Abstract
Purpose
Testicular torsion requires emergency surgery; thus, prompt and correct diagnosis is very important. Ultrasound with color Doppler is usually the first-choice modality for diagnosis; however, skill and experience are required for confident diagnosis. Recently, contrast-enhanced ultrasound for the diagnosis of testicular torsion has been reported, but there have been only a few reports. This study aimed to compare contrast-enhanced ultrasound findings in cases of testicular torsion and non-testicular torsion.
Methods
Patients who underwent contrast-enhanced ultrasound for acute scrotum at our institution between April 2010 and January 2023 were divided into testicular torsion (n = 17) and non-testicular torsion (n = 16) groups. The respective contrast-enhanced ultrasound findings were retrospectively examined and compared.
Results
In 16 out of 17 cases of testicular torsion, the parenchyma of the affected testis was not enhanced. In the remaining case, reduced contrast enhancement was observed; however, it was still notably less than that observed on the unaffected testis. On the other hand, in all cases of non-testicular torsion (n = 16), the parenchyma of the affected testis was notably enhanced.
Conclusion
Contrast-enhanced ultrasound is considered an easy and accurate method for diagnosing testicular torsion.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Among acute scrotal diseases, testicular torsion requires emergency surgery; thus, prompt and correct diagnosis is important. High-frequency ultrasound with color Doppler is usually the first-choice diagnostic modality for testicular torsion. However, even if color Doppler demonstrates blood flow in the testicular vasculature, testicular torsion cannot be ruled out [1,2,3], because even if the spermatic vein is compressed and congestive necrosis progresses, the testicular artery can still deliver blood, albeit little. On the other hand, children, in particular, have low blood flow velocities in the testis; therefore, it is sometimes difficult to display blood flow with color Doppler, even in normal testes. Therefore, it relies on the skill and experience of the examiner to determine whether a finding that appears to be blood flow is merely an artifact or weak true blood flow.
In recent years, contrast-enhanced ultrasound has been used to diagnose liver and breast tumors, and its efficacy and safety have been recognized [4, 5]. This method has the unique advantage of visualizing microcirculatory perfusion and very low-velocity blood flow in fine microcirculatory vessels. Contrast-enhanced ultrasound is also used for the diagnosis of testicular torsion, but there have been only a few reports on this technique [6, 7]. Furthermore, there have been no reports comparing contrast-enhanced ultrasound findings of testicular torsion and non-testicular torsion.
This study aimed to compare ultrasound findings, including contrast-enhanced ultrasound findings, in cases of testicular torsion with those of non-testicular torsion.
Materials and methods
This study was approved by the Japanese Red Cross Society Himeji Hospital Institutional Review Board (2022–22) and complied with the Health Insurance Portability and Accountability Act. All procedures were performed in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from patients ≥ 18 years of age or from the legal guardians of patients aged < 18 years.
The participants in this study were patients who underwent contrast-enhanced ultrasound for acute scrotum at our institution between April 2010 and January 2023. Only patients with scrotal pain, indicating “acute scrotum” at the time of contrast-enhanced ultrasound, were included in this study. Patients with no scrotal pain at the time of the contrast-enhanced ultrasound were excluded. The ultrasound technician or the attending physician decided whether to perform contrast-enhanced ultrasound in addition to the common ultrasound examination. These patients were divided into testicular torsion and non-testicular torsion groups, and their respective ultrasound findings (including color Doppler and contrast-enhanced ultrasound findings) were examined retrospectively. Artifacts were considered as a color signal in this study because the echo images were evaluated retrospectively, and it was impossible to determine whether the color signal was due to actual blood flow or an artifact.
Ultrasonographic technique
Ultrasound was performed in all patients in the ultrasound room using the Aplio-XG system, Aplio-500, or Aplio-i800 device (Canon Medical Systems, Tokyo, Japan) with a linear array ultrasound transducer. During the examination, the patients were placed in the supine position. Swelling of the testis, peripheral edema, and internal echogenicity were observed with high-frequency ultrasound in B mode. The sampling frame was then adjusted to a low-velocity scale, and multiple locations on the bilateral testes were scanned using high-frequency color Doppler ultrasound.
