Abstract
Purpose
To investigate whether a novel method that combines breast imaging reporting and data system (BI-RADS) with strain elastography contributes to diagnostic performance in differentiation of malignant and benign breast lesions.
Methods
In 81 patients, 81 breast lesions were prospectively investigated. Breast lesions were separately evaluated with ultrasonography and strain elastography. While evaluations with ultrasonography were based on 2003 BI-RADS-US, strain elastography evaluations were based on a 5-point scale and strain ratio. Diagnostic performances of ultrasonography, strain elastography, and the combined method were compared.
Results
Among 81 lesions, 43 (53.1%) were benign and 38 (46.9%) were malignant. When a cutoff point of category 3 was used, sensitivity, specificity, positive and negative predictive values, and accuracy for BI-RADS were 100, 11.6, 50, 100, and 53%, respectively. When BI-RADS and strain ratio were combined, sensitivity, specificity, positive and negative predictive values, and accuracy were 89.5, 93, 91.9, 90.9, and 91.3%, respectively. When BI-RADS and elastography scores were combined, sensitivity, specificity, positive and negative predictive values, and accuracy were 86.8, 97.7, 97.1, 89.4, and 92.5%, respectively.
Conclusions
The combination of strain elastography and BI-RADS was found to have better diagnostic performances to diagnose breast lesions than BI-RADS alone.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breast cancers are among the most common types of cancers in both developing and developed countries [1]. Compared to other methods, breast ultrasonography (US) is the first-line noninvasive imaging modality in clinical practice. Conventional US can be used to distinguish between benign breast lesions and malignancies based on such features as the appearance of lesions, irregularities, shape of margins, echogenicity, and shadowing [2].
Compared to other screening methods, the breast imaging reporting and data system (BI-RADS) has shown promising results in the differentiation of benign breast lesions from malignant ones [3]. BI-RADS-US terminology is intended to provide a common language for sonogaphic reporting and research and to avoid ambiguity in the communication and teaching of sonographic interpretation [4].
Strain elastography (SE) is a supplementary method for conventional US used for the diagnostic confirmation by defining the degree of tissue stiffness [5]. The principle of SE is to define the response given by tissue to compression resulting in deformation within the tissue; in other words, as the tissue becomes harder, its displacement occurs at a lower rate. SE allows physicians to calculate tissue elasticity by superimposing the information in color on B-mode images, with each color showing a specific level of elasticity [6]. Thus, SE enables us to obtain objective data on tissue stiffness via the quantity of tissue displacement [5, 6].
In our study, we aimed at determining whether a novel method that combines BI-RADS and SE contributes to increasing the diagnostic performance in differentiating benign breast lesions from malignant ones.
Materials and methods
Patients
After obtaining approval from the local ethics committee, this prospective study was conducted with 81 breast lesions detected in 81 patients admitted to the Medical Faculty of Baskent University Hospital with various clinical complaints between February 2013 and February 2015. The inclusion criteria for the breast lesions were the existence of a breast lesion detected by conventional US and no history of previous treatments, such as breast surgery, chemotherapy, or radiotherapy. SE and US examinations were performed before biopsy in all patients by a radiologist with 10 years of experience in breast US.
Conventional ultrasound examination
B-mode US images of the lesions were acquired with a Siemens Acuson S3000 device (Siemens Medical Solutions, Mountain View, CA, USA) with an 18 L6 HD (5.5–18 MHz) linear transducer. B-mode US findings of the breast lesions were evaluated in terms of shape, long axis orientation, margins, lesion boundary, internal echo pattern, and posterior acoustic features described by Stavros et al. [7].
Determined through US alone and independently of mammography, the lesions were grouped as BI-RADS 3, 4, or 5 [3]. BI-RADS 4 lesions were classified into three subgroups as 4A (likelihood of malignancy between 2 and 10%), 4B (likelihood of malignancy between 10 and 50%), and 4C (likelihood of malignancy between 50 and 95%). In our study, BI-RADS 3 breast lesions were regarded as benign, while BI-RADS 4 and 5 lesions were accepted as malignant.
