Abstract
Optimising ultrasonography imaging (UI) applications for clients is a highly specific and sensitive add-on method. The aim of this meta-analysis was to systematically evaluate the clinical utilisation of UI in musculoskeletal conditions by rehabilitation providers in the past decade. Two reviewers independently assessed relevant research articles from five databases electronically (Medline, Cochrane Library, EMBASE, ProQuest, EBSCO) and screened titles and abstracts based on predefined eligibility criteria (2010- 2020). A total of 147 articles were screened for eligibility by two reviewers independently, and any disagreements were resolved by another reviewer using Rayyan QCRI software. Ninety-seven duplicates were removed, and after excluding 21 studies, 16 randomized controlled trials were included and full texts retrieved. Data were synthesised using Revman 5.4 software for qualitative analysis and risk-of-bias assessment. Four similar studies were statistically analysed for heterogeneity of abdominal muscle contraction ratios. Two interventional studies were also analysed to assess the effect of feedback. The diagnostic application of UI was investigated using a consistent amount of literature, though from a rehabilitation perspective the literature is inconclusive. The clinical utility of UI in rehabilitation by physical therapists is conclusive and has potential to advance clinical practice. Further well-designed randomized controlled trials minimising selection biases will help improve the quality in this domain. Critical reflection, clinical reasoning, and mutual goal setting will help practising physical therapists to scrutinize the clinical practice more objectively.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Rehabilitative ultrasonography imaging (RUSI), the advent of which dates back to the 1980s, is a validated method in the field of rehabilitation permitting visualization for real-time study of muscles as they contract over time by measuring muscle size in relation to the other muscles [1,2,3]. Further development continued until the first meeting of the International Symposium of RUSI (Rehabilitative Ultrasonography Imaging) held in 2006 in San Antonio, Texas, which announced the theoretical framework. In an attempt to measure ‘muscle and related soft tissue morphology and function’, researchers dwelled on the upgradation of previously identified gaps within the jurisdiction which are constantly evolving [4].
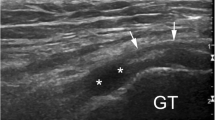
Use of musculoskeletal sonography is rapidly extending beyond its traditional implementation by radiology professionals and is no longer used exclusively as a diagnostic tool. Researchers and practitioners are beginning to document potential uses of sonography to enhance patient care in a variety of ways [5]. Variations in muscle thickness via muscle contractions can be judged by the muscle size, i.e., by measuring thickness and/or cross-sectional area, and muscle function can be assessed by the level of timing of muscle activation, all of which can present challenges that can be quantified by reliability and validity studies [6]. Motor control is very subjective and complex. Activation of muscle depends on various factors like the initial fascicle length and type of contraction [7]. Musculoskeletal ultrasonography has carved out a significant role in rehabilitation due to its many advantages (convenience, low cost, noninvasive nature, repeatability, dynamic nature, and no exposure to radiation). Real-time ultrasonography imaging (RTUI) is currently being used in physiotherapy practice to provide biofeedback of muscle activation [8].
In the past decade, two systematic reviews were published with respect to sensitivity and specificity in carpal tunnel syndrome. Albeit, there is an increasing curiosity amongst clinicians including rehabilitation providers. Clarity concerning guidelines, standardised training, and best clinical practices has always existed. Hands-on experience, definite training hours, and skill development require time, effort, and mentoring. These wavering gaps are echoed while research is being carried out worldwide [9, 10]. Past meta-analyses; systematic, scoping, and narrative reviews; and expert opinions blended well with the scope of practice and served as a reminder for regularising best clinical practices by pointing out the lacunae within the physical therapy framework [11,12,13,14,15,16,17,18].
Finally, to ensure effective implementation, consistent expert mentoring is an important component of the post-professional process, something not readily available for non-physician rehabilitation providers. It is evident that the systematic reviews conducted explored in this realm have not been revised in the past decade. A systematic review was piloted in 2019, confined to the lumbar region, abdomen, and pelvic floor, which bid to encompass the picture of how ultrasonography has influenced and prospered in the past decade with respect to physical therapy [19].