Contrast-enhanced ultrasound technique
When contrast-enhanced ultrasound was performed, the Contrast Harmonic Imaging mode was used (the mechanical index was set at 0.2–0.3). The contrast agent, perflubutane microbubbles (Sonazoid; Daiichi Sankyo, Chuo-ku, Tokyo), was suspended in 16 μL (one vial) with 2 mL of water for injection. In general, the recommended clinical dose for imaging is 0.015 mL encapsulated gas per kilogram of body weight. Approximately half of the recommended dose [8, 9] was administered as a bolus and appropriately flushed with saline in this study. The degree of contrast in the parenchyma of the testes was scanned without interruption for approximately 5 min after contrast agent administration. Written informed consent was obtained from the patients before performing contrast-enhanced ultrasound.
Statistical analysis
Data were analyzed using Statcel-Useful Addin Forms on Excel-4th ed. (OMS Co., Ltd., Tokyo, Japan). The chi-square test was used for independent variables, and the Mann–Whitney U test was used for continuous variables. Differences were considered statistically significant at p ≤ 0.05.
Results
During the relevant period, 33 patients with acute scrotum underwent contrast-enhanced ultrasound. All the patients underwent the aforementioned ultrasound procedures. Among these were 17 cases of testicular torsion, designated as the torsion group. All patients with testicular torsion underwent emergency surgery immediately after diagnosis, and the diagnosis of testicular torsion was confirmed. Fourteen of the 17 patients with testicular torsion were diagnosed with complete necrosis of the testis during the operation and underwent excision of the affected testis. Three patients did not have complete necrosis; their testes were preserved by releasing the torsion, and there was no testicular atrophy after the surgery.
There were 16 cases of non-testicular torsion (11 cases of torsion of the appendix testis, three cases of epididymitis, and two cases of unknown etiology), designated as the non-torsion group. All cases of torsion of the appendix testis could be diagnosed with contrast-enhanced ultrasonography. The diagnosis of torsion of the appendix testis was based on the oval or round heterogeneous structure attached to the testis with no enhancement on contrast-enhanced ultrasound, and the indication for surgery was determined by the surgeon. Surgery was performed in six of the 11 cases of torsion of the appendix testis, and the diagnosis of torsion of the appendix testis was confirmed in all operated cases. In the remaining cases that did not undergo surgery, their symptoms gradually subsided for a few days; therefore, we determined that it was not testicular torsion.
Patient characteristics of the torsion and non-torsion groups are shown in Table 1. The median age at diagnosis was 14.0 years in the torsion group (eight patients were ≥ 16 years of age) and 9.5 years in the non-torsion group (one patient was ≥ 16 years of age). Hence, the torsion group was significantly older. The laterality of the affected testis in the torsion group was right in three cases and left in 14. In the non-torsion group, it was right in 10 cases and left in six. Testicular torsion occurred more frequently on the left side compared with non-testicular torsion. The median time from onset to ultrasound was approximately the same in both groups.
Ultrasound findings for both groups are shown in Table 2. Affected-side testicular swelling was observed in 14 of the 17 patients in the torsion group. On the other hand, not a single case of testicular swelling was observed in the non-torsion group. Therefore, testicular swelling was significantly more common in patients with testicular torsion (sensitivity: 82.4%, specificity: 100%). Regarding the echogenicity of the affected testicular parenchyma, it was homogenous in all cases in the non-torsion group. In contrast, it was heterogeneous in 12 of the 17 cases in the torsion group (sensitivity: 70.6%, specificity: 100%). For the three cases in the torsion group in which the testes were preserved, the internal texture was homogeneous. Peritesticular edema was observed in approximately half of the cases in both groups (sensitivity: 52.9%, specificity: 50.0%).
