Abstract
Carotid artery ultrasonography is capable of diagnosing or inferring the presence or absence of stenosis or occlusion of the internal carotid artery (ICA) and vertebral artery (VA), as well as the not directly observable distal ICA, middle cerebral artery (MCA), and basilar artery (BA). Stenosis at the origin of the ICA is mainly evaluated using the parameter peak systolic velocity (PSV), with values of ≥ 200–230 cm/s indicating severe stenosis. Recently, the acceleration time ratio has been reported for diagnosis of ICA origin stenosis. An indicator called the end-diastolic (ED) ratio can be used for diagnosing occlusion of the distal ICA or the M1 segment of the MCA. The PSV of stenosis can be used to diagnose stenosis at the beginning of the VA or V1, and mean flow velocity, mean ratio, and diameter ratio can be used to diagnose distal VA occlusion. Furthermore, the usefulness of the VA pulsatility index and resistance index has been suggested for diagnosing stenosis or occlusion of the BA. This review outlines diagnostic sonography criteria for stenosis and occlusion of extracranial and intracranial arteries.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
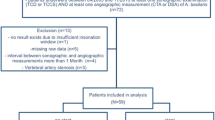
In the general population, the prevalence of asymptomatic extracranial internal carotid artery (ICA) stenosis is 0–7.5% for moderate stenosis of ≥ 50% and 0–3.1% for severe stenosis of ≥ 70% [1, 2]. In patients with moderate stenosis of ≥ 50%, 0.5–2% develop ischemic stroke on the side with stenosis [3,4,5,6], leading to a mortality rate of 7.7% per year in a survey with a follow-up period of about 2.8 years [7]. Mild carotid artery stenosis is not an indication for carotid endarterectomy (CEA) or carotid artery stenting (CAS), but these procedures should be considered in patients with moderate and especially severe stenosis [8]. Moreover, CEA or CAS can be considered in ischemic stroke patients with ≥ 50% stenosis of the carotid artery [9].
Carotid artery stenosis screening can be performed with magnetic resonance angiography (MRA), contrast-enhanced MRA, contrast-enhanced computed tomography (CT), and carotid artery ultrasonography. However, MRA findings may overestimate the frequency of moderate stenosis, and unwanted effects may occur when using contrast agents for contrast-enhanced CT angiography, although not very often [10]. By contrast, carotid artery ultrasonography is a noninvasive method that is useful for diagnosing carotid artery stenosis and occlusion. It correlates particularly well with digital subtraction angiography (DSA) for carotid artery stenosis [11]. This review describes the use of carotid artery ultrasonography in the diagnosis of carotid artery stenosis and occlusion.
Diagnosis of stenosis at the origin of the ICA
Due to hemodynamic factors, plaque tends to form between the origin of the ICA and the carotid sinus [12], and stenotic lesions are likely to appear. Therefore, this region needs to be examined in detail.
B-mode and color Doppler imaging can be used to calculate the area stenosis rate from the short-axis view, as well as the diameter stenosis rate from the long- and short-axis views. Two methods have been suggested for measuring the diameter stenosis rate [13], i.e., the European Carotid Surgery Trial (ECST) method [14] and the North American Symptomatic Carotid Endarterectomy Trial (NASCET) method [15] (Fig. 1). Although both use the same DSA measurement approach, with carotid artery ultrasonography, it is often difficult to determine the diameter of the distal ICA; thus, it is easier to assess the diameter stenosis rate using the ECST method. However, for individual cases, the area stenosis rate, diameter stenosis rate using the ECST method, and diameter stenosis rate using the NASCET method are not consistent. Generally, the area stenosis rate leads to the highest stenosis rate, whereas the NASCET method leads to the lowest rate [11]. Therefore, the method used for stenosis rate assessment should always be included in the report. As the DSA-based NASCET stenosis rate is used to determine whether CEA or CAS is indicated, it is best to assess the stenosis rate using the NASCET method whenever possible. The stenosis rate can also be calculated based on the parameter peak systolic velocity (PSV) determined using pulsed-wave Doppler (PWD) measurements.
Measurement of the area stenosis rate and diameter stenosis rate. Using conventional B-mode ultrasound with superb microvascular imaging, the short-axis view (a, b) and long-axis view (c) are shown. The area stenosis (a) is calculated by (B − A)/B × 100 (%), the stenosis rate according to the ECST method (b, c) is calculated by (D − C)/D × 100 (%), and the stenosis rate based on the NASCET method (c) is calculated by (E − C)/E × 100 (%). ECST European Carotid Surgery Trial, NASCET North American Symptomatic Carotid Endarterectomy Trial. Reprinted from reference [13]
Koga et al. [16] evaluated carotid artery echocardiography and DSA in 75 patients with cerebrovascular disease. The results revealed that the PSV of ICA stenosis (ICAPSV) greater than 200 cm/s was the most reliable predictor of ICA stenosis greater than 70% according to the NASCET criteria using DSA findings. In another study of 376 carotid arteries, AbuRahma et al. [17] conclude that when the PSV of ICAPSV is ≥ 125 cm/s or the ratio of the ICAPSV to the common carotid artery (CCA) PSV (CCAPSV; ICAPSV/CCAPSV) is ≥ 2, and the ICA end-diastolic velocity (EDV) (ICAEDV) is < 40 cm/s, a stenosis of ≥ 50% according to the NASCET criteria using DSA findings can be assumed. Moreover, they report that for stenosis of ≥ 70% according to the NASCET method, the ICAPSV is > 230 cm/s or the ratio ICAPSV/CCAPSV is > 4, and the ICAEDV value is ≥ 40 cm/s. The parameter ICAPSV was particularly useful, with an area under the receiver operating characteristic curve (AUC) of 0.97 for stenosis of ≥ 50% and 0.97 for stenosis of ≥ 70% according to the NASCET method. Diagnosing stenoses of ≥ 50% and ≥ 70% based on the NASCET method had sensitivity values of 96% and 99%, specificity values of 82% and 96%, positive predictive values (PPVs) of 93% and 98%, negative predictive values (NPVs) of 90% and 97%, and accuracy of 92% and 98%, respectively. Tokunaga et al. [18] conducted a retrospective analysis of 127 blood vessels and found that when the ICAPSV was ≥ 130 cm/s, diagnosing stenosis of ≥ 50% based on the NASCET method had 95% sensitivity, 85% specificity, 75% PPV, 97% NPV, and 88% accuracy. When the ICAPSV was ≥ 200 cm/s, diagnosing stenosis of ≥ 70% using the NASCET method had 96% sensitivity, 95% specificity, 83% PPV, 99% NPV, and 95% accuracy. However, another study that compared CT angiography with carotid artery ultrasonography showed little correlation between the stenosis rate determined by the CT angiography-based NASCET method and that determined by ultrasound-based PWD. For NASCET-based stenosis of ≥ 70%, the AUC was only 0.51 with an ICAPSV cutoff value of 230 cm/s [19].
