Abstract
Aim
Smart wearable devices for continuous monitoring of health conditions have bbecome very important in the healthcare sector to acquire and assess the different physiological parameters. This paper reviews the nature of physiological signals, desired vital parameters, role of smart wearable devices, choices of wearable devices and design considerations for wearable devices for early detection of health conditions.
Subject and methods
This article provides designers with information to identify and develop smart wearable devices based on the data extracted from a literature survey on previously published research articles in the field of wearable devices for monitoring vital parameters.
Results
The key information available in this article indicates that quality signal acquisition, processing and longtime monitoring of vital parameters requires smart wearable devices. The development of smart wearable devices with the listed design criteria supports the developer to design a low power wearable device for continuous monitoring of patient health conditions.
Conclusion
The wide range of information gathered from the review indicates that there is a huge demand for smart wearable devices for monitoring health conditions at home. It further supports tracking heath status in the long term via monitoring the vital parameters with the support of wireless communication principles.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The field of smart wearable technology has grown quickly in recent years and advances in wearable biosensing led to the development of more facile measurement systems. Advanced techniques and sensing principles haved helped in the miniaturization of wearable medical devices. The development of different wearable sensors and their integration with processing units enables the measurement of biosignals. Simultaneously, the conceptualization of using multiple biosensors in a single portable device also gained increased attention. The application of such different modalities helps to overcome the limitation of a specific biosensor over another. The use of biosensors in wearable devices varies based on the application of the device. The wide range of applications of wearable devices supports use in healthcare networks, sport activities, for military personnel and environmental health monitoring.
In recent years, various diseases such as COVID-19, cardiovascular diseases, tumours and chronic illnesses are affecting patients’ health conditions drastically, and they need to be monitored continuously. In critical care units, continuous 24-h monitoring of heart rate, respiration rate, blood pressure, blood oxygen saturation, blood glucose level and body temperature are essential. Wearable medical devices help to monitor these vital signs continuously and provide useful information for disease diagnosis. The benefits include vital sign acquisition during ambulatory condition and continuous monitoring of wellness over the long term. The information gathered can be effectively used for disease diagnosis and to deliver proper treatment at the right time. Wearable health devices not only support identifing diseases but also help in predicting diseases to improve the quality of life of patients. IoT-based wearable devices enhance the affordability and improve the quality of health care. The information gathered using the biosensors are stored and transmitted through the wireless communication protocols to the remote locations for monitoring, guiding patients remotely during an emergency situation and providing them timely treatment. Wearable technology shows enormous potential in the healthcare system due to uninterrupted monitoring of human physiological indicators in real time. It is crucial for keeping track of people’s fitness and critical health issues during their daily activities without interfering with their regular tasks. In recent years, extensive efforts have been made by many researchers to develop innovative and more reliable wearable devices. These wearable devices acquire the signals and estimate the vital parameters such as heart rate, respiratory rate, blood pressure, body temperature, oxygen saturation and pulse rate. The Internet of Things (IoT) and wearable devices can be integrated together in healthcare applications for remote applications in healthcare environments. This paper briefly describes the nature of different biosignals and sensors used for the evaluation of vital signs and narrates the different vital parameters used for diagnosis purposes. This paper also focusses on different wearable devices along with the IoT in the healthcare system for identifying, diagnosing and remote monitoring, and it concludes by presenting the design consideration for the implementation of smart wearable devices. This paper is organized into five sections. Section I includes the different biosignals generated from the human body for identifying vital signs. Section II explains the importance of the different vital signs used for medical diagnosis. Section III provides the recent progress in smart wearable devices for obtaining the essential vital parameters. Section IV explains the importance of the IoT in smart wearable devices, and Section V concludes the paper by narrating the design considerations for wearable devices.
Biosignals: origin and characteristics
Biosignals are the bioelectric signals generated from the electrical activities of organs. They are the change in electric current due to the electric potential difference over particular organs or tissues such as the cardiovascular system, neural system, respiratory system, etc. Different biosignals are generated from the human body based on electrical activities. Some of the bioelectric signals are electrocardiogram (ECG), photoplethysmogram (PPG), electroencephalogram (EEG), electromyogram (EMG), electrooculogram (EOG), galvanic skin response (GSR), electroretinogram (ERG) and electrogastrogram (EGG). This section of the paper depicts the features of ECG, PPG and EEG signals with their graphical waveforms.
Electrocardiogram (ECG)
ECG is a method that uses cables, electrodes and gels to identify problems related to the cardiovascular system. An ECG records the heart’s electrical activities by placing the electrode above the skin at a particular location of the body. To diagnosis heart diseases, different wave patterns are obtained from an ECG signal, such as P, Q, R, S and T waves, which contribute crucial information about how the the heart is working. The obtained wave pattern includes the prominent peaks and valleys of the P, Q, R, S and T waves. Normal human ECG signals have a frequency range of 0.05–120 Hz, and it has very low amplitude in milli volts. The P wave is generally used to represent the atrial depolarization of the heart whose duration is less than 0.11 s and 0.25 mV amplitude. The QRS complex is the most common wave pattern used for diagnosing different diseases. It represents the ventricular depolarization with the duration of 0.08–0.10 s. The first negative deviation in the QRS complex is the Q wave with a typical amplitude of 25% of R wave; the R wave is seen, which is the positive deviation with amplitude 1.60 mV, and the negative deviation ends with the S wave. The T wave is the representation of ventricular depolarization with an amplitude of 0.1 to 0.5 mV. The PR interval is the time duration taken from the initial atrial depolarization to the initial ventricular depolarization and the atrioventricular nodal delay. Time duration of the PR interval is 0.12 to 0.20 s. The QT interval is a measure of both the ventricular depolarization and repolarization within the duration of 0.20 to 0.40 s. The ST segment shows the isoelectric period of depolarized ventricles.
Figure 1 shows the wave pattern generated from the electrical activities of the human heart. One of the most important features obtained from an ECG is the R peak (Merah et al. 2015). The location of other wave patterns can be identified using this R peak as a reference point. QRS detection has the most significant role in disease diagnosis (Tang et al. 2018). The QRS detection system is classified into two categories. One of these categories needs extra computational support through digital signal processors (DSP), and the second category merges DSP and analog to digital converters (ADC) that process data in real time. From the literature, it was observed that the needed information for diagnosis can be obtained by detecting the intervals and amplitudes generated by the characteristic wave peaks and boundaries of ECG signals.
Photoplethysmogram (PPG)
Photoplethysmography plays a major role in identifying changes in blood pressure. The PPG sensor can estimate the heartbeat without any electrodes. A normal PPG signal is generated by pulse oximeter based on the change in light absorption by illuminating the skin. It monitors how the blood is pumped into the dermis and the tissue beneath the skin. A light-emitting diode (LED) is used to illuminate the area, and the change in blood volume caused by the pulse pressure is recorded by either measuring the light reflected to the photodiode or by monitoring the quantity of illumination transmitted (Volkov et al. 2017). It operates at red or near infrared wavelength. The use of green light is highly preferred in PPG sensors due to its capability of balancing the light absorbance and the penetration of light (Fallow et al. 2013).
