeletal muscles are the major actuator in the human body, and abnormal muscle mechanical function can both cause muscle disorders (e.g., disuse causes muscle atrophy) and arise as a result of disease processes (e.g., contracture after stroke). Such abnormalities can impair musculoskeletal function, and they thus provide major challenges for rehabilitation engineers aiming to design assistive technologies.
Non-invasive measurements of muscle mechanical properties in human subjects could be very valuable to rehabilitation clinicians, as they could provide a quantitative assessment of muscle status that is directly related to physiological function and muscle structure. There is also clear potential for clinical use of in vivo muscle mechanical property measurements to assist with diagnosis of muscle disorders, and also in monitoring disease progression and treatment response.
Our understanding of the mechanical behavior of muscles has come a long way since researchers first began trying to quantify the force required to elongate passive muscle.7 It is now well recognized that skeletal muscles are mechanically anisotropic and nonlinearly viscoelastic.21,76,77 However, quantifying these complex mechanical properties in vivo remains an open challenge in biomechanics, with no single method providing a comprehensive characterization of muscle properties. While it is relatively straightforward to measure the overall mechanical behavior of muscle–tendon groups that cross easily manipulated joints by measuring torque–angle relationships during passive joint movements it is much more difficult to obtain measurements of the mechanical behavior of individual muscles, and to separate the behavior of tendons from the muscle bellies. In this paper, we review recent developments in measuring muscle properties in vivo, and lay out some of the remaining challenges. While we focus here on passive properties, active contraction properties are obviously also important, but elastography and other methods for characterizing these in vivo are currently less well established. We primarily discuss the properties of the muscle belly, which we will refer to as ‘muscle’, and where we refer to the properties of the muscle–tendon unit, this will be noted explicitly.
Passive Muscle Mechanical Properties
Passive muscle tissue, particularly skeletal muscle, is a hierarchically organized, anisotropic, nonlinearly viscoelastic soft tissue. Skeletal muscle is anisotropic due to its microstructural arrangement consisting of parallel fiber bundles. Skeletal muscle’s hierarchical structure can be visualized at different length scales (see Fig. 1). Each muscle is surrounded by a connective tissue layer called epimysium, which is continuous with tendons and attaches muscles to bones. Each muscle consists of a bundle of muscle fascicles. Each muscle fascicle is surrounded by perimysium and contains many myofibers surrounded by endomysium, which are in turn made up of numerous myofibrils.62 The myofibrils consist of actin, myosin and titin filaments in organized structures that move relative to each other during contraction.43 This hierarchical structure gives rise to some of muscle’s characteristic mechanical behavior, as different elements of the microstructure deform and interact under load to give rise to the complex overall mechanical response. Moreover, alterations in the structure of muscles, due to cell loss, fatty infiltration, and fibrosis in disease processes are reflected in the mechanical behavior of the tissue, as discussed below in the section on muscle disorders.
Hierarchical structure of skeletal muscle tissue (used with permission from OpenStax College58)
Muscles exhibit the typical nonlinear length–tension (or stress–strain) behavior of most soft biological tissues, whereby stiffness increases with applied stretch. Relaxation experiments show a broad spectrum of relaxation time constants (e.g., Kwon et al.71), likely indicating a range of different relaxation processes occurring within muscle tissue, perhaps related to its hierarchical structure, although this has not been proven.
Muscle has also been shown to be thixotropic,61 where the passive behavior of a muscle exhibits a yield stress during small amplitude deformations after contraction. The apparent increase in stiffness is reduced by large passive movements, although the mechanisms are not completely understood.
Methods for measuring muscle mechanical properties must therefore take into account the complex mechanical behavior of these tissues, particularly when comparing measurements made in different joint positions or muscle lengths, where the nonlinear behavior will strongly influence any measures that do not capture the full nonlinear behavior. This includes the vast majority of elastography measurements, which estimate properties from small deformation loading.
Elastography and Imaging-Based Methods for Measuring Muscle Mechanics
Elastography encompasses a group of techniques that estimate the mechanical properties of a tissue based on the relationship between mechanical properties and the propagation characteristics of mechanical vibration waves, typically in the acoustic frequency range (10–1000 Hz). The wave propagation is usually measured using some form of medical imaging (ultrasound and MRI are the most common), and the tissue modulus estimated from the wave equation (see Eq. 1).
