Abstract
Periprosthetic joint infection (PJI) is one of the severe complications of prosthetic joint replacement. Delayed PJI diagnosis may anchor bacteria in periprosthetic tissues, and removal of the prosthesis might be inevitable. The diagnosis of PJI depends on the identification of microorganisms by standard microbiological cultures or more advanced molecular diagnostic methods for detection of bacterial genes. However, these methods are relatively time-consuming, labor-intensive and not human error-free. Moreover, it is challenging to distinguish live from dead bacteria by using DNA-based molecular diagnostics since bacterial DNA will be remained in the tissue even after the death of the bacteria. In this work, an integrated microfluidic system has been developed to perform the entire molecular diagnostic process for the PJI diagnosis in a single chip. We combined the loop-mediated isothermal amplification (LAMP) with ethidium monoazide (EMA) in an integrated microfluidic system to identify live bacteria with reasonable sensitivity and high specificity. All the diagnostic processes including bacteria isolation, cell lysis, DNA amplification and optical detection can be automatically performed on the integrated microfluidic system by using a compact custom-made control system. The integrated system can accommodate four primers complementary to six regions of the target genes and improve the detection limit by using LAMP. The limit of detection in this multiple EMA-LAMP assay could be as low as 5 fg/reaction (~1 CFU/reaction) when choosing an optimized primer set as we demonstrated in mecA gene detection. Thus, the developed system for PJI diagnosis has great potential to become a point-of-care device.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Periprosthetic joint infection (PJI) is one of the most severe complications of prosthetic joint replacement. Incidence rate of PJI in total joint arthroplasties (TJA) is between 1 and 12% (Barrack et al. 1995; Pulido et al. 2008; Qu et al. 2013). In recent years, as the number of TJA performed has been increasing, the number of PJI patients has been rising accordingly (Kurtz et al. 2007). It was estimated that there will be 420 thousands of patients who may suffer from PJI in the USA in 2030, and the costs of PJI in the USA could be surmised to be $1.62 billion in 2020 (Kurtz et al. 2007, 2012; Schairer et al. 2014). The treatment expenses of arthroplasty have a huge financial burden for both patients and medical facilities (Jafari et al. 2010; Kapadia et al. 2016; Shahi and Parvizi 2015; Stranges et al. 2009). Patients with inadequate treatments may suffer from many disabilities complicated with sinus discharge, joint dislocation, joint effusion and purulence on the joint (Parvizi et al. 2011; Paxton et al. 2015).
The most common microorganisms leading to PJI is Staphylococcus aureus (S. aureus, SA), which commonly exists in hospitals and healthcare facilities (Pulido et al. 2008; Schairer et al. 2014; Trampuz and Zimmerli 2005). Due to the abuse of antibiotics, the nosocomial infections have been aggravated in the hospitals and nursing homes. Furthermore, some S. aureus has developed a resistance to methicillin, penicillin and β-lactam such that the infections could no longer be treated by using those antibiotics. For instance, methicillin-resistance Staphylococcus aureus (MRSA) is one of the most prevailing pathogens with antibiotics-resistant activities (Baddour et al. 2006; Doebbeling 1995; Levy and Marshall 2004; Pulido et al. 2008; Wang et al. 2011). In addition to these two gram-positive bacteria, there are other common microorganisms such as Escherichia coli (E. coli), Acinetobacter baumannii (A. baumannii), Klebsiella pneumoniae and Pseudomonas aeruginosa that are gram-negative bacteria and have been commonly observed for PJI infections (Lentino 2003; Trampuz and Zimmerli 2005). Supplementary Information Table 1 lists the isolation rate of clinical strains from Kaohsiung Chang Gung Memorial Hospital, Taiwan in 2014. Among them, SA, MRSA, E. coli and A. baumannii are the common bacteria in clinical surgery of PJI in Taiwan. Therefore, it is of great need to develop a tool to detect these four bacteria with high accuracy.
Currently, hospitals manage the PJI by using a staged operation protocol of arthroplasty (Chang et al. 2014; Huang et al. 2012; Lima et al. 2013; Trampuz and Zimmerli 2005). In the staged reimplantation surgery, the first-stage process includes the removal of the infected artificial joint, thorough debridement auxiliary with systemic and local antibiotic therapy (Gallo et al. 2004; Shahi and Parvizi 2015). When the PJI is cured and no live bacteria in the joint are detected, then a new prosthesis could be implanted. Therefore, an accurate PJI diagnosis is critical and essential for the subsequent treatments (Esposito and Leone 2008). There are several diagnostic methods to detect infectious pathogens for PJI in clinical practices, such as cell culture, polymerase chain reaction (PCR) and ribosomal ribonucleic acid (rRNA)-based approaches (Bergin et al. 2010; Esposito and Leone 2008; Gallo et al. 2004; Kapadia et al. 2016; Shahi and Parvizi 2015; Trampuz and Zimmerli 2005). Conventional approaches for PJI diagnosis were based on the cultures from joint fluids or tissues (Alijanipour et al. 2013; Hartley and Harris 2014). However, it could take 3–7 days to get the final bacteriological report such that a decision for the choice of antibiotics could only be made accurately. The inaccuracy rate (false-positive and false-negative) is also relatively high for these above-mentioned approaches. For instance, the contamination between the samples may cause serious false-positive results. Furthermore, deoxyribonucleic acid (DNA) amplification-based methods for PJI diagnosis cannot distinguish live from dead bacteria because the DNA of dead bacteria remains intact and can be amplified to get a false-positive result (Jacovides et al. 2012; Vandercam et al. 2008; Josephson et al. 1993). Other methods including radionuclide scans suffer from their low-resolution characteristics, lack of specificity and thus false-negative issues remain a concern (Fernandez-Suarez and Ting 2008; Kherlopian et al. 2008).
