Abstract
Introduction and purpose
Estimation of the contractility of the left ventricle during exercise is an important part of the rehabilitation protocol. It is known that cardiac contractility increases with an increase in heart rate. This phenomenon is called the force–frequency relation (FFR). Using wave intensity, we aimed to evaluate FFR noninvasively during graded exercise.
Methods
We enrolled 83 healthy subjects. Using ultrasonic diagnostic equipment, we measured wave intensity (WD), which was defined in terms of blood velocity and arterial diameter, in the carotid artery and heart rate (HR) before and during bicycle ergometer exercise. FFRs were constructed by plotting the maximum value of WD (WD1) against HR. We analyzed the variation among FFR responses of individual subjects.
Results
WD1 increased linearly with an increase in HR during exercise. The average slope of the FFR was 1.0 ± 0.5 m/s3 bpm. The slope of FFR decreased with an increase in body mass index (BMI). The slopes of FFRs were steeper in men than women, although there were no differences in BMI between men and women.
Conclusions
The FFR was obtained noninvasively by carotid arterial wave intensity (WD1) and graded exercise. The slope of the FFR decreased with an increase in BMI, and was steeper in men than women.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In an exercise program for patients with heart disease, it is important to assess the cardiac contractility during exercise. Normally, cardiac contractility increases with an increase in heart rate (HR), which is called the force–frequency relation (FFR) [1,2,3,4,5]. It is also known that HR increases together with an increase in the intensity of exercise load in humans. Exercise has been found to markedly enhance the positive FFR in healthy dogs and humans [4, 5]. However, the behavior of FFR during exercise in patients with cardiovascular disease differs from that in healthy individuals [6,7,8,9,10,11,12,13,14,15,16,17,18].
In conventional methods of obtaining FFRs, the maximum rate of left ventricular (LV) pressure rise (peak dP/dt) measured with a catheter-tipped micromanometer was used as an index of cardiac contractility, and atrial pacing was used to change HR (peak dP/dt–HR relation). In spite of its potential for evaluating cardiac function during exercise, the peak dP/dt–HR relation has not been widely used because of its invasive nature.
The conventional carotid arterial wave intensity (WI), which is defined in terms of blood velocity and arterial pressure, and is noninvasively measured with a combined system of color Doppler and echo tracking, has been reported to be a sensitive index of LV contractility [19,20,21,22,23,24,25].
We applied WI in evaluating LV contractility during exercise to obtain FFR, and studied the variation in FFR among healthy individuals. In addition, we analyzed changes in HR with an increase in workload (HR–workload relations).
Methods
Noninvasive measurements of wave intensity
WD is defined by the following equation:
where dD/dt and dU/dt are the derivatives of arterial diameter (D) and arterial blood flow velocity (U) with respect to time, respectively. It has been reported that diameter-change waveforms and blood velocity waveforms in the carotid artery are measured simultaneously and noninvasively with a combined system of color Doppler and echo tracking incorporated in an ultrasonic diagnostic unit (ProSound α10; Hitachi, Tokyo, Japan) [22]. The system also yields carotid arterial WD. The positive first peak of WD during the initial ejection period (WD1 in Fig. 1a) is related to left ventricular peak dP/dt [26]. FFRs were constructed by plotting WD1 against HR.
a Representative recordings of carotid arterial diameter (D), blood flow velocity (U), calculated wave intensity (WD), and electrocardiogram (ECG) obtained from a healthy individual. b Simultaneous measurements of diameter-change waveform and blood flow velocity. Data were acquired from the common carotid artery at about 2 cm proximal to the carotid bulb. View on the monitor during the measurements: left color doppler/B-mode long-axis view of the common carotid artery. The yellow-green line (A) and the sky blue line (B) indicate the ultrasonic beam for echo tracking and for blood flow velocity measurement, respectively. By setting the tracking positions displayed as small yellow-green bars on the echo-tracking beam to arterial walls, echo tracking automatically starts. The blood flow velocity averaged along the Doppler beam (sky blue line) crossing the artery was measured using range-gated color Doppler signals (color of the blood flow velocity is removed to indicate the tracking bars clearly). Right The diameter-change waveform (C), which is calculated by subtracting the distance to the near wall from that to the far wall (A′–A′), and the velocity waveform is displayed on the M-mode view (B′)
Subjects
We studied 83 healthy volunteers (52 men, mean age 20.8 ± 1.5 years, age range 18–28 years). We obtained informed consent from all of the subjects (Table 1). Approval from the Ethics Committee of Himeji Dokkyo University was obtained before study initiation.
