Abstract
Objectives
With the rapid development and spread of information technology, mobile healthcare (M-healthcare) is emerging as a feasible option for improved monitoring and treatment of patients with chronic diseases such as diabetes, particularly for those with limited access to medical institutions. Our study group has developed and evaluated an M-healthcare system that provides remote guidance for diabetic patients. This paper introduces the diabetic M-healthcare system and describes progress in implementation for remote and mobile healthcare in China. We provide evidence that this system improves diabetic patient management and can contribute to the establishment of a new model for patient-centered mobile healthcare.
Target audience
The main groups that this paper is aimed at are doctors, nurses, nutritionists, and sportspersons engaged in the design of mobile medical systems, and computer engineers involved in the construction of intelligent medical software systems.
Scope
The present article has as its scope designing the M-healthcare clinical follow-up system, identifying the advantages that the M-healthcare system has in comparison with traditional medical treatment, the clinical application effect of the M-healthcare system, and the development status of remote/mobile medical research in China and abroad.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Global diabetes prevalence is increasing rapidly, and China has experienced a particularly dramatic surge in recent years (Laugesen et al. 2015). For instance, the estimated prevalence increased from 9.7% in 2007 to 11.6% in 2010 (Xu et al. 2013; Zhang et al. 2016). In parallel with this increase are growing incidences of common complications, such as retinopathy, kidney disease, neuropathy, and coronary heart disease (Teliti et al. 2018). Effective prevention and management should focus on strict control of blood glucose levels. However, multiple epidemiological studies have found poor glycemic control rates across the globe (Pantalone et al. 2018). Koro et al. (2004) found that glycemic control in American patients with type 2 diabetes mellitus (T2DM), as defined by hemoglobin A1c (HbA1c) < 6.5%, was only 41%, and Liebl et al. (2018) found a control rate of only 31% in European patients based on the same standard. Further, Chuang et al. (2002) reported poor glycemic control in 55% of diabetic patients in Asia and Fu et al. (2012) reported that the overall blood glucose control rate in China (HbA1c < 6.5%) was only 39.7%. With the rapid aging of the Chinese population, the incidences of diabetes and associated secondary comorbidities are projected to rise even higher.
To mitigate this problem, there is an increasing trend to employ mobile information technology (IT) to shift medical treatment services for chronic patients from hospital centers to interactive mobile healthcare (M-healthcare) systems (Baig et al. 2015; Chérrez-Ojeda et al. 2018). This new medical model based on IT has proven feasibility for the management of diabetes in various countries (Ganapathy 2018; Harte et al. 2018; Jeon and Park 2018). Further, the development of biotechnology and IT has allowed for the development of a variety of small medical sensors able to transmit patient data directly to hospitals at any time of the day through mobile phones and other communication tools (Shende et al. 2017; Yapici and Alkhidir 2017; Park et al. 2018). In response, hospitals can provide immediate health guidance for patients. In this review, we focus on the current status of M-healthcare development and application in China, as well as existing problems, in order to provide ideas for improving the control of diabetes.
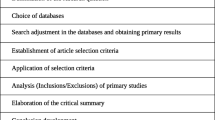
Establishment of an M-healthcare clinical visit system
Comprehensive diabetes self-management includes dietary monitoring, regular exercise, self-monitoring of blood glucose levels, and mental status adjustments. Telemedicine management systems provide personalized medical advice based on current conditions and medical history (Yoo et al. 2009). M-healthcare uses wired and wireless network technologies to provide medical services “whenever and wherever possible” through the internet and mobile phones. Recently, the popularity of smartphones and chat applications has spread to the middle-aged and elderly, not only in urban areas, but also to rural areas, where older diabetes patients may have little experience with computers (Nguyen et al. 2015; Ma et al. 2016). This ubiquity provides opportunities for the widespread development of telemedicine. The M-healthcare system is not only suitable for chronic diseases, but also for sub-healthy populations and healthy populations that require occasional or ongoing health management services (Rosmarin et al. 2010).
Implantation of Bluetooth and 3G chips in blood glucose and blood pressure meters facilitates real-time data transmission through mobile phones to a medical group (Kuroda et al. 2015). The medical group’s server first screens the information, analyzes the risks associated with the current status, such as hyperglycemia and hypoglycemia, and judges whether the patient’s medical behavior is in error. Prediction algorithms for disease development and emergency situations requiring immediate attention by the medical team can assist in decision-making. The medical team can also periodically provide recommendations, feedback information, and reminders for blood glucose monitoring (Baig et al. 2015).
