Abstract
Studies of health trends in older populations usually focus on single health indicators. We include multiple medical and functional indicators, which together indicate the broader impact of health problems experienced by individuals and the need for integrated care from several providers of medical and long-term care. The study identified severe problems in three health domains (diseases/symptoms, mobility, and cognition/communication) in three nationally representative samples of the Swedish population aged 77+ in 1992, 2002, and 2011 (n ≈ 1900; response rate >85 %). Institutionalized people and proxy interviews were included. People with severe problems in two or three domains were considered to have complex health problems. Results showed a significant increase of older adults with complex health problems from 19 % in 1992 to 26 % in 2002 and no change thereafter. Changes over time remained when controlling for age and sex. When stratified by education, complex health problems increased significantly for people with lower education between 1992 and 2002 and did not change significantly between 2002 and 2011. For higher-educated people, there was no significant change over time. Among the people with severe problems in the symptoms/disease domain, about half had no severe problems in the other domains. People with severe mobility problems, on the other hand, were more likely to also have severe problems in other domains. Even stable rates may imply an increasing number of very old people with complex health problems, resulting in a need for improved coordination between providers of medical care and social services.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since the mid-twentieth century, life expectancy in Sweden has increased largely as a consequence of falling mortality in older ages (Christensen et al. 2009; Rau et al. 2008). The proportion of the population aged 80 years or older is projected to double until 2050 when almost 10 % of the population is predicted to be 80 years or older (Statistics Sweden 2015). Similar trends are observed across EU and OECD countries (OECD/European Union 2013). Since age is strongly associated with health problems, a frequently debated question is whether the years ‘added to life’ are characterized by good health and independence or by health problems—often multiple problems. This issue has implications for individuals and their families as well as for society in financing and organizing medical and social care services (i.e., institutional living and home-help services).
Most studies that have addressed health trends in older populations have used single indicators and fewer studies have addressed multiple morbid conditions in the older population. However, after age 80, chronic conditions and functional declines precede most deaths (Larsson et al. 2008; Lunney et al. 2003). The simultaneous presence of multiple health problems is one of the greatest challenges in eldercare (Valderas et al. 2009). This entails the medical challenge of balancing treatment strategies (Barnett et al. 2012; Rockwood and Mitnitski 2011), as well as integrating medical care in the long-term care (LTC) plan that can include rehabilitation, social services, and informal care (Meinow et al. 2006). To develop effective models for communication and coordination between providers, it is necessary to identify patterns of health problems and follow how they change over time. This study investigates changes between 1992, 2002, and 2011 in the prevalence of complex health problems, i.e., the simultaneous presence of diseases/symptoms, cognitive, and physical functional limitations, in three national representative samples of the Swedish population aged 77 and over.
Speculation about the compression or expansion of morbidity in the population has led to numerous trend studies using population survey data (Chatterji et al. 2015; Robine and Michel 2004; Sole-Auro and Alaniz 2014). Results have revealed diverging trends depending on countries, time points, methodology and on which health indicator has been used (Crimmins and Beltrán-Sánchez 2011; Parker and Thorslund 2007). In general, prevalence rates of chronic diseases have been found to increase since the early 1990s while studies using disability and physical functional indicators have shown mixed results (Crimmins and Beltrán-Sánchez 2011; Galenkamp et al. 2013; Martin et al. 2012; Parker and Thorslund 2007).
Composite measures may to a larger extent reflect the broader impact of health problems experienced by individuals and their families. From a policy and planning perspective such indicators reflect the extent of complex care needs in the older population involving different sources of medical and social services (Meinow et al. 2006). In clinical research growing attention to complex health profiles has led to the creation of composite measures such as multimorbidity (Barnett et al. 2012; Marengoni et al. 2011), frailty (Fried et al. 2004; Rodriguez-Manas et al. 2012), and multiple chronic conditions (Freid et al. 2012). These measures have arisen from different perspectives and with different aims (Valderas et al. 2009). Rather than studying population health trends, studies based on these concepts usually focus on how the coexistence of diseases and/or physiological markers are associated with other outcomes. The main goal is often to identify people at risk for negative outcomes, e.g., disability and death, in order to improve medical treatment and prevention (Sourial et al. 2013; Whitson et al. 2007). These measures rely primarily on clinical data such as diagnosed disease and physiological markers and are therefore highly correlated with an individual’s needs for medical care.