A steady-state or non-pulsatile direct current (DC) component and an oscillating or pulsatile alternating current (AC) component make up a typical PPG signal (Lee et al. 2013). AC components are associated with the blood flow in the arteries synchronized with the heartbeat, and the DC components are associated with the venous blood volume regulation in addition to non-pulsatile components of the arteries. To block the receiver saturation, the DC components in the reflected light should be eliminated as it reaches 99% of the original signal (Lee et al. 2016a, b). The direct pressure applied from the heart’s left ventricle towards the periphery of the body is called the systolic peak and the reflection of pressure exerted by the arteries from the lower valves of the body is called the diastolic peak which is also known as inflection. The dicrotic notch is the node at which the aortic valves are closed and generated before the secondary dicrotic wave. The PPG frequency range is very low ranging from 0.5 Hz to 4 Hz (Peng et al. 2014). The characteristics of the PPG wave pattern comprise peaks and valleys, namely systolic peak, dicrotic notch and diastolic peak (Liu et al. 2018), as shown in Fig. 2.
Electroencephalogram (EEG)
Electroencephalogram is a non-invasive method for diagnosing the different neurological conditions by acquiring the brain impulses from the surface of the human scalp through an electrode. The voltage fluctuations generated by the ionic current produced in the brain neurons are measured using the EEG signal. The representation of different EEG wave patterns is depicted in Fig. 3.
An EEG is used to diagnosis epilepsy, tumors, stroke, sleep disorders and brain deaths. While acquiring the EEG signal, oscillation occurs due to multiple frequencies. These oscillations are based on the different conditions of brain functioning. The EEG waveform is classified based on the signal frequency, amplitude of the signal, morphology and continuity of the signal, and location of the signal (Nayak and Anilkumar 2021). The amplitude of the EEG is measured in terms of microvolts (μV). The EEG signal frequency ranges are referred to as delta from 0.5 to 4 Hz, theta from 4 to 7 Hz, alpha from 8 to 12 Hz, beta from 13 to 30 Hz and gamma from 25 to 140 Hz.
Need for physiological vital parameter
Vital parameters are the measurements of key indicators to detect the diseases which can be estimated through the signal processing methods. The most common vital signs include heartbeat, respiration rate, body temperature, blood oxygen saturation and blood pressure. Vital signs provide the critical information about the body organs and show the variation in an organ’s functioning inside the body. Wearable devices play an important role in monitoring these vital signs continuously either at a clinic or at home. Vital signs may vary from person to person based on their age, health status and weight. The most essential and common vital signs required for identifying the health status of the patients are shown in Fig. 4.
Heart rate (HR)
The number of times the heart beats in a minute is known as the heart rate or pulse rate. The heart rate fluctuates from time to time and from person to person. An adult normal heart rate ranges from 60 to 100 beats per minute, whereas the normal heart rate for children ranges from 70 to 100 beats per minute at resting condition. The heart pumps the blood to all parts of the body to supply the required oxygen and other nutrients. During resting condition, the heart pumps a minimal amount of blood for suppling oxygen to the brain and all vital organs. Measurement of HR indicates the heart rhythm. Fast HR or tachycardia represents heart beats that are greater than 100 times per minute, and slow HR or bradycardia shows the HR less than 60 beats per minute during resting condition. A sudden change in HR represents irregular functioning of the heart and also shows symptoms such as fatigue or dizziness and fainting.
HR can be measured using ECG or by PPG signals (Jegan and Nimi 2018). Though ECG and PPG signals have different morphological wave patterns, the HR information obtained by ECG and PPG is very similar. HR can also be measured by ballistocardiogram (BCG) (Giovangrandi et al. 2012), inertial sensors (Aarts et al. 2017) and phonocardiogram (PCG) (Brusco and Nazeran 2005), but the accuracy of HR obtained by BCG and PCG are very low compared to ECG and PPG. Heart rate variability can also be evaluated to assess the health status of the person with cardiovascular issues. HR measurement is done for many disease diagnoses such as sleep apnea (Jung et al. 2017), arrhythmia recognition (Zhu et al. 2019) and stress measurements (Erika et al. 2018).
Respiration rate (RR)
Respiration rate refers to the measure of the number of breaths a person takes in one minute. The respiratory system exchanges oxygen and carbon dioxide to satisfy the energy requirements of a person. RR is measured during the resting condition by counting the number of breaths per minute based on the movement of the chest or the number of times that the chest rises in one minute. The wave pattern is generated due to the inspiration and expiration caused by the change in chest volume. Normal RR ranges from 12 to 18 breaths per minute for adults and 18 to 60 for children. Table 1 shows the ranges of respiration rate for all ages.
Elastomeric plethysmography, impedance plethysmography, accelerometers, polymer-based sensors, optical fibres and respiratory inductive plethysmography are some of the methods used to determine respiration function. The RR measurement provides an early indication of acidosis. RR is one of the major sensitive indicators in critical health illnesses such as distress and potential hypoxia and plays a major role in predicting cardiac arrest (Malcolm and Alysia 2012). Rapid change in respiration rate shows different patterns of respiration such as eupnoea (respiration at resting or normal condition), bradypnea (respiration rate is too low) and tachypnoea (respiration rate is higher) (Fekr et al. 2014). Monitoring respiratory rate when moving is very essential in the diagnosis of sleep apnea, chronic obstructive pulmonary disease and asthma, and it is very important for monitoring children with pulmonary diseases.
Blood pressure (BP)
Basically, the arteries may expand and contracts due to blood flow when the heart pushes blood along the arteries. The force exerted on the blood against the artery is known as blood pressure. Systolic and diastolic pressure values are used to record blood pressure. Blood pressure can be measured in mmHg (millimeters of mercury). The highest arterial pressure that can exist while the left ventricle of the heart contracts is known as systolic pressure. Systole represents the period at which the ventricular contraction takes place. The heart pumps blood through blood arteries to all regions of the body during the systolic period. Diastolic pressure is the term used to describe the lowest arterial pressure that is experienced when the heart’s ventricles relax. Diastole represents the period at which the ventricular relaxation takes place. During the diastolic period, the heart chamber fills with blood and the blood pressure is reduced. The normal blood pressure range is 120/80 (systolic/diastolic) mmHg. Table 2 explains different blood pressure levels. The traditional method to measure BP uses an inflatable pressure cuff with a stethoscope which is wrapped around the user’s arm (Dias and Paulo 2018).
Variation in BP causes stroke, heart failure and increases the risk for heart attack. BP is to be regularly checked even for asymptomatic persons. In most cases, a person with hypertension shows no symptoms. Hypertension is one of the major threats to society which causes cardiovascular diseases. Cardiovascular diseases can be highly predicted by monitoring BP continuously.
