Abstract
Aims
We sought to gather experts’ perspectives on Medicaid coverage gaps during reentry to identify high-yield policy solutions to improve the health of justice-involved individuals in the United States.
Subject and methods
We interviewed 28 experts at the intersection of Medicaid and criminal justice via telephone between November 2018 and April 2019. Interviewees included Medicaid administrators, health and justice officials, policy makers, and health policy researchers. We performed thematic analysis of semi-structured interview transcripts to identify emergent themes and distill policy recommendations.
Results
Three themes emerged: 1) Medicaid coverage gaps during reentry contribute to poor health outcomes and recidivism, 2) excessive burden on justice-involved people to re-activate Medicaid leads to coverage gaps, and 3) scalable policy solutions exist to eliminate Medicaid coverage gaps during reentry. Policy recommendations centered on ending the federal “inmate exclusion,” delaying Medicaid de-activation at intake, and promoting re-activation by reentry. Experts viewed coverage gaps as problematic, viewed current approaches as inefficient and burdensome, and recommended several policy solutions.
Conclusion
By pursuing strategies to eliminate Medicaid gaps during reentry, policymakers can improve health outcomes and efficiency of government spending on healthcare, and may reduce cycles of incarceration.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
With over 2.2 million adults and 45,000 youth involuntarily detained on any given day in correctional facilities in the United States (USA), the incarcerated population is sizable and faces significant health inequities (Kaeble and Cowhig 2016; Sickmund et al. 2019; Binswanger et al. 2009; Braverman and Morris 2011; Bronson and Berzofsky 2017). Compared to the general US adult population, incarcerated adults are 20% more likely to have hypertension, 30% more likely to have asthma, 25% more likely to have cervical cancer, and have an excess risk of serious infections, including HIV/AIDS, tuberculosis, and hepatitis B and C (Binswanger et al. 2009; National Commission on Correctional Health Care 2002). The majority of incarcerated adults meet diagnostic criteria for a substance use disorder and many have mental health disorders; the rate of “serious psychological distress” is four-fold higher than the general adult population (Bronson and Berzofsky 2017). Similarly, 70% of US detained adolescents meet diagnostic criteria for at least one psychiatric disorder, and rates of sexually transmitted infections, pregnancy, and teen parenting far exceed those of the general adolescent population (Braverman and Morris 2011; Teplin et al. 2002). For example, 15% of detained adolescent boys and 9% of detained adolescents girls in the USA are teen parents, compared to 2% and 6% of adolescent boys and girls, respectively, in the general US adolescent population (Sedlak and Carol 2010).
Given the health vulnerability and high stakes during transitions to home after incarceration, access to healthcare during reentry is critical. During reentry, people must re-connect with their families while re-integrating into housing, healthcare, and employment or school, all while meeting court requirements that may include attending behavioral health appointments (Altschuler and Brash 2004; Freudenberg et al. 2005). Formerly incarcerated adults have 12.7 times the risk of mortality within the first 2 weeks after release compared to matched peers (Binswanger et al. 2007). Self-reported general health deteriorates in the year following release, and rates of hospitalizations and emergency room visits far exceed those for individuals without recent incarceration histories (Frank et al. 2014; Mallik-Kane and Visher 2005). One study of a representative sample of 1100 US adults undergoing reentry found that 70% of individuals with medical or mental health diagnoses utilized health care within the first 9 months after release, with one-third presenting to emergency rooms and one-fifth requiring hospitalization (Mallik-Kane and Visher 2005).
Medicaid can provide an important source of health insurance coverage in the USA for individuals undergoing reentry, as many are low-income and qualify for Medicaid (Albertson et al. 2020). Established in 1965, Medicaid is a public health insurance program that provides care for approximately 100 million low-income Americans. By federal mandate, Medicaid covers hospital and physician care, diagnostic services, home health, nursing care services, and prescription drug coverage. In many US states, Medicaid additionally covers dental, vision, and hearing services, as well as personal care services for individuals with disabilities (Center on Budget and Policy Priorities 2020). In states that expanded Medicaid under the Affordable Care Act, most adults with a recent history of justice system involvement are eligible for Medicaid coverage at release, and at least two-thirds of detained youth in the justice system are estimated to be eligible (Albertson et al. 2020).