For example, multimorbidity addresses the simultaneous presence of two or more diseases in the same individual (Marengoni et al. 2011). ‘Frailty’ is a concept that has been used to describe a geriatric syndrome, implying a multifactorial state of physiologic vulnerability, regardless of the presence or absence of disease, when the body’s ability to recover from physiological stress is limited (Fried et al. 2004; Walston et al. 2006). Although there is yet no consensus about how to measure frailty (Rodriguez-Manas et al. 2012), there are two main approaches: The phenotypic operationalization is typically based on the presence of a number of clinical criteria, e.g., weakness, unintentional weight loss, and slow gait speed (Fried et al. 2004). The deficit accumulation approach, on the other hand, is based on the number of deficits that an individual has accumulated from a given number of potential deficits, rather than specifying which deficits should be considered (Rockwood and Mitnitski 2011; Searle et al. 2008).
Several studies have shown that multimorbidity and frailty increase the risk for negative outcomes. For example, frailty has been shown to predict future institutionalization (Puts 2005), and multimorbidity has been found to predict subsequent decline in mobility and ability to perform activities of daily living (ADL) (Gijsen et al. 2001; Marengoni et al. 2011). Both concepts are valuable for identifying individuals who may benefit from interventions in order to prevent and/or delay disability and/or LTC (e.g., home-help services, home nursing, and institutional living). However, neither concept fully reflects actual needs for LTC, i.e., the major portion of formal care provided among the oldest old (Forma et al. 2009). While some people with multimorbidity also need LTC, many others are able—with treatment—to live independently. On the other hand older people’s health problems are not always attributable to a specific disease, e.g., dizziness, fatigue, memory loss, and walking difficulties. These problems may not be treatable and often lead to a need for LTC. Many composite measures do not include cognitive impairment, a condition that is strongly related to the need for LTC. Disease-based clinical measures therefore do not capture the total need for medical and social care.
We were interested in estimating the total care needs, including physical and cognitive disabilities, in the population and studying change in care needs over time. Few studies have examined trends over time in measures that encompass this broad range of multiple conditions. Rather than identifying people at risk for negative outcomes who can be targeted for interventions, focus in this study is on those older persons who are already overtly functionally compromised and experience severe problems in multiple health domains.
We constructed a measure of multiple health problems based on a nationally representative population-based survey. The term ‘complex health problems’ reflects the simultaneous presence of severe problems in different health domains, related to needs for care from several providers of medical and social services. Using nationally representative samples of the Swedish population, we identified three important health domains: symptoms/diseases, cognition/communication, and mobility. Persons with severe problems in at least two domains were considered to have complex health problems. An earlier study revealed an increase in the prevalence of complex health problems between 1992 and 2002 (Meinow et al. 2006). This study investigates (i) whether this trend persisted in a 2011 wave of the same survey, (ii) to what extent changes in prevalence rates were due to compositional changes with regard to age, sex, and education, and (iii) whether trends in prevalence rates differed by sociodemographic factors (sex, age, and education). We also explore the prevalence of different combinations of severe problems, i.e., to what extent do severe problems in one domain occur in combination with other domains?
Materials and methods
Data source and collection
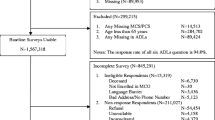
The study was based on the Swedish Panel Study of Living Conditions of the Oldest Old (SWEOLD), a nationally representative survey among Swedes aged 77 or older, conducted in 1992, 2002, and 2011 (n = 537; 621 and 904) (Lennartsson et al. 2014). The Swedish system of personal identification numbers facilitated random samples of the population that are representative in regards to the national distribution of age, sex, geography, and proportion living in institutional care facilities.
We achieved high response rates (1992: 90 %; 2002: 87 %; 2011: 86 %) through intensive fieldwork that was designed to include very frail and cognitively impaired older persons. This necessitated the use of several interview modes: Direct face-to-face interviews were conducted in the respondent’s dwelling whenever possible. If a respondent refused to meet the interviewer or was not able to manage an interview on his or her own, we offered to conduct the interview by telephone with the respondent or with the support of a relative (mixed interview). Proxy interviews with relatives or caregivers were carried out when the respondent was unable to participate at all. Mail questionnaires were used in 2011 as a last resort. The same questionnaire was used irrespective of the interview mode although the mail questionnaire was shorter. Sample characteristics in the three surveys are shown in Table 1. The later samples were older, had more years of education, and included a somewhat higher proportion of proxy interviews. Due to missing information on two of the three health domains (cognition/communication; mobility), mail questionnaires were excluded from further analyses. However, we assessed the extent to which mail questionnaire respondents and directly interviewed respondents deviated in regards to other available health items (see discussion).