where \(\vec{u}\) is the displacement vector, ρ is the density of the tissue, μ is the shear modulus, λ the second Lamé coefficient, \(\eta\) the shear viscosity and ξ is the viscosity of the compressional wave. The subscript t refers to the time derivative. Despite some concerns over the validity of this approach,68 a much simplified version is often used, that estimates local wave speed from the imaging data, and calculates the shear modulus from:
where ν is the frequency of the vibration and λ is the local wavelength. Development of robust inversion techniques to estimate the viscoelastic properties from elastography imaging data is an ongoing area of research, as this is an inherently ill-conditioned numerical problem. Poor quality datasets with low signal-to-noise ratio tend to provide unreliable tissue property estimates, with different biases depending on the inversion algorithms applied. While most studies use some form of direct numerical inversion, recent work is exploring the use of finite-element inversion techniques that have the potential to be more robust, e.g., Van Houten et al.75
The term elastography is also often applied to qualitative elastography, typically using ultrasound, where relative stiffness of different tissue regions is estimated from the effect of static mechanical compression on local tissue deformation.37
Ultrasound Methods
While not strictly an elastography technique, traditional B-mode ultrasonography has been used together with dynamometry measurements of joint torques to quantify the passive length–tension curves and strain in specific muscles32 and muscle groups in vivo but this method is limited in its field of view and can only image superficial muscles.35 Cross-correlation techniques can be used on the image sequences to quantify fascicle strains, which are combined with muscle length–tension data to estimate fascicle length–tension curves.32 This has a key advantage that it gives large-deformation information about the muscle fascicles, and thus can detect differences in muscle properties in clinical groups where the nonlinear mechanical behavior is altered.38 The reliability of this method was found to be good for same-day measurements within the same subject but measurements taken more than 1 week apart could not be reliably reproduced possibly due to misalignment of the ankle and knee joint axes with the axes of the apparatus.32
The most common ultrasound elastography technique, strain elastography (or compression elastography), relies on manually deforming a tissue with the ultrasound transducer, and inferring the stiffness of the tissue from the deformation observed in the ultrasound images.18 Localized stiff regions deform less than softer tissue regions. The local deformation can be used to construct a map of apparent tissue stiffness. A map of “Young’s modulus” is sometimes constructed by assuming that the transducer applies a uniform stress to the imaged tissue, and that the modulus is therefore proportional to the local tissue strain. This technique is most useful for providing qualitative information about variation in stiffness of tissue within the imaging field of view, as the assumptions used for estimating tissue moduli are difficult to support, because the deformation of a tissue varies with depth, the stress induced by manual compression of tissue with an ultrasound transducer is not uniform, and the nonlinear mechanical properties of tissues mean that the modulus cannot be estimated simply from the observed deformation. Moreover, it assumes that all tissues in the imaging field of view are loaded in series by the transducer, and if they are loaded in parallel, then the assumption of the stress being uniform is invalid. Instead, the strain is more likely to be uniform, and the stress will vary with the modulus, so that different stiffnesses will not be detected by a variation in strain. Repeatability and operator-dependent measurements are also significant challenges for this technique. Nonetheless, this technique has been used to study muscle mechanical behavior in both healthy volunteers and patient populations.6,17,55,78 It is currently unable to provide information on muscle anisotropy.
An extension of ultrasound strain elastography is acoustic radiation force impulse (ARFI) elastography.54 Instead of manually compressing the tissue, ARFI creates a focused ultrasound pulse that travels through the tissue. Using rapid imaging ultrasound pulse echoes, the tissue deformation can be tracked, and analyzed to provide a qualitative stiffness map. Its main advantage over strain elastography is that it is not limited to superficial tissues that can be manually deformed,20 although it is still limited by ultrasound penetration depths.
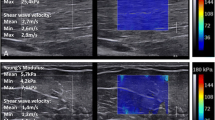
More recently, efforts to provide quantitative mechanical property data from ultrasound elastography led to the development of shear wave elastography, which relies on similar physical principles to MR elastography (see below), where propagation of an externally imposed acoustic wave is tracked, and used to estimate the tissue shear modulus. This stimulus can be generated by ARFI, and its propagation imaged with high frame rate ultrasound, as in the supersonic elastography technique.67 An example of this technique applied to lower limb muscles is shown in Fig. 2. This system can provide elastograms at a frame rate of approximately 1 Hz, and is therefore suitable for studies of quasistatic muscle processes, such as slow or sustained contractions.57 Measurements in muscle vary with transducer orientation with respect to the muscle fascicles, and anisotropic measurements are typically not available. It has only moderate repeatability and reliability in muscle applications.81
Supersonic shear wave ultrasound elastography of the muscles of the lower leg during standing. The colored region shows the calculated shear modulus, superimposed on a B-mode image. Localized stiffnesses can be calculated (small circles, α, β). (a, b) Tibialis anterior at rest and during contraction, respectively. (c, d) Medial gastrocnemius and soleus at rest and during contraction, respectively, with knee extended. (e) Medial gastrocnemius and soleus during contraction with knee flexed. (f) Medial gastrocnemius and soleus during quiet standing (used with permission from Shinohara et al.67)
Transient elastography was originally developed to image liver fibrosis, and works by the same principle as shear wave elastography. However, only a single impulse vibration is delivered, and the shear modulus is estimated from the propagating and reflected ultrasound echoes.10,19 It has been used in a small number of muscle studies to provide an estimate of “muscle hardness”. One example is estimating muscle stiffness changes during passive stretching.56 It provides rapid results, but is essentially a one-dimensional technique, so is prone to bias as a result of device placement and angulation with respect to the muscle fascicles. Each measurement is acquired over 50–100 ms,66 so that, in principle, near real-time acquisition is possible, but in practice, a single dataset requires 8–10 repetitions to provide a reliable result, so that measurements require 8–10 min to perform.1 Reproducibility is limited,56 limiting its utility for robust measurements in both clinical and scientific rehabilitation settings.
Magnetic Resonance Elastography
The most common alternative to ultrasound elastography is Magnetic Resonance Elastography (MRE), which is a magnetic resonance imaging technique that works by measuring the shear wave propagation through soft tissues.53 The shear wave is generated by an MR-compatible mechanical transducer that is synchronized to the MR image acquisition. The displacement data are captured by using motion sensitive gradients in the imaging sequence. MRE can acquire displacement data throughout cyclic deformations in three orthogonal directions. The data can then be used to numerically solve the wave equations (Eqs. 1, 2) to provide estimates of the linear viscoelastic properties of tissues. Early studies focused on the elastic properties only, but more recent studies have also been able to estimate the viscous properties of soft tissues using this technique. The majority of MRE studies obtain data at a single vibration frequency, but there is increasing interest in obtaining more information by measuring the responses at multiple frequencies, e.g., Bensamoun et al.36 This can be done by repeating measurements at different frequencies, or by using an input vibration stimulus consisting of multiplexed single frequency inputs23 and using post-processing to extract the response at each of the component frequencies.