One group has developed an integrated microfluidic system for fast PJI diagnosis (Chang et al. 2014). It employed EMA with the PCR to detect live bacteria. EMA, a DNA-staining dye, can penetrate into the broken cell walls of dead bacteria and intercalate into double-stranded DNA (dsDNA) to prevent DNA from denaturation in PCR. With this approach, all the diagnostic process (bacteria isolation, cell lysis, DNA amplification and optical detection) could be automatically performed on the integrated microfluidic chip. In the current work, we aim to increase the specificity and sensitivity of the detection by using loop-mediated isothermal amplification (LAMP) since the sensitivity of LAMP is one order of magnitude higher than PCR (Soo et al. 2013) and the specificity of LAMP could be enhanced by increasing the primer sets. Furthermore, isothermal reaction of LAMP may alleviate the requirement for thermocycling, which is commonly used for PCR. Moreover, a compact custom-made control system and a compact pneumatic supply were developed in this work such that the developed system may be used for point-of-care applications. It is the first time that LAMP with EMA has been demonstrated in an integrated microfluidic system to diagnose live bacteria for PJI automatically. Furthermore, four common bacteria found in PJI could be distinguished and detected in this work. When compared to the previous works (Chang et al. 2014, 2015) which used EMA and PCR assays, this new system is lighter (27.0 vs. 41.5 kg) and smaller (42.0 cm × 33.0 cm × 47.0 cm vs. 46.0 cm × 35.0 cm × 47.0 cm) which makes it more feasible for bedside examination. Moreover, the air supply modules were also integrated into a small box, allowing for easy experimental setup. Furthermore, the new system exhibited higher specificity (i.e., LAMP reaction will be carried out successfully only when all four primers are exactly complementary to six regions of the target gene) and higher sensitivity (i.e., the detection limit of the multiple EMA-LAMP assay could be as low as 1 CFU/reaction when choosing an optimized primer set as we demonstrated in mecA gene detection, which is two orders of magnitude better than the previous work (~102 CFU/reaction)). More importantly, the strain of S. aureus with antibiotic resistance could also be distinguished by using the mecA primer sets such that MRSA could be detected, which may provide important information for antibiotics-resistant treatment.
2 Materials and methods
2.1 Experimental procedure
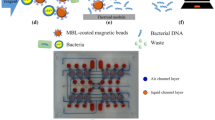
Figure 1 illustrates the experimental processes for the detection of live bacteria in human joint fluids performed on the integrated microfluidic system. The experimental procedures are described briefly as follows. First, the EMA was added to the samples to covalently bind to the DNA of dead bacteria and magnetic beads coated with vancomycin were then used to capture the bacteria (both live and dead bacteria) (Chang et al. 2014). Note that EMA can penetrate into the broken cell walls of dead bacteria and cause irreversible intercalation in dsDNA such that it cannot be served as templates in subsequent LAMP process. The detail information for photoactivation of EMA could be found in our previous work (Chang et al. 2014). Furthermore, vancomycin-coated beads have been demonstrated to exhibit excellent capability to capture gram-positive and gram-negative bacteria (Wang et al. 2014). Then, a permanent magnet was placed under the microfluidic chip to collect bacteria–magnetic beads complexes by applying a magnetic field (~500 Gauss) for 4 min. Furthermore, the waste unit was applied with a negative gauge pressure (suction force) to suck out the unbound debris. Note that this process is crucial since it allows one to isolate bacteria from complicate clinical samples such that the subsequent processes such as LAMP could be performed with high yield (Chang et al. 2014). Next, after removing the magnet, a temperature control module (FTC100D, Accuthermo Technology Corp., USA) and a thermoelectric (TE) cooler (TEC1-241.10, TANDE Corp., Taiwan) were used to perform the cell lysis process at 95 °C for 4 min. Then, the LAMP reagent was transported to the LAMP reaction chamber, followed by performing the LAMP process at 60 °C for 55 min by using the same temperature control module. Note that the sample and reagents were automatically transported and regulated by using built-in micropumps and microvalves (Chang et al. 2014). Finally an optical detection module was used to detect the fluorescent signals of LAMP products.
A schematic illustration of the entire experimental process for detection of live bacteria for PJI diagnosis. a EMA was added, and bacteria were captured by magnetic beads coated with vancomycin. b Bacteria-magnetic beads complexes were collected by applying an external magnetic field. c The debris was removed. d Cell lysis was performed to release DNA from bacteria. d Transportation of LAMP reagent. f Amplification of LAMP process
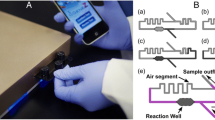
2.2 Design and fabrication of integrated microfluidic chip
An integrated microfluidic chip was fabricated by using a hot-embossing process provided from the Jabil Circuit Inc., Ltd., Taichung, Taiwan. It was composed of two silica gel layers and a glass substrate (Fair & Cheer Inc., Taiwan) (Chang et al. 2014). A schematic illustration of the integrated microfluidic chip is shown in Fig. 2a. It was consisted of several open chambers (including “sample + beads + EMA” chambers, positive control chambers, negative control chambers, LAMP reagent chambers and wash chambers), normally closed microvalves, micropumps and a waste unit. An exploded view of the integrated microfluidic chip is shown in Fig. 2b, which is composed of two silica gel layers and a glass substrate. A photograph of the integrated microfluidic chip is shown in Fig. 2c. The dimensions of the integrated microfluidic chip were measured to be 75.0 mm × 59.0 mm × 6.8 mm (length × width × height). Note that there are four identical modules in this chip such that we may perform positive control (P), negative control (N) and four sample detections (S) (see Fig. 2a). The detail information about the performance and characterization of micropumps and micromixers could be found in our previous work (Chang et al. 2014).
