Abstract
Objective
Universal health coverage and maternal health outcomes have become a part of the global health agenda in low and middle-income countries including India. To achieve the sustainable development goals (SDG-3), maternal healthcare services utilization is a significant intervention in decreasing maternal mortality and morbidity. This study aims to assess the potential association between health insurance coverage (HIC) and maternal healthcare services utilization in India.
Methods
Data was obtained from the fifth round of the National Family Health Survey (NFHS-5), conducted during 2019–21. Bivariate, spatial analysis and logistic regression models have been used to assess association between utilization of maternal healthcare services and HIC combined with other background factors in India.
Results
HIC among women was found to be 24%. Approximately 59%, 90% and 46% of women had full antenatal care (ANC) visits, skilled birth attendant (SBA) and post-natal care (PNC), respectively. The study results suggested that individuals with HIC were more likely to have ANC visits (OR = 1.28; 95% CI 1.25–1.31), SBA (OR = 1.41; 95% CI 1.36–1.46) and PNC (OR = 1.16; 95% CI 1.13–1.18) services, respectively. Moreover, socioeconomic characteristics and other predictor variables were significantly associated with maternal healthcare service utilization in India.
Conclusion
The study concludes that HIC is a significant predictor for the maternal and child healthcare services in India, and women with HIC were more likely to have full ANC visits, SBA and PNC. Overall, to accelerate the progress towards achieving SDGs related to maternal and child health, the government should expand and strengthen the existing policies to increase coverage of health insurance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Encouraging women to have an institutional birth has been an important global health strategy in reducing maternal and infant deaths in low- and middle-income countries (LMICs) (Bishanga et al. 2018; Mukherjee et al. 2018; Shah et al. 2018). The World Health Organization (WHO) reported that approximately 295,000 women died during and following pregnancy and childbirth, whereas 94% of all preventable maternal deaths occurred in LMICs (WHO 2019). These deaths could have been avoided by reducing maternal and child mortality and providing the opportunity to have safe childbirth (WHO 2017) by bestowing women access to maternal healthcare services such as antenatal care (ANC), skilled birth attendant (SBA) and emergency obstetric care (Kassebaum et al. 2016). Services for maternal healthcare remain crucial markers for tracking the advancement of maternal health outcomes and maternal mortality. The majority of maternal mortality and morbidity arise due to inadequate utilization of maternal healthcare services (Murray and Lopez 1997; Alvarez et al. 2009). Antenatal care is a key component of the Safe Motherhood Initiative and assists in providing interventions necessary for successful pregnancy outcomes. Moreover, it is well-established that maternal healthcare service utilization is an important precursor for reducing maternal mortality and morbidity (Firoz et al. 2018). The timely management and treatment of pregnancy-related issues are strengthened by pre-natal care, institutional health delivery with a professional birth attendant, and postnatal care, which help lower maternal mortality.
Although India has made a remarkable progress in reducing the maternal mortality ratio (MMR), it remains a significant contributor to global maternal deaths. Available estimates indicate that MMR in the country has declined from 210 to 145 per 100,000 live births for the period 2010–2017 (World Bank 2019). However, the rate of maternal mortality decline has been inadequate to meet the global Millennium Development Goals (MDGs) targets which were exclusively focused on developing nations. Therefore, to achieve the Sustainable Development Goals (SDGs), maternal healthcare services utilization is an important precursor for decreasing maternal mortality and morbidity.
One of the most pressing issues in public health programmes and policies is ensuring equitable access to maternal healthcare, including prenatal, delivery and postnatal treatments. A wide array of literature has examined socio-economic, geographic and maternal differences in the utilization of ANC, assistance during delivery, and other maternal healthcare indicators (Gebremedhin et al. 2020). Poverty, distance to healthcare facilities, access to information, quality health services and cultural practices are likely to impact access to maternal health services (Kumar et al. 2014; WHO 2021). Numerous structural and contextual factors have an impact on maternal healthcare service utilization, which requires careful consideration.
Health insurance coverage
Health insurance coverage (HIC) is an essential pro-poor initiative in LMICs and dispite its enormous benefits, the prior literature suggests that maternal healthcare services utilization, in particular, ANC visits, SBA and post-natal care (PNC) are still not majorly covered by the health insurance, even India is no exception (WHO and UNICEF 2003; Dong 2012; Goli et al. 2016; Ameyaw et al. 2017). Under the National Health Mission (NHM), India introduced the world’s largest conditional cash transfer scheme, i.e. Janani Suraksha Yojana (JSY) aimed to overcome financial obstacles in maternal healthcare services utilization. However, some questions remain unanswered, i.e. the provision of poor quality healthcare services by the Government and the higher cost of private healthcare services in India (Goli et al. 2016). Therefore, India needs to prioritize its public health spending to tackle the higher out-of-pocket expenditure for maternity care.