For applications in muscle mechanics, a few different approaches to generating the vibration have been used. One approach is to use a pneumatic driver secured around the muscle of interest.69 While this is easy to use and is reasonably free of transducer-associated imaging artefacts, there are two key limitations. The first is that to achieve good wave transmission into the tissue the transducer must be place firmly on the muscle, and this tends to deform the muscle locally, and can alter the local mechanical properties, due to muscle’s inherent nonlinearity. That is, as muscle is compressed, its stiffness increases. The second is that the pneumatic technique makes it more difficult to achieve tight control over the input waveform, making multi-frequency measurements substantially more difficult. An alternative approach is to use an electromechanical driver that creates vibration by coupling a coil carrying current synchronized to the imaging gradients to the primary (B0) field of the MRI. In studies of the lower limb in our group, we apply this technique, coupling the transducer to the tibia, which then transmits vibration into the muscles of the calf without compressing them.27,28 The primary disadvantages of this method are a more complex setup to ensure that any stray magnetic field from the transducer does not impinge on the area of interest, and the need to carefully control the electrical components for safety. This method is amenable to multi-frequency measurements. Other approaches place drivers outside the MRI fringe field and use mechanical linkages to connect to the subject.
Thus far, MRE has successfully been used to measure the shear modulus of a range of tissues in vivo, including muscle,5,24,27,28 breast,68,74 brain26,31,49 and liver,33,34 in both healthy and clinical populations.
Methods to measure anisotropy in soft tissues using MRE have been recently developed64 and applied to muscle tissue. Most of these methods assume transverse isotropy of the shear moduli to simplify parameter estimation (see Eq. 3). The earliest method used numerical optimization in the inversion process to identify symmetry axes, and solved a transversely isotropic version of the linear viscoelastic wave equation, to estimate the shear moduli parallel and perpendicular to the material symmetry axis (in this case, aligned with the z-coordinate axis).
\(\mu_{ \bot }\) and \(\mu_{//}\) are the elastic components of the shear modulus perpendicular and parallel to the axis of symmetry respectively. Other symbols are the same as in Eq. 1.
We have recently developed and validated a method that uses diffusion tensor imaging (DTI) to identify the tissue structural symmetry axis, and combined this with numerical solution of the anisotropic wave equation to estimate tissue anisotropy. The degree of mechanical anisotropy can be quantified by the ratio of the shear moduli parallel and perpendicular to the symmetry axis. We have applied this to healthy human calf muscles27 (See Fig. 3), and have demonstrated its potential utility in assessing muscle degenerative conditions (see “Muscle Degeneration” section).
Anisotropic lower limb muscle MRE measurements from Green et al.27 used with permission. (a) Wave image data, showing the three muscle regions of interest (tibialis anterior, TA; medial gastrocnemius, MG; and soleus, Sol) outlined in white dashed line. (b) Shear modulus perpendicular to the direction of the muscle fascicles as identified by diffusion tensor imaging. (c) Shear modulus parallel to the direction of the muscle fascicles as identified by diffusion tensor imaging
Sample MR image (upper row, a, d, g), shear wave image (middle row, b, e, h) and elastogram (bottom row, c, f, i) for the biceps muscle in a human volunteer. Right column (g, h, i) are from an arm that was immobilized for X. The left column (a, b, c) images are from the contralateral limb when the position of the arm was matched to the experimental limb after immobilization. The middle column (d, e, f) images are from the contralateral limb when the joint torque at the elbow was matched to the experimental limb. λ: wave length. Longer wavelengths indicate higher stiffness (depicted as warmer colors in elastograms in the bottom row). Note that the proximal (upper) part of the biceps muscle in the limb that had been immobilized is stiffer than the contralateral limb (used with permission from Muraki et al.52)
Another open challenge for elastography techniques, both ultrasound and MR-based, is that they are generally not able to measure large-deformation tissue mechanics, due to both the magnitude of the vibration stimulus (usually in the order of tens of microns) and the theory used to estimate the shear modulus. This is because elastography methods rely on the theory of wave propagation through a linear viscoelastic medium, and are thus limited to small deformation (linear viscoelastic regime). For most soft tissues this is ≪1% strain. However, new developments are beginning to address this challenge. For example, research is currently underway in our group to superimpose MRE measurements on static large deformations of lower limb muscles to estimate the large-deformation, anisotropic properties of human muscles in vivo. Tissue quasistatic deformations can be measured using a range of MRI techniques, including tagging methods.11,59,80 Proof of principle has been demonstrated in isotropic tissues.13
Non-elastographic Methods
In addition to ultrasound and magnetic resonance elastography, other techniques have been used to measure mechanical properties of muscles. For example, myotonometry estimates mechanical properties by applying an impulsive compressive load to the tissue, and measuring the resulting muscle tissue motion, which is a damped free oscillatory decay. The oscillation frequency and the decay constant are interpreted as reflecting elastic and viscous components of the muscle mechanical properties.73 A handheld device based on these concepts (the Myoton-3) has been shown to provide reliable measures of muscle ‘tone’ (stiffness arising from a combination of passive properties and muscle contraction) in controls and various patient groups.12,41 While it does not provide objective viscoelastic properties that could be used in modeling or rehabilitation engineering design applications, myotonometry has been used clinically for assessing spasticity and tissue compliance in patient groups with a range of neuromuscular disorders, e.g., Leonard et al.,42 Marusiak et al.,48 and Rydahl and Brouwer.65
Table 1 summarizes the key features of these different methods for measuring muscle mechanical properties in vivo.
Table 2 summarizes quantitative muscle properties obtained from studies of in vivo muscle mechanical properties, including in selected muscle disorders addressed in the following section.
In Vivo Muscle Measurements in Muscle Disorders
Many of the techniques outlined above have been used in preclinical or early clinical research, in both human patients and animal models of these disorders, with promising results. Changes in the mechanical properties of skeletal muscle have been found after exercise28 and in a wide range of metabolic and neuromuscular disorders such as spastic paraplegia, stroke and diabetes.3,25,30,50 Mechanical property changes could also be a useful indicator for the progression of a disease, such as in muscular dystrophies63 or pressure ulcers,45 thus providing useful information on supportive technologies and other treatments. Here, we review the applications of these techniques across a range of disorders affecting muscle tissues.