Protocol
Before measuring WD1 and HR, the subjects lay down in the supine position for 10 min. The location to be measured was the common carotid artery at about 2 cm proximal to the carotid bulb. We used scanning in the long-axis view, and obtained a B-mode image of a longitudinal section of the artery. Optimal images were best achieved by positioning and orienting the probe so that clear and parallel delineation of the intima–media complex at both the anterior and posterior walls could be seen. The echo-tracking beam was steered so that it was orthogonal to the arterial walls. With the B- and M-mode scans displayed simultaneously on a split screen, the echo-tracking system tracked the vessel wall movements to produce displacement waveforms of the anterior and posterior artery walls, which yielded diameter-change waveforms (Fig. 1b). After measuring WD1 and HR at rest, graded bicycle exercise was performed starting at an initial workload of 20 W and lasting for 2 min; thereafter, the workload was increased stepwise by 20 W at 1-min intervals. Electrocardiogram was continuously monitored. The blood pressure was measured approximately every 30 s. Data were recorded continuously for 20 s at each step of graded exercise. Five consecutive beats were selected at each step to obtain the ensemble-averaged waveform as the representative waveform at that step. Criteria for interrupting the test were maximal predicted heart rate [(220-age) × 0.8], systolic blood pressure >200 mmHg, and signs of fatigue to end exercise.
Data analysis
Statistical analysis: data are expressed as mean ± SD. Correlation between WD1 and HR was assessed by the linear regression method before and during exercise. The regression line was interpreted as the FFR. A value of p <0.05 was considered statistically significant.
Results
Subject baseline data are shown in Table 1. Hemodynamic data at peak load are shown in Table 2. HR increased linearly with an increase in workload in all subjects. Figure 2a shows a representative relation between HR and workload. The goodness-of-fit of the regression line of HR on workload in each subject was very high (r2 = 0.94 ± 0.04). The slopes (k) of the HR–workload relations were steeper in women than in men (0.59 ± 0.14 vs 0.46 ± 0.21 bpm/W, p < 0.0001) (Fig. 2b). WD1 increased linearly with an increase in HR. Figure 3 shows a representative relation between WD1 and HR. The goodness-of-fit of the regression line of WD1 on HR in each subject was very high (r2 = 0.7 ± 0.2).
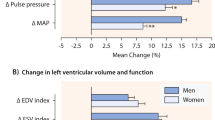
The slope (k) of the WD1–HR relation (FFR) varied with the individual, ranging from 0.30 to 2.89 (m/s3 bpm). k was smaller for greater BMI (k = − 0.04 BMI + 1.92, p <0.05) (Fig. 4a). The slopes were gentler in women than in men (0.72 + 0.23 m/s3 bpm vs. 1.14 + 0.62 m/s3 bpm, p < 0.001.) (Fig 4b) although there was no difference in BMI between men and women (p = 0.46) (Table 1).
WD1 also increased linearly with an increase in workload. Figure 4c shows a representative relation between WD1 and workload. The goodness-of-fit of the regression line of WD1 on workload was rather high (r2 = 0.65±0.23). There was no difference in the slope (M) of the regression line of WD1 on workload between men and women (Fig. 4d).
The coefficient of variation for the measurement of FFR was assessed in 20 subjects. The coefficient of variation was 0.20, which was within the clinically practical range.
Discussion
Evaluation of the changes in the contractile state of the left ventricle during exercise is an important part of the cardiac rehabilitation protocol. The positive inotropic effect of increased heart rate (HR) produced by pacing has been demonstrated in healthy individuals, which has been called the force–frequency relation (FFR) [3,4,5]. In conventional methods of obtaining FFRs, the maximum rate of left ventricular (LV) pressure rise (peak dP/dt) measured with a catheter-tipped micromanometer was used as an index of cardiac contractility, and atrial pacing was used to change HR (peak dP/dt–HR relation). Instead of invasive atrial pacing, we applied graded exercise. During the exercise, HR increased linearly with an increase in workload (Fig. 2a); therefore, atrial pacing was not needed for changing HR. In normal hearts, the peak dP/dt–HR relation is markedly enhanced (the slope is increased) during exercise compared with during pacing, which is due to β-adrenergic stimulation induced by exercise [3,4,5]. The peak dP/dt–HR relation (FFR) during exercise is significantly affected by a variety of heart diseases, and has the sensitivity to detect contractile impairment [1,2,3,4,5,6,7,8,9,10]. In spite of its potential for evaluating cardiac function during exercise, peak dP/dt–HR relation has not been widely used because of its invasive nature.
Instead of measuring peak dP/dt with a catheter, we measured carotid arterial wave intensity (WD) noninvasively using a combined system of color Doppler and echo tracking. The definition of WD (Eq. (1)) is different from the conventional definition of wave intensity (WI), which is
where dP/dt and dU/dt are the derivatives of blood pressure (P) and velocity (U) with respect to time, respectively [22]. Both wave intensities are related as follows [26]:
where β is the stiffness parameter, which is defined as
where Ps and Pd are the systolic and diastolic pressures, and Ds and Dd are the systolic and diastolic diameters, respectively.
