Abstract
Purpose
Typical myxomatous fibroadenomas have a small depth/width (D/W) ratio on ultrasonography. The small D/W ratio of fibroadenomas is speculated to be caused by the softness of the mass and its orientation along the longitudinal aspect of the ductal elements without adhesion to the surrounding tissue; however, this has not been clearly proven. This study aimed to confirm the reason why fibroadenomas present with a small D/W ratio on ultrasonography.
Methods
We retrospectively analyzed imaging data from 17 patients who were diagnosed with typical fibroadenomas on ultrasonography and who underwent magnetic resonance imaging (MRI) at our hospital.
Results
The median D/W ratio obtained from ultrasonography images was 0.48 (0.32–0.67), while that obtained from MRI was 1.38 (0.62–1.68). The D/W ratios calculated from MRI were significantly greater than those calculated from ultrasonography images (p < 0.001). The D/W ratio obtained using ultrasonography was not greater than the D/W ratio obtained using MRI in any of the cases.
Conclusion
This study revealed that the small D/W ratio of fibroadenomas on ultrasonography may be attributable to the horizontal force acting on the breast against the chest wall in the supine position, the elasticity of the fibroadenoma, and the lack of adhesion between the mass and surrounding tissue.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breast ultrasonography is useful for the differential diagnosis of breast masses, and several diagnostic criteria to distinguish between benign and malignant breast tumors have already been established and are widely used [1, 2]. The depth/width (D/W) ratio of the tumor and the presence or absence of interruption of the interface between adipose and gland or an echogenic halo have particularly important diagnostic value. The D/W ratio is defined as the ratio of the maximum depth diameter of the mass not including the echogenic halo and maximum parallel diameter to the skin surface [3, 4]. The D/W ratio of breast cancer was first reported by Kato in 1983 [5]. At present, the D/W ratio is the only quantitative criteria for differentiating between benign and malignant breast masses using ultrasonography; a cut-off value of 0.7 has been adopted to differentiate malignant tumors from benign ones.
A fibroadenoma is defined as a circumscribed benign neoplasm of the terminal duct lobular unit with biphasic proliferation of epithelial and stromal components. It is one of the most frequently encountered benign breast masses in clinical practice. A typical myxomatous fibroadenoma is detected as a well-circumscribed, round to ovoid mass with a small D/W ratio. At initial screening using ultrasonography, breast masses that are smaller than 2 cm, have clear and smooth borders, and have a sufficiently small D/W ratio are considered to be typical fibroadenomas and are classified as “category 2” tumors, which means that they do not require close examination. Notably, fibroadenomas have varying histopathological types, including hyalinized fibroadenomas and atypical fibroadenomas, which may have a large D/W ratio. However, classifying a fibroadenoma as benign based on initial ultrasound findings could help avoid unnecessary scrutiny of a typical fibroadenoma with a myxomatous appearance. The D/W ratio is one of the most important findings in making such decisions, and thus plays a crucial role in both screening and treatment of breast masses [1, 2].
The small D/W ratio of a fibroadenoma is theoretically caused by the softness of the mass and its orientation along the length of the ductal element without adhesion to the surrounding tissue [6]. However, to the best of our knowledge, there are no studies that have verified the accuracy of this theory, and thus, this explanation remains speculative.
While ultrasound examinations are performed in the supine position, magnetic resonance imaging (MRI) of the breast is performed in the prone position using a dedicated breast coil at many facilities. This is because imaging in the prone position is less susceptible to measurement errors during respiration and the breast can be stretched wider, which is useful in assessing the extent of the lesion on the images. In this study, we compared the D/W ratio calculated using ultrasonography and MRI, which have different directions of gravitational force, to see if we could prove why fibroadenomas have a small D/W ratio on ultrasonography.
Materials and methods
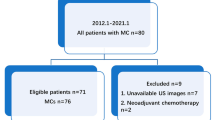
All procedures in our study were performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The institutional review board or ethics committee at our hospital approved this retrospective observational study (study no. 20-R186). Consecutive patients who underwent ultrasonography and MRI for breast cancer treatment at our hospital between March 2020 and October 2020 and in whom a typical fibroadenoma was incidentally detected were included in this study. A typical fibroadenoma on ultrasonography is an oval mass with well-defined smooth borders and a small D/W ratio. Since a typical fibroadenoma presents as a well-defined smooth mass with a high signal on T2-weighted images (T2WI) on MRI, T2WI were used in this study because T2WI best delineate fibroadenomas among other sequences of MRI. Fibroadenomas with a maximum diameter between 5 and 20 mm were included in the study. To correspond with the D/W ratio obtained through ultrasonography, the direction of gravity was defined as the longitudinal diameter (D), and the direction perpendicular to gravity was defined as the transverse diameter (W), in the MRI (Fig. 1). The D/W ratios of all masses were calculated retrospectively from ultrasonography images and MRI and were then compared using univariate analysis (Mann–Whitney U test). Considering the possibility that breast size may affect the difference in D/W ratio, we measured the breast thickness in the depth direction using MRI. Single linear regression analysis was performed to determine the association between breast thickness and the D/W ratio obtained using ultrasonography and MRI.