a A schematic illustration of the integrated microfluidic chip. It was composed of several open chambers (including sample + beads + EMA chambers, positive control chambers, negative control chambers, LAMP reagent chambers and wash chambers), normally closed microvalves, micropumps and a waste unit. b An exploded view of the integrated microfluidic chip, which is consisted of two silica gel layers and one glass substrate. c A photograph of the integrated microfluidic chip. The dimensions of the integrated microfluidic chip were measured to be 75.0 mm × 59.0 mm × 6.8 mm (length × width × height). The orange color represents the air channel layer, and the green color indicates the liquid channel layer and chambers (color figure online)
2.3 Experimental setup
As shown in Supplemental Figure 1, the experimental setup was composed of a compact pneumatic supply, a custom-made control system and a computer. This custom-made control system was composed of a flow control module, a temperature control module and an optical detection module. The flow control module was equipped with electromagnetic valves (EMVs, SR 310M5, CHELIC CORP., LTD., Taiwan) and flow regulators (RVUM, PISCO Inc., USA). The temperature control module was equipped with a thermoelectric (TE) cooler, a thermocouple and a temperature controller (FTC100D, Accuthermo Technology Corp., USA). The optical detection module was composed of a laser (MBL-III-473, CNI Corp., China), a band-pass filter (ET525/20 m, Chroma Technology Corp., USA) and a linear polarizing glass filter (#43-786, Edmund Optics Inc., USA) to filter and transmit the laser beam, a dichroic mirror (T495LP, Chroma Technology Corp., USA) to reflect and transmit the light with specific wavelengths separately, and a photomultiplier tube (PMT, R928, Hamamatsu Corp., Japan) to collect the fluorescent signals from LAMP products. It makes the whole diagnosis system to be more compact in size such that it may have great potential to be a point-of-care device. In this work, all the experimental process could be performed automatically by using the computer to activate the control system and the compact pneumatic supply such that temperature and fluid in this integrated microfluidic chip could be automated and regulated. Furthermore, the LAMP products could be optically detected by using the optical detection module.
A photograph of the working platform of the custom-made control system is shown in Supplemental Figure 2. The dimensions of the system were measured to be 42.0 cm × 33.0 cm × 47.0 cm (length × width × height), and the weight was only 27.0 kg, which is much lighter than the previous one (41.5 kg) (Chang et al. 2014). With this approach, the entire diagnostic process including EMA treatment, bacteria isolation, cell lysis, DNA amplification and optical detection can be automatically performed on the integrated microfluidic system.
A schematic illustration of the compact pneumatic supply is further shown in Supplemental Figure 3(a). The dimensions of the compact pneumatic supply were measured to be 23.0 cm × 13.5 cm × 13.5 cm (length × width × height). It was composed of a vacuum pump (DC-16V, UNi-CROWN CO., LTD., Taiwan) for providing negative gauge pressure to actuate the micropumps, normally closed microvalves and the suction unit, a compressor (TC-10, Sun Mines Electrics Co., Ltd., Taiwan) for supplying the positive gauge pressure to control a shutter of the optical detection module, the magnet, the micropumps and normally closed microvalves, if necessary. It was also equipped with a pressure regulator (NR100-01, CHELIC CORP., LTD., Taiwan) for the compressor and another pressure regulator (IRV10, SMC Inc., Japan) for the vacuum pump to control the output pressure. Furthermore, two pressure sensors (the one for the compressor was from Delta Electronics, Inc., Taiwan and the one for the vacuum pump was from Guanjing ENTERPRISE CO., LTD., Taiwan) were used to measure the output pressure.
2.4 Preparation of EMA
EMA (Molecular Probes, Inc., USA) was dissolved in 99% ethanol (Sigma-Aldrich Co., USA) to a final concentration of 1 mg/mL for the subsequent experiments. Furthermore, the EMA solution was stored at −20 °C and was kept in the dark microcentrifuge tube to prevent from light exposure prior to usage. The shelf life of EMA was measured to be about 6 months. Note that EMA is potentially carcinogenic and mutagenic (Nogva et al. 2003). Therefore, it should be used with caution as any other DNA chelating agents.
2.5 Preparation of bacterial samples
The clinical human joint fluidic samples were provided from Kaohsiung Chang Gung Memorial Hospital, Taiwan under the approval of Institutional Review Board (Nos. 103-6831B, 104-7148C and 104-2206C).