We have reported that the maximum value of WI (W1) during a cardiac cycle correlates with peak dP/dt [21]. Therefore, the maximum value of WD (WD1) also correlates with peak dP/dt. WD contains (1/β), and β increases with an increase in age, though WI does not depend on age. This dependency of WD on age is a disadvantage of WD as an index of cardiac contractility. To obtain WI, it is necessary to measure upper arm systolic and diastolic pressures with a sphygmomanometer at each step of graded exercise. This is rather a hard task. On the other hand, WD is obtained by measuring U and D without measuring upper arm pressures. Nevertheless, our study group ranged in age from 18 to 28 years. Therefore, we do not have to consider the dependence of WD on age.
The slope (k) of WD1–HR relation (FFR) decreased with an increase in BMI (Fig. 4a). The mechanism of this phenomenon is unclear. Nevertheless, Seo et al. [27] reported the relations between BMI and echocardiographic indices of diastolic function in subjects with normal hearts. In their study, the participants were classified as normal weight (BMI < 23.0 kg/m2), overweight (BMI 23.0–27.4 kg/m2), or obese (BMI ≥ 27.5 kg/m2). In their multivariate analyses, BMI was independently associated with higher A (late transmitral velocity), lower E′ (early diastolic mitral annulus velocity), and higher E/E′ (E = early transmitral velocity). The risk of diastolic dysfunction was significantly higher among overweight and obese participants. Janssen [28] reported strong coupling between contraction and relaxation of the myocardium. The force of contraction and the speed of relaxation increased with an increase in contraction frequency. Although the mechanisms responsible for the relation between k and BMI are currently unclear, the contraction–relaxation coupling may account for the decrease in k with an increase in BMI, at least in part. In addition, k was steeper in men than in women (Fig. 4b) although there was no difference in BMI between men and women in our study group (Table 1). The slope (k) of the HR–workload relation was steeper in women than in men (Fig. 2b). We also studied the relation between WD1 and workload (Fig. 4c) although this relation was not validated as an index of cardiac function and was rarely used. There was no difference in the slope (M) of the WD1–workload relation between men and women (Fig. 4d). Thus, the same level of workload causes a greater increase in HR in women than in men, but causes the same level of increase in WD1 both in men and women. This explains superficially the reason why the slope (k) was steeper in men than in women. However, the real underlying mechanism is unclear.
Limitation
The final goal of our study was to apply the noninvasive method of measuring the force–frequency relation to cardiac rehabilitation. However, we did not enroll patients with heart disease in the present feasibility study. Although the WD1–HR relation depends on age, our study subjects only ranged from 18 to 28 years old. We should enroll a greater number of subjects with a wider age range and divide them into age groups in a future study.
Conclusions
Using an ultrasonic system to measure wave intensity and graded exercise to change heart rate, we developed a noninvasive method of obtaining the force–frequency relation (FFR). The slope of obtained FFR decreased with an increase in BMI. The slope of FFR was steeper in men than women, despite there being no difference in BMI between men and women.
References
Alpert NR, Leavitt BJ, Ittleman FP, et al. A mechanistic analysis of the force–frequency relation in non-failing and progressively failing human myocardium. Basic Res Cardiol. 1998;93:23–32.
Hove-Madsen L, Gesser H. Force frequency relation in the myocardium of rainbow trout. Effects of K+ and adrenaline. J Comp Physiol B. 1989;159:61–9.
Kambayashi M, Miura T, Oh BH, et al. Enhancement of the force–frequency effect on myocardial contractility by adrenergic stimulation in conscious dogs. Circulation. 1992;86:572–80.
Miura T, Miyazaki S, Guth BD, et al. Influence of the force–frequency relation on left ventricular function during exercise in conscious dogs. Circulation. 1992;86:563–71.
Ross J Jr, Miura T, Kambayashi M, et al. Adrenergic control of the force–frequency relation. Circulation. 1995;92:2327–32.
Bhargava V, Shabetai R, Mathiasen RA, et al. Loss of adrenergic control of the force–frequency relation in heart failure secondary to idiopathic or ischemic cardiomyopathy. Am J Cardiol. 1998;81:1130–7.
Kass DA. Force–frequency relation in patients with left ventricular hypertrophy and failure. Basic Res Cardiol. 1998;93:108–16.
Maier LS, Schwan C, Schillinger W, et al. Gingerol, isoproterenol and ouabain normalize impaired post-rest behavior but not force–frequency relation in failing human myocardium. Cardiovasc Res. 2000;45:913–24.