The SWEOLD 1992 data collection was approved by Uppsala University Hospital Ethical Committee (Dnr 247/91), the SWEOLD 2002 data collection was approved by the Karolinska Institutet Ethical Research Committee (Dnr 03-413), and the SWEOLD 2011 data collection was also approved by the Regional Ethical Review Board in Stockholm (Dnr 2010/403-31/4).
Measures
Measures were selected to represent a variety of health domains that are related to the need for different types of services (Meinow et al. 2006). In general, symptoms and diseases imply needs for medical care, while mobility problems imply needs for social services and/or informal care. Individuals with severe cognition/communication problems often need help from several kinds of care providers.
In order to provide comparable and nationally representative estimates, we used only measures that were identical for all survey years and available for the whole sample, including proxy interviews. This excluded tests of function (with the exception of the cognition test, see below) and subjective evaluations of health. Moreover, we selected measures that are less vulnerable to environmental change, e.g., we studied changes in mobility instead of ADL disability.
Severe problems in three health domains were identified:
-
(1)
Symptoms/diseases This domain was based on a summed index from a list of common symptoms and diseases headed by the question “Have you had any of the following diseases or symptoms during the previous 12 months? (Table 2) “No” was coded as 0, “Yes, mild” was coded as 1, and “Yes, severe” was coded as 3. Body mass index (BMI) under 16 was coded as severe underweight (3), between 16 and under 22 as mild underweight (1) and 22 or more as not underweight (0) (Andersen 2003). Underweight is considered to be a good predictor of mortality among old people (Seidell and Visscher 2000). The summed index ranged from 0 to 42 and a cut-off for severe problems for this domain was determined at the highest quintile for the 1992 sample (corresponding to 9 on the summed scale) (Meinow et al. 2006). Accordingly, the persons belonging to the highest quintile had, e.g., at least three severe symptoms/diseases or two severe and three mild. The same cut-off was used for the 2002 and 2011 samples.
Table 2 Prevalence rates for health problems in 1992, 2002, and 2011. Unadjusted and adjusted for the age and sex distribution in 2002 -
(2)
Mobility This domain was an index of four items: the reported ability to walk 100 meters fairly briskly without difficulties, walk up stairs, rise from a chair without difficulty, and stand without support. Limitations in at least three of the four activities were coded as severe mobility problems.
-
(3)
Cognition/communication A short form of the Mini-Mental-State Examination (Folstein et al. 1975) with 11 of the 30 original points was used. A cut-off (<7) was determined using data from a larger Swedish study HARMONY with the full MMSE scale and clinical dementia diagnoses (Gatz et al. 2005). The same items and cut-off were used in all three surveys. Interviewer notes showed that proxy interviewed persons were too sick or weak to participate, the vast majority due to cognitive problems or, in a few cases, aphasia. Therefore, respondents who scored below 7 in the test, did not do the test, or were proxy interviewed were coded as having severe cognitive/communication problems. Thus, this measure is not an indicator of pure cognition but rather roughly captures respondents having at least cognitive impairment or being unable to communicate with the interviewer. This involves an important dimension of dependence in daily life, not least in managing one’s own care contacts.
People who had severe problems in two or three health domains were considered to have complex health problems.
Education, based on years of schooling, was dichotomized into 0–8 years (which corresponds to compulsory education only) or 9 years or more in Table 1. In Table 4, years of education were given linear representation.
Analyses
Tables 2 and 3 present unadjusted prevalence rates of health problems and rates adjusted for differences in the age and sex composition of the three samples. Estimations of unadjusted prevalence rates provide key information for planning appropriate services while adjusted rates can explain whether time trends are independent of compositional changes in the population. Logistic regressions were used to analyze the impact of survey year, sex, and education on the odds of having complex health problems (Table 4). We also included interaction terms for the survey year and sex, the survey year and age and the survey year and education, in order to analyze whether trends in the prevalence of complex health problems differed for subgroups of the older population.
Results
Figure 1 shows the combinations of severe problems in the three health domains in 2011. The inner circles represent the 55 % of the sample with severe problems in at least one domain. Among these, almost half (46 %) also had severe problems in one or both of the other domains. The majority of respondents with severe mobility limitations or cognition/communication problems had severe problems in other domains(s). Among the 24 % in the total sample facing severe mobility problems, the vast majority (86 %) also had severe problems in at least one other domain. Among the 28 % with severe cognition/communication problems, over two thirds (70 %) also had severe problems in one or both of the other domains. In contrast, among those 34 % respondents with multiple severe symptoms/diseases, about half (49 %) had no severe limitations in other domains. Figure 1 shows figures for the 2011 wave; however, patterns of combinations were similar for all three waves.