According to these studies, the carotid artery ultrasonography-based diagnosis of the stenosis rate in Japan is as follows: When the ICAPSV is ≥ 125 or 130 cm/s, or when the ratio ICAPSV/CCAPSV is ≥ 2, the stenosis rate based on the NASCET method using DSA is ≥ 50%; when the ICAPSV is ≥ 200 or 230 cm/s, or when the PSAICA/PSVCCA ratio is ≥ 4, the stenosis rate with the NASCET method is ≥ 70% [11, 13] (Fig. 2).
NASCET stenosis rate using the peak systolic velocity. PWD (a, b) and DSA (c) measurements are shown. PSV in the CCA (a) is 100.7 cm/s, and PSV and EDV at the ICA stenosis (b) are 422.8 cm/s and 237.9 cm/s, respectively. Thus, the ratio PSVICA/PSVCCA is 4.20. DSA (c) reveals stenosis of > 70% according to the NASCET method (arrow). PWD pulsed-wave Doppler, DSA digital subtraction angiography, CCA common carotid artery, PSV peak systolic velocity, EDV end-diastolic velocity, ICA internal carotid artery, NASCET North American Symptomatic Carotid Endarterectomy Trial
PSV has also been reported to be useful for predicting asymptomatic carotid artery stenosis. Hicks et al. [20] followed 282 patients with moderate asymptomatic carotid artery stenosis ≥ 50% and < 70% for about 2 years. They found that the ratio ICAPSV/CCAPSV was the most useful indicator for predicting stenosis progression. When the ICAPSV/CCAPSV ratio was > 2.5, > 3.3, and > 3.8, the risk of stenosis progression was ≥ 10%, ≥ 20%, and ≥ 30%, respectively. The diagnosis of moderate stenosis in their study was not based on DSA findings but was assessed using PWD carotid artery ultrasonography as ICAPSV > 125 cm/s and < 230 cm/s, ICAEDV > 40 cm/s and < 100 cm/s, and ICAPSV/CCAPSV > 2.0 and < 4.0. In addition to the lack of a DSA-based diagnosis, the exact stenosis rate remains unknown in this study because an ICAPSV value ≥ 200 cm/s may represent stenosis of ≥ 70% with the NASCET method according to the diagnostic criteria of Tokunaga et al. [18]. However, ICAPSV is a useful indicator for detecting the risk of stenosis progression and for the screening of patients who need careful follow-up.
When diagnosing stenosis with PWD, it is important to accurately measure PSV with an insonation angle of < 60º [11]. The insonation angle is the angle between the direction of the ultrasound beam and the direction of the blood flow. When the direction of the blood flow at the stenosis site is parallel to the vessel wall, correction of the insonation angle is easy, but when the blood flow at the stenosis site is not parallel to the vessel wall, PSV differs when the angle is corrected to be parallel to the vessel wall and when it is aligned with the direction of the blood flow. In a study of 50 cases by Igarashi et al., diagnosing a stenosis rate of ≥ 70% based on the NASCET method using DSA, PWD sonography with the insonation angle being parallel to the vessel wall had an AUC of 0.765, and with a cutoff value of ICAPSV ≥ 256.9 cm/s, the sensitivity was 70.0% and the specificity was 80.0%. By contrast, when the angle was aligned with the blood flow direction, the AUC was 0.973, and with a cutoff value of 203.5 cm/s, the sensitivity was 100% and the specificity was 85.7% [21]. Therefore, the stenosis diagnosis seems to be more accurate when the insonation angle is aligned with the direction of the blood flow.
On the other hand, Tola et al. [22] examined the NASCET stenosis rate with DSA and according to the insonation angle in 87 patients with an ICAPSV value of > 125 cm/s. Their results indicate that an insonation angle of 45º may underestimate the stenosis rate. Therefore, the guidelines of the Society for Vascular Ultrasound [23] recommend setting the insonation angle to 60º.
Diagnosis of an ICA origin stenosis using the acceleration time (AcT) ratio
In cases of plaque with an acoustic shadow, especially circumferential calcified plaque, the parameter ICAPSV sometimes cannot be measured at the region of greatest stenosis. In such cases, the pulse Doppler waveform after the stenosis shows a turbulent flow or the AcT on the distal side is prolonged [11] (Fig. 3). However, there are no clear AcT-based criteria for diagnosis of the stenosis rate.