Hebert et al. in 2009 and Koppenhaver in 2011 conducted systematic reviews highlighting RUSI is a valid measure in quantitative assessment of abdominal and lumbar muscles [20]. On the other hand, Cheng in 2010 described the role of RTUI in physiotherapy evaluation of abdominal and lumbar muscles in low back pain patients. From the perspective of rehabilitation, the trend over the past decade needs to be reviewed again. Carnero in 2019 piloted a systematic review confined to the lumbo-pelvic region, in which the usage of UI in specific musculoskeletal conditions was evaluated. Considering the advantages of ultrasonography imaging (UI), a comprehensive review of the growing trend of usage of UI not only in the lumbo-pelvic region but overall, in musculoskeletal conditions, is required. A meta-analysis has not been attempted since the literature started exploding.
The objectives of this meta-analysis are as follows:
-
a.
to evaluate the clinical usage of UI in musculoskeletal conditions in studies published in 2010–2020;
-
b.
to Identify the type of usage of this tool—whether diagnostic or rehabilitative;
-
c.
to study the global distribution of clinical utilisation of UI and existing facilitators and barriers as a rehabilitative tool by physical therapists:
-
d.
to compare the TrA-CR with IOEO-CR of abdominal muscles in asymptomatic and low back pain populations in the past decade.
Methodology
Protocol and registration
This systematic review protocol was registered prospectively in the International Prospective Register and Dissemination from the University of York with the registration number PROSPERO 2020 CRD42020165340, which is available at this link: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020165340. Patients or public partners did not play a part in designing, conducting, or interpretation of this review. However, the protocol was registered as a systematic review, and after data synthesis it was compiled into a meta-analysis.
Eligibility criteria
Studies included were those published between 01 Jan 2010 and 31 Dec 2020. Included were those that used Ul as a rehabilitative tool in estimation of muscle morphology and size, conducted within a physical rehabilitation context with a rehabilitation-related diagnosis characterised by musculoskeletal conditions, done by non-physician rehabilitation providers, physical therapists, or occupational therapists. Included were level II studies (randomised controlled trials) and level III studies (cohort studies and prospective studies) that compared USG with MRI and/or EMG done on humans.
Excluded were studies conducted by radiologists or physicians solely; level I meta- analyses and systematic reviews; level V non-systematic reviews, scoping reviews, narrative reviews; level VI case series and reports; and level VII expert opinions and descriptive/educational blogs. Also excluded were reliability and validity studies, those involving therapeutic ultrasound, and studies published in languages other than English.
Databases
A comprehensive electronic search of the period from 2010 to 2020 was undertaken using five databases: Medline, Cochrane Library, EMBASE, ProQuest, and EBSCO.
Keywords
The search terms for data extraction were as follows (Table 1):
-
1.
Rehabilitative ultrasonography imaging OR Real-time ultrasonography imaging OR Sonography OR Elastography AND
-
2.
Physiotherapy OR Physical therapy AND
-
3.
Clinical utility OR Clinical utilisation AND
-
4.
Muscle thickness OR Muscle cross-sectional area AND
-
5.
Biofeedback
Selection criteria and review process
Two reviewers (SZ and TD) independently applied eligibility criteria for screening the titles and abstracts of the articles via keywords in the respective databases. The abstracts were imported and screened for eligibility in Rayyan QCRI software, which blinded the two reviewers, and duplicates were removed. Any disagreements were resolved by a third reviewer (AD) [21]. Manual search and grey literature search were done to not overlook eligible articles [22, 23]. Further qualitative analysis using Revman 5.4 software and Risk of bias assessment by the Cochrane risk of bias 2: a revised tool for assessing risk of bias in randomised trials [24].