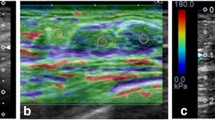
Strain elastography
To evaluate the stiffness of lesions, SE was performed using a Siemens Acuson S3000 device (Siemens Medical Solutions, Mountain View, CA, USA) with a 9L4 (4–9 MHz) linear transducer. In performing SE, the freehand compression method described by Itoh et al. was used [6]. In the supine position, the US transducer was positioned parallel to the breast lesion. To achieve appropriate contact with the skin, slight pressure was applied through the transducer. We acquired elastography images for breast tissues displacing 1–2 mm posteriorly and coming back to its initial location. The compression sufficiency was adjusted according to quality factor (QF) 60 and higher as an adequate value. Color maps produced based on the elastography images were assessed using the 5-point elastography scoring (ES) system defined by Itoh et al. [6]. Lesions with scores of 1, 2, and 3 were considered benign, and those with scores of 4 and 5 were considered malignant. A region of interest (ROI) box was placed on the targeted lesion, and another ROI box was placed on reference tissue determined to be adjacent subcutaneous fat tissue, irrespective of the depth, to measure strain ratio (SR). SR was calculated by comparing the strain value of the reference tissue with that of the targeted lesion.
In forming the classification via SE using one cutoff value, lesions with a mean SR value equal to or greater than the cutoff value were evaluated as malignant, while those less than the cutoff value were considered benign. Based on ES classification, ES 1, 2 and 3 breast lesions were regarded as benign, while ES 4 and 5 lesions were evaluated as malignant. For ES, the cutoff value was accepted as classification 3.
Combination of BI-RADS and strain elastography
According to the novel combined method using BI-RADS and SE together, the diagnostic results of BI-RADS 3 and 5 breast lesions were used without being changed. BI-RADS 4 lesions were categorized again according to the results of SR and ES. Therefore, lesions under the cutoff value of SR (2.84) and those ≥2.84 were re-categorized into BI-RADS 3 and BI-RADS 5, respectively. Similarly, lesions with ES 1, 2, or 3, and those with ES 4 and 5 were re-classified into BI-RADS 3 and BI-RADS 5, respectively (Fig. 1). According to the results of the combined method, sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy were calculated.
Pathologic diagnosis
Biopsy was recommended for all lesions categorized as BI-RADS 4 and 5. Although biopsy was unnecessary for BI-RADS 3 lesions, pathological confirmation was obtained in these patients due to the clinical evaluation and other reasons in the patients. The histopathological investigations of all lesions were performed through 14-gauge automated gun core biopsy or excision biopsy with US guidance within 48 h after US. Only core biopsy results diagnosed markedly were accepted; those with inadequate results were exposed to excision. The specimens of all lesions were evaluated by a pathologist with 8 years of experience with breast diseases.
Statistical analysis
Statistical analyses were performed using SPSS package for social sciences (version 15.0; SPSS, Chicago, IL, USA). Continuous data, such as SR, were expressed as mean ± standard deviation (SD). The independent sample t and the analysis of variance (ANOVA) tests were used to compare continuous outcomes. Categorical data were presented as frequencies and percentages, and compared using Pearson’s Chi-square or Fisher’s exact tests where they were appropriate. Area under the receiver operating characteristic curves (AUROC) is used to evaluate the predictive ability. Using maximum cutoff values, we determined the rates of sensitivity, specificity, PPV, NPV, and accuracy. A p value of <0.05 was accepted as statistically significant.
Results
Patients
Of the 81 patients in our study, 80 (98%) were female, while only one (2%) was male. The mean age was 51.3 ± 13.1 years (range 19–85 years), and the mean size of lesions calculated according to the longest axis was 16.3 ± 11.9 mm (range 3–70 mm). The characteristics of breast lesions are presented in Table 1. The histopathological results of breast lesions in the study are shown in Table 2.
Elasticity score
The rates of sensitivity, specificity, PPV, NPV, and accuracy of ES were calculated as 71.1 (27/38), 97.7 (42/43), 96.4 (27/28), 79.2 (42/53), and 85.1% (69/81), respectively. Twenty-eight (34.5%) lesions were assessed as ES 4 or 5. Of these lesions, 27 (96.4%) were diagnosed as malignant, while only one was diagnosed as benign (3.6%). One false-positive benign lesion classified as ES 5 was diagnosed as fat necrosis on histopathological investigation.