Results
A total of 17 patients met the inclusion criteria. Patient age ranged from 29 to 69 years, with a median age of 50 years. The average depth thickness of the breast was 45 mm, and the average body mass index (BMI) was 20.5 kg/m2 (Table 1).
The median D/W ratio calculated from ultrasonography images was 0.48 (0.32–0.67), and the median D/W ratio calculated from MRI was 1.38 (0.62–1.68). The median D/W ratio obtained from MRI was significantly greater than that obtained from ultrasonography images (p < 0.001) (Table 2). There was no case where the D/W ratio obtained using ultrasound was greater than that obtained using MRI. Assuming that the data were normally distributed, the mean difference between the D/W ratio obtained using MRI and ultrasonography was 0.797 (95% confidence interval [CI]: 0.61 ~ 0.97).
An increase in breast size was associated with an increase in the D/W ratio measured using MRI, indicating a positive correlation; however, this correlation was not statistically significant (β coefficient 0.0028, 95% CI − 0.0074 to 0.013, p = 0.57). The D/W ratios measured using ultrasonography were not correlated with breast size (β coefficient 0.00056, 95% CI − 0.0027 to 0.0038, p = 0.72) (Fig. 2).
Representative cases for both imaging modalities (ultrasonography and MRI) are shown in Figs. 3 and 4. Ultrasonography images from both cases showed hypoechoic masses with well-defined circumscribed borders and D/W ratios smaller than 0.7. In contrast, MRI from both cases showed that one of the masses had a D/W ratio greater than 1 and a longer depth profile than the other.
A representative case of a 56-year-old woman with a fibroadenoma. a Ultrasound images show a well-circumscribed, ovoid mass with a small D/W ratio. b T2-weighted MRI shows a well-defined smooth mass with a homogenous high signal. The D/W ratio measured using ultrasound was 0.39, which was smaller than the D/W ratio measured using MRI (1.37). D/W ratio depth/width ratio, MRI magnetic resonance imaging
A representative case of a 66-year-old woman with a fibroadenoma. a Ultrasound images show a well-circumscribed, ovoid mass with a small D/W ratio. b T2-weighted MRI shows a well-defined smooth mass with a homogenous high signal. The D/W ratio measured from ultrasonography images was 0.78, which was smaller than that measured from MRI (D/W ratio, 1.44). D/W ratio depth/width ratio, MRI magnetic resonance imaging
Discussion
Our study results revealed that the shape of the fibroadenoma may be altered by the effect of gravity during diagnostic imaging. In the past, the small D/W ratio of fibroadenomas was theorized to be caused by compression of water sacs, which were used during ultrasound tomography at that time [7]. Some speculation also attributed the small D/W ratio of fibroadenomas to the high tissue elasticity of the mass, which facilitated easy deformation. However, no reliable evidence has been presented for these theories. Therefore, by comparing the D/W ratios obtained through ultrasonography performed in the supine position and MRI performed in the prone position, we could provide some insight into why the D/W ratios observed in ultrasonography are small. Furthermore, during ultrasonography performed in the supine position, the breast is placed horizontally against the chest wall, and the ducts and glandular lobe structures extend from the nipple toward the periphery. Fibroadenomas are composed of a normal two-cell layer arrangement of epithelial elements and stromal proliferation. The stromal component is usually of uniformly low cellularity and edematous [8]. These myxomatous changes in the stroma cause typical fibroadenomas to be soft due to low fibroblast activity. On the other hand, cancers are hard due to high fibroblast activity and fiber production inside and at the border of the tumors [9]. One of the reasons why cancers are not prone to deformation is that the tumors are hard and adhere to their surrounding tissue, while benign tumors such as fibroadenomas are soft and do not adhere to the surrounding area, and are therefore affected by lateral extension of the anatomic structures, which is also thought to reduce the D/W ratio. They are also affected by the lateral extension of the anatomical structures, which is also thought to decrease the D/W ratio.
We selected fibroadenomas with a diameter of 5–20 mm for our study because the benign or malignant nature of a fibroadenoma can most accurately be diagnosed using the D/W ratio when the mass diameter is within this range (5–20 mm). If the mass is too small, the shape will resemble that of a sphere, and if it is too large, the mass will be too long horizontally, indicating a large aspect ratio; in both cases, it would be difficult to differentiate between benign and malignant masses. However, breast masses with a diameter between 5 and 20 mm can be diagnosed as benign with high accuracy if their D/W ratio is 0.7 or less [10].
