Abstract
Aim
This study examines the current scenario of the self-reported prevalence of non-communicable diseases (NCDs) in India and states, with a gender perspective. It also explores different factors affecting the prevalence of NCDs among men and women.
Subjects and methods
The study has used data from recent NSSO (71st Round, 2014) survey. Simple bivariate analyses are used to calculate the prevalence rate of NCDs per thousand persons. Binary logistics regression is applied to examine the effects of demographic and socioeconomic variables on the prevalence of NCDs.
Results
The overall prevalence of NCDs is 55 per thousand persons. The prevalence is higher among women (63) as compared to men (47). Among Indian states, difference in the prevalence of NCDs between men and women is the highest in Punjab (45), followed by Himachal Pradesh (44) and Uttaranchal (37), whereas among the union territories (UTs), Daman and Diu (230) shows the widest gap in the prevalence of NCDs between men and women. Rural women (86) are found at the higher risk of NCDs as compared to rural men (64) and their counterpart in urban areas (53). The NCD prevalence is significantly higher among the population aged above 60 years (OR = 8.30, p < 0.001) and in richer section (OR = 1.21, p < 0.001).
Conclusions
In India, women are disproportionately affected by NCDs as compared to men. Across the region, a large gap exists in NCD prevalence between men and women. Hence, there is an urgent need to address this issue in high NCD prevalent states, particularly focusing women from socio-economically disadvantaged background.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The increasing prevalence of non-communicable diseases has become a serious health threat to the global population, and it has been gaining policy recognition over the last decade (World Health Organization 2010). Globally, out of ten deaths, six are due to non-communicable conditions; three to communicable, reproductive or nutritional conditions; and one to injuries (World Health Organization 2008). The non-communicable diseases (NCDs), including cardiovascular diseases, diabetes, asthma, chronic respiratory infections, and cancer are not the only leading causes of deaths, but they increase the burden of morbidity and mortality in the developed as well as in the newly industrialized country like India (Acton et al. 2002; Simpson and Sheikh 2010; Upadhyay 2012; Crocetti et al. 2013). An estimated 36 million people die every year due to such diseases, and nearly 80 % of the burden of such diseases is in low and middle-income countries (LMICs) (World Health Organization 2010). The burden of NCDs is rapidly increasing in LMICs, adversely affecting the society and economy of a nation along with the health status of individuals in the twenty-first century (Beaglehole et al. 2011). In India, about 5.8 million people die because of lung and heart diseases, stroke, cancer, and diabetes. In other words, one in four Indians has the risk of dying due to NCDs before reaching age 70 years (World Health Organization 2010).
Further, gender is one of the important socioeconomic determinants of health. Although men have higher rates of mortality, women report and have more morbidity than men have. There are two broad theories: (1) biological, contending that most of the problem is related to hormonal and genetic differences between men and women, and (2) psychosocial, according to which the difference is due mainly to women’s role in society and their behavior towards illness (Mendoza-Sassi and Béria 2007). This dissimilarity varies across the industrialized as well as the developing countries (Vlassoff 2007). Further, gender differences are reported in health care utilization and after controlling for health outcomes, women have higher utilization rates of medical services than men (Hassanzadeh et al. 2014). In the high-income countries, gender plays an important role in determining the prevalence of self-reported disease and their management (Hosseinpoor et al. 2012). The effect of gender on the actual and reported prevalence of NCDs is persistent in LMICs, affecting the type of and exposure to different risk factors (Shakya et al. 2014; Khuwaja and Kadir 2010). Moreover, gender norms can predict current and future NCD risk. The recent studies have shown that women and men have different levels of exposure and vulnerability to the risk factors of NCDs. Women are more vulnerable to the risk of particular NCDs (such as obesity, diabetes, heart disease, stroke, cancer, chronic respiratory diseases etc.) as compared to men (Anish et al. 2013; Bonita and Beaglehole 2014). It is also evident that women experience more ill health than men do. Factors like the division of labour by gender, differential exposure and vulnerability to stress among women and men etc., are the important stressors which result in poor health of women (McDonough and Walters 2001). Gender relations also affect accessibility to preventive care and treatment for NCDs (Hosseinpoor et al. 2012; Silva et al. 2014).