Fifty-three (65.4%) lesions were assessed as ES 1, 2, or 3. Forty-two (79.2%) and 11 (20.7%) of these lesions were histopathologically diagnosed as benign and malignant, respectively. Among 11 false-negative lesions, two were diagnosed as ductal carcinomas in situ (DCIS), one as medullar carcinoma (Fig. 2), one as invasive lobular carcinoma, and seven as invasive ductal carcinomas.
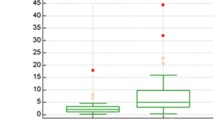
Strain ratio
The mean SR for malignant lesions (4.3 ± 1.5; range 1.6–7.3) was statistically higher than that of benign lesions (1.8 ± 0.9; range 0.5–4.9; p < 0.001). To achieve the highest sensitivity and specificity, the cutoff value for SR was determined to be 2.84; thus, the rates of sensitivity, specificity, PPV, NPV, and accuracy were calculated as 78.9 (30/38), 90.7 (39/43), 88.2 (30/34), 82.9 (39/47), and 85.1% (69/81), respectively.
On the receiver operating characteristic (ROC) curve of SR values drawn to distinguish between benign and malignant lesions, the AUROC value was 0.927, which was statistically significant (p < 0.001). Two of four false-positive lesions were diagnosed as sclerosing adenosis and two as fibroadenomas. Five, one, and two of eight false-negative lesions were diagnosed as invasive ductal carcinomas, medullary carcinoma, and DCIS, respectively (Fig. 3). The association between BI-RADS groups and SR measurements is presented in Table 3, which shows that as SR measurements increase, BI-RADS scores also increase statistically and significantly.
Combination of BI-RADS and strain elastography
Acquired via a novel method that combines SR and ES results with those of BI-RADS separately, the rates of sensitivity, specificity, PPV, NPV, accuracy, and AUROC are shown in Table 4. Based on these results, the specificity, PPV, and accuracy of both methods combined with SR and ES explicitly increased, compared with BI-RADS alone. Additionally, the sensitivity, specificity, PPV, and accuracy of the combined methods also increased in comparison to SR alone, and only the sensitivity and accuracy of the combined methods increased in comparison to ES alone.
Discussion
BI-RADS is an important B-mode US classification system used to estimate malignant lesions by standardizing breast lesions according to their morphological features [8]. This classification system describes only the morphological characteristics of lesions and has a higher sensitivity rate, but the specificity rate of BI-RADS is still under the desired level. Some difficulties are encountered, especially in the differentiation of BI-RADS 4 subgroups. In previous studies, malignancy rates were reported at different intervals between 7.6–10, 21–38.7, and 57–81.9% for BI-RADS 4A, 4B, and 4C subcategories, respectively [3, 9, 10]. In our study, malignancy rates were 7.6, 21.4, and 70% for BI-RADS 4A, 4B, and 4C subcategories, respectively.
SE can be performed along with US to demonstrate and define tissue elasticity [4]. Thus, in addition to the morphological findings obtained through BI-RADS, SE yields information on lesion elasticity. We investigated whether combining these two methods would increase the diagnostic performance in the differentiation of breast lesions. In a similar study performed by Hao et al., where US elastography and BI-RADS were used together, an increase was detected in specificity, PPV, and accuracy, and their rates were found to be 72.9, 76, and 82%, respectively [4]. In another study by Zhi et al., in which BI-RADS and US elastography were used in combination, an increase was detected in the rates of specificity, PPV, and accuracy, compared to BI-RADS alone, and these rates were reported as 87.8, 76.5, and 86.3%, respectively [11]. In our study, specificity, PPV, and accuracy of BI-RADS alone were found to be lower, compared to those of SE alone. Our findings obtained through SE alone were consistent with those reported in other studies [12–15]. In addition, both SR and ES were separately combined with BI-RADS in our study. According to the results of both combined methods, PPV and accuracy were observed to increase with both combined methods, with the rates being 91.9% for PPV and 91.3% for accuracy with BI-RADS + SR, while they were 97.1% and 92.5%, respectively, in the case of BI-RADS + ES. While specificity was 97.7% with BI-RADS + ES and showed no changes, the rate was calculated as 93% with BI-RADS + SR and showed an increase. Therefore, the novel combination of two different methods showed almost the same diagnostic performance. However, we consider that the diverse and subjective assessments of breast elastic images influence the diagnosis of the ultrasonographer. As such, it is difficult to distinguish whether a lesion is 3 or 4 using the five-point scoring system. We also found that SR assessment exhibited much better diagnostic performance for large lesions as compared with ES. This may be related to the fact that the size of lesions is likely to lead to changes, such as degeneration, necrosis, or hemorrhage. As a result of this, large lesions that should have been assessed a score of 4 or 5 may be misleadingly given a score of 2. Although SR assessment yields more objective results, different cutoff measurements of SR can be obtained via different brands of devices [14, 16–18].