However, federal law, through the Medicaid Inmate Exclusion Policy, disrupts Medicaid insurance coverage for justice-involved individuals rather than promoting it (Acoca et al. 2014; Gates et al. 2014). Although access to healthcare during incarceration is a constitutional mandate, the “inmate exclusion” prohibits federal Medicaid dollars from funding healthcare for individuals detained or incarcerated in the correctional system, except for inpatient care lasting 24 h or more (US Congress 1965). To comply with the inmate exclusion, jurisdictions typically suspend or terminate Medicaid upon intake in correctional facilities (Fiscella et al. 2017). The correctional facility—be it juvenile hall for adolescents, or county jail or state or federal prison for older adolescents and adults—is then responsible for funding care in detention settings, regardless of whether a person entered the facility with Medicaid, private insurance, or no health insurance. The delivery of correctional care may be contracted to private entities or provided by the government, such as by a county health agency delivering care in a county juvenile detention facility or adult jail (Acoca et al. 2014). While mechanisms to de-activate Medicaid coverage seem to function effectively, many facilities do not prioritize re-activation upon release. As a result, formerly incarcerated adults and youth enrolled in Medicaid at intake may return to the community without Medicaid insurance coverage (Albertson et al. 2020).
Data on the prevalence of Medicaid gaps during reentry are sparse, but suggest the problem is significant (Albertson et al. 2020). Lack of health insurance has been cited as a major barrier to care during reentry (Golzari and Kuo 2013). National data indicate that adults with a recent history of justice involvement are uninsured at twice the rate of those without justice involvement (Winkelman et al. 2016). Furthermore, coverage gaps during reentry are associated with worse health outcomes (Fu et al. 2013; Louden 2011; Winkelman et al. 2016). Lack of health insurance among adults with HIV during the month after release from jail has been associated with recidivism and shorter time to re-incarceration (Fu et al. 2013). Lack of insurance also correlates with lower utilization rates of behavioral health treatment among justice-involved individuals (Winkelman et al. 2016); in turn, untreated mental illness has been associated with recidivism (Louden 2011). Eliminating gaps in Medicaid coverage during reentry can promote access to evidence-based healthcare interventions, and may improve health during reentry.
Currently, wide variation in Medicaid de-activation and re-activation practices by Medicaid agencies and correctional systems exist across jurisdictions in the USA (Evans Cuellar et al. 2005). Isolated descriptions of promising practices for minimizing disruptions in Medicaid coverage at reentry exist, but are limited to single-site program descriptions, mostly available in white papers (Albertson et al. 2020). One study inventoried the strategies of 64 programs that enroll justice-involved individuals in Medicaid, highlighting practice approaches, but did not include the perspectives of providers or policy experts (Bandara et al. 2015). The peer-reviewed literature lacks comprehensive recommendations for eliminating gaps in Medicaid coverage during reentry. Solutions that cross jurisdictions, age groups, and correctional settings (e.g., juvenile hall, jail, prison) may exist but have yet to be clarified. We therefore sought to gather experts’ perspectives to identify policy solutions for reducing gaps in Medicaid coverage during reentry.
Methods
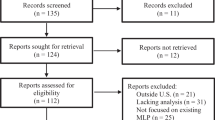
We conducted semi-structured interviews, via telephone, between November 2018 and April 2019 with clinical and policy experts across the USA at the intersection of criminal justice and Medicaid to identify challenges and solutions related to eliminating gaps in Medicaid coverage during reentry. We identified potential informants by generating a list of known experts, based on literature review and contacts from prior studies (Hoffman et al. 1995). We then expanded the sample using snowball sampling. Informants included state and federal Medicaid administrators; adult and juvenile corrections officials, including reentry care coordinators; correctional and community health providers; policymakers; justice advocacy groups; and health policy researchers. We purposively sampled (Palinkas et al. 2015) to gather expertise that included federal, state, and county-level perspectives; this spanned adult and youth corrections, and included representatives from the professional stakeholders groups perceived as key to understanding the problem, and potential solutions. Invitees represented a diversity of geographic regions. Because we sought people who viewed themselves as experts about Medicaid and reentry, participants tended to have several years of experience in the field of criminal justice. Some participants were state or national policy leaders while others were on-the-ground practitioners; our focus was to gather views from the different types of professionals with perspectives central to solving coverage gaps in Medicaid during reentry. Of the 44 individuals invited via email, 28 participated in the study (64%).
The semi-structured interview guide (see Appendix: 'Semi-structured interview guide') explored contributors to gaps in Medicaid coverage during reentry, and included a list of proposed solutions, gathered through literature review. Participants were asked to discuss perceived impact and feasibility of proposed solutions, and to suggest any additional solutions. With interviewee permission, we audio-recorded the interviews, which were then transcribed by a professional transcription service.