Muscle Degeneration
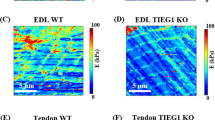
Degenerative muscle disorders cause changes in muscle structure, fatty infiltration, and atrophy.29,60,72 Current methods of tracking such changes in patients are somewhat limited, and typically clinical functional tests are used. However, early signs of disease progression are often missed by such tests. While it has long been thought that muscle degeneration is accompanied by mechanical changes,14 attempts to quantify these changes have only been successful more recently. Drakonaki and Allen,17 using strain elastography to examine the thigh muscles of a single Bethlem myopathy patient. They reported that affected areas of the muscle (based on traditional ultrasound and MRI images) were stiffer than surrounding healthy muscle tissue.17 More recently, Qin et al.,63 showed that mechanical anisotropy (the ratio of the shear modulus parallel and perpendicular to the muscle fiber axis, see above for details of the theory underpinning this method) is altered even in mildly affected muscles in a rodent model of muscular dystrophy, the mdx mouse.63 Moreover, this method was able to detect degeneration that was not apparent on anatomical or diffusion-weighted images, indicating that this has potential for tracking early disease progression. The mechanical anisotropy was correlated with muscle necrosis and reflected changes in the structural arrangement of muscle fascicles in the degenerating muscle. It remains to be seen whether the technique is equally useful in human muscular dystrophy patients.
Neuromuscular Disorders
Neurological disorders such as stroke, spinal cord injury and cerebral palsy often cause contractures (loss of passive joint range of motion). The mechanisms of contracture, which are a major source of disability for patients with neuromuscular disorders, are still not known.44 However, these muscle–tendon units appear stiff, and it has long been hypothesized that the shortened muscle–tendon unit length is accompanied by an increased stiffness in the muscle and/or tendons across the affected joint. Relatively few studies have quantified mechanical properties of the muscles in these conditions. However, using a combination of ultrasound and dynamometry, it has been shown that in stroke and spinal cord injury patients with contractures, the length of the gastrocnemius was reduced and the fascicular stiffness was increased in patients compared to controls across the range of motion.16,22,38 More specifically, the lower limb muscles of spinal cord injured patients with contractures have been studied using dynamometry combined with ultrasound imaging.15,16 Subjects who have had a limb immobilized also can develop contractures. Patients with contractures were shown to have substantially stiffer (~50%) gastrocnemius muscle–tendon units than control subjects. These changes were well established at 3 months after injury and did not change between 3 and 12 months.15 In cerebral palsy patients with contracture, similar methods demonstrated that increased joint stiffness was accompanied by a reduction in muscle fascicle elongation, indicating an increased stiffness in the muscle–tendon unit. One study of cerebral palsy patients using strain elastography and ARFI shear wave elastography found that both techniques indicated an increase in gastrocnemius stiffness in cerebral palsy patients with contracture compared to age matched healthy controls,40 however the leg positions were not reported, so it is not known whether there was any bias introduced by different muscle lengths (arising from the nonlinear muscle length–tension properties). Figure 5 shows some sample data from that study. The same research group has shown that Botulinum A toxin injection (used to treat spasticity in cerebral palsy patients) reduced muscle stiffness39 in one patient, although other studies have seen no change in stiffness using passive ankle flexion measurements over 10° of ankle dorsiflexion.2 Muraki et al.52 showed in an experimental study of dog forelimb immobilization that the biceps muscle is stiffer after 6 weeks of immobilization, using MR elastography (See Fig. 4). There is clearly additional research needed to determine the best protocols and methods for tracking the full range of nonlinear muscle property changes in neuromuscular disorders such as these.
Sample B-mode ultrasound images (left column, a, c) and shear wave elastography images (right column, b, d) from the lower leg of a child with spastic cerebral palsy (upper row, a, b) and a healthy control (lower row, c, d). MG, medial gastrocnemius; Sol, soleus muscle. In the elastograms, the warmer colors indicate stiffer tissue (HD), and the cooler colors (blue and purple) indicate softer tissue (SF). Note that the medial gastrocnemius in the cerebral palsy patient appears stiffer (warmer colors) than in the healthy control subject. Adapted from Kwon et al.40 used with permission
Metabolic and Other Systemic Disorders
Muscle mechanics can also be affected by metabolic and other systemic disorders. Hyperthyroid patients are thought to have weak muscles. One MRE study found that patients prior to treatment had significantly less stiff thigh muscles than healthy controls.4 The stiffness returned to normal after treatment for the thyroid condition.
Obstructive sleep apnoea (OSA) is a common respiratory condition associated with increased collapsibility of the upper airway during sleep. Repeated airway collapses result in regular arousals, daytime sleepiness leading to increased risk of accidents, and cardiovascular sequelae. The mechanical behavior of the upper airway muscles, particularly the tongue and airway lateral wall dilator muscles, is thought to contribute to the increased risk of airway collapse, especially in obese individuals. Veldi et al.79 used myotonometry to estimate tongue stiffness, and showed that despite reports of increased muscle activity in the tongue during wakefulness,51 the tongues of OSA patients were less stiff than healthy control subjects. More recently, Brown et al.,9 using MRE, reported that OSA patients have tongues that had an approximately 10% lower shear modulus than age and BMI matched healthy controls. Moreover, by using anisotropic analysis of the MRE data, they showed that the change in stiffness occurred in the direction of the muscle fascicles in the genioglossus. These studies suggest that there is potential for non-invasive measurements of muscle mechanical properties to provide insight into other disease processes affecting muscles.