SE, due to its semi-quantitative and user-dependent structure, is to be performed only after a certain level of experience has been acquired. In a study where shear-wave elastography and SE were compared by Chang et al., similar findings of elasticity were obtained through both methods, and no significant difference was found between the two [19]. In another study that investigated the combination of shear-wave elastography and BI-RADS, Li et al. calculated the highest sensitivity, specificity, and PPV values as 81, 94.8, and 85.5%, respectively. In their study, an increase was found in the rates of specificity and PPV due to the combination of BI-RADS and shear-wave elastography [20]. The elasticity measurements of breast lesions were performed with SE in our study. Sensitivity, specificity, and PPV were 89.5, 93, and 91.9%, respectively, with the combination of BI-RADS and SR, while they were 86.8, 97.7, and 97.1%, respectively, with the combination of BI-RADS and ES. In addition, unlike shear-wave elastography, ES values obtained through the color scale of lesions could be calculated in our study.
We also detected a statistically significant increase between the results of BI-RADS groups and SR measurements. Thus, we consider that BI-RADS classification can be grouped more easily with the results of SR measurements. However, different measurements obtained via different brands of equipment and differences between elastography methods prevent the standardization of measurements.
When SE was used alone in our study, false-negative results were found in invasive ductal and lobular carcinomas, DCIS, and medullar carcinomas, while false-positive results were observed in fibroadenomas, sclerosing adenosis, and fat necrosis. We consider that such reasons as calcification and fibroplastic proliferation seen in benign breast lesions, and others, such as necrosis, hemorrhage, or the soft nature of tumors observed in malignant breast lesions, also led to false-positive or false-negative results in our study, consistent with other studies [6, 14, 20, 21]. However, thanks to our combined method, false-negative and false-positive results are considered to be minimized. Additionally, ES and SR values of four lesions diagnosed as granulomatous mastitis in our study were determined under the cutoff values. US discrimination between granulomatous mastitis and malignant breast lesions is among the most difficult comparisons in breast imaging [22]. We believe that some lesions like granulomatous mastitis that are quite difficult to recognize through conventional US can be diagnosed more easily by using the combined method.
Our study has also some limitations. First, the absence of interobserver or intraobserver variability was a negative factor in assessing the results of US and SE. Second, SE measurements were not always performed optimally due to multiple factors, such as breast size and density, depth and proximity of a lesion to the retroareolar region, and pain in breast tissues. Third, the sample size was relatively small. Finally, the variation of histopathologic results was also limited.
Conclusion
In conclusion, we consider that the novel combined method will contribute to and improve the diagnostic performance in differentiation of breast lesions, compared with BI-RADS or SE alone; therefore, BI-RADS 4 lesions, which are the most difficult to classify, will be able to be classified more easily.
References
Botha JL, Bray F, Sankila R, et al. Breast cancer incidence and mortality trends in 16 European countries. Eur J Cancer. 2003;39:1718–29.
Margolin FR, Leung JW, Jacobs RP, et al. Percutaneous imaging-guided core breast biopsy: 5 years’ experience in a community hospital. AJR Am J Roentgenol. 2001;177:559–64.
Wiratkapun C, Bunyapaiboonsri W, Wibulpolprasert B, et al. Biopsy rate and positive predictive value for breast cancer in BI-RADS category 4 breast lesions. J Med Assoc Thai. 2010;93:830–7.
Hao SY, Ou B, Li LJ, et al. Could ultrasonic elastography help the diagnosis of breast cancer with the usage of sonographic BI-RADS classification? Eur J Radiol. 2015;84:2492–500.