Table 2 presents the proportion of people having problems with each of the items included in the three health domains in 1992, 2002, and 2011. Table 3 presents corresponding figures for the proportions of severe problems in each of the three domains and for the number of domains with severe problems. For most health problems, unadjusted and adjusted prevalence rates were similar. Significant differences for 1992 compared to 2002, for 2002 compared to 2011, and for the whole study period 1992–2011 are indicated with asterisks.
Adjusted prevalence rates: the clearest increase in severe problems occurred for the symptoms/disease domain, from 21 % in 1992 to 32 % in 2002 and 34 % in 2011 (Table 3). The significant increase occurred mainly during the first 10-year period. Several symptoms (e.g., pain, fatigue/sleeplessness) and diseases (e.g., myocardial infarction/other heart problems, diabetes) and mild and severe problems showed increases (Table 2). With the exception of low BMI none of the symptoms/diseases showed a significant decrease over time.
The development for severe mobility limitations showed a similar trend as the disease/symptom domain, but the increase was only significant at the 10 %-level (Table 3). Within the mobility domain the development was ambiguous: while the prevalence of older adults who had difficulties rising from a chair or walking up stairs increased, there was no clear trend in regards to the ability to walk 100 m and to stand without support (Table 2). Severe cognition/communication problems also showed a significant increase from 27 to 33 % between 1992 and 2002, but a decrease thereafter (significant at the 10 %-level). For the whole 19-year period there was no significant change (Table 3).
Number of domains with severe problems: the adjusted proportion of individuals with complex health problems showed a significant increase from 19 % in 1992 to 26 % in 2002 and remained relatively stable thereafter. The prevalence of severe problems in one domain showed a similar pattern (Table 3).
In Table 4, the odds ratios show the odds of having complex health problems in 1992 and in 2011 compared to 2002, and in 2011 compared to 1992. In the first model, only differences over time were analyzed. Compared to 2002, the odds of having complex health problems were 37 % lower in 1992, while there was no difference between 2002 and 2011. For the whole 19-year period, the odds for complex health problems were 55 % higher in 2011 compared to 1992. Models 2–4 examine if the odds of having complex health problems was influenced by sociodemographic variables known to be related to health. The age and sex distributions were slightly different in the three waves and the educational level rose during the period. However, the results remained when adding age, sex, and education one by one in models 2–4. Controlled for the other three variables, women had 54 % higher odds of having complex health problems compared to men. For every 5 years of age, the odds of having complex health problems increased by 84 %. In contrast, for every additional year of education the odds decreased by 12 %.
The association between age and complex health problems and the association between sex and complex health problems did not differ significantly between the survey waves, i.e., there were no significant interactions between the survey year and sex and the survey year and age (not shown). However, the association between education and complex health problems differed between the survey years, significant at the 10 %-level (p = 0.09) (Table 4). For lower-educated people, complex health problems increased significantly from 1992 to 2002, followed by a non-significant increase from 2002 to 2011. When change was modeled consecutively between 1992, 2002, and 2011, the association was statistically significant (OR 1.39; p = 0.001; not shown). For higher-educated people, there was no significant change over time in the odds of having complex health problems.
Discussion
This study defined complex health problems as severe problems in at least two of three health domains (symptoms/diseases, mobility, and cognition/communication). Using three nationally representative samples of the Swedish population aged 77 and older, we examined changes in the prevalence of complex health problems between 1992, 2002, and 2011, whether trends were independent of compositional changes of the population, and whether trends differed for different groups of older adults. We also explored the extent to which severe problems in one domain occurred in combination with severe problems in other domains.
Results showed that complex health problems increased significantly from 19 % in 1992 to 26 % in 2002 with no significant change thereafter. A similar pattern occurred for severe problems in one health domain. The greatest increase in severe problems occurred for multiple symptoms/diseases, from about one fifth in 1992 to one third in 2011. Mobility problems and cognition/communication problems also increased significantly between 1992 and 2002 with no clear trends thereafter. The results remained when adjusting for age and sex meaning that compositional changes in the samples did not explain the observed time trend. Yet, consistent with previous studies that investigated factors associated to health (Agborsangaya et al. 2012; Uijen and van de Lisdonk 2008), our results indicated that female sex, higher age, and low education significantly and independently increased the odds of having complex health problems. If the level of education had not increased as it did between 1992 and 2011, the increase in complex health problems would probably have been greater.
Few studies have examined trends in the prevalence of multiple health problems, and these are usually limited to diseases and/or physiological indicators. For example, a Dutch study of multimorbidity showed an increase between 1985 and 2005 (Uijen and van de Lisdonk 2008). Swedish survey data found an increased prevalence of multiple chronic conditions among people aged 65–84 between 1988/1994 and 1995/2002 (Rosén and Haglund 2005). Survey data from the US for the community-dwelling population 65 years and older between 1998 and 2008 (Hung et al. 2011) and between 1999/2000 and 2009/2010 also found increased prevalence rates (Freid et al. 2012).