Injury
Increased muscle stiffness is often reported after eccentric exercise, as part of the “Delayed Onset Muscle Soreness” syndrome. This has been studied in vivo using MRE by Green et al.,28 who showed that 48 h after a bout of eccentric exercise induced by walking backwards on a treadmill, the calf muscles of human volunteers had a shear modulus that was an average of 21% higher than that pre-exercise. The shear modulus returned to pre-exercise levels by 7 days after exercise.
Muscle crush injury has been studied using supersonic shear imaging46 over the first 72 h after injury in a rabbit model. The injured muscle region was significantly stiffer than the surrounding uninjured tissue at all time points. The technique was able to distinguish between injured and uninjured regions, with an area under the receiver-operator curve of >0.9 up to 2 h after injury.
Future Directions
To date, in vivo muscle mechanical measurements have been primarily part of preclinical evaluation studies in small study groups. Only a small number of studies have examined reliability and reproducibility of the methods, and few studies have been replicated in larger and/or independent populations. Moreover, the utility of these measures in making clinical decisions for an individual patient, including for assessment of rehabilitation strategies and treatment response, requires quantification of the sensitivity and specificity of the measures. Such studies are essential before such measures can be deployed routinely in the clinic. Moreover, many of the techniques described in this review are currently implemented in research settings only, and equipment and techniques need further refinement for practical clinical workflows. However, some of the existing data are likely to be useful for rehabilitation engineers by giving some indication of the likely changes in muscle mechanics in patients with a range of muscle disorders.
There are also several areas where technical improvements in the methods would be beneficial. This includes improved temporal resolution of many elastography techniques, in order to open up the possibility of dynamic (or even real time) quantitative elastography. MR elastography datasets typically require a few minutes to collect, and even in shear wave elastography, the temporal resolution is of the order of seconds, limiting the capacity to study dynamic processes, or to capture the nonlinear behavior of a muscle across its full length range. This is particularly relevant for muscles that undergo cyclic contraction, such as cardiac and respiratory muscles. Spatial resolution improvements might also allow more localized measurements of mechanical properties. Currently, MR elastography in particular is limited to providing regional data, due to a trade-off between better wave penetration (low frequencies) and spatial discrimination (at higher frequencies). While average muscle properties, and even regions of focal damage of the order of centimeters can be detected, smaller lesions and gradations in mechanical properties associated with focal loading are currently not reliably detected, or require long scan times. The ability to measure large deformation properties is also currently limited. While dynamometry-based methods can characterize the whole length–tension curve of some muscle groups (e.g., Hoang et al.,32 Kwon et al.70), most elastography measurements are conducted at a single muscle length and reflect the local shear modulus at that particular muscle length. Although there is promising research using multiple elastography measurements to estimate the shear modulus in muscles across a range of muscle lengths,47 this requires further development to properly characterize the anisotropic nonlinear viscoelastic properties in a robust and repeatable manner.
Significant challenges exist for studying active muscle tissue also, including how to characterize the combined effects of muscle contraction and nonlinear elasticity, both of which increase the apparent stiffness of muscles. In neuromuscular disorders, where muscle structural changes such as contracture may be accompanied by spasticity, this is particularly important. Applications to heart muscle are similarly challenging.
Conclusions
In vivo methods for measuring muscle mechanical properties are developing rapidly, but there are still significant challenges to overcome for these techniques to become easy, fast, accessible and affordable in the clinical setting. However, these techniques clearly have the potential to be useful in the context of rehabilitation engineering, opening up the possibility of making patient-specific measures of muscle mechanics and function to assist in tailoring rehabilitation equipment, and also for monitoring treatment.
References
Afdhal, N. H. Fibroscan (transient elastography) for the measurement of liver fibrosis. Gastroenterol. Hepatol. 8:605–607, 2012.
Alhusaini, A. A. A., J. Crosbie, R. B. Shepherd, C. M. Dean, and A. Scheinberg. No change in calf muscle passive stiffness after botulinum toxin injection in children with cerebral palsy. Dev. Med. Child Neurol. 53:553–558, 2011.
Basford, J. R., T. R. Jenkyn, K. N. An, R. L. Ehman, G. Heers, and K. R. Kaufman. Evaluation of healthy and diseased muscle with magnetic resonance elastography. Arch. Phys. Med. Rehabil. 83:1530–1536, 2002.
Bensamoun, S. F., S. I. Ringleb, Q. S. Chen, R. L. Ehman, K. N. An, and M. Brennan. Thigh muscle stiffness assessed with magnetic resonance elastography in hyperthyroid patients before and after medical treatment. J. Magn. Reson. Imaging 26:708–713, 2007.
Bensamoun, S. F., S. I. Ringleb, L. Littrell, Q. Chen, M. Brennan, R. L. Ehman, and K. N. An. Determination of thigh muscle stiffness using magnetic resonance elastography. J. Magn. Reson. Imaging 23:242–247, 2006.
Botar-Jid, C., L. Damian, S. M. Dudea, D. Vasilescu, S. Rednic, and R. Badea. The contribution of ultrasonography and sonoelastography in assessment of myositis. Med. Ultrason. 12:120–126, 2010.
Brodie, T. G. The extensibility of muscle. J. Anat. Physiol. 29:367, 1895.
Brown, E. C., S. Cheng, D. K. McKenzie, J. E. Butler, S. C. Gandevia, and L. E. Bilston. Respiratory movement of upper airway tissue in obstructive sleep apnea. Sleep 36:1069–1076, 2013.
Brown, E. C., S. Cheng, D. K. McKenzie, J. E. Butler, S. C. Gandevia, and L. E. Bilston. Tongue stiffness is lower in patients with obstructive sleep apnea during wakefulness compared with matched control subjects. Sleep 2014. (in press).