Included RCTs were required to use UI as a primary outcome measure for measurement, or used for estimation of muscle morphology and thickness. Studies must have been published in peer-reviewed journals. Studies conducted by those other than rehabilitation providers (radiologists, physicians) were excluded. To minimise the extraneous variables, validity and reliability studies were excluded. PRISMA Guidelines for conducting a systematic review were followed for data selection, extraction, and synthesis [25].
After identifying 163 articles for screening of titles and abstracts, four articles were added by manual search and grey literature search. Rayyan QCRI software blinded the two reviewers while selecting the studies, and duplicates were automatically removed by the software. In all, 16 full-text articles were retrieved and included for analysis. The risk of bias assessment was calculated for each study. (Fig. 1). Four similar studies were statistically analysed for heterogeneity of transversus abdominis, internal oblique, and external oblique contraction ratios, which were comparable outcomes. These four studies included in the meta-analysis were selected based on type of population, muscles tested, assessment of abdominal muscles thickness, matched age-groups, and similar methodology. Two interventional studies were also analysed to assess the effect of feedback by UI on muscle thickness over a period of time.
Data extraction and quality appraisal
Assessment/categorisation of characteristics
The qualitative assessment included characteristics based on detailed methodology (Table 2 [28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43]. Extracted data were dissected in a standardised data-extraction sheet. Data included characteristics by descriptive statistics, namely, the age group, sample size, condition of the patients, and study design. Technical aspects (Table 3) of the methodology was probe position, frequency of probe, type of probe used, mode of UI, muscles assessed, test position, any comparison done with another gold standard tool, whether UI was used for biofeedback for intervention (Table 4) or otherwise and used for calculation of measurements using SPSS Statistical Software (version 23.0).
Risk of bias assessment
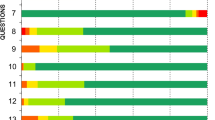
The risk of bias assessment was analysed using Revman 5.4 software with data being segregated in terms of homogeneity using the revised Cochrane risk-of-bias-assessment tool (RoB version-2). We assessed the random sequence generation, concealment of allocation, blinding of participants, personnel and outcome assessment, incomplete data outcome, selective reporting of outcomes, and other bias. The categories for classification were ‘low risk’, ‘high risk’, and ‘unclear risk’, which refers to lack of information [26].
Qualitative data synthesis
A qualitative analysis was carried out to identify the trend of characteristics between individualised studies and the common standardized procedures followed over the past decade.
Results
The comprehensive search was narrowed down to 16 RCTs that were used for further analysis. Descriptive statistics were categorised into three broad domains using SPSS software v.23.
A. Computation of common estimates in qualitative analysis
The trial population included young adults, older adults, and elderly individuals. The mean age was 50.2279 ± 275.09. The sample population varied between asymptomatic to symptomatic including mainly low back pain (specific, non-specific, acute, and chronic), shoulder impingement, and carpal tunnel syndrome. The mean sample size was computed to be 54.13 ± 53.53. Methodology wise, the common clinical practices were very standardised in terms of mid-axillary probe position (43%), muscles tested (TrA, IO, EO = 50%, Mf = 25%, Rf = 6%), and type of mode (Brightness mode = 31%, whereas 70% of studies did not mention the type of mode used). The type of probe used was linear (69%) more often than curvilinear (13%).
B. Global assessment of clinical usage of UI by physical therapists
Of the 16 studies, 75% were diagnostic versus 25% rehabilitative. The US (25%) followed by South Korea (18%) led the countries with respect to the number of publications, and maximum publications started trending from the year 2016 onwards.
C. Risk of bias (ROB) quality analysis and summary
The risk of bias of individual included studies is summarised in (Fig. 2), and the risk of bias within the studies is shown in (Fig. 3). Domains with ‘high risk’ of bias were blinding of participants, i.e., selection bias (35%) and blinding of participants and personnel (20%). Ninety percent of the studies fared well in terms of reporting complete outcome data, i.e., minimal attrition bias followed by ‘low risk’ in selective reporting (80%).