2.6 Preparation of LAMP primers and LAMP reagents
The LAMP reagent mixtures contained a DNA amplification kit (Eiken Chemical Co., Ltd., Japan), double-distilled water (ddH2O, 19 μL), 10 pM B3 primers and F3 primers, 60 pM backward inner primer (BIP) and forward inner primer (FIP) (Sigma-Aldrich Co., USA), 1 μL fluorescent detection reagent (Eiken Chemical Co., Ltd., Japan) and 5 μL of the template. Note that the volume of total reaction mixtures is 25 μL. The reagent chambers corresponding to S chambers in Fig. 2a were first preloaded with 22 μL of LAMP reagent mixtures without the template. Similarly, the reagent chambers corresponding to P chambers in Fig. 2a were preloaded with 25 μL of LAMP reagent mixtures and 5 μL of template (500 pg plasmid DNA). Similarly, the reagent chambers corresponding to N chambers in Fig. 2a were preloaded with 25 μL of LAMP reagent mixtures without DNA templates. Note that the sequences of F3, B3, FIP and BIP primers of four primer sets are listed in Supplementary Information Table 2. The spa primers and Ab-ITS primers could be found in the previous studies (Soo et al. 2013; Wang et al. 2011). The mecA primers were designed by selecting the conserved sequence region among the Accession Nos. KC243787, GU227428 and EF190335 from the GenBank at the National Center for Biotechnology Information (NCBI), and redesigned it to appropriate sequences. Similarly, the EcoUspA primers were also designed by selecting the conserved sequence region among the Accession Nos. CP015832, CP015831, CP015074 and CP015138 form the GenBank at NCBI and redesigned it to appropriate sequences.
2.7 Experimental process performed on integrated microfluidic chip
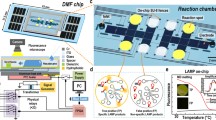
The entire experimental process for the detection of live bacteria in human joint fluids performed on the integrated microfluidic system is shown schematically in Fig. 3. The left column in this figure schematically illustrates the experimental procedures, and the right column shows the corresponding experimental procedures performed on the integrated microfluidic chip. The experimental procedures are briefly described as follows. First, 34 μL of clinical samples (human joint fluids) mixed with 5 μL of vancomycin-coated magnetic beads (30 × 109 beads/mL) and 1 μL of EMA (1 mg/mL), 120 μL of wash buffer (ddH2O) and 25 μL of LAMP reagent with 30 μL of mineral oil (Sigma-Aldrich Co., USA) were first preloaded into the corresponding reagent chambers (S, W and LR chambers in Fig. 2). Note that the mineral oil was added to prevent evaporation during the LAMP reaction. Furthermore, reagents for positive control and negative control cases were preloaded to the corresponding reagent chambers (P and N chambers in Fig. 2). Then, the magnet was placed under the chip to collect bacteria–magnetic beads complexes by applying an external magnetic field for 4 min after the incubation process by activating the micromixer. Furthermore, the waste unit was applied with a negative gauge pressure (4 psi) to suck out the unwanted debris while activating the micropumps to transport the wash buffer. After removing the magnet, the temperature control module was used to thermally perform the cell lysis process at 95 °C for 4 min. Then, the LAMP reagent was transported to the corresponding reaction chamber, followed by the LAMP reaction performed at 60 °C for 55 min. After isothermal DNA amplification, the optical detection module was used to detect the fluorescent signals form calcein which was intercalated in the LAMP product. Note that four kinds of bacteria could be detected by using designed primers in this work.
A schematic illustration of the entire experimental process performed on the integrated microfluidic chip for PJI diagnosis. a In the first step, the bacteria-contained sample was mixed and captured with vancomycin-coated magnetic beads and EMA treatment was performed to bind covalently to DNA in cells that have compromised membranes to eliminate the following LAMP amplification. b Bacteria–magnetic beads complexes can be collected by applying an external magnetic field. c The unbound debris was removed by activating micropumps, and the remaining fraction was washed with PBS buffer and ddH2O from the buffer reservoir chamber. d Cell lysis was executed on a heating block which was placed under the reaction chambers at 95 °C to release DNA from bacteria. e LAMP process was performed by controlling the temperature at 60 °C for the heating central area after transporting all the LAMP reagent to the central chamber. f Fluorescent signal was induced and collected by using an optical module which comprised a laser and a PMT detector
2.8 Internal control of LAMP diagnostic assay
Isothermal amplification of the 16S rRNA of tested bacterial strains was used as internal control in the developed microfluidic diagnostic assay since it could be used as an indication for bacterial infections. The sequences for universal 16S rRNA LAMP primer pairs were designed by PrimerExplorer V4 software in the Eiken Genome Site (https://primerexplorer.jp/e/) and listed on Supplemental Information Table 3. A total reaction volume of 30 μL contained 3.3 μM of each FIP and BIP primer, 0.3 μM of each F3 and B3 primer, 2 μL of dNTPs (10 μM, Promega, USA), 3 μL of 10× thermo-polymerase buffer (with 200 μM tris–HCl, 100 μM KCl, 100 μM (NH4)2SO4, 20 μM MgSO4 and 0.1% Triton X-100 (pH 8.8) at 25 °C), 100 ng of bacterial genomic DNA, 3 μL of ddH2O and 2 μL of 8 U Bst DNA polymerase (large fragment; New England Biolabs Inc., USA). Finally, the LAMP products were visualized on 2% agarose gels stained with ethidium bromide (EtBr, 50 mg mL−1, Sigma, USA), followed by image acquisition utilizing an ultraviolet (UV) analysis system (302 nm, BioDoc-It™ imaging system, UVP, Canada).