Through a rise in the coverage of health insurance, a growing set of studies have investigated the potential association with maternal healthcare services utilization (Comfort et al. 2013; Khan and Singh 2016; Wang et al. 2017; Kibusi et al. 2018; Fernandes et al. 2021); however, the impact of health insurance on maternal healthcare services utilization across various socio-economic groups in India has not gained much recognition in the existing literature (Randive et al. 2014; Mukherjee and Singh 2018; Gebremedhin et al. 2020). Thus, this study aims to investigate the magnitude of the relationship between HIC and the use of maternal healthcare services. Understanding the factors that influence the use of healthcare services is essential to comprehend maternal well-being. Consequently, the goal of this study is to assess the inequities in the determinants of maternal healthcare usage in India, specifically the utilization of ANC, SBA and PNC. Therefore, the present study will help understand the current status of maternal healthcare services utilization in the country and how well the HIC has impacted the usage of these services, especially in the era when the Indian Government has invested considerable resources in the healthcare sector.
Theoretical framework
Several complex factors influence maternal healthcare service utilization to revolve around demographic, socioeconomic and geographical factors (Mukherjee and Singh 2018; Ameyaw et al. 2021; Singh et al. 2021). For the concept of maternal healthcare service utilization and its contextual factors to be well understood, this study utilizes contextual variables from Anderson’s Behavioural Model (BM) of healthcare services utilization (Andersen and Newman 1973; Andersen 1995), where we aimed to investigate the association between HIC and the use of maternal healthcare services (measured by 4+ANC visits, SBA and PNC). In this study, the BM assumes that maternal healthcare services utilization rests on predisposing, enabling and need factors that operate at both contextual and individual levels (Andersen and Newman 1973; Andersen 2008).
Materials and methods
Data source
The present study uses the data from the most recent round of India’s DHS, i.e. National Family Health Survey (NFHS-5) conducted during 2019–21. This is the national-level large-scale survey that covered 36 states/UTs including 707 districts in India. This survey was conducted under the supervision of the Ministry of Health and Family Welfare (MoHFW), Government of India, and the International Institute for Population Sciences (IIPS), Mumbai, was the nodal agency for that survey. This survey provides an estimation of clinical, anthropometric and biochemical (CAB) components along with information on morbidity condition and variables such as malnutrition and HIV through biometric measurement (IIPS and ICF 2021). A multistage stratified sampling design was adopted for data collection.
Sample selection
For our analysis, we identified mothers who had given birth in the past five years preceding the survey covered in the National Family Health Survey-5 (2019–21). In this study, a total of 173,696 women aged 15–49 years were found eligible for inclusion in the final analysis. The dataset is freely available for download from The DHS Program – India: Standard DHS, 2019–21 Dataset. Appropriate sampling weights have been used to adjust for the non-proportional allocation of the sample.
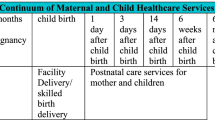
Dependent variables
The outcome variable of interest is maternal healthcare services utilization. Under the WHO guidelines, maternal healthcare services utilization includes at least four antenatal visits, skilled birth attendants and post-natal care for the child. In the NFHS-5 (2019–21) survey, the women were asked about the number of ANC visits they made during their pregnancies and the answer was recorded as ‘0–3’ (< 3 ANC visits) and ‘4 & above’ (≥ 4 ANC visits). For an SBA, the women were asked ‘Who assisted [NAME] during delivery?’ The response options were regrouped into ‘births delivered with the assistance of doctors, auxiliary nurse midwives, nurses, midwives, and lady health visitors’ and coded as ‘1’ (yes) or else as ‘0’ (no). For PNC, the women were asked ‘Did [NAME] go for postnatal checks within 2 months?’ The response options to this question were coded as ‘1’ (yes), and ‘0’ (no). The responses of ‘don’t know’ were dropped for both ANC and PNC variables. The recording and categorization used in this study were based on previous evidence (Rai et al. 2012; Ahinkorah et al. 2021; Singh et al. 2021; Yaya et al. 2021).
Independent variables
Independent variables used in this study were adopted from the existing literature (Gebremedhin et al. 2020; Fernandes et al. 2021; Amu et al. 2022). The contextual variables include health insurance coverage categorized as ‘yes’ or ‘no’ based on their response to the question ‘Are you covered by any health scheme or any health insurance’; women’s age (<20 years, 20–24, 25–29, 30–34 years & 35 and above); education (no formal education, primary, secondary and higher); marital status (never married/widowed/divorced/separated and currently married); religious group (Hindu, Muslim, Christian, others); birth order (1, 2 and 3 & above); getting permission to go (not a major problem, major problem); getting money for treatment (not a major problem, major problem); distance to health facility (not a major problem, major problem). Moreover, the mass media exposure was assessed by using three variables, i.e. frequency of watching television, frequency of reading newspapers/magazines and frequency of listening to the radio. By adding the row total, this was re-coded as four major categories (often, sometimes, rarely & never). The geographical region of the country was grouped as ‘North’, ‘East’, ‘Northeast’, ‘Central’, ‘West’ and ‘South’ based on criteria used by NFHS-5 (2019–21). The wealth index was sorted as poorest, poorer, middle, richer and richest. Finally, the respondent’s place of residence was categorized as ‘urban’ or ‘rural’.