D. Analysis of heterogeneity
Two homogenous groups of studies were sorted. The first group was contraction ratios (CR) of abdominal muscles, i.e., transversus abdominis (TrA CR) versus internal and external oblique (IO + EO CR), in an asymptomatic population, whereas the second group compared the same outcomes in a low back pain population. Continuous data in both the groups were given as the mean and standard deviation (SD) with 95% confidence interval (CI). Four out of 19 studies were categorised as homogenous based on the muscles assessed, i.e., TrA, IO, and EO, in an age-matched asymptomatic population. These studies assessed the thickness of the above-mentioned muscles in relaxed and contracted states (during ADIM). The mean values of TrA CR and IO + EO CR were selected as variables for meta-analysis. Heterogeneity was assessed using an inverse variance test with a fixed effect model (I2 < 50%). A forest plot (Fig. 4) summarizes the total mean difference as 0.43 with a confidence interval of 0.38–0.49, favouring IO + EO CR on the right side of the line of no difference in the asymptomatic population. Statistical heterogeneity (I2 = 21%) is less, indicating similarity between studies, and is significant at p < 0.00001, implying the results are completely based on the variability in effect estimates rather than chance alone. Similarly, in (Fig. 5), the total mean difference is 0.32 with a confidence interval of 0.28–0.36, favouring IO + EO CR on the right side of the line of no difference in the low back pain population. Statistical heterogeneity (I2 = 0%) shows similarity between studies and is highly significant at p < 0.00001.
Discussion
This review aimed at evaluating the clinical utilisation of UI in musculoskeletal conditions by physical therapists as a rehabilitative tool for biofeedback globally. By and large, muscle activation is an important consideration in determining involuntary function activities. Objectivity can be maximised by measuring muscle morphometry whilst visualising them during its literal activation. Quantifying motor control is multifaceted. UI plays an intricate role in ‘detecting change’ in contraction due to its real-time and dynamic quality.
Many studies [44,45,46,47,48,49] have used non-weight-bearing test positions (supine-hook lying, prone) for evaluating thickness and contraction ratios, as previously pointed out by Cheng in 2010. Functional tasks involve unilateral weight bearing with bilateral activation of the evaluated muscles. In the rehabilitation context, physical therapists have already identified the probable pros and cons of UI. Despite these efforts, a dearth of understanding of maximising usage is the key. Studies have been chiefly carried out in asymptomatic populations followed by low back pain. Physical therapists can make well-informed decisions with respect to training TrA dysfunction by formulating elaborate, tailor-made, client-specific protocols. Keeping a tab on progress by documenting objective data is the need of the hour. RCTs described the methods in terms of midaxillary versus midclavicular probe position. This could easily serve as a standardised point as the midaxillary point in line with the umbilicus just above the iliac crest produces a consistent image with the thoracolumbar fascia on the top left of the image.
Selection bias was observed in 35% studies, highlighting the lacuna in random sequencing, which was not described in sufficient detail. Many studies mention recruitment of subjects via fliers, posters, and word of mouth, thereby eliminating the selection bias found in other studies. There were negligible chances of selection bias in studies with intervention allocations foreseen before or after enrolment as the subjects were recruited from clinics, local universities, and symptomatic clients compared to vulnerable populations. Eligibility criteria (attrition bias) have been extensively described in almost all studies. Blinding of participants and personnel was likely done, but studies lacked sufficient details, probably due to performance bias introduced via participant knowledge of allocation or while training them prior to procedures, for example training for the abdominal draw-in manoeuvre, or lack of skilled personnel in the study. Outcome assessment was fairly blinded as participants had less or no knowledge of which intervention he/she would receive, which was described in detail.
The forest plot for the asymptomatic population favours the IO + EO CR over the TrA CR, clearly indicating that these muscles are more activated or get activated preferentially in the case of asymptomatic individuals. Targeting the TrA muscle, therefore, becomes more than necessary, and use of any form of visual biofeedback is of utmost importance. The variability for Grooms [31] is broad but has low risk of bias in almost all domains, though Pulkovski [38] has more weightage with few unclear biases in blinding and randomisation. More trials are needed in this meta-analysis for low back pain as the entire summarisation is dependent only on two studies. More research will fuel the above result and further our understanding.