3 Results and discussion
3.1 Universal 16S rRNA LAMP detection
As mentioned previously, 16S rRNA could be used for detection of bacterial infections. The Supplemental Information Figure 4 showed that all of tested bacteria in this study, including A. baumannii, CNS, E. coli, S. aureus and MRSA could be amplified successfully by observing ladder LAMP products. In addition, Enterococci (Ent), vancomycin-intermediate Staphylococcus aureus (VISA) and vancomycin-resistant enterococci (VRE) could be also amplified successfully to generate LAMP products. Therefore, the universal 16S rRNA LAMP primer pairs were demonstrated to be capable of detecting various bacteria in the LAMP diagnostic assay.
3.2 Limit of detection
The limit of detection (LOD) of the developed EMA-LAMP assay was further explored, and the results were shown in Fig. 4. Note that gel electropherograms using 2% agarose for the LAMP products of corresponding bacterial genes were also shown for comparison. 10 pg μL−1 (50 pg/reaction) of plasmid DNA was first used to perform serial tenfold dilutions to explore the LOD of mecA primer sets (for MRSA) by using the on-chip LAMP process. The LOD of the mecA gene was experimentally determined to be 1 fg μL−1 (5 fg/reaction, ~1 CFU/reaction), as shown in Fig. 4a. The fluorescent intensities of the positive and negative control cases were measured to be 5.18 ± 0.16 and 1.24 ± 0.11 V, respectively. The standard deviation of all signals was within 17%. Note that two repeated measurements were performed.
LOD tests of the LAMP assay showing LAMP products for mecA, Ab-ITS, spa and EcoUspA primer sets by using fluorescent signals and gel electropherograms. a Lane NC negative control without DNA templates; Lanes 3–8 10-fold serial dilutions of mecA plasmid DNA from 1 pg μL−1 (5 pg/reaction) to 100 ag μL−1 (500 ag/reaction); Lane M 100-bp (base pairs) DNA ladders. The LOD of mecA gene was measured to be 1 fg μL−1 (5 fg/reaction). The fluorescent intensities of the positive control and negative control cases were 5.18 ± 0.16 and 1.24 ± 0.11 V, respectively. The standard deviation of all signals was within 17%. Note that two repeated measurements were performed. b Lane NC negative control without DNA templates. Lanes 3–8 10-fold serial dilutions of A. baumannii genomic DNA from 1 pg μL−1 (5 pg/reaction) to 100 ag μL−1(500 ag/reaction); Lane M 100-bp DNA ladders. The LOD of Ab-ITS gene was measured to be 10 fg μL−1 (50 fg/reaction). The fluorescent intensities of the positive control and negative control cases were 4.82 ± 0.8 and 1.12 ± 0.17 V, respectively. The standard deviation of all signals was within 26%. Note that two repeated measurements were performed. c Lane NC negative control without DNA templates; Lanes 1–5 10-fold serial dilutions of spa plasmid DNA from 1 ng μL−1 (5 ng/reaction) to 100 fg μL−1 (500 fg/reaction); Lane M 100-bp DNA ladders. The LOD of spa gene was measured to be 10 pg μL−1 (50 pg/reaction). The fluorescent intensities for the positive control and negative control cases were 6.48 ± 0.46 and 1.46 ± 0.09 V, respectively. The standard deviation of all signals was within 9%. Note that two repeated measurements were performed. d Lane NC negative control without DNA template; Lanes 1–5 10-fold serial dilutions of EcoUspA plasmid DNA from 1 ng μL−1 (5 ng/reaction) to 100 fg μL−1 (500 fg/reaction); Lane M 100-bp DNA ladders. The LOD of EcoUspA gene was measured to be 10 pg μL−1 (50 pg/reaction). The fluorescent intensities of the positive control and negative control cases were 5.85 ± 0.35 and 1.6 ± 0.05 V, respectively. The standard deviation of all signals was within 4%. Note that two repeated measurements were performed. The confidence level was calculated to be 84%
Similarly, 10 pg μL−1 (50 pg/reaction) of genomic DNA was used to perform serial tenfold dilutions to investigate the LOD of Ab-ITS primer sets (for A. baumannii). The LOD of the Ab-ITS gene was measured to be 10 fg μL−1 (50 fg/reaction, ~10 CFU/reaction), as shown in Fig. 4b. The fluorescent intensities of the positive and negative control cases were measured to be 4.82 ± 0.8 and 1.12 ± 0.17 V, respectively. The standard deviation of all signals was within 26% for two repeated experiments.
Again, 10 pg μL−1 of plasmid DNA was used to perform serial tenfold dilutions to explore the LOD of spa primer sets (for SA). The LOD of the spa gene was measured to be 10 pg μL−1 (50 pg/reaction, ~104 CFU/reaction), as shown in Fig. 4c. The fluorescent intensities of the positive and negative control cases were measured to be 6.48 ± 0.46 and 1.46 ± 0.09 V, respectively. The standard deviation of all signals was within 9% for two repeated experiments.
Finally, 10 pg μL−1 of plasmid DNA was used to perform serial tenfold dilutions to explore the LOD of EcoUspA primer sets (for E. coli) by using the LAMP process. The LOD of the EcoUspA gene was measured to be 10 pg μL−1 (50 pg/reaction, ~104 CFU/reaction), as shown in Fig. 4d. The fluorescent intensities of the positive and negative control cases were measured to be 5.85 ± 0.35 and 1.6 ± 0.05 V, respectively. The standard deviation of all signals was within 4% for two repeated experiments.