In addition to automatic acquisition of monitoring values from terminal devices, the patient can also manually input medical information for self-management and evaluation of effectiveness under the guidance of the medical team. For example, the patient can transmit current diet and exercise conditions for adjustment according to calorie intake letter classification. Further, exercise compliance can be monitored by collection of motion information or heat dissipation through terminal devices. With the rapid development of network technology, it is also possible to transmit high-quality images, audio signals, or videos, thereby, allowing the M-healthcare system to become an extension of the medical information delivery system, constituting a new type of medical service, with the patient and medical team in a closely interactive environment (González et al. 2013).
The diabetes M-healthcare system developed by our research group
In an earlier telemedicine study, we found that a personal computer (PC) was well adapted to automatically transmit blood glucose meter readings (Wang et al. 2017). However, the PC is not a portable device, and passing information from the patient to the computer and onto the medical team was not very efficient. The emerging popularity of smartphones and chat applications among all age groups provides an alternative for a more ubiquitous and mobile medical communication platform. Although some users find computers difficult to master, many are more open to using a smartphone and may demonstrate proficiency in smartphone use that far exceeds their proficiency in computer use (Davis et al. 2018; Kolar et al. 2017; Ryan et al. 2017). We designed a smartphone-based M-healthcare management platform considering known obstacles to smartphone use and designed the user interface functions with maximum possible simplicity and automation to encourage use by all age groups. This smartphone-based M-healthcare system includes diabetes remote monitoring, an integrated diagnosis management platform, and a diabetes health education network platform.
For remote monitoring and intelligent diagnosis of diabetes by the integrated management platform, patients use a Bluetooth-equipped blood glucose meter and other electronic instruments to send vital signs and other health information, such as medication use, to the data center, where the information is then analyzed by algorithms to rate the level of urgency. For instance, if the blood glucose target value is achieved more than 50% of the time, the system may classify management as good, and send feedback automatically. If not, the system will indicate poor blood glucose management, which will inform the medical group and automatically summarize the patient’s historical data. The patient’s statistical data, preliminary intelligence analysis reports, pending problems, drug treatments, important event reminders, medication history, immunization history, test data, electrocardiogram, radiological data, and other required data are analyzed by the clinical decision-making system (Cho et al. 2010).
This intelligent system not only has the capacity for assessment and prediction, but also evaluates the individual’s self-treatment ability. The patient’s self-management ability is judged according to intelligence, as measured by the Folstein mental state checklist and the Montreal cognitive assessment, and fitness, such as flexibility and endurance for physical activity, physical impairments, fall and fracture risks, visual acuity, and hearing capacity (Thanthrige et al. 2014). This automated integration of reference data and screening can improve clinical monitoring and help doctors prioritize cases for the most efficient workflow.
The M-healthcare system compensates for incomplete medical information gathered during traditional treatment, making up for medical data gaps. Patients with diabetes, hypertension, or other chronic diseases will usually visit a clinic once every three to four months. During the intervening period, poor blood glucose and blood pressure control may have occurred, with a frequency and severity unique to each patient. Therefore, these patients require a more detailed glycemic profile than provided by periodic measures. Actual blood glucose fluctuations and characteristics of blood glucose changes, mainly fasting or postprandial blood glucose elevation and short-term or long-term hyperglycemia, factors affecting glycemic control, including diet and exercise, existing hypoglycemic conditions, and drug risks can be evaluated in real-time by M-healthcare. Further, feedback urging better self-monitoring, such as recommending blood glucose monitoring before breakfast and dinner, the most basic observation points, and according to need 2 h after each meal plus at bedtime, constituting all-day blood glucose observations, will provide information for the evaluation of individual blood glucose type and adjustment of hypoglycemic treatment.
The information stored by the M-healthcare system includes a variety of electronic medical records, such as personal and family medical history, smoking history, drinking history, reproductive history, drug allergy history, occupational environment, and current drug and insulin preparations. These data can provide the medical group with a detailed understanding of the patient and provide personalized health management advice (Granja et al. 2018). According to previous medical history, signs, and related examinations, abnormalities in main organ function or potential insufficiencies can be detected. Further, this information may be used to assess the presence of malignant tumors or other serious diseases that affect life span, and how nutritional status, according to the nutrition screening table, affects health to assess general life quality. For instance, nutritionists may receive patient dietary status on a daily basis through nutrition management software and then use it to provide monthly or weekly dietary advice, while a sports medicine department may assess activity levels by physical assessment software and, under the guidance of doctors, construct a workout plan for the month (Uhm et al. 2017; Marx et al. 2018).