In developed countries, infrastructure and advancements in technology facilitate the prospect of UI in rehabilitation. In countries like India, however, legal jurisdiction acts as a barrier in amplifying the unawareness amongst physical therapists along with the issue of cost to a certain extent. The Indian scenario is different in view of the Pre-Conception Pre-Natal Diagnostic Techniques Act (PCPNDTA) of 1994, which was introduced by the government of India to curb female infanticide. This act regularises the use of UI by non-radiologists including physicians and physical therapists in India. The solution is to introduce training protocols and residency protocols, and enforce collaborations that will enhance mastering knowledge and skills for UI.
Barring the challenges, RUSI has been promising in the past decade. Baseline normative data have been well established in the asymptomatic population; under different conditions it needs to be explored. Use of UI is still more in the diagnostic domain, with less focus on investigation of long-term rehabilitation protocols. Standardisation has been slowly established in regard to position of probe, type of probe used, and mode of UI. More blinded RCTs augmenting the biofeedback principle in rehabilitation in weight-bearing tasks and transfer of training translating to motor control and motor learning are needed. This meta-analysis will help clinicians across the globe to put standardisation into practice, as well as add an impetus to policymakers in countries like India to consider its utilisation in clinical practice by weighing the benefits versus harm.
Conclusion
The current level of evidence for the clinical utility of UI is minimal and inconclusive. More RTCs will help us determine minimal clinical important differences and help in planning client-specific protocols for early recovery and rehabilitation. Structured RCTs and case control studies minimising biases are recommended. The current literature review has incited additional probabilities that will foster the usage of this tool by physical therapists in clinical practice.
Implications for practice and future scope
If RUSI is incorporated in physical therapy practice, the clinical outcomes will be more unbiased and independent of extraneous factors likely to affect muscle activation. As a medium of visual biofeedback, it is an excellent tool for simple understanding by both the therapist and patient, more convenient, and easily adaptable to the patient in comparison to EMG and other costly imaging tools.
Limitations
The scope of future reviews can be expanded to other areas of physiotherapy practice apart from the musculoskeletal domain. A review of reviews in the future should be highly considered.
References
Young A, Hughes I, Russell P, et al. Measurement of quadriceps muscle wasting by ultrasonography. Rheumatology. 1980;19(141):148.
Stokes M, Young A. Measurement of quadriceps cross–sectional area by ultrasonography: a description of the technique and its applications in physiotherapy. Phys Pract. 1986;2:31–6.
Hides J, Richardson C, Jull G, et al. Ultrasound imaging in rehabilitation. Aust Physiother. 1995;41:187.
Whittaker JL, Ellis R, Hodges PW, et al. Imaging with ultrasound in physical therapy: what is the PT’s scope of practice? A competency-based educational model and training recommendations. Br J Sports Med. 2019;53:1–7.
Ozeakar L, Tok F, Muynck MD, Vanderstraeten G. Musculoskeletal ultrasonography in physical and rehabilitation medicine. J rehabil med. 2012;44:310–8.
Hodges PW. Ultrasound imaging in rehabilitation: just a fad? J Orthop Sports Phys Ther. 2005;356:333–7.
Hebert JJ, Koppenhaver SL, Parent EC, Fritz JM. A systematic review of the reliability of rehabilitative ultrasound imaging for the quantitative assessment of the abdominal and lumbar trunk muscles. Spine. 2009;34:E848–56.
Van K, Hides JA, Richardson CA. The use of real-time ultrasound imaging for biofeedback of lumbar multifidus muscle contraction in healthy subjects. J Orthop Sports Phys Ther. 2006;3612:920–5.