As shown in Fig. 4, gel electropherograms using 2% agarose for LAMP products of these four genes were also shown for comparison. The results were consistent with the fluorescent signals obtained from the optical detection module. It indicates that LAMP for detection of four bacteria in PJI diagnosis could be performed by using the developed microfluidic system. Furthermore, when compared to the traditional PCR process, the LOD of this LAMP multiple assay was one order of magnitude higher than traditional PCR approach (Soo et al. 2013). Moreover, when compared to traditional gel electrophoresis, the fluorescent detection could be performed within 2 min. Note that the difference of LODs among these four primer sets may be due to the fact that the sequences were not optimized and can be further improved through further optimization process.
The reproducibility of this four primer sets was also investigated by using different clinical strains (obtained from Kaohsiung Chang Gung Memorial Hospital, Taiwan and National Yang-Ming University, Taiwan). Specifically, four different strains of E. coli and A. baumannii were used to test the reproducibility of EcoUspA and Ab-ITS primer sets. Similarly, three different strains of MRSA were used to test the reproducibility of spa and mecA primer sets since they exhibited these two gens simultaneously. The electropherogram results of four primer sets for these four genes are shown in Supplemental Information Figure 5. The experimental results showed that four primer sets were reproducible for detecting four target bacteria. Furthermore, the values of LOD regarding each primer sets for four bacteria were further determined by each lowest colony-forming unit (cfu) from serial dilutions of overnight culture (Supplementary Fig. 6).
3.3 EMA for distinguishing dead/alive bacteria
Ethidium monoazide (EMA) is a double-stranded DNA intercalating compound to prevent the amplicon production during PCR process. Furthermore, its characteristic of membrane permeability in cells with compromised membranes has been applied to distinguish the dead and alive bacteria. In this study, the same results and features of the application of EMA in LAMP amplification can be also observed. The released DNA from thermal cell lysis was chelated by EMA, which resulted in a negative signal when compared to these without EMA treatment (Supplementary Fig. 7). The combination of EMA and LAMP to rule out the detection of dead bacteria has a potential to provide a sensitive and precise diagnosis on clinical samples and drug abuse.
3.4 Specificity
The specificity of the LAMP primer sets used in this study corresponding to specific bacteria was further explored. Seven kinds of bacteria strains (including E. coli, A. baumannii, Enterococcus sp., Pseudomonas syringae (P. syringae), S. aureus, MRSA and Coagulase-negative staphylococci (CNS)) were used to perform the specificity tests of the four primer sets that were listed in Supplementary Information Table 2. Note that six kinds of bacteria are common bacteria found in PJI (Chang et al. 2015) and another one (A. baumannii) is the target bacteria in this work. The results for specificity tests of these primer sets are shown in Fig. 5. For instance, the result of EcoUspA primer sets is shown in Fig. 5a. It shows that only the specific gene of E. coli bacteria could be amplified by the LAMP process and there were no amplicons shown for the other six nontargeted bacteria. Similarly, the result of Ab-ITS primer sets is shown in Fig. 5b. Again, only specific gene of A. baumannii bacteria could be amplified after the LAMP process and there were no amplicons shown for the other six nontarget bacteria. The result of spa primer sets is shown in Fig. 5c. Note that due to the fact that the spa primer sets could detect the bacteria with spa gene (including S. aureus and MRSA), both specific genes of S. aureus and MRSA bacteria could be amplified after the LAMP process and there were no amplicons shown for the other five nontargeted bacteria. Similarly, the result of mecA primer sets is shown in Fig. 5d. Again, the mecA primer sets could be detected if the bacteria are drug-resistant (beta-lactam antibiotics). Due to the fact that CNS bacteria have the possibility to exhibit the mecA gene (Tsuji et al. 1998), for these seven bacteria, both genes of MRSA and CNS bacteria could be amplified after the LAMP process and there are no amplicons shown for the other five nontarget bacteria. Again, the electropherogram results were also consistent with the fluorescent signals since there were no amplicons from nontargeted bacteria in gel electropherograms. It therefore indicated high specificity of this four primer sets. With this diagnostic system, the common bacteria found in PJI, such as S. aureus, E. coli and A. baumannii, could be successfully detected. Furthermore, it could provide important information for the clinicians to prescribe the most suitable antibiotics treatment (for MRSA).
Specificity tests of four primer sets for LAMP process. Lane M 100-bp DNA ladders; Lane NC negative control without DNA templates; Lane 1 E. coli; Lane 2 A. baumannii; Lane 3 Enterococcus sp.; Lane 4 P. syringae: Lane 5 S. aureus; Lane 6 MRSA; Lane 7 CNS. a EcoUspA primer sets: only specific gene of E. coli bacteria (EcoUspA) could be amplified by the LAMP process. b Ab-ITS primer sets: only specific gene of A. baumannii bacteria (Ab-ITS) could be amplified by the LAMP process. c Spa primer sets: both specific genes of S. aureus and MRSA bacteria (spa and mecA) could be amplified by the LAMP processes. d MecA primer sets: both specific genes of MRSA and CNS bacteria could be amplified by the LAMP process
3.5 Spiked sample tests
The spiked samples were then used to verify the performance of developed EMA-LAMP assay such that we may evaluate if it could be used for clinical applications in the near future. Figure 6 shows that the spiked samples (A. baumannii with clinical human joint fluids) could be successfully detected on the integrated microfluidic system. Briefly, 10 μL of overnight cultured A. baumannii (12,860,000 CFU) was spiked into 24 μL of clinical samples (join fluids) with 1 μL of EMA and 5 μL of vancomycin-coated beads in this test. The fluorescent intensity of the positive control and negative control cases was measured to be 5.41 and 1.68 V, respectively, while the fluorescent signal for the spiked sample was 4.73 V. Note that the gel electropherogram using 2% agarose shows the consistent results with the fluorescent signals. The entire process including bacteria isolation, cell lysis, DNA amplification and optical detection can be automatically performed on the integrated microfluidic system by using a compact custom-made control system.