Takekawa et al. [24] measured acceleration times to examine the usefulness of the AcT ratio, calculated as the ratio AcT at the distal ICA/AcT at the ipsilateral CCA. In 127 vessels, the parameters AcT ratio and ICAPSV had a correlation coefficient of 0.82 (p < 0.0001). With a cutoff value of 1.75, diagnosing ICAPSV ≥ 150 cm/s had a sensitivity of 92.3% and a specificity of 97.4%. When the cutoff value was 2.0, diagnosing ICAPSV ≥ 200 cm/s had a sensitivity of 90.0% and a specificity of 96.6%. In a study of 265 vessels [25], the correlation coefficient between the AcT ratio and the diameter stenosis rate based on the ECST method using carotid artery ultrasonography was 0.60 (p < 0.00001). Using a cutoff value of 1.5, diagnosing a stenosis rate of > 65% had a sensitivity of 90.0% and a specificity of 93.5% (odds ratio [OR] 128.8). Nishihira et al. [26] examined the relationship between the NASCET stenosis rate using DSA and the AcT ratio in 177 blood vessels. Their results showed that the AcT ratio had the highest correlation with stenosis rate, with the correlation coefficient for ICAPSV being 0.647, that for the ratio ICAPSV/CCAPSV being 0.670, and that for the AcT ratio being 0.744 (all p < 0.0001). When the cutoff value of the AcT ratio was 1.31, diagnosing stenosis of ≥ 50% had 94.5% sensitivity, 91.0% specificity, 82.6% PPV, 97.4% NPV, and 92.1% accuracy. With an AcT ratio cutoff of 1.35, diagnosing stenosis of ≥ 70% had 97.1% sensitivity, 83.2% specificity, 99.2% NPV, and 85.9% accuracy, while the PPV was low at 57.9%.
In these studies, the AcT of the distal ICA was measured at about 3 cm distal to the carotid bulb with a convex array probe, and that of the CCA at about 2 cm proximal to the carotid bulb with a linear array probe. In general, AcT is the time from the minimum flow rate to the maximum flow rate, i.e., the time from EDV to PSV. However, the methods described by Takekawa et al. [24, 25] and Nishihira et al. [26] measure the time to PSV as the time until the inflection point when the pulse Doppler waveform is a mono-modal peak pattern with a distinct flection point, and in cases with a bimodal peak pattern, the time to the first peak is measured. Iizuka et al. [27] compared the methods of Takekawa et al. and Nishihira et al. with a method of measuring the time from EDV to PSV for measuring the AcT. The NASCET stenosis rate using DSA exhibited significant positive correlations with the AcT ratios calculated based on the method by Takekawa et al. and Nishira et al., as well as with the AT ratio defined as the ratio distal ICA AcT/ipsilateral CCA AcT calculated using the time from EDV to PSV (Fig. 4). The AUC for the diagnosis of stenosis of ≥ 50% was 0.971 for the AcT ratio, whereas the AT ratio was not useful, with an AUC of 0.572. Likewise, the AUC for stenosis of ≥ 70% was 0.621 for the AT ratio, compared to an AUC of 0.920 for the AcT ratio. These findings indicate that the method used by Takekawa et al. and Nishihira et al. to measure AcT is more useful, i.e., measuring the time to the inflection point in the mono-modal peak pattern with a distinct flection point, and the time to the first peak is measured in the bimodal peak pattern.
Measurements of the AcT ratio and AT ratio. The AcT ratio measures the time to the inflection point, if an obvious one exists, before reaching PSV, or the time to the first peak in bimodal cases (time between solid lines). The AT ratio measures the time to PSV (time between dotted lines). a Type A: This is a bimodal peak pattern; the initial peak of the waveform is consistent with PSV. b Type B: This is a bimodal peak pattern; the second peak of the waveform is consistent with PSV. c Type C: This is a mono-modal peak pattern; the waveform has a clear inflection point. d Type D: This is a mono-modal peak pattern, where the inflection point is unclear. AcT and AT acceleration time, PSV peak systolic velocity. Reprinted from reference [27]
It should be noted that, when the AcT is prolonged in the bilateral CCAs, ICAs, and external carotid arteries, aortic stenosis might be a differential diagnosis [28]. However, Okamura et al. [29] examined the correlation between aortic stenosis and the AcT ratio in 60 cases and found that the AcT ratio was not affected by aortic stenosis.
Carotid artery ultrasonography in patients with carotid artery stenting (CAS)
CEA and CAS are recommended for severe symptomatic extracranial ICA stenosis of ≥ 70% in patients with ischemic stroke, whereas CEA is recommended for moderate stenosis of ≥ 50% [9]. Even in cases of asymptomatic extracranial ICA stenosis without ischemic stroke, CEA or CAS should be considered in patients with moderate-to-severe stenosis, especially those with severe stenosis [8] (Fig. 5). Although the choice between CEA and CAS is based on the patient’s condition and other factors, preoperative carotid artery ultrasonography plays an important role.
B-mode imaging of CAS and CEA. Conventional B-mode ultrasound images of the carotid artery in CAS (a) and CEA (b) are shown. Stent struts (solid line arrows) and sutures (dotted line arrows) are observed. CAS and CEA are recommended for severe stenosis, especially for severe symptomatic stenosis of the extracranial internal carotid artery. CAS carotid artery stenting, CEA carotid endarterectomy
Preoperative assessments include measurements of the stenosis rate, plaque properties, stenosis length, degree of flexion of the ICA distal to the stenosis, vessel diameter, and internal diameter [11]. In particular in patients scheduled for CAS, it is important to identify cases of poor dilatation and reduced blood pressure during diastole when calcified plaque is ≥ 3/4 of the circumference. Echolucent plaque increases the risk of distal emboli or filter cloggings during distal filter protection. Data on stenosis length, internal diameter, and flexion are also important factors when choosing the stent. Carotid artery ultrasonography is useful for these assessments, and stenosis length and internal diameter correlate well with corresponding DSA findings [30]. Carotid artery ultrasonography is also useful in cases of postoperative restenosis, dissection, fluid collections, thromboembolism, and stent deformation [31].