Blood oxygen saturation (SpO2)
Blood oxygen level represent the amount of oxygen carried by the red blood corpuscles. Blood oxygen saturation is the amount of blood hemoglobin that is occupied by oxygen in the blood stream. It is the ratio of the oxygenated hemoglobin to the sum of the oxygenated and deoxygenated hemoglobin which exists in the blood.
where HbO2 represents the oxygenated hemoglobin and Hb represent unsaturated or deoxygenated hemoglobin. The normal blood oxygen saturation level is 95 to 100%. The reduction in oxygen level leads to shortness of breath, headache, chest pain, rapid heartbeat and symptoms of cyanosis. It is difficult to survive for a prolonged period if the oxygen supply to the human brain is not constant. The percentage of oxygenated hemoglobin is determined using optical transducers which are directly applied to the skin. SpO2 measurement alone cannot provide accurate diagnosis in some cases. The PPG signal and signal processing methods can be integrated and evaluate the SpO2 by measuring the changes in blood vessels using the two different wavelengths 660 nm and 905 nm. SpO2 can be effectively measured from the fingers through oximetry principles.
Blood glucose (BG)
Blood glucose level is the estimation of the concentration of glucose which exists in human blood. In the human body, around 4 grams of glucose are stored in the liver cells and skeletal muscles continuously in the form of glycogen. Food plays a major role in the formation of sugar content in the human body. The generated simple sugars are transmitted to all the body cells to provide an energy source to the cells through the bloodstream. The blood glucose level is measured in terms of mg/dL (milligrams per decilitre) or mmol/L (millimoles per litre). Table 3 shows the blood glucose level before and after intake of food.
Nowadays, the effects of diabetes are rapidly increasing globally. The risks of diabetes, mainly hyperglycaemia and hypoglycaemia, cause major health issues. Hypoglycaemia is the state at which the blood sugar level falls too low, whereas hyperglycaemia is due to an excess glucose level. Both of these stages if not properly identified may leads to many health issues. Diabetes may also lead to various physiological abnormalities such as cerebral vascular disturbance, macrovascular complications, nephropathy and retinopathy. These complications can be avoided by maintaining the glucose level in a standard normal range or by injecting insulin into the human body to controll the blood glucose concentration if there is a change in blood glucose level.
Body temperature
Body temperature evaluates the temperature or heat that the human body can withstand and measures the amount of heat that can be lost by the human body. Generally, there is a variation in human body temperature based on the age of the person, time of the day, health condition of the person and the exertion level. It is the consequence of balancing among the temperature generation and temperature reduction in the physical body (Teng et al. 2008). There are two ways to monitor body temperature: via the skin and via the core (Buller et al. 2013). Core body temperature is the heat generated in the internal organs such as blood, heart, brain and liver of the human body. Skin body temperature is the measure taken from the peripheral surface of the body such as mouth, ear and armpit. The circulation of blood affects the skin body temperature which is correlated with the heart rate and metabolic rate. Additionally, body temperature is impacted by the circulation of air, atmospheric temperature, climatic condition and humidity (Gaura et al. 2013]. Table 4 shows the ranges of body temperature. Figure 4 displays some of the vital signs measured using different wearable devices.
Smart wearable devices: need and significance
In the healthcare network, smart wearable devices play a major role in real-time monitoring of different physiological parameters of the human body. Wearable devices with the help of various biosensors provide easy monitoring of the electrical activities of the body. It is quite challenging to deliver adequate therapy in real time today. Hence, a number of variations in health care devices are preferred for disease diagnosis. Especially during pandemic situations, it is vital to monitor the patient’s health status frequently. If the physiological status or the abnormalities are not properly recognized, it may lead to severe health related problems such as organ failure, or even death. Many of the public healthcare systems make use of conventional medical devices that require a high cost and can lead to congestion in most of the clinical centres, which makes the patients restless and stressed. Therefore, it is very important to diagnose diseases in a comfortable zone and with low cost. There is a very essential and immense need in the medical field to detect different diseases personally in tandem with cutting-edge technologies. Smart wearable devices have rapidly increased in recent days due to miniaturization of the devices, flexibility, higher efficiency and their non-invasiveness. The wearable devices to date are limited because only certain physiological parameters can be measured by a single wearable device. There is a huge need to develop a smart wearable device for monitoring multi parameters of patient health conditions.
Evolution of wearable devices
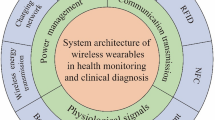
Wearable devices are developed with a great difference from the existing medical devices in view of portability, their user approachability and environmental flexibility (Guk et al. 2019). The advancement in electronics, biocompatibility and nanomaterials have allowed the development of implantable devices for disease diagnosis with the help of tiny sensors. The evolutions of flexible and skin-attachable electronic devices are also beneficial in identifying vital signs without any disturbance. Current wearable devices are developed with multiple functions which act as a microcomputer that authorizes the connection of the entire system, data gathering and processing to external communication. These devices communicate with external devices through wireless technologies such as bluetooth, radio-frequency identification (RFID), wireless fidelity (WiFi), long range (LoRa) protocol, and near-field communication (NFC). Wearable technology is employed for remote and ongoing continuous monitoring with the support of the IoT in homes and the healthcare industry.
Basically, the large conventional machines are used in healthcare for acquiring the signal and predicting the diseases. The portable devices are designed in multiple patterns and classified based on their attachment to the body. They are classified as wrist worn devices such as watches, rings, bracelets and gloves, head devices such as glasses, mouth guards, helmets and clothing such as coats, singlets, pants and belts (Gui and Liu 2018). The technique implemented in the portable device is a non-invasive monitoring technique with two basic functions: continuous observation of physiological indicators and external communication with other smart electronic devices. Physiological signals, such as heart rate, respiration rate, body temperature, SpO2 and blood glucose levels, can be measured and monitored using portable devices. Figure 5 depicts the development stages of wearable devices.
Wearable devices can be further integrated with flexible nanomaterials and become attachable monitoring devices through a flexible substrate. The combination of polydimethylsiloxane (PDMS) and silver nanowires can be used for designing a biosensor which will be effectively applicable for collecting biosignals. The advantage of an attachable device are its flexibility and adaptability to the skin. It also provides an accurate sensing without any discomfort. In attachable devices, the sensors are attached to the skin or fitted to the surroundings such as chairs, car seats, etc. Skin patches and contact lenses are some of the attachable devices developed in the biomedical instrumentation research domain. A skin patch is a soft, malleable and stretchable bio-electronic device that can be affixed to bodily tissue for continuous medical monitoring (Liu et al. 2017). A skin patch provides more accurate information as it is not disturbed by body movement. Contact lenses use both optical and electrical methods for continuous monitoring of the chemical concentration in the eye membrane and measure the electrical conductivity of the eye via tear fluid (Elsherif et al. 2018).