In seven of the 17 cases in the torsion group, the color Doppler findings of the affected testis demonstrated a reduced color signal, including artifacts, compared to the unaffected testis. In the remaining 10 cases in the torsion group, no color signal was observed. In all cases in the non-torsion group, the color signal was visible, the same as for the unaffected testis. When a reduced color signal or no signal was observed, both the sensitivity and specificity were 100%. Moreover, a reduced color signal was observed in one of the three cases of incomplete necrosis; in the remaining two cases, no color signal was observed.
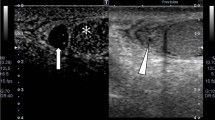
Regarding contrast-enhanced findings of the testicular parenchyma, 16 out of the 17 cases in the torsion group showed that the parenchyma of the testis was not enhanced at all. In the remaining case, reduced contrast enhancement was observed; however, it was still notably less than that of the unaffected testis. On the other hand, the parenchyma of the affected testis was well enhanced in all cases in the non-torsion group. Regarding the contrast effect on healthy testicular parenchyma that could be evaluated, the parenchyma was enhanced clearly in both groups. When reduced or no contrast enhancement was observed, both sensitivity and specificity were 100%. Moreover, reduced contrast enhancement was observed in one of three cases of incomplete necrosis, as with color Doppler. In the remaining two cases, no contrast enhancement was observed. Example cases are shown in Fig. 1a–c. No contrast agent side effects were observed in any patients.
a Non-testicular torsion. Sixteen-year-old boy with left scrotal pain. Contrast-enhanced ultrasound shows that the bilateral testes parenchyma are enhanced to the same degree. Therefore, testicular torsion was negative. Symptoms resolved spontaneously with no treatment. The diagnosis is unknown. b Testicular torsion with necrosis. Fourteen-year-old boy with left scrotal pain for 48 h. Contrast-enhanced ultrasound shows that contrast was not observed in the affected testis parenchyma. On the other hand, contrast is notably observed in the unaffected testis parenchyma. Testicular torsion was diagnosed based on these findings, and an emergency operation was performed. The testis was necrotic and was removed. c Testicular torsion without necrosis. Fourteen-year-old boy with left scrotal pain for 4 h. Contrast Harmonic Imaging mode and normal B-mode are synchronized and displayed on the same screen (right: B-mode; left: Harmonic Imaging Mode). B-mode findings were almost identical in both testes. Contrast-enhanced ultrasound shows that contrast was not observed in the affected testis parenchyma. On the other hand, contrast is notably observed in the unaffected testis parenchyma. An emergent operation was performed for left testicular torsion, and the testis could be preserved. No testicular atrophy has been observed after the operation
Discussion
Our study found that contrast-enhanced ultrasound can effectively diagnose testicular torsion. Testicular torsion is an acute scrotal disease that requires emergency surgical treatment. The first step in diagnosis is the ultrasound examination, typically by evaluating the blood flow using color Doppler ultrasound. The efficacy of color Doppler ultrasound has been previously reported, and the results have been acceptable. Dogra et al. reported decreased blood flow or absence of blood flow in the affected testicle, with a sensitivity of 86–100% and a specificity of 97.9–100% [10]. However, even testicular torsion can appear to exhibit blood flow on color Doppler imaging, especially in the early stages of testicular torsion where the spermatic vein is compressed and blood return to the testis is impaired while the testicular artery still has a pulse without any efficient blood flow. Therefore, a small blood flow pulse can be detected using color Doppler imaging depending on the situation [1, 2]. Moreover, if the sampling frame is adjusted to a low-velocity scale, artifacts are more likely to be seen on the color Doppler ultrasound. Artifacts were also regarded as a color signal in this study, because the echo images were evaluated retrospectively, and it was impossible to determine whether the color signal was due to actual blood flow or artifacts. In fact, color Doppler showed a small degree of color signal in the testicular parenchyma of the affected testis in our study, even in the torsion group, which could result in a misdiagnosis.