Furthermore, while the incidence of restenosis ≥ 70% does not differ between CEA and CAS, restenosis ≥ 50% or occlusion is more common with CEA than with CAS (OR 2.00, 95% confidence interval 1.12–3.60) [32]. The rate of restenosis ≥ 50% was 3.9% after 6 months and 5.7% after 12 months [33], with a cumulative 5-year risk of 40.7% [34]. PSV at the stenosis site can be used to diagnose restenosis with carotid artery ultrasonography, but the PSV cutoff value differs between surgical and nonsurgical cases. Setacci et al. [35] evaluated restenosis in 814 patients who underwent CAS. They found that ICAPSV at the stenosis site was ≤ 174 cm/s for 30–50% restenosis and ≤ 299 cm/s for moderate restenosis of 50–70%. In addition, restenosis of more than 70% was defined as ICAPSV ≥ 300 cm/s, ICAEDV ≥ 140 cm/s, and ICAPSV/CCAPSV ratio ≥ 3.8. The AUC values were 0.99 for ICAPSV, 0.98 for ICAEDV, and 0.99 for ICAPSV/CCAPSV, demonstrating high reliability. Several other studies have shown that in severe stenosis of 70% or 80% after CAS, ICAPSV at the stenosis site is ≥ 300–330 cm/s, ICAEDV is ≥ 120–140 cm/s, and ICAPSV/CCAPSV is ≥ 3.2–4.0 [36]. AbuRahma et al. [37] examined 200 patients who underwent CEA. They found that the sensitivity, specificity, PPV, NPV, and accuracy were all 98% for diagnosing restenosis ≥ 30% when the ICAPSV was ≥ 155 cm/s at the site of restenosis after CEA. The sensitivity, specificity, PPV, NPV, and accuracy were 99%, 100%, 100%, 98%, and 99%, respectively, for ≥ 50% restenosis when the ICAPSV was ≥ 213 cm/s. Furthermore, when ICAPSV was ≥ 274 cm/s, severe restenosis of ≥ 70% could be diagnosed with a sensitivity of 99%, specificity of 91%, PPV of 99%, NPV of 91%, and accuracy of 98%. However, limited research exists on the use of carotid artery ultrasonography for diagnosing restenosis after CEA, and there are no clear diagnostic criteria. Recently, the usefulness of transoral carotid ultrasonography has been demonstrated, with contrast-enhanced transoral carotid ultrasonography being especially useful for assessments before and after CAS [38].
Diagnosing ICA and middle cerebral artery (MCA) occlusion
In the acute phase of cerebral infarction, the indications for intravenous recombinant tissue plasminogen activator or mechanical thrombectomy must be determined based on the time of onset or discovery, clinical symptoms, and imaging findings [39]. Mechanical thrombectomy is a particularly good indication for occlusion of the M1 or M2 segment of the MCA, and acute cerebral infarction requires a rapid diagnosis of the occluded vessel.
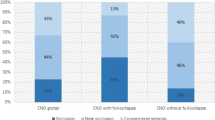
Yasaka et al. [40] examined whether the occlusion site could be inferred from the EDV of the CCA in 46 patients with acute cardioembolic cerebral infarction. Their results demonstrated the usefulness of the ED ratio, i.e., the ratio of the EDV of the CCA of the nonaffected side divided by that of the affected side. The ED ratio was ≥ 4.0 for ICA occlusion, 1.3–4.0 for M1 segment occlusion, and < 1.3 for MCA occlusion distal to M1. The accuracy was 97% for ICA occlusion and 93% for M1 occlusion, and the ED ratio is now widely used for occlusion diagnosis (Fig. 6). Kimura et al. [41] examined the usefulness of EDV and ED ratio of the CCA for diagnosing ICA occlusion. Their results showed that in acute atherothrombotic cerebral infarction, the ED ratio was ≥ 1.4 and EDV was 10.9 ± 6.1 cm/s. The ED ratio was ≥ 1.4 in cardioembolic cerebral infarction with ICA occlusion, but the EDV was 1.8 ± 3.4 cm/s, which was significantly lower than in atherothrombotic cerebral infarction. In 25 healthy participants, the ED ratio was < 1.4 and EDV was 20.3 ± 6.0 cm/s. These findings show that the ED ratio is ≥ 1.4 in acute cerebral infarction with ICA occlusion, that EDV is significantly lower in patients with occlusion than in healthy individuals, and that EDV is significantly lower in patients with acute cardioembolic cerebral infarction than in those with atherothrombotic cerebral infarction [13] (Fig. 7). Some patients with ICA occlusions have mobile thrombi that quickly move to the cranial side in the systolic phase with relatively uniform echogenicity, then slowly return to the original position during the diastolic phase. This type of mobile thrombus is also called an oscillating thrombus (Fig. 8) and tends to appear in ICA occlusion due to acute cardioembolic cerebral infarction [13, 42].