Statistical analysis
We estimated the weighted prevalence of HIC and use of maternal healthcare services by socio-economic status during 2020–21. We ran a binary logistic regression model to understand the effects of socioeconomic, demographic and cultural variables on the likelihood of use of maternal healthcare services. The mathematical expression of the logistic regression analysis is:
where P = probability of occurrence of the event (going for 4 or more ANC visits, SBA and PNC) which is influenced by a set of predictor variables in the manner specified with parameters β0, β1, β2… βk as the coefficients and X1, X2,…Xk are predictor variables. P/(1-P) is the measure of odds, and hence the ratio of P/(1-P) is the log of odds or the logit of P. The analysis was carried out using STATA 16. To understand the geographical variation of HIC and the use of maternal healthcare services utilization, spatial analysis was conducted using software ArcGIS 10.8.
Results
Prevalence of HIC and maternal healthcare services utilization – geographical variations
The geographical variation of HIC and maternal healthcare services utilization at the state/UTs level in India is (2019–21) shown in Table 1. At the national level, only one-fourth of the respondents (24%) were covered by any health insurance and approximately 59% had four and above ANC visits during pregnancy, and 46% received PNC check-ups for the last child. Furthermore, the majority of the births (90%) were assisted by a skilled attendant. There were, however, inter-state variations in India. The prevalence of HIC was highest in Rajasthan (82%), followed by Meghalaya (64%), Lakshadweep (64%) and Chhattisgarh (61%). On the contrary, Andaman & Nicobar Islands (< 1%), Jammu & Kashmir (2%) and Uttar Pradesh (6%) have the lowest prevalence of HIC among women aged 15–49 years in India.
Substantial variations in maternal healthcare services utilization were observed. The prevalence of full ANC visits ranged from 21% in Nagaland to 95% in Lakshadweep. In contrast, SBA ranged between 57% in Nagaland to 100% in Lakshadweep. The prevalence of PNC was highest in Odisha (76%) and lowest in Nagaland (9%). The components of maternal healthcare service utilization were found to be very low in states such as Nagaland, Bihar, Jharkhand, Arunachal Pradesh and Meghalaya.
Figure 1(a) illustrates district-level geographical variations in the prevalence of HIC in 2019–21. Districts from Western (Gujarat), Central (Chhattisgarh), Southern (Telangana, Andhra Pradesh, Kerala), North-east (Assam, Meghalaya and Mizoram) and Northern (Rajasthan and Uttarakhand) parts of India showed a high prevalence of HIC, while districts from Central (Madhya Pradesh, Uttar Pradesh), Eastern (Bihar), Western (Maharashtra) Southern (Karnataka) and Northern (Panjab, Ladakh) parts of India showed a lower prevalence of HIC among women aged 15–49 years. Figure 1(b) shows the district-level variations in full ANC visits in India during 2019–21. For instance, the districts from Southern (Kerala, Tamil Nadu), Western (Gujarat), Eastern (West Bengal and Odisha) and Northern (Ladakh, Jammu & Kashmir, and Himachal Pradesh) parts of India showed a higher percentage of women having at least four ANC visits. On the other hand, the Central regions of India (Madhya Pradesh, Uttar Pradesh) and some districts in the West (Gujarat) and the East (West Bengal, Odisha) parts of India showed a low prevalence of at least four ANC visits.
Figure 2(a) presents the prevalence of SBA across the districts of India during 2019–21. Districts from the south (Kerala, Tamil Nadu and some part of Andhra Pradesh), west (some districts from Maharashtra, Gujarat and Rajasthan) and north (Ladakh, Jammu & Kashmir, Punjab and Haryana), as well as some district from the eastern (West Bengal and Odisha) parts of India showed a higher proportion of births occured in the presence of SBA. Whereas a lower proportion of births occurred in the presence of SBA in central (Uttar Pradesh, Madhya Pradesh), eastern (Bihar, Jharkhand) and north-eastern (Himachal Pradesh, Uttarakhand) parts of India. Moreover, Fig. 2(b) shows the district level differences in PNC for a child in India, 2019–21. The proportion receiving PNC check-ups for a child was higher in southern (Tamil Nadu), eastern (Odisha and West Bengal), central (some districts from Uttar Pradesh, Chhattisgarh, Madhya Pradesh) and northern (Punjab and some districts from Himachal Pradesh and Uttarakhand) parts of India. However, northern (Ladakh, Jammu & Kashmir, Haryana), north-eastern (Mizoram, Manipur, Nagaland, Arunachal Pradesh, Tripura and some districts from Assam) Western (Rajasthan and Maharashtra) Southern (Karnataka, Andhra Pradesh and Telangana) and eastern (Bihar and Jharkhand) parts of India showed a low prevalence of PNC check-up for a child.