MEMS technology are used in developing the implantable devices (Kiourti et al. 2013). Implantable devices are inserted either fully or partially into the body through surgeries or through some medical procedures. Hence, implantable devices should be designed with utmost care such that it should not affect health. Cardiac pacemakers, tattoo-based glucose detection device, electronic tattoos (e-tattoos), Abbot confirm RX implantable devices and bio sensitive inks (bioinks) are some of the implantable devices available in the biomedical research domain. A non-invasive method used to acquire the fluid information of the human body is an ingestible sensor (Kalantar et al. 2017). It is used to monitor the various hormones, enzymes around the abdomen and the biometric information. An ingestible pill is one of the ingestible sensors used for monitoring the fluid content in the human body. After being ingested into the body, the stomach acid activates the pill due to the chemical reactions inside the stomach and delivers the signal to the body patch. The patch helps to monitor HR, BP, pH and body temperature along with external communication. Wireless technology in implantable and ingestible devices allow transferring the gathered information without loss of data, and it also maintains the device’s functioning and battery status.
Recent development of wearable devices
Electronic devices embedded with biosensors in the form of fitbits, jewels, smart glasses and smart watches have been developed for continuous monitoring and collecting of information about the user’s health status. During recent decades, the number of wearable health devices has increased based on the need for early identification of diseases, quality of the signal acquired and self-monitoring purposes (Jegan and Anusuya 2015). Due to the increased demand of self-monitoring, development of the wearable devices is also increased multiple times for the last few years (Alicia 2019). Researchers are currently working to develop a smart wearable health device with greater advantages in application and functionality. Wearable devices are integrated with smart sensors, IoT, artificial intelligence (AI), data processor and robots for managing and preventing various diseases. Figure 6 shows the different forms of portable wearable devices used in medical applications to measure vital signs.
The most prevalent wearable technology is wrist worn devices used for continuous monitoring of vital signs. Wrist watches have higher farm factor than wrist bands (Nimi et al. 2021). Smart watches are mostly preferred by athletes and patients with cardiac problems for monitoring workout time, energy level, heart rate and calories burnt. Modern technologies and tiny biosensors are integrated with glasses and attached to helmets or Google Glasses in head mounted devices. EEG and EOG sensors are used to measure physiological signals from the brain or ears to diagnose disorders. There are also devices such as mouth guards, hearables, head bands, smart glasses, helmets for measuring different physiological signals from the electrical activities of the brain, eyes, saliva and ears. A person’s behaviour can be monitored by their facial expressions, person-to-person interaction, conversational period and other physical activities with the help of an electronic badge developed for the wearable computing platforms (Daniel et al. 2009). The Oura ring is used to measure the quality of the user’s sleep based on their eye movement and sleep balancing (Oura Ring 2017).
Monitoring vital signs is very important for the patient to identify their health condition and to detect the clinical deterioration. Early warning scores with multiparameter helps to detect the change in physiological signals which further identifies the risk level of the patient, thereby reducing unplanned admissions to the intensive care unit (ICU) that helps to reduce mortality. Continuous monitoring is required to identify the clinical deterioration as early as possible, which helps the physician to provide proper treatment at the correct time to avoid critical conditions. Table 5 gives the details of different wearable devices developed for extracting different vital signs in different applications.
Wearable devices provide an easy view of patients at all times by monitoring the vital signs instantly (Boatin et al. 2016). It also improves patients’ comfort with fewer measurements. The electrodermal activity of a person can be detected using a wearable neoprene band that serves as a solution for patients with alcoholic addiction and stress disorder (Fletcher et al. 2011). Respiration rate can be measured by monitoring the chest movement by an adjustable fabric chest strap (Zephyr 2016). Continuous use of cuffs for monitoring blood pressure causes skin irritation in some patients, and also increases the stress level of the patient (Yilmaz et al. 2010). This can be avoided by developing a cuffless non-invasive method with advanced signal processing algorithms. One of the best ways to measure the BP is identifying the pulse transmit time acquired from the wrist PPG and chest ECG signals (Puke et al. 2013). Blood pressure can be measured using pulse wave velocity obtained from two microelectromechanical sensors attached to the wrist and neck (Hsu and Young 2014). A watch-type prototype is developed using a pressure sensor which is placed in the radial artery to estimate accurate blood pressure with the help of smart phones (Woo et al. 2014). Respiration rate can be obtained using a dielectric active polymer based on the fluid metals. The chest volume variations are measured based on this dielectric active polymer (Xiaohui et al. (2017). To determine the blood oxygen saturation, PPG signals are also employed. Ring type wearable devices are mostly used for measuring the SpO2 because blood oxygen saturation levels can be easily obtained from a finger.
Recently, tiny chips on ear lobes are used to measure SpO2, and brain oxygenation can be measured using PPG sensors placed on the forehead (Mendelson et al. 2013). SpO2 can also be estimated by integrating the PPG sensors into optical fibers which are embroidered with textile to analyse the various depths of the tissues. They use optical fibers as light-sources and detectors (Krehel et al. 2014). Also, it can be monitored by integrating the e-textiles with flexible plastic strips consisting of LEDs and photodiodes. Glucowatch is a commercial device used to monitor the glucose level of blood (Tierney et al. 2001). The glucose level is monitored through reverse iontophoresis and the information is provided to the user every 20 min. Dexcom is used to monitor the glucose level continuously, which consists of a fully implantable sensor for monitoring the glucose level. There are multiple devices developed for measuring the vital signs using different techniques. An oximeter built into a ring is used to measure the heart rate (Boo and Sokwoo 2000), a wrist band with an electrodermal sensor is used to estimate the stress level (Sandulescu et al. 2015), an electromyographic sensor integrated within the clothing is used to monitor muscle activity (Finni et al. 2007) and a smart watch with an accelerometer can be used to monitor the physical activity of the user (Yang and Hsu 2010).
Choices of wearable devices in healthcare applications
The development of smart wearable devices in the healthcare network provides a flexibility to measure and monitor certain vital parameters. The accurate measurement of different vital parameters helps the doctor to analyse and predict the health status. The different vital parameters, including pulse rate, blood pressure, respiration rate, SpO2, temperature, blood glucose level, body mass index, heart rate variability, body fitness and sweat rate, can be monitored using sensors which are integrated in singlet (Salvo et al. 2010). The need for suitable wearable devices in the healthcare domain and public environment will be drastically increasing to monitor and control applications. By anticipating the need for caution and warning the driver via cell phones, smartwatches help to reduce traffic accidents. The test was administered to individuals of various ages, and results were contrasted by including and excluding gender type (Lee et al. 2016a, b). A smart helmet has been developed that uses robust multivariate signal processing to find the R peaks in noisy ECG and EEG inputs to avoid traffic accidents (Rosenberg et al. 2016). A smartphone app has been designed and built for tracking changes in parameters relating to a person’s physiological health state while they move. It automatically alerts users during potentially harmful health conditions (Botilias et al. 2022). The use of different wearable devices and their applications are summarized in Table 6.