On the other hand, some patients, especially children, also have slender blood vessels and sparse or slow blood flow, making it more difficult to visualize the blood flow signal on color Doppler ultrasound, even in normal testes [11, 12]. Garmela et al. reported that power Doppler, which is more sensitive than color Doppler mode, showed no detectable blood flow in 21.74% of healthy testicles and poor flow in 28.99% of them [13]. In such cases, the blood flow in the affected testis cannot be compared to that in the unaffected testis using Doppler ultrasound. Additionally, pediatric patients suspected of having acute testicular torsion tend to have poor cooperation during examinations, which makes blood flow assessment difficult.
In the present study, the examinations were performed by sufficiently experienced ultrasound technicians, and a reliable diagnosis could be made even with color Doppler (both sensitivity and specificity were 100%). However, ultrasound technicians skilled in ultrasonography are not always available in emergencies. For those unfamiliar with ultrasonography, it may be difficult to accurately and confidently diagnose testicular torsion using common ultrasonography alone. Therefore, a novel method that allows anyone to easily and reliably diagnose testicular torsion is required.
Contrast-enhanced ultrasound has recently been considered a reliable imaging technique for the study of tissue perfusion, and its use in the diagnosis of lesions involving various organs has been standardized [14]. A report on the use of contrast-enhanced ultrasound for diagnosis of acute scrotal diseases was published in 2011 [6], and a case series on contrast-enhanced ultrasound in testicular torsion was published in 2022 [7]; however, no report has evaluated the difference in enhanced ultrasonographic findings between testicular torsion and non-testicular torsion.
Our study revealed that, in the case of contrast-enhanced ultrasound, the contrast effect is markedly diminished in the affected testis compared to the healthy testis of a patient experiencing testicular torsion, whereas these changes are not observable in the testes of patients with acute scrotum without testicular torsion. Therefore, it is possible for any clinician, regardless of ultrasonographic experience, to differentiate whether the cause of the acute scrotum is testicular torsion or not. For physicians with limited ultrasound experience, sending a patient home after ruling out testicular torsion seems very worrisome. Contrast-enhanced ultrasonography can easily rule out testicular torsion because it can depict the actual blood flow in the testis more clearly than color Doppler, and the attending physician can send the patient home with confidence. We believe that this is one of the advantages of contrast-enhanced ultrasound.
Zou et al. reported that contrast-enhanced ultrasound could distinguish between incomplete and complete necrosis of the testicle, but color Doppler could not [7]. However, in the present study, only a slight contrast effect was observed in one of the three cases of incomplete necrosis in which the testis was eventually spared. Therefore, the relationship between the degree of ischemia and contrast effect could not be evaluated in this study and remains an issue to be addressed in the future.
We think that the best way to apply the probe in contrast-enhanced ultrasound while using Contrast Harmonic Imaging mode for the diagnosis of testicular torsion is to display both testes on the same screen, inject the contrast medium intravenously, and compare the contrast effect in the parenchyma of the affected and healthy testes. In the present study, patients were observed for 5 min after contrast agent administration to examine diseases other than testicular torsion, such as torsion of the appendix testis. However, 1 min of observation after contrast administration is sufficient to diagnose testicular torsion.
Color Doppler can display blood flow pulses with a certain velocity in blood vessels of a certain size, but it cannot display the actual microcirculation with very low flow velocity. On the other hand, we believe that contrast-enhanced ultrasound dynamically displays the microcirculation of tissue clearly, even if the flow velocity is too low to be detected with color Doppler. Moreover, color Doppler ultrasonography requires detailed settings, such as adjustment of the sampling frame for detecting very low flow velocity without any artifact. On the other hand, contrast-enhanced ultrasonography using Contrast Harmonic Imaging mode can show microcirculation more clearly than color Doppler without difficult adjustments. This is the advantage of contrast-enhanced ultrasonography over color Doppler. Therefore, contrast-enhanced ultrasonography appears to be one of the most efficient ways to diagnose testicular torsion, although it requires intravenous injection and is more invasive than color Doppler. Additionally, even children who are uncooperative during the examination can be easily evaluated for testicular blood circulation.