Prevalence of maternal healthcare services utilization across groups
Table 2 shows the proportion of women (aged 15–49 years) utilizing maternal health care services by background characteristics. The results indicated that HIC was significantly (p < 0.001) associated with 4+ ANC visits, SBA and PNC for a child. For instance, Fig. 3 shows that a higher proportion of women with health insurance coverage had full ANC, SBA and PNC visits compared to their counterparts (4+ANC visits 65% vs 57%; SBA 93% vs 90%; PNC 49% vs. 45%).
At least four ANC visits and SBA were higher among younger mothers than older mothers. Further, higher 4+ANC visits, SBA and PNC was observed among women with secondary and higher education than those with no formal education. Various components of maternal healthcare utilization varied across the religious group. With the higher birth orders, the proportion of women having full ANC visits, SBA and PNC declined. The use of maternal healthcare services was higher among women who had permission to go outside, or getting money for treatment was not a major problem or distance to a health facility was not an issue.
Women from the southern region received the highest 4+ANC visits and SBA (78% and 97% respectively). The proportion of women availing PNC check-ups for a child was highest among women from the eastern region (49%) followed by the southern region and lowest among women from the central region (33%) of India. As we moved from the poorest to the richest wealth quintile, the proportion of women having full ANC visits, births taking place in the presence of skilled attendants and PNC increased. Unsurprisingly, complete ANC visits and SBA were lower among women from rural areas. In contrast, post-natal check-ups were higher in rural areas than in urban areas (Table 2).
Association between HIC and maternal healthcare services utilization in India
Table 3 presents the logistic regression results indicating the association between the utilization of maternal healthcare services and HIC along with background characteristics, 2019–21. The results suggested that HIC was associated with higher odds of full ANC visits (OR = 1.26; CI 1.23–1.29). Similarly, women who were covered by health insurance were more likely to have delivered in the presence of a skilled attendant (OR = 1.35; CI 1.30–1.41) during delivery and went for PNC check-ups for a child (OR = 1.25; CI 1.22–1.28). The likelihood of full ANC visits and SBA among women increased with higher age, increasing levels of education, mass media exposure and wealth index. Women aged 35 and above, having secondary and higher education, everyday mass media exposure and with the richest wealth quintile were 1.38, 1.41, 1.50 and 1.42 times, respectively, more likely to utilize full ANC services than their counterparts women aged <20 years, without any formal education, without exposure to mass media and women from the poorest wealth quintile. On the other hand, multiparous women, who had difficulties getting permission to go outside (OR = 0.75; CI 0.72–0.77), whose residences were at a distance from a health facility (OR = 0.89; CI 0.87–0.91) or had trouble getting money to access ANC services (OR = 1.13; CI 1.10–1.16) and women from rural (OR = 0.92; CI 0.89–0.94) areas were less likely to utilize ANC services compared to their respective counterparts. Similarly, women with two and three or higher parity were (18% and 38%, respectively) less likely to have full ANC visits compared to women with first parity. Women from the western region were 1.73 times (OR = 1.73; CI 1.83–2.01) more likely to have full ANC visits than women from the northern region.
In the context of SBA, women aged 35 and above, having secondary and higher education, frequent mass media exposure and the richest wealth quintile was, respectively, 1.48, 2.01, 1.51 and 2.64 times more likely to have SBA during delivery compared to their counterpart groups women aged <20 years, uneducated, no exposure to mass media and the poorest wealth quintile. On the contrary, women whose residence was at a distance from a health facility were 26% less likely to have SBA than women whose residence was near the health facility (OR = 0.74; CI 0.71–0.76). With the increasing birth order, the likelihood of deliveries taking place in the presence of an SBA declined by 33% (2nd birth order) and 58% (3rd birth order) about the first-order birth. The likelihood of having SBA increased with an increase in the wealth of women and the odds of SBA were lower among women residing in rural areas (OR = 0.90; CI 0.85–0.95) compared to those living in urban areas. Women from the Southern region had the highest likelihood to have SBA while women from the Central region were least likely to have deliveries accompanied by SBA in India (Table 3).
The odds of PNC check-ups for a child among women increased with their age, wealth status and exposure to mass media. Women aged 35 and above (OR = 1.24; CI 1.16–1.34), frequent mass media exposure (OR = 1.38; CI 1.33–1.44) and rural place of residence (OR = 1.22; CI 1.19–1.26) were more likely to avail PNC for a child than women aged <20 years, no mass media exposure, and urban place of residents. Moreover, the likelihood of utilization of PNC services declined with increasing levels of education and higher-order births. For instance, the PNC check-ups for a child were 1.14 times and 1.11 times higher for women with a primary and higher level of education than women without any formal education. Utilization of PNC services was highest in the eastern region (OR = 1.28; CI 1.24–1.32) and lowest in the central region (OR = 0.47; CI 0.45 0.49) in reference to the northern region in India (Table 3).
Discussion
The present study examined the impact of health insurance coverage and its association with components of maternal healthcare services utilization among women in the reproductive age group in India. Overall, 24% of women were covered under health insurance schemes in the country. Approximately 59%, 90% and 46% of the women had full ANC visits, delivered in the presence of skilled attendants and went for PNC check-ups for a child, respectively. Overall, a significant relationship between HIC and the use of maternal healthcare services has been observed, which is in line with several previous studies (Comfort et al. 2013; Wang et al. 2017; Kibusi et al. 2018; Yaya et al. 2019). The study findings suggest that being covered by any health insurance increased the odds of full ANC visits.