IoT in smart wearable devices
Smart wearable devices help healthcare providers to monitor patients’ conditions in clinics based on real-time requirements. They also update the information about the users’ physiological conditions during their daily activities through a wireless network to a remote monitoring centre or to monitor themselves. The information gathered is also recorded in medical information systems for further offline processing. Wearable health devices are used to monitor and communicate patients’ data who are hospitalized, via cloud/server to the medical professional to provide useful information about the treatment or to indicate emergencies. Vital signs are also transmitted to another portable devices through wireless communication protocol for displaying and examining the users’ state of health. The coordination of the users and the communication module is sustained effectively for safer transmission. The vital signs can be stored in clouds or micro-SD memory cards for future reference and medical diagnosis. Thus, IoT has the potential to integrate different medical devices, biosensors and the professionals in the healthcare network to provide efficient health services from an isolated place. IoT in healthcare networks enhances the safety of the patients, minimizes the medical expenses and improves the efficiency of the health maintenance network. One of the major concerns while implementing an IoT-based wearable devices is sustaining the quality of service provided such as the security of data transmitted, privacy of the patient’s information, reliability, flexibility and expenses.
The IoT value chain explains all the activities carried out in developing a wearable medical device. The value chain changes according to the application used, level of experience, in-built hardware and software platform, reliability of the requirements, processor used, processing methods and the connectivity towards cloud processing. Figure 7 highlights the IoT value chain for wearable medical devices. According to global data, the wearable technology is mainly classified based on application layer, connectivity layer, data layer and the device layer.
The application layer is centred on process-to-process communication to provide the end user service through the Internet Protocol (IP) network. Two parts make up the application layer. The apps, i.e. the software developed is the first category, and the second section is the platforms that act as the environment where the software can be executed. The connectivity layer deals with the communication between the human and their digital surroundings. For real-time communication, wearable technology makes use of smartphones, which makes the body-worn devices fully automatic. There are different connectivity tools such as Bluetooth, LoRa, NFC, RFID, WiFi and other tools that link with smartphones. If the communication does not require any real-time processing, then the connectivity can be done with the support of universal serial bus (USB) and ethernets. The data layer provides the storage and computation environment, and the interface to the device layer. It helps to transmit the information from the biosensors into the databases. Different learning algorithms are used to analyse these data and it is transmitted again to the users via a web server or to the device itself.
Design consideration for implementation of wearable devices
Worldwide, the disease rate of COVID-19 drastically increased among people in a short span. In pandemic situations, continuous monitoring is essential not only for the patients but for every individual. It is essential to continuously monitor every vital sign such as body temperature, blood pressure, blood glucose level, oxygen saturation, heart rate and respiration rate. However, in the healthcare network, it is a challenging task to provide medical services to multiple patients simultaneously. The expense of the medical service and medical equipment, lack of space available in hospitals, limited number of physicians for providing treatment, all make monitoring the individual’s health status and their activities very difficult. The wearable health devices act as a supportive mechanism to overcome this situation by providing self-monitoring in home or by monitoring the patients remotely. It helps in early detection of diseases and provides alerts in emergency situations. Many research studies are investigating the development of smart devices in the medical environment for monitoring the patient’s physiological activities. Commercially, there are different wearable devices developed by numerous vendors so far for various healthcare applications. Since the wearable devices are body attached, certain design considerations should be satisfied during the development stage of wearable health devices, including affordability (Svanaes 2013), comfort, safety, reliability, responsiveness and user friendliness (Cho 2010), contextual awareness (Armagan and Cigdem 2011), ergonomy (Lin et al. 2020), ease of use, simplicity, fashion, wearability and intuitiveness (Dan et al. 2008), connectivity (Staff 2015), and obtrusiveness and privacy (Darko et al. 2007).
The ultimate goal in designing a smart wearable health device is that it must have low power consumption or be self-powered, quality signal acquisition, early predictability or detection of disease and long-term continuous monitoring. Power consumption is one of the major factors to be considered while designing a wearable device as the entire system requires a power supply to operate the device for continuous monitoring. Also, the choice of modules such as biosensors, the processor and wireless modules may further reduce the power consumption. The alternate solution to reduce the power consumption is integrating the device with an energy harvesting unit. The role of an energy harvesting unit is to deliver the required energy to the device and store energy in batteries and super capacitors for future use. The energy harvesting unit can be designed by accumulating the energy generated from the surroundings through an efficient power management unit. This helps in continuous monitoring of vital signs both in indoor and outdoor environments. The other method to reduce the power consumption will be designing the system with sleep mode functionality. This will help the device for long-term monitoring without any interruption. Implementing various wireless technologies in the device is also a necessary component while designing the wearable device. The physiological signal and vital parameters can be continuously monitored and transmitted to the physicians or to themselves only based on the wireless communication network. Data synchronization is to be prioritized when working with multiple sensors within a device. These design criteria help the designer to develop wearable health devices for different healthcare applications.
Conclusion
This paper presents the importance of the different smart wearable devices for monitoring physiological and vital signs of individuals. The information presented in this paper helps designers to identify the essential requirements for designing smart devices for healthcare networks. The integration of the IoT with wearable devices provides easy communication of data to remote locations to provide timely support to the patients. The development of low power wearable devices is very important to offer continuous long-time monitoring of certain vital parameters. This article narrated the design considerations during the development phase of smart low power wearable devices for measuring vital signs. It is concluded that the details about the different sensors used, the vital signs to be monitored continuously, choices of different wearable devices and design considerations will help the designers and the researchers to develop new smart wearable devices for quality signal acquisition and effective processing and monitoring of vital parameters for adults and children to further provide enhanced cardiac care to patients. Also, the information available in this article helps the public to identify the need for suitable wearable devices to measure certain vital parameters for early detection of many diseases.