Notably, because of the use of hen egg-derived stabilizers, this agent is not recommended for use in patients with egg allergy.
Limitations
The number of patients included in this study was small. Furthermore, there were only three cases in the testicular torsion group in which the testes were preserved. Therefore, it is necessary to collect more cases of contrast effect, especially in cases in which the testis is not completely necrotic with a lower degree of torsion.
Conclusion
Contrast-enhanced ultrasonography is considered a reliable and easy way to diagnose testicular torsion and is suitable for any clinician, regardless of ultrasonographic experience.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Günther P, Rübben I. The acute scrotum in childhood and adolescence. Dtsch Arztebl Int. 2012;109:449–57 (quiz 458).
Bandarkar AN, Blask AR. Testicular torsion with preserved flow: key sonographic features and value-added approach to diagnosis. Pediatr Radiol. 2018;48:735–44.
Laher A, Ragavan S, Mehta P, et al. Testicular torsion in the emergency room: a review of detection and management strategies. Open Access Emerg Med. 2020;12:237–46.
Schellhaas B, Strobel D. Tips and tricks in contrast-enhanced ultrasound (CEUS) for the characterization and detection of liver malignancies. Ultraschall Med. 2019;40:404–24.
Omoto K, Matsunaga H, Take N, et al. Sentinel node detection method using contrast-enhanced ultrasonography with sonazoid in breast cancer: preliminary clinical study. Ultrasound Med Biol. 2009;35:1249–56.
Valentino M, Bertolotto M, Derchi L, et al. Role of contrast enhanced ultrasound in acute scrotal diseases. Eur Radiol. 2011;21:1831–40.
Zou B, Zeng F, Yang Y. Using contrast-enhanced ultrasonography to assess the degree of acute testicular torsion: a case series. BMC Med Imaging. 2022;22:220.
Maruyama H, Ishibashi H, Takahashi M, et al. Effect of signal intensity from the accumulated microbubbles in the liver for differentiation of idiopathic portal hypertension from liver cirrhosis. Radiology. 2009;252:587–94.
Maruyama H, Takahashi M, Ishibashi H, et al. Ultrasound-guided treatments under low acoustic power contrast harmonic imaging for hepatocellular carcinomas undetected by B-mode ultrasonography. Liver Int. 2009;29:708–14.
Dogra VS, Gottlieb RH, Oka M, et al. Sonography of the scrotum. Radiology. 2003;227:18–36.
Nebot CS, Salvador RL, Aliaga SP, et al. Perinatal testicular torsion: ultrasound assessment and differential diagnosis. Radiologia. 2017;59:391–400.
Lee YS, Kim MJ, Han SW, et al. Superb microvascular imaging for the detection of parenchymal perfusion in normal and undescended testes in young children. Eur J Radiol. 2016;85:649–56.
Visalli C, Vinci SL, Mondello S, et al. Microvascular imaging ultrasound (MicroV) and power Doppler vascularization analysis in a pediatric population with early scrotal pain onset. Jpn J Radiol. 2022;40:192–201.
Claudon M, Cosgrove D, Albrecht T, et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS)—update 2008. Ultraschall Med. 2008;29:28–44.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
The authors did not receive support from any organization for the submitted work. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
HF drafted the manuscript. NM performed the ultrasound examinations. MO and YT supervised the writing of the manuscript. HF, MO, YT, and AW evaluated the echo images.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the institutional review board of the Japanese Red Cross Society Himeji Hospital (No. 2022–22). Informed consent was obtained from all patients. All patients consented to the publication of their data and photographs.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Fukuzawa, H., Minoda, N., Okamoto, M. et al. Contrast-enhanced ultrasound findings in testicular torsion and non-testicular torsion. J Med Ultrasonics 51, 133–138 (2024). https://doi.org/10.1007/s10396-023-01384-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-023-01384-x