The findings indicate that the coverage of health insurance was positively associated with a higher proportion of SBA during delivery and PNC, which has been well-established in previous literature (Khan and Singh 2016; Were et al. 2017; Fernandes et al. 2021). Being covered by health insurance reduces the economic barrier and increases access to the use of maternal healthcare services. Researchers emphasize that the HIC reduces the burden of costs associated with institutional delivery, ANC visits and PNC check-ups, and encourages mothers to access healthcare services (Randive et al. 2014; Kumar et al. 2014; Fernandes et al. 2021). As observed in our study, decreased utilization of ANC services with higher order birth can be attributed to increased confidence from previous pregnancy experiences, constraints of time and resources, poor prior experience with the healthcare system and financial obstacles (Miteniece et al. 2018; Kumar et al. 2019).
Women’s education, economic status and mass media exposure were highly associated with full ANC visits, which corroborates with some previous literature (Sakeah et al. 2017; Hijazi et al. 2018; Miteniece et al. 2018; Kumar et al. 2019). Studies have identified education as a major determinant of maternal healthcare and health-seeking behaviour (Hahn and Truman 2015; Dimbuene et al. 2018). Richer women generally have higher economic status and social access to healthcare services, which may improve full ANC visits (Kumar et al. 2019; UNICEF 2022). Increasing age, economic status, and mass media exposure increase the likelihood of SBA and access to PNC check-ups among children in the country (Fernandes et al. 2021; Amu et al. 2022). The wealth-related inequality refutes the SDGs aim of leaving none behind. Our findings revealed that women from rural areas were found to be less likely to utilize maternal healthcare services. This finding has similarities with previous literature (Mahajan and Sharma 2014; Adedokun and Yaya 2020; Nuamah et al. 2019; Wu et al. 2019). Disproportionate maternal healthcare utilization has been reported among people from different classes, creeds and religions despite the high demand (Lopez-Cevallos and Chi 2010; Zere et al. 2011).
Our findings showed that getting permission to go outside and distance to the health facility is negatively associated with different components of healthcare utilization. Previous studies reported that decision-making autonomy among women in the household leads to improvement in educational and health-related outcomes for children (Bloom et al. 2001; Anderson and Eswaran 2009; Lépine and Strobl 2013; Gebremedhin and Mohanty 2016). Several studies have observed the ‘distance decay’ effect in healthcare utilization in Asian and South African countries (Kumar et al. 2014; McLaren et al. 2014; Nuamah et al. 2019) indicating the negative association between geographical accessibility and healthcare utilization as an obstacle in improving maternity care scenario (Masters et al. 2013). The regional variation in maternal healthcare utilization indicated the important role of traditional birth attendants, religious beliefs and cultural practices.
The findings of this study provide important evidence highlighting the nature of existing inequalities in the use of maternal healthcare services. Aligned with the MDGs objectives, the government of India implemented the JSY programme in 2005 integrating cash assistance with delivery and post-delivery care. Owing to the programme, there has been a substantial increase in institutional births; however, there remain major challenges that need to be addressed. Our findings suggest that educational policies should be more centred on women from poor and deprived backgrounds, which might help in reducing inequality in accessing maternal healthcare services. Additionally, the coverage of health insurance is quite low. Moreover, this study highlights the need for adequate implementation of policies to improve maternal healthcare uptake in India.
The present study has some limitations. Firstly, the responses concerning the individual components of coverage of health insurance and maternal healthcare utilization were self-reported and, therefore, are prone to recall bias. To reduce the bias, the analysis is restricted to births in the year preceding the survey (last birth). Secondly, the study did not include variables such as health literacy, care-seeking behaviour, distance from the nearest healthcare facility, provider discrimination and other system-side factors for which information was not collected in NFHS-5.
Conclusion
The present study contributes to providing remarkable geographical variations in HIC and maternal healthcare services utilization in India along with the associated factors affecting the use of these maternal healthcare services. Overall, the study found a positive association between HIC and maternal healthcare services utilization in the country. Based on findings from the current study, we recommend that the public health programmes must target districts with persisting low healthcare utilization and needful measures, including education, economic status and mass media exposure, should be taken to increase the healthcare utilization among women in India. To accelerate progress, the government should adopt more interventions to increase health insurance coverage and make maternal healthcare services an integral part of helath insurance. Additioanlly, the quality of the existing programmes should be improved, including the conditional cash transfer scheme, which would improve the country’s progress on the track to the SDGs.
