Abstract
A 67-year-old man consulted our department with gross hematuria. Computed tomography (CT) revealed a huge renal tumor with a paracaval metastatic lymph node (mLN). Right total nephrectomy was planned for the renal tumor diagnosed as renal cell carcinoma preoperatively. Just before the resection of the renal vein and artery, intraoperative ultrasonography revealed an inferior vena caval tumor thrombus (IVCTT) extending from the mLN. Ultrasonography clearly and dynamically demonstrated a rhythmic flapping movement of the IVCTT with blood flow in the inferior vena cava. Following right radical nephrectomy, IVCTT resection with the vessel wall was performed to reduce the risk of pulmonary tumor thrombus. Histopathological diagnosis of the renal tumor was clear cell renal cell carcinoma, and the resected IVCTT was confirmed histopathologically as tumor involvement from the mLN of the renal cell carcinoma. Intraoperative ultrasonography can detect IVCTT extending from the mLN, whereas CT cannot.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal cell carcinoma (RCC) tends to extend into blood vessels, and tumor thrombus is one of the characteristic progression forms of RCC. Extension of RCC into the renal vein and inferior vena cava (IVC), in particular, is problematic for the prognosis and surgical management of RCC, given that pulmonary tumor thrombus (PTT) can cause sudden death. Inferior vena caval tumor thrombus (IVCTT) from the primary tumor is indicative of a poor prognosis in cases of RCC [1]. Computed tomography (CT), magnetic resonance imaging (MRI), and ultrasonography (US) are used for the detection of IVCTT preoperatively, and US can be a useful modality to determine the size and location of IVCTT intraoperatively. On the other hand, an IVCTT extending from a metastatic lymph node (mLN) is extremely rare in RCC, whereas a primary tumor of RCC can sometimes have IVCTT itself. Here, we report a case of RCC with IVCTT extending from the mLN. Intraoperative US was useful to detect IVCTT extending from the mLN, and it helped to avoid PTT.
Case report
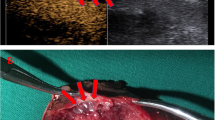
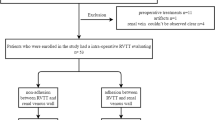
A 67-year-old man with gross hematuria consulted our department. CT revealed a huge renal tumor with a paracaval mLN (Fig. 1a, b). A small tumor thrombus in the right gonadal vein was detected by CT 14 days before surgery (Fig. 1c). However, CT did not reveal any tumor thrombus extending from the primary tumor in the IVC (Fig. 1d). MRI was not performed, and US did not reveal IVCTT. The patient required blood transfusion for anemia induced by hematuria. Right radical nephrectomy was planned for the renal tumor. Lymphadenectomy following radical nephrectomy was one of the treatment options depending on the intraoperative findings. Just before resection of the renal vein and artery, intraoperative US was performed to detect the tumor thrombus in the right gonadal vein, and also to evaluate mLN adhesion to the IVC. US images were obtained on a HI VISION Preirus (Hitachi Medical, Tokyo, Japan) with a linear probe (5–18 MHz). US attached to the IVC detected a small tumor in the right gonadal vein, and the safety margin of resection was confirmed. In addition, US incidentally revealed a floating IVCTT extending from the mLN in a teardrop shape in B-mode and color Doppler mode (Fig. 2a, b). A rhythmic flapping movement of the IVCTT synchronized with blood flow in the IVC was observed by US (Fig. 2c, d, e). IVCTT resection with the vessel wall of the IVC was performed to reduce the risk of PTT. The metastatic lymph node was adhesive to the surrounding tissue. We gave up on removing the lymph node. However, considering the possibility of sudden death due to PTT, we decided to remove the IVCTT with resection of the vessel wall with tumor invasion. The histopathological diagnosis was clear cell renal cell carcinoma (G3, pT3a). The resected IVCTT contained histopathological components similar to those of the primary tumor, and was tightly connected to the vessel wall (Fig. 3a, b). IVCTT extending from the mLN was confirmed histopathologically (Fig. 3c). The patient received temsirolimus (25 mg/week) for 7 months and axitinib (10 mg/day) for 3 months as treatment for the mLN. After induction of chemotherapy, multiple metastases were detected in the lungs and skin, and the patient died due to respiratory insufficiency induced by a metastatic lung tumor 15 months after the surgery.