On-chip fluorescent signals and gel electropherograms of the EMA-LAMP assay for spiked sample tests. Lane NC negative control without DNA template, Lane P positive control, Lane S sample reaction. Lane M 100-bp DNA ladders. The relative intensity of the positive control reaction was about 5.41 V, while the sample reaction was about 4.73 V and the negative control without DNA template reaction was about 1.68 V
4 Conclusions
Accurate and timely diagnosis of live bacteria is critical for the treatment of PJI. In this study, an integrated microfluidic system for live bacteria detection in PJI has been demonstrated. With this multiple EMA-LAMP assay, the entire processes including bacteria isolation, cell lysis, DNA amplification and optical detection could be automatically operated on the developed system automatically. This is the first time that LAMP with EMA has been demonstrated in an integrated microfluidic system to diagnose PJI. Compared to the conventional PCR process, the LOD in this multiple LAMP assay could be as low as 5 fg–50 pg. Furthermore, the universal 16S rRNA LAMP assay was used for detection of bacterial infections. More importantly, the drug-resistant characteristic of S. aureus could also be distinguished by using the mecA primer sets. The developed microfluidic system has great potential to become a powerful platform for the clinical practice in near future.
Abbreviations
- A. baumannii :
-
Acinetobacter baumannii
- BIP:
-
Backward inner primer
- bp:
-
Base pairs
- CNS :
-
Coagulase-negative staphylococci
- DNA:
-
Deoxyribonucleic acid
- dsDNA:
-
Double-stranded DNA
- ddH2O:
-
Double-distilled water
- E. coli :
-
Escherichia coli
- EMA:
-
Ethidium monoazide
- EMVs:
-
Electromagnetic valves
- FIP:
-
Forward inner primer
- LAMP:
-
Loop-mediated isothermal amplification
- LOD:
-
Limit of detection
- MRSA:
-
Methicillin-resistance Staphylococcus aureus
- NCBI:
-
National Center for Biotechnology Information
- P. syringae :
-
Pseudomonas syringae
- PJI:
-
Periprosthetic joint infection
- PCR:
-
Polymerase chain reaction
- PMT:
-
Photomultiplier tube
- rRNA:
-
Ribosomal ribonucleic acid
- SA:
-
Staphylococcus aureus
- TE:
-
Thermoelectric
- TJA:
-
Total joint arthroplasties
- VISA:
-
Vancomycin-intermediate Staphylococcus aureus
References
Alijanipour P, Bakhshi H, Parvizi J (2013) Diagnosis of periprosthetic joint infection: the threshold for serological markers. Clin Orthop Relat Res 471:3186–3195
Baddour MM, AbuElKheir MM, Fatani AJ (2006) Trends in antibiotic susceptibility patterns and epidemiology of MRSA isolates from several hospitals in Riyadh, Saudi Arabia. Ann Clin Microbiol Antimicrob 5:30
Barrack RL, Hoffman GJ, Tejeiro WV, Carpenter LJ (1995) Surgeon work input and risk in primary versus revision total joint arthroplasty. J Arthroplasty 10:281–286
Bergin PF, Doppelt JD, Hamilton WG, Mirick GE, Jones AE, Sritulanondha S, Helm JM, Tuan RS (2010) Detection of periprosthetic infections with use of ribosomal RNA-based polymerase chain reaction. J Bone Joint Surg Am 92A:654–663
Chang WH, Wang CH, Yang SY, Lin YC, Wu JJ, Lee MS, Lee GB (2014) Rapid isolation and diagnosis of live bacteria from human joint fluids by using an integrated microfluidic system. Lab Chip 14:3376–3384
Chang WH, Wang CH, Lin CL, Wu JJ, Lee MS, Lee GB (2015) Rapid detection and typing of live bacteria from human joint fluid samples by utilizing an integrated microfluidic system. Biosens Bioelectron 66:148–154
Doebbeling B (1995) The epidemiology of methicillin-resistant Staphylococcus aureus colonisation and infection. J Antimicrob Chemother 7:99–103
Esposito S, Leone S (2008) Prosthetic joint infections: microbiology, diagnosis, management and prevention. Int J Antimicrob Agents 32:287–293
Fernandez-Suarez M, Ting AY (2008) Fluorescent probes for super-resolution imaging in living cells. Nat Rev Mol Cell Biol 9:929–943
Gallo J, Raska M, Dendis M, Florschuetz AV, Kolar M (2004) Molecular diagnosis of prosthetic joint infection. A review of evidence. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 148:123–129
Hartley JC, Harris KA (2014) Molecular techniques for diagnosing prosthetic joint infections. J Antimicrob Chemother 69:21–24
Huang R, Hu CC, Adeli B, Mortazavi J, Parvizi J (2012) Culture-negative periprosthetic joint infection does not preclude infection control. Clin Orthop Relat Res 470:2717–2723
Jacovides CL, Kreft R, Adeli B, Hozack B, Ehrlich GD, Parvizi J (2012) Successful identification of pathogens by polymerase chain reaction (PCR)-based electron spray ionization time-of-flight mass spectrometry (ESI-TOF-MS) in culture-negative periprosthetic joint infection. J Bone Joint Surg Am 94:2247–2254