As expected, the D/W ratio obtained from MRI was significantly greater than that obtained from ultrasonography, indicating that the difference in body position had an effect. The change in morphology could be explained as follows: since a fibroadenoma is a substantial mass and not a fluid, it may rotate in accordance with the direction of gravitational extension of the mammary tissue. However, when comparing the long axis of the images from the two modalities (depth in MRI and width in ultrasonography), ultrasonography showed a larger image. Myxomatous fibroadenomas are found to be elastic and may easily deform on dynamic examination. Elastography—an imaging test that has become widespread recently—of a fibroadenoma shows that the elasticity inside the mass is relatively high; in a typical case, the elasticity score is 2, which indicates a “soft mass” [11]. The force of gravity may be pushing against the chest wall, a solid structure on the dorsal side, while the breasts are spread laterally in the supine position, thus causing flattening or deformation and rotation of the mass. A myxomatous fibroadenoma has a very high signal on T2WI, which contributes significantly to the diagnosis, but the finding of a larger D/W ratio on MRI than on ultrasonography on any sequence may also support the diagnosis of a benign mass.
Our study had a few limitations. First, this was a single-center, retrospective study, and there may have been selection bias. However, to the best of our knowledge, there are no previous reports that compare the D/W ratios obtained using ultrasonography and MRI of fibroadenomas, which we believe is of great importance. Second, the diagnosis of fibroadenoma could not be confirmed because no histopathological investigations were performed. However, ultrasound findings are the gold standard for diagnosing typical myxomatous fibroadenomas and are not considered inferior to histopathology in this regard. Rather, fibroadenomas that are histologically diagnosed are often atypical and may not be appropriate for this study; thus, we chose diagnostic imaging to identify typical fibroadenomas.
Conclusion
The shape of fibroadenomas was revealed to be altered by the effect of gravity in different positions during examination. The small D/W ratio of fibroadenomas on ultrasonography could be attributed to the horizontal force acting on the breast against the chest wall in the supine position, elasticity of the fibroadenoma, and lack of adhesion between the mass and surrounding tissue.
References
Terminology and Diagnostic Criteria Committee, Japan Society of Ultrasonics in Medicine. Recall criteria for ultrasound breast cancer screening. J Med Ultrason. 2016;43:301–13.
Taira N, Arai M, Ikeda M, et al. The Japanese Breast Cancer Society clinical practice guidelines for epidemiology and prevention of breast cancer, 2015 edition. Breast Cancer. 2016;23:343–56.
Ban K, Tsunoda H, Suzuki S, et al. Verification of recall criteria for masses detected on ultrasound breast cancer screening. J Med Ultrason. 2018;45:65–73.
Watanabe T, Yamaguchi T, Tohno E, et al. B-mode ultrasound diagnostic flowchart for solid breast masses: JABTS BC-01 study. J Med Ultrason. 2021;48:71–81.
Kato Y, Hiyoshi D, Fujimoto Y, et al. Breast cancer ultrasound study. Proceedings of a meeting. J Med Ultrason. 1983;42:639–40.
Tohno E, Cosgrove DO, Sloane JP. Ultrasound diagnosis of breast diseases. 1st ed. Edinburgh: Churchill Livingstone; 1994. p. 80.
Fujimoto Y, Kato Y, Hiyoshi D, et al. Elasticity of breast tumors in ultrasonogram. Proceeding of a meeting. J Med Ultrasonic. 1983;43:263–4.
Thike AA, Brogi E, Harada O, et al. Fibroadenoma. WHO classification of tumours editorial board. Breast tumors WHO classifications of tumours. 5th ed. 2019. p. 168–71.
Rakha EA, Allison KH, Bu H, et al. Invasive breast carcinoma of no special type. WHO classification of tumours editorial board. Breast tumors WHO classifications of tumours. 5th ed. 2019. p. 102–9.
Tsunoda-Shimizu H, Kato Y, Ueno E, et al. Usefulness of depth to width ratio in differentiation of regular invasive ductal carcinoma from fibroadenoma. In: Research and development in breast ultrasound. Tokyo: Springer; 2005. p. 57–61.
Itoh A, Ueno E, Tohno E, et al. Breast disease: clinical application of US elastography for diagnosis. Radiology. 2006;239:341–50.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Contributions
KS and HT were involved in study design and data interpretation. SF was involved in the data analysis. KO, KY, and YK critically revised the work for important intellectual content. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Kana Suga, Hiroko Tsunoda, Sho Fukui, Ken Oba, Kazuyo Yagishita, and Yasuyuki Kurihara declare that they have no conflicts of interest.
Ethical statement
All procedures in our study were performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The institutional review board or ethics committee at our hospital approved this retrospective observational study (study no. 20-R186).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Suga, K., Tsunoda, H., Fukui, S. et al. Why is the depth/width ratio of a typical fibroadenoma small in breast ultrasonography?. J Med Ultrasonics 50, 97–101 (2023). https://doi.org/10.1007/s10396-022-01267-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-022-01267-7