Patients diagnosed with diabetes often express the need to acquire diabetes-related medical knowledge. The diabetes health education network multimedia teaching platform can provide such knowledge. This teaching network platform can provide audiovisual education for patients with diabetes at home or on the hospital ward. The diabetes health education network platform also includes a special communication platform, allowing interactions among patients and between patients and the medical team to improve self-management and compliance. In the past, we emphasized the importance of blood glucose management but neglected the importance of mental health, particularly depression. However, treatment of depression is as crucial as antihyperglycemic drug treatment to obtaining a satisfactory therapeutic effect. Improvement in quality of life, including mood, requires the provision of positive information to the patient (Eker 2018). This content should help improve other aspects of treatment compliance by enhancing motivation, which is negatively impacted by depression.
Effectiveness evaluation of the M-healthcare system
To verify the effectiveness and practicability of the M-healthcare system, we conducted an internet-based telemedicine study of an urban population in 2013. The results confirmed that telemedicine can improve patient glucose and lipid metabolism, as well as patient self-management skills. However, the effectiveness of this system had not been evaluated in China for comparably economically underdeveloped rural areas without modern communications, or for elderly people with relatively little computer experience. Therefore, we set up a smartphone-based M-healthcare system and conducted two clinical trials, one for rural adults with diabetes and one for urban elderly diabetes patients.
Medical resources in rural areas of China are less developed and lack not only large hospitals, but also experienced physicians. Therefore, M-healthcare is a promising method to bridge the gap between supply and demand for rural medical services. In our study of diabetes mobile medicine for the rural population, the intervention group showed a 1.27% decrease in HbA1c after six months of remote management, whereas the control group experienced a 0.68% decrease at three months that was not maintained at six months. After the trial, we conducted a patient satisfaction survey on current treatment, convenience, and willingness to recommend the treatment received to other patients with diabetes. All questions were rated on a 5-point scale, with higher scores indicating greater satisfaction, and the satisfactory ratings ranging from 3.3 to 3.9. In addition, at the end of the study, more than 80% of patients in the intervention group were conducting blood glucose monitoring 2 or 3 days per week and the compliance rate was 72%, indicating that this M-healthcare system can effectively improve patient compliance, even in rural areas with relatively undeveloped medical and economic conditions (Wang et al. 2017).
In China, the diabetes prevalence rate in adults over 60 years of age reached 20.40% in 2008 and 22.86% in 2010. Compared to 2002, there was a 13.60% increase by 2008 and a 16.06% increase by 2013, corresponding to 38 and 41 million patients nationwide, respectively (Yang et al. 2010; Xu et al. 2013). Approximately one in five older patients with T2DM suffers from severe complications, such as diabetic neuropathy, nephropathy, retinopathy, and vasculopathy, which are the major risk factors for renal failure, loss of sight, and loss of lower limbs. Diabetes and diabetic complications jeopardize patient quality of life, independence, and optimism, and place a financial burden on patients, their families, and community healthcare systems (Zimmet et al. 2001; Engelgau et al. 2004).
To investigate smartphone-based telemedicine applications for the management of older Chinese patients with T2DM, we designed a user interface application to facilitate operation with maximum possible simplicity and automation. In our study of diabetes mobile medicine for the urban elderly, HbA1c progressively decreased among the intervention group patients, and six-month levels were significantly lower than those recorded at baseline (P < 0.05) and lower than the control group at six months (P < 0.05). The decrease from baseline was significantly larger in the intervention group than the control group (1.0% versus 0.66%, P < 0.05). The intervention group also demonstrated continuous improvement in postprandial glucose levels from baseline (P < 0.01) and at three months (P < 0.05).
We also obtained satisfaction survey results from patients in the experimental group. Each question was worth one point, and the highest possible score was seven points, with higher point totals indicating greater satisfaction. The average satisfaction score was 6.3 ± 0.78. All individual questions also scored highly, with all means > 0.80, as follows: current treatment satisfaction (0.89 ± 0.19), convenience of M-healthcare monitoring (0.81 ± 0.20), assistance with self-monitoring of blood glucose (0.93 ± 0.14), assistance with diet and exercise management (0.85 ± 0.20), enhancement of diabetes awareness (0.98 ± 0.08), relief of depression (0.96 ± 0.12), and would you recommend M-healthcare monitoring to others (0.91 ± 0.02).