We performed in-depth thematic analysis of the interview transcripts to identify emergent themes about Medicaid coverage gaps, applying the six-step procedure enumerated by Braun and Clarke (2006). We first open-coded several transcripts to familiarize ourselves with the data. Through weekly team meetings, we generated initial codes, created a codebook, and applied the codes to the transcripts using Dedoose software 1.3.34 (SCRC, Manhattan Beach, CA). Each interview was coded by two team members and reviewed by a third coder. We collated codes into themes based on recurring ideas, and then defined and named the themes. We continued interviews until we reached and surpassed saturation of major themes, defined as hearing the same ideas repeated and not hearing new ideas (Hoffman et al. 1995). Although the initial study objective focused on youth in the juvenile justice system (published separately, forthcoming), the sampling and coding resulted in findings relevant to justice-involved adults, which generated adequate information for this analysis. To assess the validity of our findings, we performed member checking and debriefed findings with a physician–scientist and an attorney with relevant expertise who were external to the study team. The University of California, Los Angeles institutional review board approved all study procedures.
Results
Three themes emerged: 1) Medicaid coverage gaps during reentry contribute to poor health outcomes and recidivism, 2) excessive burden on justice-involved people to re-activate Medicaid after incarceration leads to coverage gaps, and 3) scalable policy solutions exist to eliminate Medicaid coverage gaps during reentry. Table 1 provides representative quotes for each theme.
Theme 1: Medicaid coverage gaps during reentry contribute to poor health outcomes and recidivism
Participants emphasized the justice-involved population’s reliance on Medicaid, and viewed Medicaid coverage gaps during reentry as a public health concern. Gaps in coverage during reentry were viewed as a cause of missed health appointments and medication non-adherence, which exacerbated health conditions. Interviewees also expressed that Medicaid coverage gaps contribute to recidivism, particularly when coverage gaps impeded access to behavioral health treatments that reduce risky behavior. In instances when Medicaid coverage was successfully restored, participants conveyed that recently incarcerated individuals can receive community health services rather than returning to detention as a means to receive care.
Participants were unable to quantify how many individuals in their jurisdictions faced coverage gaps; however, all the participants stated that coverage gaps existed and were problematic. Many participants lacked clarity regarding the details of de-activation and re-activation processes, but conveyed a wide variation in Medicaid de-activation and re-activation practices. One participant stated that her correctional facility detained individuals for several weeks before Medicaid becomes de-activated, whereas other participants described Medicaid de-activation occurring shortly after arrest.
Theme 2: Excessive burden on justice-involved people to re-activate Medicaid after incarceration leads to coverage gaps
Interviewees expressed that Medicaid de-activation during incarceration and the subsequent need to re-activate Medicaid creates a burden on Medicaid, correctional agencies, and health systems. However, more concerning to participants was the burden placed on justice-involved individuals and their families with regard to Medicaid re-activation. Interviewees provided two main justifications for ending de-activation and removing barriers to Medicaid re-activation: the current system is unfair and is also inefficient.
Participants expressed that it seemed unjust to require justice-involved individuals to re-activate Medicaid, as many entered the system with Medicaid in place. Participants explained that the burden placed on individuals exiting the justice system—or on parents, in instances of youth incarceration—was high, which was concerning giving the challenging context of reentry. Participants described justice-involved people as “marginalized” and “oppressed” by a system that seems “set up” to make justice-involved individuals “fail.”
Additionally, participants stated that placing re-activation requirements on justice-involved individuals created inefficiencies. Participants described the waste of time, money, and personnel when Medicaid becomes de-activated, which necessitates re-activation. Most described Medicaid re-activation processes as “slow,” sometimes taking weeks to months. Participants also described current Medicaid re-activation procedures as "confusing," "complicated," "labor intense," and "difficult," including requiring information that may be difficult to obtain (e.g., address, if experiencing homelessness). Participants explained that when Medicaid-eligible individuals leave incarceration without Medicaid, families struggle to re-activate Medicaid coverage. Participants expressed that many justice-involved individuals struggle to meet basic needs, and face mental health disorders that make carrying-out Medicaid re-activation more challenging. One participant stated, “The re-enrollment process for Medicaid is very challenging for adults, nonetheless if they have a mental illness, they’re disabled. They really need help on this area.” Interviewees explained that for justice-involved individuals to thrive in the community, providing more “hand-holding” to assist with Medicaid re-activation is worthwhile and potentially cost-saving. Participants felt that shifting the burden of re-activation away from justice-involved families could decrease coverage gaps, which could prove more efficient for correctional, Medicaid, and healthcare agencies, in addition to benefiting justice-involved individuals.