Patterns over time in the prevalence of complex health problems did not differ significantly between men and women or between age groups. However, for lower-educated people the odds of having complex health problems increased significantly between 1992 and 2002 with no significant change thereafter. For higher-educated people, there was no significant change over time in the odds of having complex health problems. Over the last two decades, persisting or widening socioeconomic health inequalities have been shown even in highly developed welfare states (Mackenbach 2012). However, the mechanisms behind the associations between socioeconomic position and health are not fully understood. According to the fundamental cause theory (Link and Phelan 1995; Phelan et al. 2009), higher-educated people use their flexible resources (such as money, knowledge, and social connections) to gain faster access to care, obtain better health information and avoid risk. Irrespectively of the mechanisms linking socioeconomic position to health, more advantaged persons will use their flexible resources to attain a health advantage over persons in lower social strata. Earlier access to medical care developments for higher-educated people during the 1990s, e.g., in regards to cardiovascular disease, could have contributed to the initial increase of complex health problems among the lower educated between 1992 and 2002. In Sweden, socioeconomic inequality in health care use was small in the 1970s and 1980s, but increased during the 1990s, especially in regards to the use of specialized care (Agerholm et al. 2013; Hanratty et al. 2007). It is also possible that the relative importance of education for health varies over time. For example, as more recent cohorts have, on average, higher education, the selection into low education may be more strongly related to poor health (Mackenbach 2012; Dowd and Hamoudi 2014).
Several medical studies have examined how diseases cluster together (Formiga et al. 2013; Marengoni et al. 2009) and how different multi-morbid constructs overlap (Fried 2003). In this study, we examined the overlap of the three domains of complex health problems. Among the people with multiple severe symptoms/diseases, about half had no severe problems in the other domains. This indicates that there may be a substantial group of older adults who need different kinds of medical care but who may be able to live independently. People with severe mobility problems or cognition/communication problems, on the other hand, were more likely to also have severe problems in other domains. Medical improvements and earlier diagnoses may contribute to the fact that people initially live with multiple diagnoses without severe functional limitations. The presence of functional limitations in addition to diseases may indicate a more severe state in the disablement process (Verbrugge and Jette 1994).
Compared to many surveys from larger countries, the SWEOLD samples are small. However, a strength of this study is the high response rate, the inclusion of people with poor cognition and institutionalized people. The health measures used in this study are necessarily crude as they were directed to a nationally representative sample, including proxy interviews. In an effort to cover the most vulnerable subset of the older population, we made our definition of complex health problems restrictive, setting high thresholds for severe problems within each domain. While composite health measures combining multiple problems in several health domains may be too broad for planning specific types of care related to specific diseases, they are useful to reflect the need for integrated and coordinated medical and social services. However, people with problems in only one domain may also need care from a variety of providers. Thus, rates of complex health problems as measured in this study probably underestimate actual needs for coordinated care in the older population.
The exclusion of mail questionnaires in 2011 due to missing information on cognition and mobility items could have affected reported prevalence rates. Analyses revealed that participants who answered by mail questionnaires were less likely to have severe problems in the symptoms/disease domain compared to directly interviewed persons. However, there were no significant differences with regard to age, sex, and ADL disability between mail respondents and directly interviewed respondents. Another development that could have affected prevalence rates of severe cognition/communication problems is the increase of proxy interviews from 12 % in 1992 to 16 % in 2011. This increase could be due to worsened health or due to a “lower threshold” for being proxy interviewed. However, adjusted for age, sex, number of diseases/symptoms, and physical function the probability of being proxy interviewed did not increase significantly over time.
Changes in prevalence rates of health problems may arise due to incidence changes and/or changes in survival despite health problems. Rates may also change due to change in reporting, better diagnoses, as well as improvements of assistive devices. For example, the increased prevalence of mild stroke between 1992 and 2002 could be due to the combined effect of stable incidence rates and increased survival after stroke reported in other Swedish studies (Hallstrom et al. 2008; Stegmayr and Asplund 2003). In addition, as a consequence of increased knowledge among patients and physicians mild strokes may have been increasingly detected and diagnosed (Stegmayr and Asplund 2003). Self-reported measures of mobility may be vulnerable to changes in expectations but are probably less affected by environmental modifications and technical aids than measures of ADL. A Dutch study that compared the agreement between self-reported and GP-recorded chronic diseases among older adults in 1992/93 and 2008/09 found that overreporting of diseases had increased during the period, while underreporting had decreased (Galenkamp et al. 2014). However, a study based on the SWEOLD data including tests of function revealed similar trends as in this study, i.e., worsening between 1992 and 2002 and little change thereafter (Fors et al. 2013). Moreover, we found increases in diseases as well as in symptoms that are inherently subjective. Yet, it is possible that similar complaints are nowadays more often reported as a problem instead of being attributed to old age (Galenkamp et al. 2014).