Our M-healthcare research found that HbA1c levels were reduced in the intervention group by three months and maintained at six months. In addition, fasting glucose and postprandial blood glucose were improved. The system allows for effective remote management based on a mobile network, so compliance was also high among rural or elderly patients without easy access to medical facilities. Thus, we found that, regardless of region and age, this intelligent M-healthcare system can improve medication and lifestyle compliance, promote patient education and self-management skills, and provide prompt feedback and advice in cases of poor outcome.
International research progress on remote and telemedicine
M-healthcare development and clinical applications have been the subject of several recent international studies. At the same time, there is a concerted effort to develop improved mobile medical instruments and connection technology (Lee and Chang 2012). At the Catholic University of Korea, mobile phone and network treatment of obesity with hypertension and T2DM resulted in a significant reduction in blood pressure, HbA1c, total cholesterol, low-density lipoprotein, and triglycerides. Cho et al. (2006) examined the long-term (30-month) effects of an internet-based blood glucose monitoring system for reducing HbA1c and stabilizing the blood glucose of T2DM patients. Compared to a control group receiving conventional therapy, the intervention group showed lower and more stable HbA1c levels.
The diabetes interactive diary (DID) is a new telemedicine system that includes carbohydrate/insulin dose calculators, and which allows communication between patients and medical staff, provides type 1 diabetes mellitus patients with a flexible diet plan, and calculates the appropriate amount of insulin required for each meal. Rossi et al. (2010) compared the efficacy of DID to standard carbohydrate counting with regard to metabolism, quality control, education, quality of life, and treatment satisfaction, and found that this system can significantly shorten the guidance time required by medical staff for each patient and greatly improve the patient’s treatment satisfaction and quality of life. Cho et al. (2017) reported on a semi-automatic recovery system that provides feedback to the patient when blood sugar is within the normal range. If the patient’s blood glucose level is abnormal and the medical team requires further analysis and evaluation, it automatically sends a medical treatment plan to the medical group application. Evaluation demonstrated that this system, with decision-making based on baseline values, can save medical work time without affecting communication between doctors and patients. Thus, intelligent data analysis systems and clinical decision support systems can make diabetes network management more effective.
Discussion
Vital medical information for diabetes management includes not only blood glucose levels, but also vital signs, medication history, calorie intake, and calorie consumption. Our diabetes M-healthcare system can collect all of this information and identify potential improvements, lapses in management, and potential risks. However, the data processing for clinical decision-making capacity is still limited for this complex condition. Therefore, it is necessary to develop a software system that reflects the real situation of patients by analyzing correlations among parameters. As the information on diabetic patients becomes even more detailed and complex, the communication technology and patient data acquisition technology will need to be integrated to improve diagnostic accuracy and effectiveness (Dió et al. 2015).
With the development of portable detection equipment for chronic diseases, widespread data transmission networks, and intelligent diagnostic facilities, self-help laboratory inspection services are evolving into self-service virtual hospitals for patients, enabling them to conduct self-management and self-assessment before seeking medical treatment. Virtual hospitals are likely to become an important part of the diabetes M-healthcare system, which will not only provide a wide range of medical information for patients, doctors, and hospitals, but also promote the participation and development of tertiary services, such as health and nutrition services, drug sales, and telecommunications network services to support patient-centered changes to the conventional model of healthcare (Limaye et al. 2017).
Conclusion
Our diabetes mobile healthcare (M-healthcare) system based on information technology (IT) is clinically effective and can reduce medical staff workload. It can be extended to other areas of healthcare in the future, such as remote management of gestational diabetes and hypertension, monitoring of depression associated with diabetes, and patient education. The rapid development of information technology (IT) and remote/mobile medical devices present a great opportunity to establish this medical service model.