Castéra, L., J. Vergniol, J. Foucher, B. Le Bail, E. Chanteloup, M. Haaser, et al. Prospective comparison of transient elastography, fibrotest, apri, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology 128:343–350, 2005.
Cheng, S., J. E. Butler, S. C. Gandevia, and L. E. Bilston. Movement of the tongue during normal breathing in awake healthy humans. J. Physiol. 586:4283–4294, 2008.
Chuang, L.-L., C.-Y. Wu, and K.-C. Lin. Reliability, validity, and responsiveness of myotonometric measurement of muscle tone, elasticity, and stiffness in patients with stroke. Arch. Phys. Med. Rehabil. 93:532–540, 2012.
Clarke, E. C., S. Cheng, M. Green, R. Sinkus, and L. E. Bilston. Using static preload with magnetic resonance elastography to estimate large strain viscoelastic properties of bovine liver. J. Biomech. 44:2461–2465, 2011.
Dalkilic, I., and L. M. Kunkel. Muscular dystrophies: genes to pathogenesis. Curr. Opin. Genet. Dev. 13:231–238, 2003.
Diong, J., L. A. Harvey, L. K. Kwah, J. L. Clarke, L. E. Bilston, S. C. Gandevia, and R. D. Herbert. Gastrocnemius muscle contracture after spinal cord injury: a longitudinal study. Am. J. Phys. Med. Rehabil. 92:565–574, 2013.
Diong, J. H., R. D. Herbert, L. A. Harvey, L. K. Kwah, J. L. Clarke, P. D. Hoang, et al. Passive mechanical properties of the gastrocnemius after spinal cord injury. Muscle Nerve 46:237–245, 2012.
Drakonaki, E. E., and G. M. Allen. Magnetic resonance imaging, ultrasound and real-time ultrasound elastography of the thigh muscles in congenital muscle dystrophy. Skeletal Radiol. 39:391–396, 2010.
Drakonaki, E., G. Allen, and D. Wilson. Ultrasound elastography for musculoskeletal applications. Br. J. Radiol. 85:1435–1445, 2012.
Friedrich-Rust, M., M. F. Ong, S. Martens, C. Sarrazin, J. Bojunga, S. Zeuzem, and E. Herrmann. Performance of transient elastography for the staging of liver fibrosis: a meta-analysis. Gastroenterology 134(960–974):e968, 2008.
Friedrich-Rust, M., K. Wunder, S. Kriener, F. Sotoudeh, S. Richter, J. Bojunga, et al. Liver fibrosis in viral hepatitis: noninvasive assessment with acoustic radiation force impulse imaging vs. transient elastography 1. Radiology 252:595–604, 2009.
Fung, Y. C. Biomechanics: Mechanical Properties of Living Tissues. New York: Springer, 1993.
Gao, F., T. H. Grant, E. J. Roth, and L.-Q. Zhang. Changes in passive mechanical properties of the gastrocnemius muscle at the muscle fascicle and joint levels in stroke survivors. Arch. Phys. Med. Rehabil. 90:819–826, 2009.
Garteiser, P., R. S. Sahebjavaher, L. C. Ter Beek, S. Salcudean, V. Vilgrain, B. E. Van Beers, and R. Sinkus. Rapid acquisition of multifrequency, multislice and multidirectional MR elastography data with a fractionally encoded gradient echo sequence. NMR Biomed. 26:1326–1335, 2013.
Gennisson, J. L., C. Cornu, S. Catheline, M. Fink, and P. Portero. Human muscle hardness assessment during incremental isometric contraction using transient elastography. J. Biomech. 38:1543–1550, 2005.
Giacomozzi, C., E. D’Ambrogi, S. Cesinaro, V. Macellari, and L. Uccioli. Muscle performance and ankle joint mobility in long-term patients with diabetes. BMC Musculoskelet. Disord. 9:99, 2008.
Green, M. A., L. E. Bilston, and R. Sinkus. In vivo brain viscoelastic properties measured by magnetic resonance elastography. NMR Biomed. 21:755–764, 2008.
Green, M., G. Geng, E. Qin, R. Sinkus, S. Gandevia, and L. Bilston. Measuring anisotropic muscle stiffness properties using elastography. NMR Biomed. 26:1387–1394, 2013.
Green, M., R. Sinkus, S. Gandevia, R. Herbert, and L. Bilston. Measuring changes in muscle stiffness after eccentric exercise using elastography. NMR Biomed. 25:852–858, 2012.
Grounds, M. D., H. G. Radley, G. S. Lynch, K. Nagaraju, and A. De Luca. Towards developing standard operating procedures for pre-clinical testing in the mdx mouse model of Duchenne Muscular Dystrophy. Neurobiol. Dis. 31:1–19, 2008.
Hafer-Macko, C. E., A. S. Ryan, F. M. Ivey, and R. F. Macko. Skeletal muscle changes after hemiparetic stroke and potential beneficial effects of exercise intervention strategies. J. Rehabil. Res. Dev. 45:261–272, 2008.
Hamhaber, U., I. Sack, S. Papazoglou, J. Rump, D. Klatt, and J. Braun. Three-dimensional analysis of shear wave propagation observed by in vivo magnetic resonance elastography of the brain. Acta Biomater. 3:127–137, 2007.
Hoang, P., R. Gorman, G. Todd, S. C. Gandevia, and R. Herbert. A new method for measuring passive length–tension properties of human gastrocnemius muscle in vivo. J. Biomech. 38:1333–1341, 2005.
Huwart, L., C. Sempoux, N. Salameh, J. Jamart, L. Annet, R. Sinkus, et al. Liver fibrosis: noninvasive assessment with MR elastography vs. aspartate aminotransferase-to-platelet ratio index. Radiology 245:458–466, 2007.