Morimoto R, Okumura T, Bando YK, et al. Biphasic force–frequency relation predicts primary cardiac events in patients with hypertrophic cardiomyopathy. Circulation. 2017;81:368–75.
Mulieri LA, Hasenfuss G, Leavitt B, et al. Altered myocardial force–frequency relation in human heart failure. Circulation. 1992;85:1743–50.
Mulieri LA, Leavitt BJ, Wright RK, et al. Role of cAMP in modulating relaxation kinetics and the force–frequency relation in mitral regurgitation heart failure. Basic Res Cardiol. 1997;92:95–103.
Mulieri LA, Tischler MD, Martin BJ, et al. Regional differences in the force–frequency relation of human left ventricular myocardium in mitral regurgitation: implications for ventricular shape. Am J Physiol Heart Circ Physiol. 2005;288:H2185–91.
Mullens W, Bartunek J, Tang WH, et al. Early and late effects of cardiac resynchronization therapy on force–frequency relation and contractility regulating gene expression in heart failure patients. Heart Rhythm. 2008;5:52–9.
Pieske B, Kretschmann B, Meyer M, et al. Alterations in intracellular calcium handling associated with the inverse force–frequency relation in human dilated cardiomyopathy. Circulation. 1995;92:1169–78.
Schmidt U, Schwinger RH, Bohm M, et al. Alterations of the force–frequency relation depending on stages of heart failure in humans. Am J Cardiol. 1994;74:1066–8.
Schotten U, Voss S, Wiederin TB, et al. Altered force–frequency relation in hypertrophic obstructive cardiomyopathy. Basic Res Cardiol. 1999;94:120–7.
Schwinger RH, Bohm M, Koch A, et al. Force–frequency relation in human heart failure. Circulation. 1992;86:2017–8.
Vollmann D, Luthje L, Schott P, et al. Biventricular pacing improves the blunted force–frequency relation present during univentricular pacing in patients with heart failure and conduction delay. Circulation. 2006;113:953–9.
Miao DM, Ye P, Zhang JY, et al. Clinical usefulness of carotid arterial wave intensity in noninvasively assessing left ventricular performance in different hypertensive remodeling hearts. Zhongguo Ying Yong Sheng Li Xue Za Zhi. 2011;27:136–9.
Niki K, Sugawara M, Chang D, et al. A new noninvasive measurement system for wave intensity: evaluation of carotid arterial wave intensity and reproducibility. Heart Vessels. 2002;17:12–21.
Ohte N, Narita H, Sugawara M, et al. Clinical usefulness of carotid arterial wave intensity in assessing left ventricular systolic and early diastolic performance. Heart Vessels. 2003;18:107–11.
Sugawara M, Niki K, Ohte N, et al. Clinical usefulness of wave intensity analysis. Med Biol Eng Comput. 2009;47:197–206.
Vriz O, Favretto S, Jaroch J, et al. Left ventricular function assessed by one-point carotid wave intensity in newly diagnosed untreated hypertensive patients. J Ultrasound Med. 2017;36:25–35.
Wang Z, Jalali F, Sun YH, et al. Assessment of left ventricular diastolic suction in dogs using wave-intensity analysis. Am J Physiol Heart Circ Physiol. 2005;288:H1641–51.
Zhang H, Zheng R, Qian X, et al. Use of wave intensity analysis of carotid arteries in identifying and monitoring left ventricular systolic function dynamics in rabbits. Ultrasound Med Biol. 2014;40:611–21.
Tanaka M, Sugawara M, Ogasawara Y, et al. Noninvasive evaluation of left ventricular force–frequency relationships by measuring carotid arterial wave intensity during exercise stress. J Med Ultrason. 2015;42:65–70.
Seo JS, Jin HY, Jang JS, et al. The relationships between body mass index and left ventricular diastolic function in a structurally normal heart with normal ejection fraction. Cardiovasc Ultrasound. 2017;25:5–11.
Janssen PML. Myocardial contraction-relaxation coupling. Am J Physiol Heart Circ Physiol. 2010;299:H1741–9.
Acknowledgements
This work was supported in part by the Grant-in-Aid for Scientific Research (C 16k01570 and C 16H04264) from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical statement
All studies involved in this manuscript received approval from the Ethics Committee of Himeji Dokkyo University before study initiation. All subjects provided written informed consent prior to measurements.
Conflict of interest
The authors declare that they have no conflicts of interest.
About this article
Cite this article
Tanaka, M., Sugawara, M., Niki, K. et al. Changes in cardiac contractility during graded exercise are greater in subjects with smaller body mass index, and greater in men than women: analyses using wave intensity and force–frequency relations. J Med Ultrasonics 46, 63–68 (2019). https://doi.org/10.1007/s10396-018-0888-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-018-0888-8