Besides, self-rated disease prevalence is found as an important health indicator and self-reported symptoms of diseases are found closely associated with morbidity and mortality, where large-scale data on diagnosed NCDs are not available (Vellakkal et al. 2013; Teh et al. 2014; Patra et al. 2014). Previous literature shows a clear difference in the prevalence of self-reported diseases between men and women across the countries. According to a study by Alves and Rodrigues (2005), conducted in São Paulo, the presence of chronic diseases in association with gender is the strongest determinant of self-rated health. Further, gender differences in years of education, marital status, work status, income, living arrangement and lifestyle practices can alter the prevalence of chronic diseases and the demand for health care services in any country (Campos et al. 2015). Vadrevu et al. (2015) have shown that women report poorer ratings on health, despite having a higher life expectancy than men have. Crimmins et al. (2011) have found that women report a higher prevalence of non-fatal but acute diseases and conditions such as arthritis, asthma, depression and cognitive loss, whereas men report, higher prevalence of some diseases including cardiovascular conditions. On the other hand, men are less likely as compared to women to suffer from high blood pressure (HBP) and arthritis, but more likely to suffer from asthma (Teh et al. 2014). Hence, gender is a key determinant of the prevalence of NCDs and plays a crucial role in reporting of diseases in the developing countries. Therefore, the present study has attempted to focus on the current scenario and gap in the reported prevalence of NCDs among men and women in India and its states. The study also tries to identify the determinants of self-reported prevalence of NCDs affected by gender difference.
Material and methods
Data
The study has used data from social consumption and health surveys which collect information on morbidity and diseases conducted by National Sample Survey Organization (NSSO, 71st Round) of India, carried out during 2014 to assess morbidity prevalence and its correlates (National Sample Survey Organisation 2014). Since stratified multi-stage sampling design is adopted for the 71st round, all our estimates are derived by using sampling weights supplied by NSSO.
Study population
The recent NSSO (71st Round) survey covered nearly 65,932 households and 333,104 individuals, and among them, nearly 33,911 individual reported morbidities and diseases during last 15 days. The prevalence rate of NCDs calculation is based on this sample. Whereas, the rest of the analysis is based on 33,876 persons which exclude the missing cases and comprises 168,697 men and 164,407 women. In the present study, for the purpose of the analysis, responses are coded into five different spells of ailment. The respondents are identified and responses are adjusted for mutually exclusive reporting of ailments instead of reporting of multiple spells.
Measurement of variables
All the variables used in this study are discussed in the following two categories:
-
Predictor variables
The principal predictor or independent variables used in the analysis are mainly demographic and socioeconomic characteristics of the respondents. In this study variables are categorized as follows: respondent’s current age (1 = 0 to 14 years, 2 = 15 to 34 years, 3 = 35 to 59 years, 4 = 60 and above years); sex (1 = men, 2 = women); residence (1 = rural, 2 = urban); marital status (1 = never married, 2 = currently married, 3 = widowed/divorced/ separated); level of education (1 = no schooling/illiterate, 2 = primary and below, 3 = middle/higher schooling, 4 = diplomas/graduate diplomas and above); castes (1 = schedule tribe or ST, 2 = schedule caste or SC, 3 = other backward classes or OBCs, 4 = other castes); religion (1 = Hindu, 2 = Muslim, 3 = Christian, 4 = other), region (1 = north, 2 = central, 3 = east, 4 = north-east, 5 = west, 6 = south) and the monthly per capita consumption expenditure (MPCE), representing economic status (1 = poor, 2 = middle, 3 = rich).
-
Outcome variable
In the present study, we have used NCDs as the dependent or outcome variable to explain the prevalence of NCDs, by using self-reported morbidity status. In the survey, question like “what is the nature of ailment during last 15 days” was asked to the household members. Nearly, 61 ailments were reported by different respondents during the survey. We have categorized the diseases according to the ‘International Classification of Diseases 10’ (ICD 10) provided by the WHO (World Health Organization 2015). Here, the outcome variable, i.e. NCDs is recoded into a binary variable (1 = NCDs, 0 = all other morbidities, and diseases).