References
Baig MM, GholamHosseini H, Connolly MJ (2015) Mobile healthcare applications: system design review, critical issues and challenges. Australas Phys Eng Sci Med 38:23–38. https://doi.org/10.1007/s13246-014-0315-4
Chérrez-Ojeda I, Vanegas E, Calero E, Plaza K, Cano JA, Calderon JC, Valdano J, Gutierrez JO, Guevara J (2018) What kind of information and communication technologies do patients with type 2 diabetes mellitus prefer? An Ecuadorian cross-sectional study. Int J Telemed Appl 2018:3427389. https://doi.org/10.1155/2018/3427389
Cho JH, Chang SA, Kwon HS, Choi YH, Ko SH, Moon SD, Yoo SJ, Song KH, Son HS, Kim HS, Lee WC, Cha BY, Son HY, Yoon KH (2006) Long-term effect of the internet-based glucose monitoring system on HbA1c reduction and glucose stability: a 30-month follow-up study for diabetes management with a ubiquitous medical care system. Diabetes Care 29:2625–2631. https://doi.org/10.2337/dc05-2371
Cho JH, Kim HS, Han JH, Lee JH, Oh JA, Choi YH, Yoon KH (2010) Ubiquitous diabetes management system via interactive communication based on information technologies: clinical effects and perspectives. Korean Diabetes J 34:267–273. https://doi.org/10.4093/kdj.2010.34.5.267
Cho JH, Kim HS, Yoo SH, Jung CH, Lee WJ, Park CY, Yang HK, Park JY, Park SW, Yoon KH (2017) An Internet-based health gateway device for interactive communication and automatic data uploading: clinical efficacy for type 2 diabetes in a multi-centre trial. J Telemed Telecare 23:595–604. https://doi.org/10.1177/1357633X16657500
Chuang LM, Tsai ST, Huang BY, Tai TY; Diabcare-Asia 1998 Study Group (2002) The status of diabetes control in Asia—a cross-sectional survey of 24 317 patients with diabetes mellitus in 1998. Diabet Med 19:978–985. https://doi.org/10.1046/j.1464-5491.2002.00833.x
Davis SR, Peters D, Calvo RA, Sawyer SM, Foster JM, Smith L (2018) “Kiss myAsthma”: using a participatory design approach to develop a self-management app with young people with asthma. J Asthma 55:1018–1027. https://doi.org/10.1080/02770903.2017.1388391
Dió M, Deutsch T, Biczók T, Mészáros J (2015) Intelligent interpretation of home monitoring blood glucose data. Orv Hetil 156:1165–1173. https://doi.org/10.1556/650.2015.30203
Eker S (2018) Prevalence of depression symptoms in diabetes mellitus. Open Access Maced J Med Sci 6:340–343. https://doi.org/10.3889/oamjms.2018.085
Engelgau MM, Geiss LS, Saaddine JB, Boyle JP, Benjamin SM, Gregg EW, Tierney EF, Rios-Burrows N, Mokdad AH, Ford ES, Imperatore G, Narayan KM (2004) The evolving diabetes burden in the United States. Ann Intern Med 140:945–950. https://doi.org/10.7326/0003-4819-140-11-200406010-00035
Fu C, Ji L, Wang W, Luan R, Chen W, Zhan S, Xu B (2012) Frequency of glycated hemoglobin monitoring was inversely associated with glycemic control of patients with type 2 diabetes mellitus. J Endocrinol Invest 35:269–273. https://doi.org/10.3275/7743
Ganapathy K (2018) Telemedicine and neurosciences. Neurol India 66:642–651. https://doi.org/10.4103/0028-3886.232346
González C, Herrero P, Cubero JM, Iniesta JM, Hernando ME, García-Sáez G, Serrano AJ, Martinez-Sarriegui I, Perez-Gandia C, Gómez EJ, Rubinat E, Alcantara V, Brugués E, Chico A, Mato E, Bell O, Corcoy R, de Leiva A (2013) PREDIRCAM eHealth platform for individualized telemedical assistance for lifestyle modification in the treatment of obesity, diabetes, and cardiometabolic risk prevention: a pilot study (PREDIRCAM 1). J Diabetes Sci Technol 7:888–897. https://doi.org/10.1177/193229681300700411
Granja C, Janssen W, Johansen MA (2018) Factors determining the success and failure of eHealth interventions: systematic review of the literature. J Med Internet Res 20:e10235. https://doi.org/10.2196/10235