Sweden has one of the world’s oldest populations in regards to the proportion of people 80 years and older and can in this respect be seen as a precursor when considering the implications of aging societies for population health. An increase of prevalence rates of complex health problems between 1992 and 2002 could reflect the emergence of a very frail old population as proposed by Robine and Michel (2004). There is no self-evident explanation for the stabilization of the prevalence of complex health problems after 2002. However, it has been suggested that the interplay of mortality and morbidity patterns may be affected by different factors (Robine and Michel 2004): Initially, survival of sick persons due to better living conditions and medical advancements may lead to an increase in the prevalence of complex health problems in the population (OECD 2009). In a 4-year mortality analysis of the 1992 and 2002 SWEOLD waves, we found that although the presence of complex health problems was a strong predictor of mortality in both survey years, survival for men with complex health problems increased while there was no change in mortality risks for healthier individuals (Meinow et al. 2010). Another Swedish study suggested that increased longevity in Sweden in the 1990s was mainly due to successful life-saving interventions from medical care, especially in regards to cardiovascular diseases, whereas it was healthier lifestyles that contributed substantially to prolonged life expectancy in the 1980s (Rosén and Haglund 2005). One contributing factor to the stability of prevalence rates of complex health problems after 2002 could be that there was not as much room for additional life-saving medical improvements during the 2000s as during the 1990s. In addition, better disease control, improvements in assistive technology and new cohorts with better living conditions and education entering old age, may lead to a subtle equilibrium between the fall of mortality and the increases in morbidity (Crimmins and Beltrán-Sánchez 2011; Robine and Michel 2004; Sole-Auro and Alaniz 2014). Further population-based studies, including incidence data, are needed to improve hypotheses for the explanation of observed health trends.
Even with optimistic assumptions about health trends, the growing number and proportion of very old people in the population entails a challenge for the amount, the structure, and the organization of medical and social services. Increasing rates of people aged 77 or older with complex health problems during the 1990s and stable rates since the beginning of the 2000s corresponded to an increase from 104,000 individuals in 1992 to 172,000 individuals in 2002 and 2011. Even under the assumption of continuous stable prevalence rates after 2011, this would entail an increase to 250,000 individuals with complex health problems in 2025 as large birth cohorts born in the 1940s pass the age of 77.
In Sweden as in other countries, medical care tends to be oriented toward single and acute conditions (Barnett et al. 2012), and coordination between, e.g., medical specialties and between inpatient and outpatient care is often poor. People with complex health problems often need a variety of services from both medical and LTC providers. As the ability to navigate the care system decreases with poor health (Meinow et al. 2011), care providers need to develop new models of communication and coordination (Boyd et al. 2007; Glendinning 2008). This is of particular relevance since there has been a dramatic decrease by almost one fourth of the beds in institutional care in Sweden since the beginning of the century, and an increasing majority of very frail old people are cared for at home (National Board of Health and Welfare 2014).