Ultrasound findings of MCA occlusion in cardioembolic cerebral infarction. PWD (a, b) and DSA (c) measurements are shown. The EDV values of the right (a) and left (b) CCA are 5.4 cm/s and 7.9 cm/s, respectively. Therefore, the ED ratio is 1.46. DSA (c) revealed an occlusion to the right M1 segment of the MCA (arrow). MCA middle cerebral artery, PWD pulsed-wave Doppler, DSA digital subtraction angiography, EDV end-diastolic flow velocity, CCA common carotid artery
Ultrasound findings of ICA occlusion. Pulsed-wave Doppler ultrasound (a, b) and MRA (c) are shown. The EDV values of the right (a) and left (b) CCA are 4.8 cm/s and 12.9 cm/s, respectively. Therefore, the ED ratio is 2.7. MRA (c) reveals occlusion of the left ICA (arrow). ICA internal carotid artery, CCA common carotid artery, MRA magnetic resonance angiography, EDV end-diastolic flow velocity. Reprinted from reference [13]
Oscillating thrombus. An oscillating thrombus is a mobile thrombus with a relatively uniform echo intensity (arrow), particularly evident in patients with ICA occlusion caused by acute cardioembolic cerebral infarction. ICA, internal carotid artery. Reprinted from reference [13]
Diagnosis of vertebral artery (VA) occlusion
Koch et al. [43] studied VA origin stenoses of ≥ 50% in 386 vessels. The AUC values for diagnosing stenosis based on the parameters VA origin PSV, ratio VA origin PSV/V1 segment PSV, and ratio VA origin PSV/V2 segment PSV were 0.821, 0.733, and 0.765, respectively, demonstrating VA origin PSV to be the most useful parameter. For diagnosing stenosis of ≥ 50%, VA origin PSV ≥ 58 cm/s had 90% sensitivity and 45% specificity, ≥ 77 cm/s had 80% sensitivity and 71% specificity, ≥ 114 cm/s had 70% sensitivity and 90% specificity, and ≥ 129 cm/s had 60% sensitivity and 92% specificity. Hua et al. [44] examined stenoses at the origin of the VA in 247 cases. They found that for mild stenosis (< 50%), the VA origin PSV was ≥ 85 cm/s, the ratio VA origin PSV/V2 segment PSV was ≥ 1.3, and the VA origin EDV was ≥ 27 cm/s. In moderate stenosis (50–69%), the VA origin PSV was ≥ 140 cm/s, the ratio VA origin PSV/V2 segment PSV was ≥ 2.0, and the VA origin EDV was ≥ 35 cm/s. For severe stenosis (≥ 70%), the VA origin PSV was ≥ 210 m/s, the ratio VA origin PSV/V2 segment PSV was ≥ 4.0, and the VA origin EDV was ≥ 50 cm/s. The AUC values were highest for VA origin PSV at 0.974 for < 50% stenosis, 0.986 for 50–69% stenosis, and 0.950 for ≥ 70% stenosis. For the ratio VA origin PSV/V2 segment PSV, the AUC values were 0.953, 0.972, and 0.907, respectively, confirming it to be almost as useful as VA origin PSV. For VA origin EDV, the AUC values were 0.640, 0.834, and 0.858, respectively, indicating it is less useful than the other assessment parameters. For VA origin PSV, the accuracy was 94.5% for < 50% stenosis, 96.2% for 50–69% stenosis, and 88.7% for ≥ 70% stenosis.
Rozeman et al. [45] studied 337 cases of vertebrobasilar stroke with ≥ 50% stenosis. They found that for diagnosing V1 segment stenosis of ≥ 50%, a PSV ≥ 140 cm/s at the stenosis had 39% sensitivity and 88% specificity, ≥ 130 cm/s had 48% sensitivity and 85% specificity, ≥ 120 cm/s had 61% sensitivity and 78% specificity, ≥ 110 cm/s had 68% sensitivity and 69% specificity, ≥ 100 cm/s had 71% sensitivity and 57% specificity, ≥ 90 cm/s had 84% sensitivity and 47% specificity, ≥ 80 cm/s had 84% sensitivity and 37% specificity, and ≥ 70 cm/s had 87% sensitivity and 25% specificity. They determined the most suitable cutoff value for V1 stenosis as 90 cm/s. However, in many cases, the V1 segment cannot be observed by carotid artery ultrasonography, and the authors concluded that carotid artery ultrasonography was of limited use in the diagnosis of VA stenosis.
Diagnosis of distal VA occlusion has also been studied. Analyzing data from 128 patients, Saito et al. [46] proposed diagnostic criteria for VA occlusion using VA vessel diameter, time-averaged maximum flow velocity (TAMV), PSV, and EDV. These authors suggest that if VA blood flow is completely absent, the VA is occluded at the VA origin. By contrast, if the blood flow in the pulse Doppler waveform is only absent during diastole, the VA is occluded before the branch of the posterior inferior cerebellar artery (PICA). If a diastolic blood flow signal can be identified, TAMV should be evaluated. A TAMV value of ≥ 18 cm/s is considered normal, but if it is < 18 cm/s, the mean ratio, i.e., the ratio between the TAMV value of the higher side and the lower TAMV value of the contralateral side, should be calculated. A mean ratio of < 1.4 is normal, but for a mean ratio ≥ 1.4, the diameter ratio (i.e., the larger vessel diameter divided by the smaller, contralateral vessel diameter) should be determined. If the diameter ratio is < 1.4, meaning there is not much of a left–right difference in vessel diameter, the VA is occluded after the PICA bifurcation on the side with the lower velocity. If the diameter ratio is ≥ 1.4, the diagnosis is asymptomatic VA occlusion or hypoplastic VA (Fig. 9). Although the accuracy of these diagnostic criteria is high at 95%, it should be noted that 65.6% of the patients in the study had acute cerebral infarction. A bow hunter’s stroke, in which an ischemic stroke is caused by cervical rotation or other movements, can be diagnosed by observing changes in the VA pulse Doppler waveform during these movements [47]. Therefore, it is important to examine the VA in different neck positions.