Harte R, Hall T, Glynn L, Rodríguez-Molinero A, Scharf T, Quinlan LR, ÓLaighin G (2018) Enhancing home health mobile phone app usability through general smartphone training: usability and learnability case study. JMIR Hum Factors 5:e18. https://doi.org/10.2196/humanfactors.7718
Jeon E, Park HA (2018) Development of the IMB model and an evidence-based diabetes self-management mobile application. Healthc Inform Res 24:125–138. https://doi.org/10.4258/hir.2018.24.2.125
Kolar DR, Hammerle F, Jenetzky E, Huss M (2017) Smartphone-Enhanced Low-Threshold Intervention for adolescents with Anorexia Nervosa (SELTIAN) waiting for outpatient psychotherapy: study protocol of a randomised controlled trial. BMJ Open 7:e018049. https://doi.org/10.1136/bmjopen-2017-018049
Koro CE, Bowlin SJ, Bourgeois N, Fedder DO (2004) Glycemic control from 1988 to 2000 among U.S. adults diagnosed with type 2 diabetes: a preliminary report. Diabetes Care 27:17–20. https://doi.org/10.2337/diacare.27.1.17
Kuroda T, Noma H, Takase K, Sasaki S, Takemura T (2015) Bluetooth roaming for sensor network system in clinical environment. Stud Health Technol Inform 216:198–201
Laugesen E, Østergaard JA, Leslie RD; Danish Diabetes Academy Workshop and Workshop Speakers (2015) Latent autoimmune diabetes of the adult: current knowledge and uncertainty. Diabet Med 32:843–852. https://doi.org/10.1111/dme.12700
Lee Y, Chang H (2012) Ubiquitous health in Korea: progress, barriers, and prospects. Healthc Inform Res 18:242–251. https://doi.org/10.4258/hir.2012.18.4.242
Liebl A, Mohan V, Yang W, Strojek K, Linjawi S (2018) 15 years of experience with biphasic insulin aspart 30 in type 2 diabetes. Drugs R D 18:27–39. https://doi.org/10.1007/s40268-018-0228-x
Limaye T, Kumaran K, Joglekar C, Bhat D, Kulkarni R, Nanivadekar A, Yajnik C (2017) Efficacy of a virtual assistance-based lifestyle intervention in reducing risk factors for type 2 diabetes in young employees in the information technology industry in India: LIMIT, a randomized controlled trial. Diabet Med 34:563–568. https://doi.org/10.1111/dme.13258
Ma Q, Chan AH, Chen K (2016) Personal and other factors affecting acceptance of smartphone technology by older Chinese adults. Appl Ergon 54:62–71. https://doi.org/10.1016/j.apergo.2015.11.015
Marx W, Kelly JT, Crichton M, Craven D, Collins J, Mackay H, Isenring E, Marshall S (2018) Is telehealth effective in managing malnutrition in community-dwelling older adults? A systematic review and meta-analysis. Maturitas 111:31–46. https://doi.org/10.1016/j.maturitas.2018.02.012
Nguyen T, Irizarry C, Garrett R, Downing A (2015) Access to mobile communications by older people. Australas J Ageing 34:E7–E12. https://doi.org/10.1111/ajag.12149
Pantalone KM, Misra-Hebert AD, Hobbs TM, Wells BJ, Kong SX, Chagin K, Dey T, Milinovich A, Weng W, Bauman JM, Burguera B, Zimmerman RS, Kattan MW (2018) Effect of glycemic control on the Diabetes Complications Severity Index score and development of complications in people with newly diagnosed type 2 diabetes. J Diabetes 10:192–199. https://doi.org/10.1111/1753-0407.12613
Park J, Kim J, Kim SY, Cheong WH, Jang J, Park YG, Na K, Kim YT, Heo JH, Lee CY, Lee JH, Bien F, Park JU (2018) Soft, smart contact lenses with integrations of wireless circuits, glucose sensors, and displays. Sci Adv 4:eaap9841. https://doi.org/10.1126/sciadv.aap9841
Rosmarin DH, Pargament KI, Pirutinsky S, Mahoney A (2010) A randomized controlled evaluation of a spiritually integrated treatment for subclinical anxiety in the Jewish community, delivered via the Internet. J Anxiety Disord 24:799–808. https://doi.org/10.1016/j.janxdis.2010.05.014
Rossi MC, Nicolucci A, Di Bartolo P, Bruttomesso D, Girelli A, Ampudia FJ, Kerr D, Ceriello A, Mayor CdeL, Pellegrini F, Horwitz D, Vespasiani G (2010) Diabetes Interactive Diary: a new telemedicine system enabling flexible diet and insulin therapy while improving quality of life: an open-label, international, multicenter, randomized study. Diabetes Care 33:109–115. https://doi.org/10.2337/dc09-1327