References
Agborsangaya CB, Lau D, Lahtinen M, Cooke T, Johnson JA (2012) Multimorbidity prevalence and patterns across socioeconomic determinants: a cross-sectional survey. BMC Public Health 12:201. doi:10.1186/1471-2458-12-201
Agerholm J, Bruce D, de Leon AP, Burström B (2013) Socioeconomic differences in healthcare utilization, with and without adjustment for need: an example from Stockholm, Sweden. Scand J Public Health 41:318–325
Andersen M (ed) (2003) Mat och näring för sjuka inom vård och omsorg [Diet and nutrition for persons receiving social services or medical care]. Livsmedelsversket, Uppsala
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B (2012) Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 380:37–43. doi:10.1016/S0140-6736(12)60240-2
Boyd CM et al (2007) Guided care for multimorbid older adults. Gerontologist 47:697–704
Chatterji S, Byles J, Cutler D, Seeman T, Verdes E (2015) Health, functioning, and disability in older adults-present status and future implications. Lancet 385:563–575. doi:10.1016/s0140-6736(14)61462-8
Christensen K, Doblhammer G, Rau R, Vaupel JW (2009) Ageing populations: the challenges ahead. Lancet 374:1196–1208
Crimmins EM, Beltrán-Sánchez H (2011) Mortality and morbidity trends: is there compression of morbidity? J Gerontol B Psychol Sci Soc Sci 66:75–86
Dowd JB, Hamoudi A (2014) Is life expectancy really falling for groups with low socio-economic status? Lagged selection bias and artefactual trends in mortality. Int J Epidemiol 43:983–988
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Forma L, Rissanen P, Aaltonen M, Raitanen J, Jylha M (2009) Age and closeness of death as determinants of health and social care utilization: a case-control study. Eur J Public Health 19:313–318
Formiga F, Ferrer A, Sanz H, Marengoni A, Alburquerque J, Pujol R (2013) Patterns of comorbidity and multimorbidity in the oldest old: the Octabaix study. Eur J Intern Med 24:40–44. doi:10.1016/j.ejim.2012.11.003
Fors S, Lennartsson C, Agahi N, Parker MG, Lundberg O, Thorslund M (2013) Äldre har fått fler hälsoproblem, men klarar vardagen bättre [Increased prevalence of health problems among older people but increased ability to manage activities of daily living]. Lakartidningen 110:1403–1405
Freid VM, Bernstein AB, Bush MA (2012) Multiple chronic conditions among adults aged 45 and over: trends over the past 10 years. NCHS data brief, no 100. National Center for Health Statistics Hyattsville, MD
Fried LP (2003) Establishing benchmarks for quality care for an aging population: caring for vulnerable older adults. Ann Intern Med 139:784–786
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G (2004) Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol Biol Sci Med Sci 59:255–263
Galenkamp H, Braam AW, Huisman M, Deeg DJ (2013) Seventeen-year time trend in poor self-rated health in older adults: changing contributions of chronic diseases and disability. Eur J Public Health 23:511–517. doi:10.1093/eurpub/cks031
Galenkamp H, Huisman M, Braam AW, Schellevis FG, Deeg DJ (2014) Disease prevalence based on older people’s self-reports increased, but patient-general practitioner agreement remained stable, 1992–2009. J Clin Epidemiol 67:773–780. doi:10.1016/j.jclinepi.2014.02.002
Gatz M et al (2005) Complete ascertainment of dementia in the Swedish Twin Registry: the HARMONY study. Neurobiol Aging 26:439–447
Gijsen R, Hoeymans N, Schellevis FG, Ruwaard D, Satariano WA, van den Bos GA (2001) Causes and consequences of comorbidity: a review. J Clin Epidemiol 54:661–674
Glendinning C (2008) Increasing choice and control for older and disabled people: a critical review of new developments in England. Soc Policy Adm 42:451–469
Hallstrom B, Jonsson AC, Nerbrand C, Norrving B, Lindgren A (2008) Stroke incidence and survival in the beginning of the 21st century in southern Sweden: comparisons with the late 20th century and projections into the future. Stroke 39:10–15. doi:10.1161/strokeaha.107.491779
Hanratty B, Zhang T, Whitebreac M (2007) How close have universal health systems come to achieving equity in use of curative services? A systematic review. Int J Health Serv 37:89–109
Hung WW, Ross JS, Boockvar KS, Siu AL (2011) Recent trends in chronic disease, impairment and disability among older adults in the United States. BMC Geriatr 11:47. doi:10.1186/1471-2318-11-47
Larsson K, Kåreholt I, Thorslund M (2008) Care utilisation in the last years of life in relation to age and time to death; results from a Swedish urban population of the oldest old. Eur J Ageing 5:349–357
Lennartsson C et al (2014) Data resource profile: the Swedish Panel Study of Living Conditions of the Oldest Old (SWEOLD). Int J Epidemiol. doi:10.1093/ije/dyu057
Link BG, Phelan J (1995) Social conditions as fundamental causes of disease. J Health Soc Behav 35:80–94
Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM (2003) Patterns of functional decline at the end of life. JAMA 289:2387–2392