Theme 3: Scalable policy solutions exist to eliminate Medicaid coverage gaps during reentry
Interviewees viewed policy solutions to reduce gaps in Medicaid coverage during reentry as “key to our society’s safety.” In addition to federal, state, and county legislative solutions, participants suggested reforming Medicaid agency and correctional system policies. Ending the federal inmate exclusion was viewed as the “obvious” and highest impact solution, as it would eliminate the policy that requires de-activation at intake. However, most felt ending the inmate exclusion was infeasible due to lack of political will. As a workaround to ending the inmate exclusion, participants recommended specific policy approaches that delay de-activation or promote re-activation. The policy solutions (Table 2) sorted into five categories: 1) reform the Medicaid “off switch,” 2) facilitate re-activation of Medicaid (“on switch”), 3) increase Medicaid-justice system collaboration, 4) collect data on Medicaid coverage gaps, and 5) ensure effective implementation of existing laws to reduce Medicaid coverage gaps during reentry.
Policy recommendation 1: reform the Medicaid “off switch”
The recommendation to reform the Medicaid “off switch” referred to policies impacting the de-activation of Medicaid for individuals held in correctional facilities. In addition to changing federal law to end the inmate exclusion, interviewees suggested strategies for improving de-activation policies. First, interviewees agreed that Medicaid should not be terminated. Instead, participants recommended Medicaid suspension policies as preferable because re-instating Medicaid is easier and faster than re-enrollment after termination. As one interviewee stated, “Suspension allows you to just turn the button back on without going through the whole re-enrollment process.” Interviewees also recommended ending time-limited suspension, the practice of automatically terminating Medicaid after a specified duration of incarceration, often 1 year. Interviewees additionally recommended adopting delayed suspension, which referred to delaying Medicaid de-activation until a specified minimum number of days or until after adjudication. Under delayed suspension, for any time period under the suggested minimum (e.g., less than 4 weeks), an individual’s Medicaid would remain active; however, the correctional system rather than Medicaid would cover the costs of healthcare delivered in correctional facilities. Finally, one interviewee suggested not de-activating Medicaid at all. The participant recommended amending state law to specify that jurisdictions may suspend Medicaid, but need not do so. This state policy recommendation was made to align with the federal Substance Use–Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities (SUPPORT) Act of 2018 (US Congress 2019), which prohibits states from terminating Medicaid benefits for juveniles at intake and, instead of termination, specifies that states “may suspend” Medicaid, but are not obligated to do so.
Policy recommendation 2: facilitate re-activation of Medicaid (“on switch”)
The second category of policy recommendations included policies that facilitate re-activation of Medicaid (i.e., “on switch”), either before release or during reentry. Participants viewed providing care coordination that includes assistance with Medicaid activation as “absolutely critical” for supporting individuals preparing for community reentry. Participants stated that having staff dedicated to overseeing re-activation procedures could resolve the current lack of organizational responsibility for Medicaid re-activation that results from the issue transecting justice, social services, and health systems. Medicaid re-activation was viewed as a task ideally completed before release; however, unanticipated release dates were a barrier to accomplishing this. A physician in an adult jail commented, “We don’t realize they’ve left until a few days later.” Policies that fund or otherwise promote Medicaid re-activation assistance programs were viewed as highly impactful and necessary.
Interviewees also recommended that lawmakers and agencies pursue policies that encourage presumptive eligibility, meaning that individuals exiting incarceration who meet set criteria (e.g., low income) are presumed eligible for Medicaid for a given time period, often 30 days, until Medicaid eligibility is confirmed. Participants explained that because many recently incarcerated individuals are eligible for Medicaid, presumptive eligibility is worthwhile as it could prevent people from “falling through the cracks.” Presumptive eligibility would allow individuals with Medicaid coverage gaps to immediately access care and medications during the first few weeks after release, which participants described as an especially vulnerable period.
Policy recommendation 3: increase Medicaid–justice system collaboration
Participants perceived agency “silos” between Medicaid, corrections, and health systems as contributing to Medicaid coverage gaps during reentry. Participants felt that challenges of sharing electronic data across Medicaid and correctional systems created a barrier to ensuring Medicaid coverage is in place at release. Integrated data systems were recommended to “automate” re-activation processes. Participants viewed lack of personal connections between Medicaid and correctional staff members as slowing progress in reducing gaps in Medicaid coverage. To overcome agency silos, participants recommended establishing task forces focused on eliminating Medicaid coverage gaps during reentry, with an emphasis on promoting collaboration and improving data sharing across Medicaid and correctional systems. The recommendation that lawmakers mandate Medicaid and corrections agencies to collaborate to ease coverage re-activation and reduce Medicaid coverage gaps also emerged.