Data availability
The data of a particular study is available in the public domain and can be extracted from: https://dhsprogram.com/Data/
Code availability
Not applicable
Abbreviations
- ANC:
-
Ante-natal care
- DHS:
-
Demographic Health Survey
- HIC:
-
Health insurance coverage
- JSY:
-
Janani Suraksha Yojana
- LMICs:
-
Low and middle-income countries
- MDGs:
-
Millennium Development Goals
- MMR:
-
Maternal mortality ratio
- NFHS:
-
National Family Health Survey
- PNC:
-
Post-natal care
- SBA:
-
Skilled birth Attendant
- SDG:
-
Sustainable Development Goals
- WHO:
-
World Health Organization
References
Adedokun ST, Yaya S (2020) Correlates of antenatal care utilization among women of reproductive age in sub-Saharan Africa: evidence from multinomial analysis of demographic and health surveys (2010–2018) from 31 countries. Archives of Public Health 78(1):1-0. https://doi.org/10.1186/s13690-020-00516-w
Ahinkorah BO, Ameyaw EK, Seidu AA, Odusina EK, Keetile M, Yaya S (2021) Examining barriers to healthcare access and utilization of antenatal care services: evidence from demographic health surveys in sub-Saharan Africa. BMC Health Services Res 21(1):1–16. https://doi.org/10.1186/s12913-021-06129-5
Alvarez JL, Gil R, Hernández V, Gil A (2009) Factors associated with maternal mortality in Sub-Saharan Africa: an ecological study. BMC Public Health 9(1):1–8. https://doi.org/10.1186/1471-2458-9-462
Ameyaw EK, Kofinti RE, Appiah F (2017) National health insurance subscription and maternal healthcare utilisation across mothers’ wealth status in Ghana. Health Econ Rev 7(1):1–5. https://doi.org/10.1186/s13561-017-0152-8
Ameyaw EK, Ahinkorah BO, Baatiema L, Seidu AA (2021) Is the National Health Insurance Scheme helping pregnant women in accessing health services? Analysis of the 2014 Ghana demographic and Health survey. BMC Preg Childbirth 21(1):1–8. https://doi.org/10.1186/s12884-021-03651-6
Amu H, Aboagye RG, Dowou RK, Kongnyuy EJ, Adoma PO, Memiah P, Tarkang EE, Bain LE (2022) Towards achievement of Sustainable Development Goal 3: multilevel analyses of demographic and health survey data on health insurance coverage and maternal healthcare utilisation in sub-Saharan Africa. Int Health 0:1–16. https://doi.org/10.1093/inthealth/ihac017
Andersen RM (1995) Revisiting the behavioral model and access to medical care: does it matter? J Health Social Behav 1:1–10. https://doi.org/10.2307/2137284
Andersen RM (2008) National health surveys and the behavioral model of health services use. Med Care 1:647–653. https://www.jstor.org/stable/40221718
Andersen R, Newman JF (1973) Societal and individual determinants of medical care utilization in the United States. The Milbank Memorial Fund Quarterly. Health Soc 1:95–124. https://doi.org/10.2307/3349613
Anderson S, Eswaran M (2009) What determines female autonomy? Evidence from Bangladesh. J Dev Econ 90(2):179–191. https://doi.org/10.1016/j.jdeveco.2008.10.004
Bishanga DR, Drake M, Kim YM, Mwanamsangu AH, Makuwani AM, Zoungrana J, Lemwayi R, Rijken MJ, Stekelenburg J (2018) Factors associated with institutional delivery: Findings from a cross-sectional study in Mara and Kagera regions in Tanzania. PloS One 13(12):e0209672. https://doi.org/10.1371/journal.pone.0209672
Bloom SS, Wypij D, Das Gupta M (2001) Dimensions of women’s autonomy and the influence on maternal health care utilization in a north Indian city. Demography 38(1):67–78. https://doi.org/10.1353/dem.2001.0001
Comfort AB, Peterson LA, Hatt LE (2013) Effect of health insurance on the use and provision of maternal health services and maternal and neonatal health outcomes: a systematic review. J Health Population Nutri 31(4 Suppl 2):S81. https://www.ncbi. nlm.nih.gov/pmc/articles/PMC4021700/pdf/jhpn0031-suppl-2-0081.pdf
Dimbuene ZT, Amo-Adjei J, Amugsi D, Mumah J, Izugbara CO, Beguy D (2018) Women’s education and utilization of maternal health services in Africa: a multi-country and socioeconomic status analysis. J Biosocial Sci 50(6):725–748. https://doi.org/10.1017/S0021932017000505
Dong H (2012) The impact of health insurance in low- and middle-income countries. (Washington, DC. USA: the Brookings Institution Press, 2010, p 221). J Int Dev 24(4):529–530. https://ideas.repec.org/a/wly/jintdv/v24y2012i4p529-530.html
Fernandes P, Odusina EK, Ahinkorah BO, Kota K, Yaya S (2021) Health insurance coverage and maternal healthcare services utilization in Jordan: evidence from the 2017–18 Jordan demographic and health survey. Arch Public Health 79(1):1–1. https://doi.org/10.1186/s13690-021-00605-4
Firoz T, McCaw-Binns A, Filippi V, Magee LA, Costa ML, Cecatti JG, Barreix M, Adanu R, Chou D, Say L et al (2018) A framework for healthcare interventions to address maternal morbidity. Int J Gynecol Obstet 141:61–68. https://doi.org/10.1002/ijgo.12469