References
Aarts V, Dellimore KH, Wijshoff R, Derkx R, Laar JVD, Muehlsteff J (2017) Performance of An Accelerometer-Based Pulse Presence Detection Approach Compared to A Reference Sensor. Proceedings of the 14th Annual Body Sensor Networks Conference 165–168. https://doi.org/10.1109/BSN.2017.7936033
Ahn J, Ra HK, Yoon HJ, Son SH, Ko J (2020) On-Device Filter Design for Self-Identifying Inaccurate Heart Rate Readings on Wrist-Worn PPG Sensors. IEEE Access 8:184774–184784. https://doi.org/10.1109/ACCESS.2020.3025776
Alicia P (2019) Latest Trends in Medical Monitoring Devices and Wearable Health Technology. Business Insider, India. https://www.businessinsider.com/wearable-technology-healthcare-medical-devices
Allen J (2007) Photoplethysmography and its application in clinical physiological measurement. Physiol Meas 28:R1–R39. https://doi.org/10.1088/0967-3334/28/3/R01
Armagan K, Cigdem E (2011) Perceived Qualities of Smart Wearables: Determinants of User Acceptance. Proceedings of the 2011 Conference on Designing Pleasurable Products and Interfaces 26:1-8. https://doi.org/10.1145/2347504.2347533
Atef M, Wang M, Wang G (2018) A Fully Integrated High-Sensitivity Wide Dynamic Range PPG Sensor with an Integrated Photodiode and an Automatic Dimming Control LED Driver. IEEE Sensors J 18(2):652–659. https://doi.org/10.1109/JSEN.2017.2777740
Boatin AA, Wylie BJ, Goldfarb I, Azevedo R et al (2016) Wireless Vital Sign Monitoring in Pregnant Women: A Functionality and Acceptability Study. Telemed J E Health 22(7):564–571. https://doi.org/10.1089/tmj.2015.0173
Boo HY, Sokwoo R (2000) Development of The Ring Sensor for Healthcare Automation. Robot Auton Syst 30(3):273–281. https://doi.org/10.1016/S0921-8890(99)00092-5
Botilias GP, Pappa L, Karvelis P, Stylios C (2022) Tracking Individuals’ Health Using Mobile Applications and Machine Learning. South-East Europe Design Automation Computer Engineering Computer Networks and Social Media Conference 1-6. https://doi.org/10.1109/SEEDA-CECNSM57760.2022.9932927
Brusco M, Nazeran H (2005) Development of an Iintelligent PDA-Based Wearable Digital Phonocardiograph. Proc. 27th Annual International Conference IEEE EMBS 3506–3509. https://doi.org/10.1109/IEMBS.2005.1617235
Buller MJ, Tharion WJ, Cheuvront SN et al (2013) Estimation of Human Core Temperature from Sequential Heart Rate Observations. Physiol Meas 34(7):781–798. https://doi.org/10.1088/0967-3334/34/7/781
Cho G (2010) Smart clothing: technology and applications. CRC Press Taylor & Francis, Boca Raton
Dan S, Asim S, Thad S (2008) Application Design for Wearable Computing. Morgan & Claypool, San Rafael
Daniel O, Benjamin NW, Taemie K et al (2009) Sensible organizations: Technology and Methodology for Automatically Measuring Organizational Behavior. IEEE Trans Syst, Man, and Cybernetics-Part B: Cybernetics 39(1):43–55. https://doi.org/10.1109/TSMCB.2008.2006638
Darko K, Nuria O, Mike S, Desney T (2007) Health-OS: A Position Paper. Conference: Proceedings of the 1st ACM SIGMOBILE International Workshop on Systems and Networking Support for Healthcare and Assisted Living Environments. https://doi.org/10.1145/1248054.1248077
David LTW, Jufeng Y, Yongfu L, Chacko JD et al (2020) An Integrated Wearable Wireless Vital Signs Biosensor for Continuous Inpatient Monitoring. IEEE Sensors J 20(1):448–462. https://doi.org/10.1109/JSEN.2019.2942099
Dias D, Paulo SCJ (2018) Wearable Health Devices-Vital Sign Monitoring. Systems and Technologies. Sensors (Basel, Switzerland) 18(8):2414. https://doi.org/10.3390/s18082414
Elsherif M, Hassan MU, Yetisen AK, Butt H (2018) Wearable Contact Lens Biosensors for Continuous Glucose Monitoring Using Smartphones. ACS Nano 12(6):5452–5462. https://doi.org/10.1021/acsnano.8b00829
Erika P, Emanuele P, Emanuele R et al (2018) Wearable Heart Rate Monitoring as Stress Response Indicator in Children with Neurodevelopmental Disorder. IEEE Int Symposium Med Measurements Appl 1-5. https://doi.org/10.1109/MeMeA.2018.8438805
Fallow BA, Tarumi T, Tanaka H (2013) Influence of Skin Type and Wavelength on Light Wave Reflectance. J Clin Monit Comput 27(3):313–317. https://doi.org/10.1007/s10877-013-9436-7
Fekr AR, Janidarmian M, Radecka K, Zilic Z (2014) A Medical Cloud-Based Platform for Respiration Rate Measurement and Hierarchical Classification of Breath Disorders. Sensors 4(6):11204–11224. https://doi.org/10.3390/s140611204
Finni T, Hu M, Kettunen P, Vilavuo T, Cheng S (2007) Measurement of EMG Activity with Textile Electrodes Embedded into Clothing. Physiol Meas 28(11):1405–1419. https://doi.org/10.1088/0967-3334/28/11/007
Fletcher RR, Tam S, Omojola O, Redemske R, Kwan J (2011) Wearable Sensor Platform and Mobile Application for Use in Cognitive Behavioral Therapy for Drug Addiction and PTSD. Proceedings International Conferences of the IEEE Engineering in Medicine and Biology Society. (EMBC) 802–1805. https://doi.org/10.1109/IEMBS.2011.6090513
Fu Y, Zhao S, Zhu R (2019) A Wearable Multifunctional Pulse Monitor Using Thermosensation-Based Flexible Sensors. IEEE Trans Biomed Eng 66(5):1412–1421. https://doi.org/10.1109/TBME.2018.2873754
Gaura E, Kemp J, Brusey J (2013) Leveraging Knowledge from Physiological Data: On-Body Heat Stress Risk Prediction with Sensor Networks. IEEE Trans Biomed Circuits Syst 7(6):861–870. https://doi.org/10.1109/TBCAS.2013.2254485
Giovangrandi L, Inan OT, Banerjee D, Kovacs GT (2012) Preliminary Results from BCG and ECG Measurements in the Heart Failure Clinic. Proceedings of the 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society 3780–3783. https://doi.org/10.1109/EMBC.2012.6346790
Gui H, Liu J (2018) Latest Progresses in Developing Wearable Monitoring and Therapy Systems for Managing Chronic Diseases. Med Phys. https://doi.org/10.48550/arXiv.1802.01747