Huwart, L., C. Sempoux, E. Vicaut, N. Salameh, L. Annet, E. Danse, et al. Magnetic resonance elastography for the noninvasive staging of liver fibrosis. Gastroenterology 135:32–40, 2008.
Kawakami, Y., H. Kanehisa, and T. Fukunaga. The relationship between passive ankle plantar flexion joint torque and gastrocnemius muscle and achilles tendon stiffness: implications for flexibility. J. Orthop. Sports Phys. Therapy 38:269–276, 2008.
Klatt, D., C. Friedrich, Y. Korth, R. Vogt, J. Braun, and I. Sack. Viscoelastic properties of liver measured by oscillatory rheometry and multifrequency magnetic resonance elastography. Biorheology 47:133–141, 2010.
Krouskop, T. A., T. M. Wheeler, F. Kallel, B. S. Garra, and T. Hall. Elastic moduli of breast and prostate tissues under compression. Ultrason. Imaging 20:260–274, 1998.
Kwah, L. K., R. D. Herbert, L. A. Harvey, J. Diong, J. L. Clarke, J. H. Martin, et al. Passive mechanical properties of gastrocnemius muscles of people with ankle contracture after stroke. Arch. Phys. Med. Rehab. 93:1185–1190, 2012.
Kwon, D. R., G. Y. Park, and J. G. Kwon. The change of intrinsic stiffness in gastrocnemius after intensive rehabilitation with botulinum toxin a injection in spastic diplegic cerebral palsy. Ann. Rehabil. Med. 36:400–403, 2012.
Kwon, D. R., G. Y. Park, S. U. Lee, and I. Chung. Spastic cerebral palsy in children: dynamic sonoelastographic findings of medial gastrocnemius. Radiology 263:794–801, 2012.
Leonard, C. T., W. P. Deshner, J. W. Romo, E. S. Suoja, S. C. Fehrer, and E. L. Mikhailenok. Myotonometer intra-and interrater reliabilities. Arch. Phys. Med. Rehabil. 84:928–932, 2003.
Leonard, C. T., J. U. Stephens, and S. L. Stroppel. Assessing the spastic condition of individuals with upper motoneuron involvement: validity of the myotonometer. Arch. Phys. Med. Rehabil. 82:1416–1420, 2001.
Lieber, R. L., and S. C. Bodine-Fowler. Skeletal muscle mechanics: implications for rehabilitation. Phys. Ther. 73:844–856, 1993.
Lieber, R. L., S. Steinman, I. A. Barash, and H. Chambers. Structural and functional changes in spastic skeletal muscle. Muscle Nerve 29:615–627, 2004.
Linder-Ganz, E., and A. Gefen. Mechanical compression-induced pressure sores in rat hindlimb: muscle stiffness, histology, and computational models. J. Appl. Physiol. 96:2034–2049, 2004.
Lv, F., J. Tang, Y. Luo, Y. Ban, R. Wu, J. Tian, et al. Muscle crush injury of extremity: quantitative elastography with supersonic shear imaging. Ultrasound Med. Biol. 38:795–802, 2012.
Maïsetti, O., F. Hug, K. Bouillard, and A. Nordez. Characterization of passive elastic properties of the human medial gastrocnemius muscle belly using supersonic shear imaging. J. Biomech. 45:978–984, 2012.
Marusiak, J., A. Jaskólska, S. Budrewicz, M. Koszewicz, and A. Jaskólski. Increased muscle belly and tendon stiffness in patients with Parkinson’s disease, as measured by myotonometry. Mov. Disord. 26:2119–2122, 2011.
McCracken, P. J., A. Manduca, J. Felmlee, and R. L. Ehman. Mechanical transient-based magnetic resonance elastography. Magn. Reson. Med. 53:628–639, 2005.
McCullough, M. B., Z. J. Domire, A. M. Reed, S. Amin, S. R. Ytterberg, Q. Chen, and K. N. An. Evaluation of muscles affected by myositis using magnetic resonance elastography. Muscle Nerve 43:585–590, 2011.
Mezzanotte, W. S., D. J. Tangel, and D. P. White. Waking genioglossal electromyogram in sleep apnea patients vs. normal controls (a neuromuscular compensatory mechanism). J. Clin. Investig. 89:1571–1579, 1992.
Muraki, T., Z. J. Domire, M. B. McCullough, Q. Chen, and K.-N. An. Measurement of stiffness changes in immobilized muscle using magnetic resonance elastography. Clin. Biomech. 25:499–503, 2010.
Muthupillai, R., and R. L. Ehman. Magnetic resonance elastography. Nat. Med. 2:601–603, 1996.
Nightingale, K., M. S. Soo, R. Nightingale, and G. Trahey. Acoustic radiation force impulse imaging. In vivo demonstration of clinical feasibility. Ultrasound Med. Biol. 28:227–235, 2002.
Niitsu, M., A. Michizaki, A. Endo, H. Takei, and O. Yanagisawa. Muscle hardness measurement by using ultrasound elastography: a feasibility study. Acta Radiol. 52:99–105, 2011.
Nordez, A., J. Gennisson, P. Casari, S. Catheline, and C. Cornu. Characterization of muscle belly elastic properties during passive stretching using transient elastography. J. Biomech. 41:2305–2311, 2008.
Nordez, A., and F. Hug. Muscle shear elastic modulus measured using supersonic shear imaging is highly related to muscle activity level. J. Appl. Physiol. 108:1389–1394, 2010.
OpenStax College. 2014. Anatomy & Physiology. OpenStax CNX, Jul 31, 2014. http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@6.27@6.27. Accessed 15 Sept 2014
Osman, N. F., W. S. Kerwin, E. R. McVeigh, and J. L. Prince. Cardiac motion tracking using cine harmonic phase (Harp) magnetic resonance imaging. Magn. Reson. Med. 42:1048–1060, 1999.