Ryan EA, Holland J, Stroulia E, Bazelli B, Babwik SA, Li H, Senior P, Greiner R (2017) Improved A1C levels in type 1 diabetes with smartphone app use. Can J Diabetes 41:33–40. https://doi.org/10.1016/j.jcjd.2016.06.001
Shende P, Sahu P, Gaud R (2017) A technology roadmap of smart biosensors from conventional glucose monitoring systems. Ther Deliv 8:411–423. https://doi.org/10.4155/tde-2017-0012
Teliti M, Cogni G, Sacchi L, Dagliati A, Marini S, Tibollo V, De Cata P, Bellazzi R, Chiovato L (2018) Risk factors for the development of micro-vascular complications of type 2 diabetes in a single-centre cohort of patients. Diab Vasc Dis Res 15:424–432. https://doi.org/10.1177/1479164118780808
Thanthrige RS, Dassanayake S, Dissanayake D (2014) Relationship between increased risk of falling and cognitive impairment in residents of an elderly home in the Colombo district. Ceylon Med J 59:21–23. https://doi.org/10.4038/cmj.v59i1.6735
Uhm KE, Yoo JS, Chung SH, Lee JD, Lee I, Kim JI, Lee SK, Nam SJ, Park YH, Lee JY, Hwang JH (2017) Effects of exercise intervention in breast cancer patients: is mobile health (mHealth) with pedometer more effective than conventional program using brochure? Breast Cancer Res Treat 161:443–452. https://doi.org/10.1007/s10549-016-4065-8
Wang G, Zhang Z, Feng Y, Sun L, Xiao X, Wang G, Gao Y, Wang H, Zhang H, Deng Y, Sun C (2017) Telemedicine in the management of type 2 diabetes mellitus. Am J Med Sci 353:1–5. https://doi.org/10.1016/j.amjms.2016.10.008
Xu Y, Wang L, He J, Bi Y, Li M, Wang T, Wang L, Jiang Y, Dai M, Lu J, Xu M, Li Y, Hu N, Li J, Mi S, Chen CS, Li G, Mu Y, Zhao J, Kong L, Chen J, Lai S, Wang W, Zhao W, Ning G; 2010 China Noncommunicable Disease Surveillance Group (2013) Prevalence and control of diabetes in Chinese adults. JAMA 310:948–959. https://doi.org/10.1001/jama.2013.168118
Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, Shan Z, Liu J, Tian H, Ji Q, Zhu D, Ge J, Lin L, Chen L, Guo X, Zhao Z, Li Q, Zhou Z, Shan G, He J; China National Diabetes and Metabolic Disorders Study Group (2010) Prevalence of diabetes among men and women in China. N Engl J Med 362:1090–1101. https://doi.org/10.1056/NEJMoa0908292
Yapici MK, Alkhidir TE (2017) Intelligent medical garments with graphene-functionalized smart-cloth ECG sensors. Sensors (Basel) 17:875. https://doi.org/10.3390/s17040875
Yoo HJ, Park MS, Kim TN, Yang SJ, Cho GJ, Hwang TG, Baik SH, Choi DS, Park GH, Choi KM (2009) A ubiquitous chronic disease care system using cellular phones and the internet. Diabet Med 26:628–635. https://doi.org/10.1111/j.1464-5491.2009.02732.x
Zhang SY, Wu JH, Zhou JW, Liang Z, Qiu QY, Xu T, Zhang MZ, Zhong CK, Jiang W, Zhang YH (2016) Overweight, resting heart rate and prediabetes/diabetes: a population-based prospective cohort study among inner Mongolians in China. Sci Rep 6:23939. https://doi.org/10.1038/srep23939
Zimmet P, Alberti KG, Shaw J (2001) Global and societal implications of the diabetes epidemic. Nature 414:782–787. https://doi.org/10.1038/414782a
Acknowledgements
This study was supported by the Science Technology Department of Jilin Province (20180623006TC) and the Interdisciplinary Project of the First Hospital of Jilin University (JDYYJC010), the Transformation Project of the First Hospital of Jilin University (JDYYZH-1902019), and the Development and Reform Commission of Jilin Province (2016C020).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sun, L., Li, Z., Xi, S. et al. Development of a diabetes mobile healthcare system and clinical application in China: a narrative review. J Public Health (Berl.) 29, 1471–1476 (2021). https://doi.org/10.1007/s10389-020-01263-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-020-01263-6