Policy recommendation 4: encourage data collection on Medicaid coverage gaps
Across the interviews, participants expressed a lack of data that measures the scope of the issue of disruption in Medicaid coverage gaps during reentry. Participants felt data were needed to understand the issue scope as well as progress in achieving improvement. Policies that incentivize and fund data collection to measure Medicaid coverage gaps were viewed as worthwhile.
Policy recommendation 5: ensure effective implementation of existing laws to reduce Medicaid coverage gaps during reentry
Interviewees expressed that lawmakers and practitioners should ensure effective implementation of existing protections to reduce Medicaid coverage gaps during reentry. In particular, juvenile justice experts recommended that federal and state lawmakers effectively implement relevant statutes in the federal SUPPORT for Patients and Communities Act (US Congress 2019), which prohibits terminating Medicaid benefits for juveniles at intake and requires that state governments take responsibility for re-activation of Medicaid following incarceration, should it be suspended. Interviewees noted that the statute, which went into effect October 2019, lacks an accountability and enforcement mechanism. Interviewees reported that while the legislation has the potential to reduce coverage gaps, implementation is unclear. Participants recommended adding enforcement mechanisms to the SUPPORT Act and to existing state statutes that promote Medicaid re-activation by release.
Discussion
The clinical and policy experts considered Medicaid coverage gaps during reentry a significant public health concern in the USA. While participants generally supported terminating the federal inmate exclusion, which disallows federal Medicaid dollars to fund correctional care for “inmates” (US Congress 1965), most felt that reversing the inmate exclusion was not politically feasible. The findings from the interviews suggest that current responses to the inmate exclusion established in 1965 (US Congress 1965) are anachronistic in today’s age of health information technology—de-activating Medicaid coverage during incarceration should no longer be needed to prevent “double billing” of Medicaid for inmates of a public institution. Nevertheless, as alternatives, interviewees offered creative, pragmatic policy solutions that would minimize Medicaid gaps during reentry. By promoting access to preventive care and ongoing treatment during reentry, adopting these policies can re-direct government spending towards health promotion rather than high-cost healthcare crises and corrections (Albertson et al. 2020). If implemented, these approaches may also alleviate administrative burden and hidden costs on Medicaid, corrections, and health agencies (Bandara et al. 2015; Bechelli et al. 2014). Additionally, reforming the Medicaid “off” or “on” switch could lessen the burden on justice-involved individuals and their families, thereby increasing their chance of success, reducing systems-level inefficiencies, and promoting fairness. In alignment with existing literature (Bandara et al. 2015; Patel et al. 2014), the clinical and Medicaid policy experts we interviewed believed that by promoting continuous Medicaid coverage at reentry, such changes could improve health outcomes and reduce recidivism for the vulnerable population of people re-entering their communities after incarceration (Bandara et al. 2015; Patel et al. 2014).
Implications
Currently most states suspend, rather than terminate Medicaid upon incarceration (Social Security Adminstration 2019). Findings suggest that states that have transitioned from suspension to termination policies, such as California, have had success in reducing Medicaid coverage gaps during reentry (Bandara et al. 2015; Boutwell and Freedman 2014; Golzari et al. 2008). The federal SUPPORT Act is a noteworthy reform for youth in the justice system because states will no longer be able to terminate Medicaid (US Congress 2019). However, even states like California with existing suspension policies and statutes that require state agencies to complete re-instatement processes, experience issues with coverage gaps (Albertson et al. 2020). Thus, unless the inmate exclusion is eliminated, policy reform must be multi-faceted. Findings suggest that state mandates, such as prohibiting Medicaid termination, are vital, but need to be coupled with programs that facilitate re-activation. Alternately, states can reform the Medicaid “off switch” by disallowing termination and possibly suspension. The current exclusion under the inmate exclusion can be maintained, yet Medicaid would not be de-activated. Doing so would not alter the amount of federal Medicaid dollars providing payment for the care of “inmates,” but would eliminate Medicaid coverage gaps during reentry that result from Medicaid de-activation policies. Instead of carrying out de-activation followed by re-activation, states and local agencies could focus on enrolling detained individuals eligible who were not enrolled upon intake. In this way, incarceration could function as a positive determinant of health, rather than one that currently obstructs basic access to care by creating gaps in coverage during reentry (Albertson et al. 2020). A barrier to not suspending Medicaid may be the monthly fee paid to Medicaid managed care programs if suspension is not carried out; however, if alternate Medicaid reimbursement models are pursued in the future, not suspending Medicaid may become more appealing.