Diagnosis of the VA occlusion site. Pulsed-wave Doppler ultrasound (a, b), and MRA (c) images are shown. In the right VA of this patient, the vessel diameter is 3.6 mm, EDV is 42.8 cm/s, and TAMV is 49.7 cm/s (a). In the left VA, the vessel diameter is 3.0 mm, EDV is 4.4 cm/s, and TAMV is 9.0 cm/s (b). The MV ratio is 5.5, the diameter ratio is 1.2, and MR angiography reveals a symptomatic left VA occlusion after the PICA branch (c). VA vertebral artery, MRA magnetic resonance angiography, TAMV time-averaged maximum velocity, PICA posterior inferior cerebellar artery, EDV end-diastolic velocity. Reprinted with modification from reference [13]
Diagnosis of basilar artery (BA) stenosis and occlusion
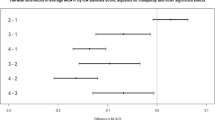
Cerebral infarction due to BA occlusion can be fatal. Okamura et al. [48] compared PWD findings in the VA with the BA diameter stenosis rate determined by MRA in 122 cases with TAMV values < 18 cm/s in both VAs. Using PWD, they examined EDV and TAMV of the VA with slower velocities (Min EDV and Min MV, respectively), as well as pulsatility index (PI) and resistance index (RI) of the VA with higher values (Max PI and Max RI, respectively) (Fig. 10). The results showed that BAs with stenosis of ≥ 50% or occlusion had significantly lower Min EDVs and Min MVs, as well as significantly higher Max PIs and Max RIs. However, the AUCs for Min EDV (0.321) and Min MV (0.237) indicated that these parameters were not very useful. Likewise, Max RI had a low AUC of 0.662, whereas Max PI had a predictive value of 0.718, which was also low but expected to indicate the usefulness of this parameter. When Max PI was ≥ 2.0 or Max RI was ≥ 0.82, diagnosis of BA with ≥ 50% stenosis or occlusion had 75.0% sensitivity, 57.0% specificity, 42.2% PPV, and 84.5% NPV. When Max PI was ≥ 2.0 and Max RI was ≥ 0.82, this diagnosis had 61.1% sensitivity, 68.6% specificity, 44.9% PPV, and 80.8% NPV. It should be mentioned that 77.9% of the study participants had acute strokes.
Ultrasound findings of BA stenosis ≥ 50%. MRA (a, b) and PWD (c, d) images are shown. The stenosis rate of the BA calculated based on findings in image b (arrow) and image a (arrow) is ≥ 50%. For the right VA (c), the PSV is 33.4 cm/s, EDV is 5.3 cm/s, TAMV is 12.0 cm/s, PI is 2.34, and RI is 0.84. For the left VA (d), the PSV is 26.4 cm/s, EDV is 4.0 cm/s, TAMV is 8.6 cm/s, PI is 2.55, and RI is 0.83. Thus, the TAMV values are < 18 cm/s in both VAs, Max PI is 2.55, and Max RI is 0.84. BA basilar artery, MRA magnetic resonance angiography, PWD pulsed-wave Doppler, VA vertebral artery, PSV peak systolic velocity, EDV end-diastolic velocity, TAMV time-averaged maximum flow velocity, PI pulsatility index, RI resistance index
Other findings
Carotid artery ultrasonography is useful for diagnosing stenosis or occlusion of the subclavian artery proximal site before the VA bifurcation. Sakima et al. [49] compared stenosis rates of the subclavian artery assessed using pulse Doppler waveform and angiography of the left VA in 22 patients. The results showed no changes in VA pulse Doppler waveform in arteries with < 50% stenosis, but a mild notch appeared in the systole in arteries with 50–59% stenosis, a retrograde flow was observed in arteries with 60–69% stenosis, more anterograde than retrograde flow in arteries with 70–89% stenosis, and only retrograde flow in arteries with ≥ 90% stenosis (Fig. 11). The degree of subclavian artery stenosis was significantly correlated with the change in VA pulse Doppler waveform (R2 = 0.646, p < 0.0001).
Pulse Doppler waveform of the VA in subclavian artery stenosis or occlusion. Depending on the presence and degree of subclavian artery stenosis, the pulse Doppler waveform in the VA can show a normal flow pattern (a), a mid-systolic notch (b), a retrograde flow smaller than the antegrade flow (c), a retrograde flow larger than the antegrade flow (d), or a retrograde flow without an antegrade flow (e). VA vertebral artery. Reprinted from reference [13]
In moyamoya disease, the ICA diameter declines rapidly after the bifurcation to less than half of that of the CCA diameter, creating the champagne bottle neck sign, or to less than the diameter of the external carotid artery, resulting in the diameter reversal sign [50]. The champagne bottle neck sign is particularly more likely to appear in patients with severe stenosis or occlusion of grade 4 or higher [51] in a major cranial artery [52].
Moreover, Takayasu’s arteritis leads to circumferential thickening of the CCA wall—called the macaroni sign—and in advanced cases, the CCA may be occluded [53].
Conclusion
This review outlined the diagnosis of stenosis and occlusion in the CCA, ICA, and VA, which can be evaluated with carotid artery ultrasonography. It is also possible to infer stenosis and occlusion in the MCA and BA, which cannot be directly observed with carotid artery ultrasonography (Table 1). These assessments provide essential data for patient risk management. Carotid artery ultrasonography is noninvasive, can be performed repeatedly at the bedside, and can provide rapid assessments and diagnoses even in emergency rooms. Therefore, in patients with acute ischemic stroke, it can provide important information regarding the pathophysiology, diagnosis, and treatment selection [13].