Jafari SM, Coyle C, Mortazavi SM, Sharkey PF, Parvizi J (2010) Revision hip arthroplasty: infection is the most common cause of failure. Clin Orthop Relat Res 468:2046–2051
Josephson KL, Gerba CP, Pepper IL (1993) Polymerase chain reaction detection of nonviable bacterial pathogens. Appl Environ Microbiol 59:3513–3515
Kapadia BH, Berg RA, Daley JA, Fritz J, Bhave A, Mont MA (2016) Periprosthetic joint infection. Lancet 387:386–394
Kherlopian AR, Song T, Duan Q, Neimark MA, Po MJ, Gohagan JK, Laine AF (2008) A review of imaging techniques for systems biology. BMC Syst Biol 2:74–91
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89:780–785
Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J (2012) Economic burden of periprosthetic joint infection in the United States. J Arthroplasty 27:61–65
Lentino JR (2003) Prosthetic joint infections: bane of orthopedists, challenge for infectious disease specialists. Clin Infect Dis 36:1157–1161
Levy SB, Marshall B (2004) Antibacterial resistance worldwide: causes, challenges and responses. Nat Med 10:S122–S129
Lima AL, Oliveira PR, Carvalho VC, Saconi ES, Cabrita HB, Rodrigues MB (2013) Periprosthetic joint infections. Interdiscip Perspect Infect Dis 2013:542796
Nogva HK, Dromtorp SM, Nissen H, Rudi K (2003) Ethidium monoazide for DNA-based differentiation of viable and dead bacteria by 5′-nuclease PCR. Biotechniques 34:804–813
Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG (2011) New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res 469:2992–2994
Paxton EW, Inacio MC, Singh JA, Love R, Bini SA, Namba RS (2015) Are there modifiable risk factors for hospital readmission after total hip arthroplasty in a US healthcare system? Clin Orthop Relat Res 473:3446–3455
Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J (2008) Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res 466:1710–1715
Qu X, Zhai Z, Li H, Liu X, Zhu Z, Wang Y, Liu G, Dai K (2013) PCR-based diagnosis of prosthetic joint infection. J Clin Microbiol 51:2742–2746
Schairer WW, Vail TP, Bozic KJ (2014) What are the rates and causes of hospital readmission after total knee arthroplasty? Clin Orthop Relat Res 472:181–187
Shahi A, Parvizi J (2015) Prevention of periprosthetic joint infection. Arch Bone Joint Surg 3:72–81
Soo PC, Tseng CC, Ling SR, Liou ML, Liu CC, Chao HJ, Lin TY, Chang KC (2013) Rapid and sensitive detection of Acinetobacter baumannii using loop-mediated isothermal amplification. J Microbiol Methods 92:197–200
Stranges E, Russo CA, Friedman B (2009) Procedures with the most rapidly increasing hospital costs, 2004–2007: statistical brief #82. In: Healthcare cost and utilization project (HCUP) statistical briefs [Internet]. Agency for Healthcare Research and Quality, Rockville, MD, US. https://www.ncbi.nlm.nih.gov/books/NBK53597/. Accessed 18 Apr 2017
Trampuz A, Zimmerli W (2005) Prosthetic joint infections: update in diagnosis and treatment. Swiss Med Wkly 135:243–251
Tsuji H, Tsuru T, Okuzumi K (1998) Detection of methicillin-resistant Staphylococcus aureus in donor eye preservation media by polymerase chain reaction. Jpn J Ophthalmol 42:352–356
Vandercam B, Jeumont S, Cornu O, Yombi JC, Lecouvet F, Lefevre P, Irenge LM, Gala JL (2008) Amplification-based DNA analysis in the diagnosis of prosthetic joint infection. J Mol Diagn 10:537–543
Wang CH, Lien KY, Wu JJ, Lee GB (2011) A magnetic bead-based assay for the rapid detection of methicillin-resistant Staphylococcus aureus by using a microfluidic system with integrated loop-mediated isothermal amplification. Lab Chip 11:1521–1531
Wang CH, Chang CJ, Wu JJ, Lee GB (2014) An integrated microfluidic device utilizing vancomycin conjugated magnetic beads and nanogold-labeled specific nucleotide probes for rapid pathogen diagnosis. Nanomedicine 10:809–818
Acknowledgements
This work was financially supported by Chang Gung Memorial Hospital in Taiwan (CMRPG3C0231; CMRPG8E1631) and “Towards a World-Class University” Project (104N2751E1). Partial financial support from Ministry of Science and Technology, Taiwan is also greatly appreciated (104-2119-M-007-009, 104-2811-E-007-031 and 104-2221-E-007-141).
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, SL., Chang, WH., Wang, CH. et al. An integrated microfluidic system for live bacteria detection from human joint fluid samples by using ethidium monoazide and loop-mediated isothermal amplification. Microfluid Nanofluid 21, 87 (2017). https://doi.org/10.1007/s10404-017-1913-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10404-017-1913-8