Pastoret, C., and A. Sebille. Mdx mice show progressive weakness and muscle deterioration with age. J. Neurol. Sci. 129:97–105, 1995.
Proske, U., D. L. Morgan, and J. E. Gregory. Thixotropy in skeletal muscle and in muscle spindles: a review. Prog. Neurobiol. 41:705–721, 1993.
Purslow, P. P. Muscle fascia and force transmission. J. Bodyw. Mov. Ther. 14:411–417, 2010.
Qin, E. C., L. Juge, S. A. Lambert, V. Paradis, R. Sinkus, and L. E. Bilston. In vivo anisotropic mechanical properties of dystrophic skeletal muscles measured by MR elastography with diffusion–tensor imaging: the mdx mouse model of muscular dystrophy. Radiology 2014. doi:10.1148/radiol.14132661.
Qin, E. C., R. Sinkus, G. Geng, S. Cheng, M. Green, C. D. Rae, and L. E. Bilston. Combining MR elastography and diffusion tensor imaging for the assessment of anisotropic mechanical properties: a phantom study. J. Magn. Reson. Imaging 37:217–226, 2013.
Rydahl, S. J., and B. J. Brouwer. Ankle stiffness and tissue compliance in stroke survivors: a validation of myotonometer measurements. Arch. Phys. Med. Rehabil. 85:1631–1637, 2004.
Sandrin, L., M. Tanter, J. L. Gennisson, S. Catheline, and M. Fink. Shear elasticity probe for soft tissues with 1-D transient elastography. Trans. Ultrasonics Ferroelectr. Freq. Control IEEE 49:436–446, 2002.
Shinohara, M., K. Sabra, J. L. Gennisson, M. Fink, and M. Tanter. Real-time visualization of muscle stiffness distribution with ultrasound shear wave imaging during muscle contraction. Muscle Nerve 42:438–441, 2010.
Sinkus, R., M. Tanter, S. Catheline, J. Lorenzen, C. Kuhl, E. Sondermann, and M. Fink. Imaging anisotropic and viscous properties of breast tissue by magnetic resonance-elastography. Magn. Reson. Med. 53:372–387, 2005.
Talwalkar, J. A., M. Yin, J. L. Fidler, S. O. Sanderson, P. S. Kamath, and R. L. Ehman. Magnetic resonance imaging of hepatic fibrosis: emerging clinical applications. Hepatology 47:332–342, 2008.
Tian, M., R. D. Herbert, P. Hoang, S. C. Gandevia, and L. E. Bilston. Myofascial force transmission between the human soleus and gastrocnemius muscles during passive knee motion. J. Appl. Physiol. 113:517–523, 2012.
Tian, M., P. D. Hoang, S. C. Gandevia, L. E. Bilston, and R. D. Herbert. Stress relaxation of human ankles is only minimally affected by knee and ankle angle. J. Biomech. 43:990–993, 2010.
Torres, L., and L. Duchen. The mutant mdx: inherited myopathy in the mouse morphological studies of nerves, muscles and end-plates. Brain 110:269–299, 1987.
Vain, A. Estimation of the Functional State of Skeletal Muscle. In: Control of Ambulation Using Functional Neuromuscular Stimulation, edited by P. H. Veltink, and H. B. K. Boom. Enschede: University of Twente Press, 1995, pp. 51–55.
Van Houten, E. E. W., M. M. Doyley, F. E. Kennedy, J. B. Weaver, and K. D. Paulsen. Initial in vivo experience with steady-state subzone-based MR elastography of the human breast. J. Magn. Reson. Imaging 17:72–85, 2003.
Van Houten, E., J. Weaver, M. Miga, F. Kennedy, and K. Paulsen. Elasticity reconstruction from experimental MR displacement data: initial experience with an overlapping subzone finite element inversion process. Med. Physics. 27:101–107, 2000.
Van Loocke, M., C. G. Lyons, and C. K. Simms. A validated model of passive muscle in compression. J. Biomech. 39:2999–3009, 2006.
van Turnhout, M., G. Peters, A. Stekelenburg, and C. Oomens. Passive transverse mechanical properties as a function of temperature of rat skeletal muscle in vitro. Biorheology 42:193–207, 2005.
Vasilescu, D., D. Vasilescu, S. Dudea, C. Botar-Jid, S. Sfrângeu, and D. Cosma. Sonoelastography contribution in cerebral palsy spasticity treatment assessment, preliminary report: a systematic review of the literature apropos of seven patients. Med. Ultrason. 12:306–310, 2010.
Veldi, M., V. Vasar, T. Hion, A. Vain, and M. Kull. Myotonometry demonstrates changes of lingual musculature in obstructive sleep apnoea. Eur. Arch. Otorhinolaryngol. 259:108–112, 2002.
Zerhouni, E. A., D. M. Parish, W. J. Rogers, A. Yang, and E. P. Shapiro. Human heart: tagging with MR imaging–a method for noninvasive assessment of myocardial motion. Radiology 169:59–63, 1988.
Zhijie, Z., K. Cw, L. Wc, and S. Fu. Shearwave ultrasound elastography of thigh muscles: intra- and inter-rater reliability. Ultrasound Med. Biol. 37:S141–S142, 2011.
Acknowledgments
Lynne Bilston is supported by an NHMRC senior research fellowship. The authors have no competing interests to declare. The authors would like to thank Professor Rob Herbert for his insightful comments on a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Amit Gefen oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Bilston, L.E., Tan, K. Measurement of Passive Skeletal Muscle Mechanical Properties In Vivo: Recent Progress, Clinical Applications, and Remaining Challenges. Ann Biomed Eng 43, 261–273 (2015). https://doi.org/10.1007/s10439-014-1186-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-014-1186-2