When a stenotic lesion is found in the extracranial carotid artery, it is important to consider surgical treatment, but the most important thing is to immediately manage the risk of vascular injury and administer antithrombotic drugs as needed, i.e., to provide the best medical treatment. Regular imaging examinations, including carotid artery ultrasonography, should be performed to assess the potential progression of stenotic lesions.
References
de Weerd M, Greving JP, Hedblad B, et al. Prevalence of asymptomatic carotid artery stenosis in the general population: an individual participant data meta-analysis. Stroke. 2010;41:1294–7.
U.S. Preventive Services Task Force. Screening for asymptomatic carotid artery stenosis: recommendation statement. Am Fam Physician. 2015;91:716J-K.
Abbott AL. Medical (nonsurgical) intervention alone is now best for prevention of stroke associated with asymptomatic severe carotid stenosis: results of a systematic review and analysis. Stroke. 2009;40:e573–83.
Hadar N, Raman G, Moorthy D, et al. Asymptomatic carotid artery stenosis treated with medical therapy alone: temporal trends and implications for risk assessment and the design of future studies. Cerebrovasc Dis. 2014;38:163–73.
Pini R, Faggioli G, Vacirca A, et al. The fate of asymptomatic severe carotid stenosis in the era of best medical therapy. Brain Inj. 2017;31:1711–7.
Abbott AL, Brunser AM, Giannoukas A, et al. Misconceptions regarding the adequacy of best medical intervention alone for asymptomatic carotid stenosis. J Vasc Surg. 2020;71:257–69.
Hackam DG. Prognosis of asymptomatic carotid artery occlusion: Systematic review and meta-analysis. Stroke. 2016;47:1253–7.
Bonati LH, Kakkos S, Berkefeld J, et al. European Stroke Organisation guideline on endarterectomy and stenting for carotid artery stenosis. Eur Stroke J. 2021;6:I–XLVII.
Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline from the American Heart Association/American Stroke Association. Stroke. 2021;52:e364-467.
Huynh K, Baghdanian AH, Baghdanian AA, et al. Updated guidelines for intravenous contrast use for CT and MRI. Emerg Radiol. 2020;27:115–26.
The Japan Society of Ultrasonics in Medicine. Standard methods for the evaluation of carotid artery lesions by ultrasound 2017. https://www.jsum.or.jp/committee/diagnostic/pdf/jsum0515_guideline.pdf. Accessed 2 Apr 2021
Saxena A, Ng EYK, Lim ST. Imaging modalities to diagnose carotid artery stenosis: progress and prospect. Biomed Eng Online. 2019;18:66.
Takekawa H, Tsukui D, Kobayasi S, et al. Point-of-care ultrasound for stroke patients in the emergency room. J Med Ultrason. 2022. https://doi.org/10.1007/s10396-021-01185-0.
European Carotid Surgery Trialists’ Collaborative Group. Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet. 1998;351:1379–87.
North American Symptomatic Carotid Endarterectomy Trial Collaborators, Barnett HJM, Taylor DW, et al. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991;325:445–53.
Koga M, Kimura K, Minematsu K, et al. Diagnosis of internal carotid artery stenosis greater than 70% with power Doppler duplex sonography. AJNR Am J Neuroradiol. 2001;22:413–7.
AbuRahma AF, Srivastava M, Stone PA, et al. Critical appraisal of the Carotid Duplex Consensus criteria in the diagnosis of carotid artery stenosis. J Vasc Surg. 2011;53:53–9.
Tokunaga K, Koga M, Yoshimura S, et al. Optimal peak systolic velocity thresholds for predicting internal carotid artery stenosis greater than or equal to 50%, 60%, 70%, and 80%. J Stroke Cerebrovasc Dis. 2016;25:921–6.
Arous EJ, Judelson DR, Malka KT, et al. Carotid duplex velocity criteria recommended by the Society of Radiologists in Ultrasound and endorsed by the Intersocietal Accreditation Commission lack predictive ability for identifying high-grade carotid artery stenosis. Ann Vasc Surg. 2019;61:227–32.
Hicks CW, Canner JK, Arhuidese I, et al. Development of a duplex-derived velocity risk prediction model of disease progression in patients with moderate asymptomatic carotid artery stenosis. J Vasc Surg. 2014;60:1585–92.
Igarashi H, Okabe R, Okamura M, et al. Influence of Doppler angle on peak systolic velocity for diagnosis of internal carotid artery stenosis. Neurosonology. 2017;30:8–12.
Tola M, Yurdakul M. Effect of Doppler angle in diagnosis of internal carotid artery stenosis. J Ultrasound Med. 2006;25:1187–92.
Society for Vascular Ultrasound. Extracranial cerebrovascular duplex ultrasound. https://higherlogicdownload.s3.amazonaws.com/SVUNET/c9a8d83b-2044-4a4e-b3ec-cd4b2f542939/UploadedImages/PPG_Docs/1__Extracranial_Cerebrovascular_Duplex_Ultrasound_Evaluation__Updated_2019_.pdf. Accessed 2 Apr 2021.
Takekawa H, Asakawa Y, Lee T, et al. Usefulness of acceleration time for assessment of stenosis in the extracranial internal carotid artery. Neurosonology. 2009;22:79–82.
Takekawa H, Suzuki K, Takada E, et al. Acceleration time ratio for the assessment of extracranial internal carotid artery stenosis. J Med Ultrason. 2014;41:63–7.
Nishihira T, Takekawa H, Suzuki K, et al. Usefulness of acceleration time ratio in diagnosis of internal carotid artery origin stenosis. J Med Ultrason. 2018;45:493–500.
Iizuka K, Takekawa H, Iwasaki A, et al. Suitable methods of measuring acceleration time in the diagnosis of internal carotid artery stenosis. J Med Ultrason. 2020;47:327–33.