Data on coverage gaps are sparse, as demonstrated in our literature review and in the interviews with experts, yet it is clear that coverage gaps exist and that they create problems. Given the views of our experts and the large size of the justice-involved population—6.7 million individuals were under correctional supervision in 2015 (US Bureau of Justice Statistics 2016)—the problem is likely to be significant. Collecting data on coverage gaps is an important aspect of understanding the scope of the issue and measuring progress. Policymakers should be aware that funding is needed to support such efforts.
Our study approach raises potential limitations. Although our snowball sampling approach broadened our sample to include stakeholders from the criminal justice system, our initial sampling and interview guide focused on the juvenile justice system. Additionally, selection bias may have been an issue. Lack of generalizability is also a concern as differences between jurisdictions and between youth versus adults exist. To mitigate this limitation, we focused the analysis to identify findings generalizable across settings. Participants discussed related issues during the interviews (e.g., expanding Medicaid eligibility, increasing access to quality providers who accept Medicaid) that were beyond the scope of this analysis. Despite these limitations, clear policy recommendations emerged that can improve population health by reducing gaps in Medicaid coverage during reentry.
Conclusion
Gaps in Medicaid coverage during reentry are a public health concern, and the inmate exclusion in US law is at the root of the problem. If efforts to end the inmate exclusion are ineffective or deemed politically infeasible, alternate policy solutions may reduce gaps in Medicaid coverage during reentry. Potential cost-savings, reduction of administrative burden, improved health outcomes, and lower rates of recidivism can motivate lawmakers and practitioners to decrease Medicaid coverage gaps for the millions of Medicaid-eligible men, women, and adolescents each year re-entering their communities after incarceration.
References
Acoca L, Stephens J, Van Vleet A (2014) Health coverage and care for youth in the juvenile justice system: the role of Medicaid and CHIP. Kaiser Family Foundation, Washington DC
Albertson EM, Scannell C, Ashtari N, Barnert E (2020) Eliminating gaps in Medicaid coverage during reentry after incarceration. Am J Public Health 110:317–321. https://doi.org/10.2105/AJPH.2019.305400
Altschuler DM, Brash R (2004) Adolescent and teenage offenders confronting the challenges and opportunities of reentry. Youth Violence Juvenile Justice 2:72–87. https://doi.org/10.2105/AJPH.2019.305400
Bandara SN, Huskamp HA, Riedel LE, McGinty EE, Webster D, Toone RE, Barry CL (2015) Leveraging the Affordable Care Act to enroll justice-involved populations in Medicaid: state and local efforts. Health Aff (Millwood) 34:2044–2051. https://doi.org/10.1377/hlthaff.2015.0668
Bechelli MJ, Caudy M, Gardner TM, Huber A, Mancuso D, Samuels P, Shah T, Venters HD (2014) Case studies from three states: breaking down silos between health care and criminal justice. Health Aff (Millwood) 33:474–481. https://doi.org/10.1377/hlthaff.2013.1190
Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, Koepsell TD (2007) Release from prison—a high risk of death for former inmates. N Engl J Med 356:157–165. https://doi.org/10.1056/NEJMsa064115
Binswanger IA, Krueger PM, Steiner JF (2009) Prevalence of chronic medical conditions among jail and prison inmates in the USA compared with the general population. J Epidemiol Community Health 63:912–919. https://doi.org/10.1136/jech.2009.090662
Boutwell AE, Freedman J (2014) Coverage expansion and the criminal justice-involved population: implications for plans and service connectivity. Health Aff (Millwood) 33:482–486. https://doi.org/10.1377/hlthaff.2013.1131
Braun V, Clarke C (2006) Using thematic analysis in psychology. Qual Res Psychol 3:77–101. https://doi.org/10.1191/1478088706qp063oa
Braverman P, Morris R (2011) The health of youth in the juvenile justice system. In: Sherman F, Jacobs F (eds) Juvenile justice — advancing research, policy, and practice. Wiley, Hoboken, pp 44–67
Bronson J, Berzofsky M (2017) Indicators of mental health problems reported by prisoners and jail inmates, 2011–2012. US Department of Justice. Bureau of Justice Statistics, Washington DC
Center on Budget and Policy Priorities (2020) Policy basics: introduction to Medicaid. Center on Budget and Policy Priorities, Washington DC. https://www.cbpp.org/research/health/policy-basics-introduction-to-medicaid. Accessed 25 September 2020
Evans Cuellar A, Kelleher KJ, Rolls JA, Pajer K (2005) Medicaid insurance policy for youths involved in the criminal justice system. Am J Public Health 95:1707–1711. https://doi.org/10.2105/AJPH.2004.056259
Fiscella K, Beletsky L, Wakeman SE (2017) The inmate exception and reform of correctional health care. Am J Public Health 107:384–385. https://doi.org/10.2105/AJPH.2016.303626