Guk K, Han G, Lim J, Jeong K, Kang T, Lim EK, Jung J (2019) Evolution of Wearable Devices with Real-Time Disease Monitoring for Personalized Healthcare. Nanomaterials 9(6). https://doi.org/10.3390/nano9060813
Haahr RG et al (2012) An Electronic Patch for Wearable Health Monitoring by Reflectance Pulse Oximetry. IEEE Trans Biomed Circuits Syst 6(1):45–53. https://doi.org/10.1109/TBCAS.2011.2164247
Haydar O, Orhan O, Yasemin K et al (2020) A Portable Wearable Tele-ECG Monitoring System. IEEE Trans Instrum Meas 69:173–182. https://doi.org/10.1109/TIM.2019.2895484
Hsu Y, Young DJ (2014) Skin-Coupled Personal Wearable Ambulatory Pulse Wave Velocity Monitoring System Using Microelectromechanical Sensors. IEEE Sensors J 14(10):3490–3497. https://doi.org/10.1109/JSEN.2014.2345779
Jegan R, Anusuya KV (2015) Real-Time ECG Peak Detection for Heart Rate Measurement Using Wavelet Packet Transform. Int J Biomed Eng Technol 19(3):244–254. https://doi.org/10.1504/IJBET.2015.072994
Jegan R, Nimi WS (2018) Sensor Based Smart Real Time Monitoring of Patients Conditions Using Wireless Protocol. Int J E-Health Med Commun (IJEHMC), 21. https://doi.org/10.4018/IJEHMC.2018070105
Jung DW, Hwang SH, Lee YJ, Jeong D, Park KS (2017) Apnea–Hypopnea Index Prediction Using Electrocardiogram Acquired During the Sleep-Onset Period. IEEE Trans Biomed Eng 64(2):295–301. https://doi.org/10.1109/TBME.2016.2554138
Kalantar ZK, Ha N, Ou JZ, Berean KJ (2017) Ingestible Sensors. ACS Sens 2(4):468–483. https://doi.org/10.1021/acssensors.7b00045
Katayama K, Chino S et al (2020) Classification of Pulse Wave Signal Measured by FBG Sensor for Vascular Age and Arteriosclerosis Estimation. IEEE Sensors J 20(5):2485–2491. https://doi.org/10.1109/JSEN.2019.2952833
Kiourti A, Psathas KA, Nikita KS (2013) Implantable and Ingestible Medical Devices with Wireless Telemetry Functionalities: A Review of Current Status and Challenges. Bioelectromagnetics 35(1):1–15. https://doi.org/10.1002/bem.21813
Krehel M, Wolf M, Boesel LF, Rossi RM, Bona GL, Scherer LJ (2014) Development of a Luminous Textile for Reflective Pulse Oximetry Measurements. Biomedical Optics Express 5(8):2537–2547. https://doi.org/10.1364/BOE.5.002537
Kroll RR, Boyd JG, Maslove DM (2016) Accuracy of a Wrist-Worn Wearable Device for Monitoring Heart Rates in Hospital Inpatients: A Prospective Observational Study. J Med Internet Res 18(9):253. https://doi.org/10.2196/jmir.6025
Kwangmuk L, Hee YC, Kyeonghwan P et al (2019) A Multi-Functional Physiological Hybrid-Sensing E-Skin Integrated Interface for Wearable IoT Applications. IEEE Trans Biomed Circuits Syst 13(6):1535–1544. https://doi.org/10.1109/TBCAS.2019.2946875
Lee YK, Jo J, Shin (2013) Development and Evaluation of a Wristwatch-Type Photoplethysmography Array Sensor Module. IEEE Sensors J 13(5):1459–1463. https://doi.org/10.1109/JSEN.2012.2235424
Lee BG, Park JH et al (2016a) Smartwatch-Based Driver Vigilance Indicator with Kernel-Fuzzy-C-Means-Wavelet Method. IEEE Sensors J 16(1):242–253. https://doi.org/10.1109/JSEN.2015.2475638
Lee Y, Lee H, Yoo S, Yoo HJ (2016b) Sticker-Type ECG/PPG Concurrent Monitoring System Hybrid Integration of CMOS Soc And Organic Sensor Device. Proc. IEEE 38th Annu. Int Conf Eng Med Biol Soc 2014–2017. https://doi.org/10.1109/EMBC.2016.7591121
Lin R, Kreifeldt JG (2001) Ergonomics in Wearable Computer Design. Int J Ind Ergon 27(4):259–269. https://doi.org/10.1016/S0169-8141(00)00055-X
Lin CL, Chiu WC, Chen FH et al (2020) Fall Monitoring for the Elderly Using Wearable Inertial Measurement Sensors on Eyeglasses. IEEE Sensors Letters 4(6):1–4. https://doi.org/10.1109/LSENS.2020.2996746
Liu Y, Matt P, Giovanni AS (2017) Lab-On-Skin: A Review of Flexible and Stretchable Electronics for Wearable Health Monitoring. ACS Nano 11(10):9614–9635. https://doi.org/10.1021/acsnano.7b04898
Liu H, Fujita D, Zhang L, Suzuki A (2018) Real-Time Pulse Waveform Profiling Algorithm for Wearable Applications. IEEE Access 6:59296–59306. https://doi.org/10.1109/ACCESS.2018.2875548
Long J, Bin G, Jun G et al (2019) Wearable Long-Term Social Sensing for Mental Wellbeing. IEEE Sensors J 19(19):8532–8542. https://doi.org/10.1109/JSEN.2018.2877427
Malcolm E, Alysia C (2012) Critical care: The Eight Vital Signs of Patient Monitoring. British J Nursing (Mark Allen Publishing) PubMed 21(10):621–625. https://doi.org/10.12968/bjon.2012.21.10.621
Massaroni C et al (2020) Respiratory Monitoring During Physical Activities with a Multi-Sensor Smart Garment and Related Algorithms. IEEE Sensors J 20(4):2173–2180. https://doi.org/10.1109/JSEN.2019.2949608
Massaroni C, Tocco JD et al (2020b) Respiratory Monitoring During Physical Activities with a Multi-Sensor Smart Garment and Related Algorithms. IEEE Sensors J 20(4):2173–2180. https://doi.org/10.1109/JSEN.2019.2949608
Melvin A, Jegan (2017) Performance Measures on Blood Pressure and Heart Rate Measurement from PPG Signal for Biomedical Applications. Proceedings of IEEE International Conference on Innovations in Electrical, Electronics, Instrumentation and Media Technology, 31-35. https://doi.org/10.1109/ICIEEIMT.2017.8116856
Mendelson Y, Dao DK, Chon KH (2013) Multi-Channel Pulse Oximetry for Wearable Physiological Monitoring. IEEE Int Conference Body Sens Networks 1-6. https://doi.org/10.1109/BSN.2013.6575518
Merah M, Abdelmalik TA, Larbi BH (2015) R-Peaks Detection Based on Stationary Wavelet Transform. Comput Methods Prog Biomed 121(3):149–160. https://doi.org/10.1016/j.cmpb.2015.06.003
Miao F, Wang X et al (2019) A Wearable Sensor for Arterial Stiffness Monitoring Based on Machine Learning Algorithms. IEEE Sensors J 19(4):1426–1434. https://doi.org/10.1109/JSEN.2018.2880434
Nayak CS, Anilkumar AC (2021) EEG Normal Waveforms. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK539805/
Nimi WS, Subha HJP, Jegan R (2021) Review on Reliable and Quality Wearable Healthcare Device. Int J Reliable Qual E Healthcare 10(4):1–25. https://doi.org/10.4018/IJRQEH.2021100101