Gebremedhin TA, Mohanty I (2016) Child schooling in Ethiopia: The role of maternal autonomy. PloS one. 11(12):e0167639. https://doi.org/10.1371/journal.pone.0167639
Gebremedhin T, Mohanty I, Niyonsenga T (2020) Public health insurance and maternal health care utilization in India: evidence from a 2005-2012 mothers’ cohort study. https://doi.org/10.21203/rs.3.rs-116912/v1
Goli S, Rammohan A, Pradhan J (2016) High spending on maternity care in India: What are the factors explaining it? PloS One 11(6):e0156437. https://doi.org/10.1371/journal.pone.0156437
Hahn RA, Truman BI (2015) Education improves public health and promotes health equity. Int J Health Serv 45(4):657–678. https://doi.org/10.1177/0020731415585
Hijazi HH, Alyahya MS, Sindiani AM, Saqan RS, Okour AM (2018) Determinants of antenatal care attendance among women residing in highly disadvantaged communities in northern Jordan: a cross-sectional study. Reproductive Health 15(1):1–8. https://doi.org/10.1186/s12978-018-0542-3
IIPS, ICF (2021) National Family Health Survey-5, 2019-21, Ministry of Health and Family Welfare, Government of India, New Delhi. http://rchiips.org/nfhs/NFHS-5Reports/NFHS-5_INDIA_REPORT.pdf
Kassebaum NJ, Barber RM, Bhutta ZA, Dandona L, Gething PW, Hay SI, Kinfu Y, Larson HJ, Liang X, Lim SS, Lopez AD (2016) Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388(10053):1775–1812. https://doi.org/10.1016/S0140-6736(16)31470-2
Khan SM, Singh K (2016) The association between health insurance coverage and skilled birth attendance in Ghana: a national study. Mater Child Health J 20(3):534–541. https://doi.org/10.1007/s10995-015-1851-6
Kibusi SM, Sunguya BF, Kimunai E, Hines CS (2018) Health insurance is important in improving maternal health service utilization in Tanzania—analysis of the 2011/2012 Tanzania HIV/AIDS and malaria indicator survey. BMC Health Services Res 18(1):1-0. https://doi.org/10.1186/s12913-018-2924-1
Kumar S, Dansereau EA, Murray CJ (2014) Does distance matter for institutional delivery in rural India? Appl Econ 46(33):4091–4103. https://doi.org/10.1080/00036846.2014.950836
Kumar G, Choudhary TS, Srivastava A, Upadhyay RP, Taneja S, Bahl R, Martines J, Bhan MK, Bhandari N, Mazumder S (2019) Utilisation, equity and determinants of full antenatal care in India: analysis from the National Family Health Survey 4. BMC Preg Childbirth 19(1):1–9. https://doi.org/10.1186/s12884-019-2473-6
Lépine A, Strobl E (2013) The effect of women’s bargaining power on child nutrition in rural Senegal. World Dev 45:17–30. https://doi.org/10.1016/j.worlddev.2012.12.018
Lopez-Cevallos DF, Chi C (2010) Health care utilization in Ecuador: a multilevel analysis of socio-economic determinants and inequality issues. Health Policy Plann 25(3):209–218. https://doi.org/10.1093/heapol/czp052
Mahajan H, Sharma B (2014) Utilization of maternal and child health care services by primigravida females in urban and rural areas of India. Int Scholarly Res Notices. https://doi.org/10.1155/2015/125498
Masters SH, Burstein R, Amofah G, Abaogye P, Kumar S, Hanlon M (2013) Travel time to maternity care and its effect on utilization in rural Ghana: a multilevel analysis. Social Sci Med 93:147–154. https://doi.org/10.1016/j.socscimed.2013.06.012
McLaren ZM, Ardington C, Leibbrandt M (2014) Distance decay and persistent health care disparities in South Africa. BMC Health Serv Res 14(1):1–9. https://doi.org/10.1186/s12913-014-0541-1
Miteniece E, Pavlova M, Shengelia L, Rechel B, Groot W (2018) Barriers to accessing adequate maternal care in Georgia: a qualitative study. BMC Health Serv Res 18(1):1–2. https://doi.org/10.1186/s12913-018-3432-z
Mukherjee S, Singh A (2018) Has the Janani Suraksha Yojana (a conditional maternity benefit transfer scheme) succeeded in reducing the economic burden of maternity in rural India? Evidence from the Varanasi district of Uttar Pradesh. J Public Health Res 7(1). https://doi.org/10.4081/jphr.2018.957
Murray CJ, Lopez AD (1997) Alternative projections of mortality and disability by cause 1990–2020: global burden of disease study. Lancet 349(9064):1498–1504. https://doi.org/10.1016/S0140-6736(96)07495-8
Nuamah GB, Agyei-Baffour P, Mensah KA, Boateng D, Quansah DY, Dobin D, Addai-Donkor K (2019) Access and utilization of maternal healthcare in a rural district in the forest belt of Ghana. BMC Preg Childbirth 19(1):1–1. https://doi.org/10.1186/s12884-018-2159-5
Rai RK, Singh PK, Singh L (2012) Utilization of maternal health care services among married adolescent women: insights from the Nigeria Demographic and Health Survey, 2008. Women's Health Issues 22(4):e407–e414. https://doi.org/10.1016/j.whi.2012.05.001