Fowler JR, Gaughan JP, Ilyas AM. The sensitivity and specificity of ultrasound for the diagnosis of carpal tunnel syndrome: a meta-analysis. Clin Orthop Relat Res. 2011;469:1089.
Roll SC, Case-Smith J, Evans KD. Diagnostic accuracy of ultrasonography vs electromyography in carpal tunnel syndrome: a systematic review of literature. Ultrasound Med Biol. 2011;37:1539–53.
Cheng C, MacIntyre NJ. Real-time ultrasound imaging in physiotherapy evaluation and treatment of transversus abdominus and multifidus muscles in individuals with low-back pain. Phys Rehabil Med. 2011;22:279–300.
Roll SC. Clinical utilization of musculoskeletal sonography involving nonphysician rehabilitation providers: a scoping review. Eur J Phys Rehabil Med. 2016;52:253–62.
Giggins O, Persson UM, Caulfield B. Biofeedback in rehabilitation. J Neuroeng Rehab. 2013;10:60.
Whittaker J. Current perspectives: the clinical application of ultrasound imaging by physical therapists. J Man Manip Ther. 2013;14:73–5.
Nyholm GA, Johannsen F. Ultrasound therapy in musculoskeletal disorders: a meta-analysis. Pain. 1995;63:85–91.
Koppenhaver DT. Rehabilitative ultrasound imaging. J Phys. 2011;57:196.
Dinnes J, Loveman E, McIntyre L, Waugh N. The effective- ness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review. Healthiness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review. Health Techno Assess. 2003;7:1–166.
Ottenheijam R, Jansen M, Staal B, et al. Accuracy of diagnostic ultrasound in patients with suspected subacromial disorders: a systemic review and meta analysis. Arch Phys Med Rehabil. 2010;91:1616.
Fernández SC. Rehabilitative ultrasound imaging evaluation in physiotherapy: piloting a systematic review. App Sci. 2018;9:1–14.
Koppenhaver SL, Hebert JJ, Parent EC, Fritz JM. Rehabilitative ultrasound imaging is a valid measure of trunk muscle size and activation during most isometric sub-maximal contractions: a systematic review. Aust J Physiother. 2009;55:153–69.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Control Found Appl. 2016;5:210.
Khan KS, Kunz R, Kleijnen J, Antes G. Five steps to conducting a systematic review. J R Soc Med. 2003;96:118–21.
Tawfik GM, Dila KAS, Mohamed F, et al. A step-by-step guide for conducting a systematic review and meta-analysis with simulation data. Trop Med Health. 2019;47:46.
Sterne JAC, Savović J, Page MJ, Elbers RG, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Moher D, Liberati A, Tetzlaff J, Altman D, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Review Manager (RevMan) [Computer program]. Version 5.4, The Cochrane collaboration. 2020.
Arimi ASM. Multifidus muscle size changes at different directions of head and neck movements in females with unilateral chronic non-specific neck pain and healthy subjects in ultrasonography. J of Body work Movt Thera. 2018;22:560–5.
Cadogan A, McNair PJ, Laslett M, Hing WA. Diagnostic accuracy of clinical examination and imaging findings for identifying subacromial pain. PLoS ONE. 2016;11:e0167738.
Hyun-Gyu C. Is abdominal hollowing excerciseusing real-time ultrasound imaging feedback helpful for selective strengthening of transversus abdominis muscle? Med. 2018;97:1–7.
Dabholkar SA, Shetty S. Effects of mobilization with movement (MWM) in shoulder impingement syndrome patients on acromio humeral distance using ultrasonography. J Ex Sc Phys. 2016;12:28–33.
Grooms DR, Grindstaff TL, Croy T, Hart JM, et al. Clinimetric analysis of pressure biofeedback and transversus abdominis function in individuals with stabilization classification low back pain. J Orthop Sports Phys Ther. 2013;43:184–93.
Gulcan H, Michener L. Active scapular retraction and acromiohumeral distance at various degrees of shoulder abduction. J Athl Train. 2018;53:584–9.