Frank JW, Linder JA, Becker WC, Fiellin DA, Wang EA (2014) Increased hospital and emergency department utilization by individuals with recent criminal justice involvement: results of a national survey. J Gen Intern Med 29:1226–1233. https://doi.org/10.1007/s11606-014-2877-y
Freudenberg N, Daniels J, Crum M, Perkins T, Richie BE (2005) Coming home from jail: the social and health consequences of community reentry for women, male adolescents, and their families and communities. Am J Public Health 98:S191–S202. https://doi.org/10.2105/AJPH.2004.056325
Fu JJ, Herme M, Wickersham JA, Zelenev A, Althoff A, Zaller ND, Bazazi AR, Avery AK, Porterfield J, Jordan AO, Simon-Levine D, Lyman M, Altice FL (2013) Understanding the revolving door: individual and structural-level predictors of recidivism among individuals with HIV leaving jail. AIDS Behav 17:145–155. https://doi.org/10.1007/s10461-013-0590-1
Gates A, Artiga S, Rudowitz R (2014) Health coverage and care for the adult criminal justice-involved population. Kaiser Family Foundation, San Francisco, CA
Golzari M, Kuo A (2013) Healthcare utilization and barriers for youth post-detention. Int J Adolesc Med Health 25:65–67. https://doi.org/10.1515/ijamh-2013-0008
Golzari M, Hunt SJ, Chamberlain LJ (2008) Role of pediatricians as advocates for incarcerated youth. Pediatrics 121:e397–e398. https://doi.org/10.1542/peds.2007-0780
Hoffman RR, Shadbolt NR, Burton AM, Klein G (1995) Eliciting knowledge from experts: a methodological analysis. Organ Behav Hum Dec 62:129–158. https://doi.org/10.1006/obhd.1995.1039
Kaeble D, Cowhig M (2016) Correctional populations in the United States, 2016. US Department of Justice. https://www.bjs.gov/content/pub/pdf/cpus16.pdf. Accessed 9 October 2019
Louden J (2011) Parolees with mental disorder: toward evidence-based practice. University of California Irvine, Irvine, CA
Mallik-Kane K, Visher C (2005) Health and prisoner reentry: how physical, mental, and substance abuse conditions shape the process of reintegration. The Urban Institute Justice Policy Center, Washington DC
National Commission on Correctional Health Care (2002) The health status of soon-to-be-released inmates. National Commission on Correctional Health Care, Chicago, IL
Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K (2015) Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Hlth 42:533–544. https://doi.org/10.1007/s10488-013-0528-y
Patel K, Boutwell A, Brockmann BW, Rich JD (2014) Integrating correctional and community health care for formerly incarcerated people who are eligible for Medicaid. Health Aff (Millwood) 33:468–473. https://doi.org/10.1377/hlthaff.2013.1164\
Sedlak A, Carol B (2010) Youth's characteristics and backgrounds: Findings from the survey of youth in residential placement. Office of Juvenile Justice and Delinquency Prevention, Washington DC. https://www.ncjrs.gov/pdffiles1/ojjdp/227730.pdf. Accessed 25 September 2020
Sickmund M, Sladky T, Kang W, Puzzanchera C (2019) Easy access to juvenile court statistics: 1997–2017. Office of Juvenile Justice and Delinquency Prevention, Washington DC. https://www.ojjdp.gov/ojstatbb/ezajcs/Accessed 7 June 2019
Social Security Adminstration (2019) Compilation of the Social Security Laws. Social Security Adminstration, Baltimore, MD. https://www.ssa.gov/OP_Home/ssact/ssact.htm. Accessed 11 October 2019
Teplin LA, Abram KM, McClelland GM, Dulcan MK, Mericle AA (2002) Psychiatric disorders in youth in juvenile detention. Arch Gen Psychiatry 59:1133–1143. https://doi.org/10.1001/archpsyc.59.12.1133
US Bureau of Justice Statistics (2016) U.S. correctional population at lowest level since 2002. US Bureau of Justice Statistics, Washington DC
US Congress (1965) Social Security Act Amendments of 1965. US Congress, Washington DC. https://www.ourdocuments.gov/doc.php?flash=false&doc=99#. Accessed 1 March 2020
US Congress (2019) SUPPORT for Patients and Communities Act. US Congress, Washington DC, https://www.congress.gov/bill/115th-congress/house-bill/6/Accessed 1 March 2020
Winkelman TN, Kieffer EC, Goold SD, Morenoff JD, Cross K, Ayanian JZ (2016) Health insurance trends and access to behavioral healthcare among justice-involved individuals-United States, 2008–2014. J Gen Intern Med 31:1523–1529. https://doi.org/10.1007/s11606-016-3845-5
Funding
Dr. Barnert’s effort was funded by the NIH National Institute on Drug Abuse (K23DA01757) and by the UCLA Children’s Discovery and Innovation Institute. Dr. Scannell is supported by the National Clinician Scholars Program at the University of California, Los Angeles, and by the VA Office of Academic Affiliations through the VA/National Clinician Scholars Program. The contents do not represent the views of the US National Institutes of Health, or the Department of Veterans Affairs, or the US Government.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Our university’s institutional review board approved the study protocol.