Computed tomography (CT) images in the present case. a CT revealed a huge hypervascular tumor on the right kidney with a diameter of 10 cm (arrowhead). b A metastatic lymph node (arrowhead) was detected on the inferior vena cava (arrow). c A small tumor thrombus (arrow) was detected in the right gonadal vein. d CT was not able to detect the tumor thrombus extending from the metastatic lymph node (arrowhead) in the inferior vena cava (arrow)
Ultrasonographic images of the present case. a A floating tumor thrombus (arrowhead) was detected in the inferior vena cava connecting to the metastatic lymph node. b A floating tumor (arrowhead) was clearly observed in color Doppler mode. c–e Flapping movement of the tumor thrombus (arrowhead) could be observed dynamically
Histopathological findings of the resected tumor thrombus. a Gross appearance of the resected tumor thrombus (arrow) and vessel wall (arrowhead). b Hematoxylin and eosin staining of the resected tumor thrombus. The floating tumor thrombus (arrow) showed histopathological findings similar to those of the primary tumor on the right kidney, and was tightly connected to the vessel wall (arrowhead). c A close-up view of the area in the black box in (b). The tumor (arrow) progressed from the vessel wall to the interior of the inferior vena cava. These findings indicated that the floating tumor thrombus came from the metastatic lymph node
Discussion
IVCTT associated with RCC is rare, accounting for 4–10% of all RCC cases [2, 3]. As an aggressive surgical approach is the mainstay of treatment for these patients, good presurgical planning depends on the reliable determination of IVCTT level, such as renal vein or IVC. Preoperatively, it is necessary to determine the presence of IVCTT to plan the surgical approach. Advances in MRI, CT, and US techniques, including color Doppler US, have enhanced our ability to detect IVCTT and plan the surgical treatment. Several studies have evaluated the abilities of MRI, CT, and US to detect tumor thrombus extension [4,5,6]. Goldfarb et al. [4] and Laissy et al. [6] demonstrated the superiority of MRI for the detection of IVCTT at the intrahepatic, hepatic, and suprahepatic levels. Moreover, intraoperative monitoring of patients with IVCTT extending into the right atrium represents the only indication for transesophageal US [7]. These reports have suggested that CT can detect IVCTT located lower than the hepatic level, MRI is superior to CT for the detection of IVCTT at the hepatic level, and transesophageal US can detect IVCTT in the right atrium. In particular, US is a useful modality for dynamically observing movement of the IVCTT during the surgical approach.
IVCTT extending from the mLN is extremely rare. To our knowledge, there have been no previous reports in the English literature of cases similar to that presented here. The difficulty in detecting IVCTT flapping in blood flow may have influenced the rarity of such reports, and CT cannot detect moving targets. In fact, transabdominal US and CT could not detect the IVCTT extending from the mLN in this case. Transabdominal US is sometimes subject to interference by colonic gas and other organs preventing observation of deep areas in the human body. CT is also not useful for examining a moving target, whereas US can be used for such targets at high frame rates. Moreover, a high-frequency US probe was used intraoperatively to observe the interior of the IVC in this case, yielding clear images and movies that allowed us to detect the IVCTT. These factors may have impacted the useful findings of intraoperative diagnosis of IVCTT by US in this case.
Indeed, we did not perform MRI in this patient. However, we did not assume IVCTT from mLN, which could not be detected by CT. Of course, the usefulness of MRI for the detection of a flapping IVCTT is debatable, and intraoperative US may be superior to MRI for detecting a moving target, as in the present case. Although our patient died due to a metastatic lung lesion, local surgical management may improve the prognosis. Considering all of the limitations in this case presentation, intraoperative US should be considered before surgery for RCC with mLN to avoid PTT.
Conclusion
Intraoperative US is useful for detecting IVCTT extending from the mLN. Intraoperative detection of IVCTT may be beneficial to avoid PTT. Further investigations are needed to evaluate the epidemiology of IVCTT extending from the mLN, and to determine the precise role of intraoperative US in detecting IVCTT extending from the mLN.
References
Giuliani L, Giberti C, Martorana G, Rovida S. Radical extensive surgery for renal cell carcinoma: long-term results and prognostic factors. J Urol. 1990;143:468–73 (discussion 473-64).
Hoehn W, Hermanek P. Invasion of veins in renal cell carcinoma—frequency, correlation and prognosis. Eur Urol. 1983;9:276–80.
Novick AC, Cosgrove DM. Surgical approach for removal of renal cell carcinoma extending into the vena cava and the right atrium. J Urol. 1980;123:947–50.
Goldfarb DA, Novick AC, Lorig R, et al. Magnetic resonance imaging for assessment of vena caval tumor thrombi: a comparative study with venacavography and computerized tomography scanning. J Urol. 1990;144:1100–3 (discussion 1103-4).
Hallscheidt P, Pomer S, Roeren T, Kauffmann GW, Staehler G. Preoperative staging of renal cell carcinoma with caval thrombus: is staging in MRI justified? Prospective histopathological correlated study. Urologe A. 2000;39:36–40.
Laissy JP, Menegazzo D, Debray MP, et al. Renal carcinoma: diagnosis of venous invasion with Gd-enhanced MR venography. Eur Radiol. 2000;10:1138–43.
Sigman DB, Hasnain JU, Del Pizzo JJ, Sklar GN. Real-time transesophageal echocardiography for intraoperative surveillance of patients with renal cell carcinoma and vena caval extension undergoing radical nephrectomy. J Urol. 1999;161:36–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
This case report was approved by the Ethics Committee of Shinshu University School of Medicine (Permission No. 3741-2017).
About this article
Cite this article
Minagawa, T., Fukui, D., Shingu, K. et al. Intraoperative detection of inferior vena caval tumor thrombus extending from metastatic lymph node of renal cell carcinoma using ultrasonography. J Med Ultrasonics 45, 367–370 (2018). https://doi.org/10.1007/s10396-017-0838-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-017-0838-x