O’Boyle MK, Vibhakar NI, Chung J, et al. Duplex sonography of the carotid arteries in patients with isolated aortic stenosis: imaging findings and relation to severity of stenosis. AJR Am J Roentgenol. 1996;166:197–202.
Okamura M, Takekawa H, Suzuki K, et al. Evaluation of the factors that prolong the acceleration time of the common and internal carotid arteries. Neurosonology. 2013;25:81–5.
Harmon L, Boccalandro F. Comparison of carotid artery dimensions and lesion length measured by B-mode ultrasonography and quantitative angiography in patients with severe stenosis undergoing percutaneous revascularization. J Clin Ultrasound. 2014;42:270–6.
Millet JD, Cavallo JJ, Scoutt LM, et al. Sonographic evaluation of complications of extracranial carotid artery interventions. J Ultrasound Med. 2018;37:769–81.
Müller MD, Lyrer P, Brown MM, et al. Carotid artery stenting versus endarterectomy for treatment of carotid artery stenosis. Cochrane Database Syst Rev. 2020;2:CD000515.
Clavel P, Hebert S, Saleme S, et al. Cumulative incidence of restenosis in the endovascular treatment of extracranial carotid artery stenosis: a meta-analysis. J Neurointerv Surg. 2019;11:916–23.
Bonati LH, Gregson J, Dobson J, et al. Restenosis and risk of stroke after stenting or endarterectomy for symptomatic carotid stenosis in the International Carotid Stenting Study (ICSS): secondary analysis of a randomised trial. Lancet Neurol. 2018;17:587–96.
Setacci C, Chisci E, Setacci F, et al. Grading carotid intrastent restenosis: a 6-year follow-up study. Stroke. 2008;39:1189–96.
Huang H, Wu L, Guo Y, et al. Treatment of the carotid in-stent restenosis: a systematic review. Front Neurol. 2021;12: 748304.
AbuRahma AF, Stone P, Deem S, et al. Proposed duplex velocity criteria for carotid restenosis following carotid endarterectomy with patch closure. J Vasc Surg. 2009;50:286–91.
Hagiwara Y, Yoshie T, Shimizu T, et al. A case in which contrast-enhanced transoral carotid ultrasonography was useful for pre- and post-procedural evaluation in carotid artery stenting. J Med Ultrason. 2017;44:207–10.
Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 Update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50:e344-418.
Yasaka M, Omae T, Tsuchiya T, et al. Ultrasonic evaluation of the site of carotid axis occlusion in patients with acute cardioembolic stroke. Stroke. 1992;23:420–2.
Kimura K, Yonemura K, Terasaki T, et al. Duplex carotid sonography in distinguishing acute unilateral atherothrombotic from cardioembolic carotid artery occlusion. AJNR Am J Neuroradiol. 1997;18:1447–52.
Kimura K, Yasaka M, Minematsu K, et al. Oscillating thromboemboli within the extracranial internal carotid artery demonstrated by ultrasonography in patients with acute cardioembolic stroke. Ultrasound Med Biol. 1998;24:1121–4.
Koch S, Romano JG, Park H, et al. Ultrasound velocity criteria for vertebral origin stenosis. J Neuroimaging. 2009;19:242–5.
Hua Y, Meng XF, Jia LY, et al. Color Doppler imaging evaluation of proximal vertebral artery stenosis. AJR Am J Roentgenol. 2009;193:1434–8.
Rozeman AD, Hund H, Westein M, et al. Duplex ultrasonography for the detection of vertebral artery stenosis: a comparison with CT angiography. Brain Behav. 2017;7: e00750.
Saito K, Kimura K, Nagatsuka K, et al. Vertebral artery occlusion in duplex color-coded ultrasonography. Stroke. 2004;35:1068–72.
Takekawa H, Suzuki K, Nishihira T, et al. Recurrent juvenile ischemic stroke caused by bow hunter’s stroke revealed by carotid duplex ultrasonography. J Med Ultrason. 2015;42:437–40.
Okamura M, Takekawa H, Okabe R, et al. Vertebral artery Doppler waveform patterns for exclusive diagnosis of basilar artery stenosis and occlusion. J Med Ultrason. 2016;43:83–9.
Sakima H, Wakugawa Y, Isa K, et al. Correlation between the degree of left subclavian artery stenosis and the left vertebral artery waveform by pulse Doppler ultrasonography. Cerebrovasc Dis. 2011;31:64–7.
Yasaka M, Ogata T, Yasumori K, et al. Bottle neck sign of the proximal portion of the internal carotid artery in moyamoya disease. J Ultrasound Med. 2006;25:1547–52.
Suzuki J, Takaku A. Cerebrovascular, “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969;20:288–99.
Yasuda C, Arakawa S, Shimogawa T, et al. Clinical significance of the champagne bottle neck sign in the extracranial carotid arteries of patients with Moyamoya disease. AJNR Am J Neuroradiol. 2016;37:1898–902.
Barreira SC, Melo AT, Ponte C, et al. Macaroni sign and carotid occlusion in Takayasu’s arteritis. Rheumatology (Oxford). 2021;60:2029–30.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
H.T. received lecture fees from Pfizer Japan Inc. and Daiichi Sankyo Co., Ltd. The other authors declare that there are no conflicts of interest.
Ethical approval
No ethical statements are required as this review describes the ultrasound diagnosis of carotid artery stenosis and occlusion.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Takekawa, H., Tsukui, D., Kobayasi, S. et al. Ultrasound diagnosis of carotid artery stenosis and occlusion. J Med Ultrasonics 49, 675–687 (2022). https://doi.org/10.1007/s10396-022-01259-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-022-01259-7