Ophir J, Cespedes I, Ponnekanti H, et al. Elastography: a quantitative method for imaging the elasticity of biological tissues. Ultrason Imaging. 1991;13:111–34.
Itoh A, Ueno E, Tohno E, et al. Breast disease: clinical application of US elastography for diagnosis. Radiology. 2006;239:341–50.
Stavros AT, Thickman D, Rapp CL, et al. Solid breast nodules: use of sonography to distinguish between benign and malignant lesions. Radiology. 1995;196:123–34.
Hao SY, Jiang QC, Zhong WJ, et al. Ultrasound Elastography Combined With BI-RADS-US Classification System: Is It Helpful for the Diagnostic Performance of Conventional Ultrasonography? Clin Breast Cancer. 2016;16:e33–41.
Chaiwerawattana A, Thanasitthichai S, Boonlikit S, et al. Clinical outcome of breast cancer BI-RADS 4 lesions during 2003-2008 in the National Cancer Institute Thailand. Asian Pac J Cancer Prev. 2012;13:4063–6.
Yoon JH, Kim MJ, Moon HJ, et al. Subcategorization of ultrasonographic BI-RADS category 4: positive predictive value and clinical factors affecting it. Ultrasound Med Biol. 2011;37:693–9.
Zhi H, Xiao XY, Ou B, et al. Could ultrasonic elastography help the diagnosis of small (≤2 cm) breast cancer with the usage of sonographic BI-RADS classification? Eur J Radiol. 2012;81:3216–21.
Cho N, Moon WK, Kim HY, et al. Sonoelastographic strain index for differentiation of benign and malignant nonpalpable breast masses. J Ultrasound Med. 2010;29:1–7.
Parajuly SS, Lan PY, Yun MB, et al. Diagnostic potential of strain ratio measurement and a 5 point scoring method for detection of breast cancer: Chinese experience. Asian Pac J Cancer Prev. 2012;13:1447–52.
Zhao QL, Ruan LT, Zhang H, et al. Diagnosis of solid breast lesions by elastography 5-point score and strain ratio method. Eur J Radiol. 2012;81:3245–9.
Zhi H, Xiao XY, Yang HY, et al. Ultrasonic elastography in breast cancer diagnosis: strain ratio vs 5-point scale. Acad Radiol. 2010;17:1227–33.
Fausto A, Rubello D, Carboni A, et al. Clinical value of relative quantification ultrasound elastography in characterizing breast tumors. Biomed Pharmacother. 2015;75:88–92.
Fischer T, Peisker U, Fiedor S, et al. Significant differentiation of focal breast lesions: raw data-based calculation of strain ratio. Ultraschall Med. 2012;33:372–9.
Zhou J, Zhan W, Dong Y, et al. Stiffness of the surrounding tissue of breast lesions evaluated by ultrasound elastography. Eur Radiol. 2014;24:1659–67.
Chang JM, Won JK, Lee KB, et al. Comparison of shear-wave and strain ultrasound elastography in the differentiation of benign and malignant breast lesions. AJR Am J Roentgenol. 2013;201:W347–56.
Li DD, Xu HX, Guo LH, et al. Combination of two-dimensional shear wave elastography with ultrasound breast imaging reporting and data system in the diagnosis of breast lesions: a new method to increase the diagnostic performance. Eur Radiol. 2016;26:3290–300.
Houelleu Demay ML, Monghal C, Bertrand P, et al. An assessment of the performance of elastography for the investigation of BI-RADS 4 and BI-RADS 5 breast lesions: correlations with pathological anatomy findings. Diagn Interv Imaging. 2012;93:757–66.
Durur-Karakaya A, Durur-Subasi I, Akcay MN, et al. Sonoelastography findings for idiopathic granulomatous mastitis. Jpn J Radiol. 2015;33:33–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was supported by the Research Fund of Medical School of Baskent University, Ankara, Turkey.
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
Informed consent
Informed consent was obtained from all patients for being included in the study.
About this article
Cite this article
Arslan, S., Uslu, N., Ozturk, F.U. et al. Can strain elastography combined with ultrasound breast imaging reporting and data system be a more effective method in the differentiation of benign and malignant breast lesions?. J Med Ultrasonics 44, 289–296 (2017). https://doi.org/10.1007/s10396-017-0772-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-017-0772-y