Informed consent
Study participants provided verbal informed consent.
Conflict of interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Semi-structured interview guide
Semi-structured interview guide
Greetings, thank you for taking the time to speak with me today. As I mentioned in my email invitation, researchers from UCLA are conducting a research study to identify policy solutions to eliminate gaps in Medicaid when youth are exiting juvenile detention facilities.
I will now read you a consent script, at the end, can you please answer yes or no if you are willing to participate? This consent will be recorded along with the interview (read script).
-
1.
Would you please tell me a bit about your current occupation?
-
a.
What are your additional experiences relevant to Medicaid and/or juvenile justice?
-
a.
-
2.
Please tell me about how Medicaid re-enrollment is handled in your county/state
-
a.
What are problems you see with how Medicaid re-enrollment is handled?
-
b.
What is working well with how Medicaid re-enrollment is handled?
-
c.
To what extent do you see reducing gaps in Medicaid coverage as a priority?
-
d.
What happens with CHIP (if different)?
-
a.
-
3.
What do you think of the following proposed solutions (feasibility [cost, infrastructure, legal barriers]/ logistics/ policy window/ unintended consequences/ priority/ level):
-
a.
Medicaid off switch:
-
a)
End inmate exclusion
-
b)
Suspension only (federal, state, or CHIP suspension for California)
-
c)
Continuous eligibility
-
d)
Wait longer to turn off
-
a)
-
b.
Pre-release:
-
a)
Assist re-enroll prior to release
-
b)
Make re-enrollment pre-release easier
-
c)
Leave with Medicaid card
-
d)
Reduced sentences for completing Medicaid application
-
e)
Care coordination and health navigation education
-
a)
-
c.
Post-release:
-
a)
Prescription for covered medication or medication supply at release
-
b)
Assist families with re-enrollment post-release (or new enrollment)
-
c)
Presumptive eligibility (one month)
-
d)
Faster reinstatement [faster eligibility determination, short form application]
-
e)
Acceptance of alternate forms of ID for Medicaid re-enrollment
-
f)
Care coordination post-release
-
a)
-
d.
Other:
-
a)
Integrative data system/ computerized re-activation
-
b)
State task force
-
c)
Other suggestions
-
a)
-
a.
-
4.
Focusing on state level solutions:
-
a.
Which of these solutions can be best addressed through state legislation?
-
b.
What state legislative policy solution would you prioritize for California?
-
c.
To what extent are solutions the same across states?
-
d.
Are there other legislative priorities regarding Medicaid or CHIP coverage for youth post-incarceration? [federal, other states, county]
-
a.
-
5.
Any other thoughts?
-
6.
Are there any other resources you suggest?
-
7.
Who do you recommend we speak to next from (POSITION or PLACE)?
-
8.
Is it okay if we contact you again if we have questions?
Thank you!
Rights and permissions
About this article
Cite this article
Barnert, E.S., Scannell, C., Ashtari, N. et al. Policy solutions to end gaps in Medicaid coverage during reentry after incarceration in the United States: experts’ recommendations. J Public Health (Berl.) 30, 2201–2209 (2022). https://doi.org/10.1007/s10389-021-01483-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-021-01483-4