Larivière C, Henry SM, Gagnon DH, Preuss R, Dumas JP. Ultrasound measures of the abdominal wall in patients with low back pain before and after an 8-week lumbar stabilization exercise program, and their association with clinical outcomes. Phy Med Rehab. 2019;11:710–21.
Sangyong L. Comparison of abdominal muscle thickness according to feedback method used during abdominal hollowing exercise. J Phys Ther Sci. 2016;28:2519–21.
Nuzzo JL, Haun DW, Mayer JM. Ultrasound measurements of lumbar multifidus and abdominal muscle size in firefighters. J Back Musculo Rehab. 2014;27:427–33.
Pamboris GM. Effects of an acute bout of dynamic stretchingon biomechanical properties of the gastrocnemius muscle determined by shear wave elastography. PLoS ONE. 2018;13:e0196724.
Park DJ. What is a suitable pressure for the abdominal drawing-in maneuver in the supine position using a pressure biofeedback unit? J Phys Ther Sci. 2013;25:527–30.
Pulkovski N, Mannion AF, Caporaso F, et al. Ultrasound assessment of transversus abdominis muscle contraction ratio during abdominal hollowing: a useful tool to distinguish between patients with chronic low back pain and healthy controls? Eur Spine J. 2012;21:S750–9.
Chowdhury SC, Savani N. Efficacy of Pilate’s exercise for strengthening of deep abdominal muscles in asymptomatic adult individuals. Eur J Pharm Med Res. 2016;3:239–47.
Sutherlin MA, Russell SA. Changes in muscle thickness across positions on ultrasound imaging in participants with or without a history of low back pain. J Athl Train. 2018;53:553–9.
Tahan N. Measurement of superficial and deep abdominal muscle thickness: an ultrasonography study. J Phys Anthr. 2016;35:17.
Yang C. Musculoskeletal ultrasonography assessment of functional magnetic stimulation on the effect of glenohumeral subluxation in acute poststroke hemiplegic patients. Hindawi Biomed Res Int. 2018;208:1–9.
Moreau B. Non-invasive assessment of human multifidus muscle stiffness using ultrasound shear wave elastography: a feasibility study. J Eng Med. 2016;230:809.
Jhu JL, Chai HM, Jan MH, Wang CL, Shau YW, et al. Reliability and relationship between 2 measurements of transversus abdominis dimension taken during an abdominal drawing-in maneuver using a novel approach of ultrasound imaging. J Ortho Sports Phys Ther. 2016;40:826.
Sions J, Megan PD. Reliability of ultrasound imaging for the assessment of lumbar multifidi thickness in older adults with chronic low back pain. J Geriatr Phys Ther. 2015;38:33–9.
Trilos MC. Upper limb neurodynamic test 1 in patients with clinical diagnosis of carpal tunnel syndrome. Man Ther. 2011;16:258–63.
Pawel N. Reliability of the ultrasound measurements of deep abdominal muscle in rehabilitative practice. J Orthop Trauma Surg Rel Res. 2016;2017:1–23.
Silva C. Quadriceps muscle architecture ultrasonography of individuals with type 2 diabetes: reliability and applicability. PLoS ONE. 2018;13:1–9.
Higgins J, Green S. Cochrane Handbook for systematic reviews of interventions version 5.10. 2011. www.cochrane-handbook.org. Accessed 27 Sept 2020.
Acknowledgements
We would like to thank and acknowledge Dr. Anant Patil for his contribution as a reviewer.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Summaiya Zareen Shaikh, Tejashree Dabholkar, and Ajit Dabholkar declare that they have no conflicts of interest.
Ethical statement
An ethical statement is not required as it a review article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Shaikh, S.Z., Tejashree, D. & Ajit, D. Clinical utility of ultrasonography imaging in musculoskeletal conditions: A Systematic review and Meta-analysis. J Med Ultrasonics 48, 285–294 (2021). https://doi.org/10.1007/s10396-021-01104-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-021-01104-3