Mackenbach JP (2012) The persistence of health inequalities in modern welfare states: the explanation of a paradox. Soc Sci Med 75:761–769. doi:10.1016/j.socscimed.2012.02.031
Marengoni A, Rizzuto D, Wang HX, Winblad B, Fratiglioni L (2009) Patterns of chronic multimorbidity in the elderly population. J Am Geriatr Soc 57:225–230
Marengoni A et al (2011) Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev 10:430–439. doi:10.1016/j.arr.2011.03.003
Martin LG, Schoeni RF, Andreski PM, Jagger C (2012) Trends and inequalities in late-life health and functioning in England. J Epidemiol Community Health 66:874–880. doi:10.1136/jech-2011-200251
Meinow B, Parker MG, Kåreholt I, Thorslund M (2006) Complex health problems in the oldest old in Sweden 1992–2002. Eur J Ageing 3:98–106
Meinow B, Parker MG, Thorslund M (2010) Complex health problems and mortality among the oldest old in Sweden: decreased risk for men between 1992 and 2002. Eur J Ageing 7:81–90
Meinow B, Parker MG, Thorslund M (2011) Consumers of eldercare in Sweden: the semblance of choice. Soc Sci Med 73:1285–1289
National Board of Health and Welfare (2014) Tillståndet och utvecklingen inom hälso- och sjukvård och socialtjänst. Lägesrapport 2014 [The situation and the development of medical care and social services in Sweden. Report 2014]. National Board of Health and Welfare, Stockholm
OECD (2009) Health at a Glance 2009. OECD Publishing, Paris
OECD/European Union (2013) A good life in old age? OECD health policy studies. OECD Publishing, Paris
Parker MG, Thorslund M (2007) Health trends in the elderly population: getting better and getting worse. Gerontologist 47:150–158
Phelan JC, Link BG, Tehranifar P (2009) Social conditions as fundamental causes of health inequalities theory, evidence and policy implications. J Health Soc Behav 51:28–40
Puts MT (2005) The effect of frailty on residential/nursing home admission in the Netherlands independent of chronic diseases and functional limitations. Eur J Ageing 2:264–274
Rau R, Soroko E, Jasilionis D, Vaupel JW (2008) Continued reductions in mortality at advanced ages. Popul Dev Rev 34:747–768
Robine JM, Michel JP (2004) Looking forward to a general theory on population aging. J Gerontol Biol Sci Med Sci 59:M590–M597
Rockwood K, Mitnitski A (2011) Frailty defined by deficit accumulation and geriatric medicine defined by frailty. Clin Geriatr Med 27:17–26. doi:10.1016/j.cger.2010.08.008
Rodriguez-Manas L et al (2012) Searching for an operational definition of frailty: a Delphi method based consensus statement. The frailty operative definition-consensus conference project. J Gerontol Biol Sci Med Sci 68:62–67. doi:10.1093/gerona/gls119
Rosén M, Haglund B (2005) From healthy survivors to sick survivors—implications for the twenty-first century. Scand J Public Health 33:151–155
Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K (2008) A standard procedure for creating a frailty index. BMC Geriatr 8:24. doi:10.1186/1471-2318-8-24
Seidell JC, Visscher TL (2000) Body weight and weight change and their health implications for the elderly. Eur J Clin Nutr 54(Suppl 3):S33–S39
Sole-Auro A, Alaniz M (2014) Are we living longer but less healthy? Trends in mortality and morbidity in Catalonia (Spain), 1994–2011. Eur J Ageing 12:61–70
Sourial N et al (2013) Implementing frailty into clinical practice: a cautionary tale. J Gerontol Biol Sci Med Sci 68:1505–1511. doi:10.1093/gerona/glt053
Statistics Sweden (2015) Population projections. http://www.statistikdatabasen.scb.se/pxweb/sv/ssd/START__BE__BE0401__BE0401A/BefolkprognRev2014/table/tableViewLayout1/?rxid=3c44ab37-4535-42f0-b8bc-2f13926a5add. Accessed 15 February 2015
Stegmayr B, Asplund K (2003) Improved survival after stroke but unchanged risk of incidence. Lakartidningen 100:3492–3498
Uijen AA, van de Lisdonk EH (2008) Multimorbidity in primary care: prevalence and trend over the last 20 years. Eur J Gen Pract 14(Suppl 1):28–32
Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M (2009) Defining comorbidity: implications for understanding health and health services. Ann Fam Med 7:357–363
Verbrugge LM, Jette AM (1994) The disablement process. Soc Sci Med 38:1–14
Walston J et al (2006) Research agenda for frailty in older adults toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc 54:991–1001
Whitson HE, Purser JL, Cohen HJ (2007) Frailty thy name is… Phrailty? J Gerontol Biol Sci Med Sci 62:728–730
Acknowledgments
This work was supported by the Swedish Council for Working Life and Social Research (FAS) (grant number 2010-0583).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Additional information
Responsible editor: D.J.H. Deeg.
Rights and permissions
About this article
Cite this article
Meinow, B., Kåreholt, I., Thorslund, M. et al. Complex health problems among the oldest old in Sweden: increased prevalence rates between 1992 and 2002 and stable rates thereafter. Eur J Ageing 12, 285–297 (2015). https://doi.org/10.1007/s10433-015-0351-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10433-015-0351-2