Randive B, San Sebastian M, De Costa A, Lindholm L (2014) Inequalities in institutional delivery uptake and maternal mortality reduction in the context of cash incentive program, Janani Suraksha Yojana: results from nine states in India. Social Sci Med 123:1–6. https://doi.org/10.1016/j.socscimed.2014.10.042
Sakeah E, Okawa S, Rexford Oduro A, Shibanuma A, Ansah E, Kikuchi K, Gyapong M, Owusu-Agyei S, Williams J, Debpuur C, Yeji F (2017) Determinants of attending antenatal care at least four times in rural Ghana: analysis of a cross-sectional survey. Global Health Action 10(1):1291879. https://doi.org/10.1080/16549716.2017.1291879
Shah R, Rehfuess EA, Paudel D, Maskey MK, Delius M (2018) Barriers and facilitators to institutional delivery in rural areas of Chitwan district, Nepal: a qualitative study. Reprod Health 15(1):1–13. https://doi.org/10.1186/s12978-018-0553-0
Singh P, Singh KK, Singh P (2021) Maternal health care service utilization among young married women in India, 1992–2016: trends and determinants. BMC Preg Childbirth 21(1):1–3. https://doi.org/10.1186/s12884-021-03607-w
UNICEF (2022) Antenatal care. UNICEF DATA. Available from: https://data.unicef.org/topic/maternal-health/%20antenatal-care/. Accessed on March 2022
Wang W, Temsah G, Mallick L (2017) The impact of health insurance on maternal health care utilization: evidence from Ghana, Indonesia and Rwanda. Health Policy Plann 32(3):366–375. https://doi.org/10.1093/heapol/czw135
Were LP, Were E, Wamai R, Hogan J, Galarraga O (2017) The association of health insurance with institutional delivery and access to skilled birth attendants: evidence from the Kenya demographic and health survey 2008–09. BMC Health Serv Res 17(1):1-0. https://doi.org/10.1186/s12913-017-2397-7
WHO (2017) Maternal health. Retrieved from http://www.who.int/maternal-health/en
WHO (2019) Maternal mortality: fact sheet. Available online: https://www.who.int/news-room/fact-sheets/detail/maternal-mortality
WHO (2021) Universal health coverage (UHC), 2021. Available at: https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(UHC)
WHO & UNICEF (2003) Antenatal care in developing countries: Promises, achievements and missed opportunities an analysis of trends, levels and differentials. 1990-2001. WHO Geneva. Bulletin of World Health Organization
World Bank (2019) Data bank: world development indicators. [cited 2019 November 15]. Available from: http://databank.worldbank.org/data
Wu Y, Zhou H, Wang Q, Cao M, Medina A, Rozelle S (2019) Use of maternal health services among women in the ethnic rural areas of western China. BMC Health Serv Res 19(1):1–2. https://doi.org/10.1186/s12913-019-3996-2
Yaya S, Da F, Wang R, Tang S, Ghose B (2019) Maternal healthcare insurance ownership and service utilisation in Ghana: analysis of Ghana demographic and health survey. Plos One 14(4):e0214841. https://doi.org/10.1371/journal.pone.0214841
Yaya S, Zegeye B, Ahinkorah BO, Seidu AA, Ameyaw EK, Adjei NK, Shibre G (2021) Predictors of skilled birth attendance among married women in Cameroon: further analysis of 2018 Cameroon Demographic and Health Survey. Reprod Health 18(1):1–2. https://doi.org/10.1186/s12978-021-01124-9
Zere E, Oluwole D, Kirigia JM, Mwikisa CN, Mbeeli T (2011) Inequities in skilled attendance at birth in Namibia: a decomposition analysis. BMC Preg Childbirth 11(1):1-10. https://doi.org/10.1186/1471-2393-11-34
Acknowledgements
We sincerely thank the IIPS Director and Principle Investigators of the NFHS project. We also thank all reviewers and the editorial board of this journal.
Author information
Authors and Affiliations
Contributions
All the authors contributed significantly to this paper. The research idea, conceptualization and study design: RDP and KG; Collected data and analysed the data: KG and RDP; Gathered material and wrote the manuscript: KG, RDP and NS; Refined and finalized the manuscript: NS and RDP.
Corresponding author
Ethics declarations
Ethics approval
There is no formal ethics approval required for this particular study since the study is based on secondary data and the survey data is available in the public domain.
Consent to participate
Not applicable
Consent for publication
Not applicable
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Prasad, R.D., Ghosh, K. & Shri, N. Does health insurance coverage improve maternal healthcare services utilization in India? Evidence from National Family Health Survey-5, 2019–21. J Public Health (Berl.) (2023). https://doi.org/10.1007/s10389-023-01960-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-023-01960-y