Oura Ring (2017) https://ouraring.com/the-ring/
Peng F, Zhang Z, Gou X et al (2014) Motion Artifact Removal from Photoplethysmographic Signals by Combining Temporally Constrained Independent Component Analysis and Adaptive Filter. Biomed Eng Online 3:50. https://doi.org/10.1186/1475-925X-13-50
Puke S, Suzuki T, Nakayama K, Tanaka H, Minami S (2013) Blood Pressure Estimation from Pulse Wave Velocity Measured on The Chest. Proceedings of the 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Osaka, Japan 6107–6110. https://doi.org/10.1109/EMBC.2013.6610946
Rosenberg WV, Chanwimalueang T et al (2016) Smart Helmet: Wearable Multichannel ECG and EEG. IEEE J Transl Eng Health Med 4:1–11. https://doi.org/10.1109/JTEHM.2016.2609927
Salvo P, Francesco FD et al (2010) A Wearable Sens Measuring Sweat Rate IEEE Sens J 10(10):1557–1558. https://doi.org/10.1109/JSEN.2010.2046634
Sandulescu V, Andrews S, Ellis D, Bellotto N, Mozos OM (2015) Stress Detection Using Wearable Physiological Sensors. International Work-Conference on The Interplay Between Natural and Artificial Computation 526-532. https://doi.org/10.1007/978-3-319-18914-7_55
Sel K, Ibrahim B, Jafari R (2020) ImpediBands: Body Coupled Bio-Impedance Patches for Physiological Sensing Proof of Concept. IEEE Trans Biomed Circuits Syst 14(4):757–774. https://doi.org/10.1109/TBCAS.2020.2995810
Staff DN (2015) 6 Considerations for Designing a Wearable Device. Available: https://www.designnews.com/6-considerations-designing-wearable-device
Svanaes D (2013) Interaction Design for And with The Lived Body: Some Implications of Merleau-Ponty’s Phenomenology. ACM Trans Comput-Hum Interact 20(1):1–30. https://doi.org/10.1145/2442106.2442114
Taiyang W, Fan W, Chunkai Q et al (2020) A Rigid-Flex Wearable Health Monitoring Sensor Patch for IoT-Connected Healthcare Applications. IEEE Internet Things J 7(8):6932–6945. https://doi.org/10.1109/JIOT.2020.2977164
Tamura T, Maeda Y, Sekine M, Yoshida M (2014) Wearable Photoplethysmographic Sensors –Past and Present. Electronics 3(2):282–302. https://doi.org/10.3390/electronics3020282
Tang X, Hu Q, Tang W (2018) A Real-Time QRS Detection System With PR/RT Interval and ST Segment Measurements for Wearable ECG Sensors Using Parallel Delta Modulators. IEEE Trans Biomed Circuits Syst 12(4):751–761. https://doi.org/10.1109/TBCAS.2018.2823275
Teng XF, Zhang YT, Poon CC, Bonato P (2008) Wearable Medical Systems for p-Health. IEEE Rev Biomed Eng 1:62–74. https://doi.org/10.1109/RBME.2008.2008248
Tierney MJ, Tamada JA, Potts RO, Jovanovic L, Garg S (2001) Clinical Evaluation of the GlucoWatch Biographer: A Continual, Non-Invasive Glucose Monitor for Patients with Diabetes. Biosens Bioelectron 16(9–12):621–629. https://doi.org/10.1016/s0956-5663(01)00189-0
Vishal VT, Xiaojun X, Devon B et al (2020) Reliable Breathing Tracking with Wearable Mask Device. IEEE Sensors J 20:5510–5518. https://doi.org/10.1109/jsen.2020.2969635
Volkov MV, Margaryants NB et al (2017) Video Capillaroscopy Clarifies Mechanism of the Photoplethysmographic Waveform Appearance. Sci Rep 7:13298. https://doi.org/10.1038/s41598-017-13552-4
Wilhelm VR, Theerasak C et al (2016) Smart Helmet: Wearable Multichannel ECG and EEG. IEEE J Translational Eng Health Med 4:1–11. https://doi.org/10.1109/JTEHM.2016.2609927
Woo SH, Choi YY, Kim DJ, Bien F, Kim JJ (2014) Tissue-Informative Mechanism for Wearable Non-Invasive Continuous Blood Pressure Monitoring. Sci Rep 4:6618. https://doi.org/10.1038/srep06618
Wu T, Wu F, Qiu C, Redoute JM, Yuce MR (2020) A Rigid-Flex Wearable Health Monitoring Sensor Patch for IoT-Connected Healthcare Applications. IEEE Internet Things J 7(8):6932–6945. https://doi.org/10.1109/JIOT.2020.2977164
Xiaohui G, Ying H, Yunong Z et al (2017) Highly Stretchable Strain Sensor Based on Swcnts/CB Synergistic Conductive Network or Wearable Human-Activity Monitoring and Recognition. Smart Mater Struct 26(9):5017. https://doi.org/10.1088/1361-665X/aa79c3
Yang CC, Hsu YL (2010) A Review of Accelerometry-Based Wearable Motion Detectors for Physical Activity Monitoring. Sensors 10(8):7772–7788. https://doi.org/10.3390/s100807772
Yeong JJ, Soon JK (2019) Wearable Sleepcare Kit: Analysis and Prevention of Sleep Apnea Symptoms in Real-Time. IEEE Access 7:60634–60649. https://doi.org/10.1109/ACCESS.2019.2913849
Yilmaz T, Foster R, Hao Y (2010) Detecting Vital Signs with Wearable Wireless Sensors. Sensors 10:10837–10862. https://doi.org/10.3390/s101210837
Yufa X, Huailing Z, Lin X et al (2018) An Automatic Cardiac Arrhythmia Classification System with Wearable Electrocardiogram. IEEE Access 6:16529–16538. https://doi.org/10.1109/ACCESS.2018.2807700
Zephyr B (2016) http://www.zephyranywhere.com
Zhu W, Chen X, Wang Y, Wang (2019) Arrhythmia Recognition and Classification Using ECG Morphology and Segment Feature Analysis. IEEE/ACM Trans Comput Biol Bioinform 16(1):131-138. https://doi.org/10.1109/TCBB.2018.2846611
Acknowledgements
The authors would like to thank the Department of Science and Technology for funding support and the management of the Karunya Institute of Technology and Sciences for providing the resources to complete this work.
Funding
The continuation of this research work is funded by the Department of Science and Technology under the file number of SP/YO/2021/2518.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no potential conflicts of interest.
Ethical approval and informed consent
The authors confirm that this study did not involve human, animal subjects or tissue.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jegan, R., Nimi, W.S. On the development of low power wearable devices for assessment of physiological vital parameters: a systematic review. J Public Health (Berl.) 32, 1093–1108 (2024). https://doi.org/10.1007/s10389-023-01893-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-023-01893-6