Statistical analyses
In the first stage, the bi-variate analysis was used to calculate the prevalence rate of NCDs per thousand persons according to the selected socioeconomic and demographic characteristics of the respondents. As the independent variables are interrelated, separate binary logistics regression was carried out to examine the effect of socioeconomic and demographic variables on the prevalence of NCDs. The advantage of logistic regression analysis is that it requires no assumption on the distribution of the independent variables, and the regression coefficient can be interpreted in terms of odds ratio (OR). The odds ratio greater than 1 is interpreted as how many times an event is more likely to occur as compared to the reference group and lesser than 1 is just vice-versa. The entire work of statistical analyses was carried out by using STATA (version13.0), whereas ArcGIS (version 10) was used to prepare the map.
Results
Distribution of sample
Table 1 represents the distribution of men and women samples by their socio-demographic background characteristics. Among 333,104 samples, 168,697 (50.6 %) are men and 164,407 (49.4 %) are women. About 30 % of the sampled populations are aged below 15 years, whereas about 8 % are of the sixty and above age group. About 57 % of the sampled populations belong to urban areas and 43 % belong to rural areas. About 5 % of the sample is widowed, divorced and separated. The proportion of respondents without any education and with high education is 32 % and 9 % respectively. The share of scheduled tribes (STs), scheduled castes (SCs) and other backward class (OBCs) population is 13 %, 17 %, and 40 % respectively. About 76 % of the respondents are Hindu, whereas Muslim, Christian, and other religions constitute about 15 %, 6 % and 4 % respectively. About 22 % samples are collected from the central region of India.
Current prevalence of NCDs in India
In India, the current prevalence of self-reported non-communicable diseases (NCDs) is 55 per thousand persons. At the national level, it is observed that the prevalence of NCDs is much higher among women (63) as compared to men (47). Among Indian states, the prevalence of NCDs is the highest in Kerala (210), followed by Goa (140), Andhra Pradesh (121) and Tamil Nadu (115). These four southern states also hold the top four ranks of the prevalence of NCDs among women and men. Further, it is also observed that NCDs are less prevalent in north-eastern states. The lowest prevalence of NCDs is found in Nagaland (4) followed by Manipur (8), Tripura (9), Assam (11), Meghalaya (13) and Mizoram (14). Among the union territories, Lakshadweep (159) has the highest NCD prevalence, whereas Delhi, the central capital, shows the lowest prevalence (13) (Table 2).
Furthermore, few north Indian states show a considerable gap in the prevalence of NCDs between men and women. Punjab (45) has the highest gap in the prevalence of NCDs among men and women followed by Himachal Pradesh (44) and Uttaranchal (37). Hence, the picture of regional differences in NCD prevalence is very clear here. Few states, particularly the southern states are the hotspot of NCDs in India, whereas the north-eastern states show the reverse scenario Fig. 1.
Gender gap in the prevalence of NCDs in India
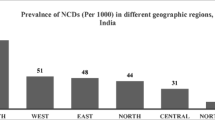
Table 3 represents the prevalence rate of non-communicable diseases (NCDs) per thousand populations according to the socio-demographic characteristics of men and women. The overall prevalence of NCDs, reported by the respondents of this study, is 47 and 63 among men and women respectively, which clearly shows that women are more vulnerable to the risk of NCDs as compared to men. The prevalence of NCDs is monotonically increased with the succeeding age groups; however, men and women of 60 years and above age, are at the high risk of acquiring NCDs, where older women (247 per 1,000) disproportionately suffer more from NCDs than older men (234 per 1,000). The prevalence of NCDs is found high in urban areas among both men and women; nevertheless, women (86) residing in urban areas suffer more from NCDs as compared to men (64). Women who are widowed, divorced and separated reported a higher risk of NCDs as compared to currently married women. The prevalence of NCDs is also found higher among illiterate or low educated women as compared to men with a similar level of education; further, the prevalence of NCDs is also found high among OBC and other castes, among Christians and in the affluent section of the society, where women show higher NCD prevalence as compared to men. The regional variation in the prevalence NCDs is also visible. The southern region (107) shows the highest prevalence of NCDs in India, and women (118) are found more vulnerable to NCDs as compared to men.
Table 4 represents the results (in terms of odds ratio or OR) from the logistic regression analysis, showing the association between different socio-economic variables and the prevalence of NCDs according to the sex of the respondents. Model 1 shows the effects of socio-economic characteristics on the prevalence of NCDs among men, while model 2 shows the prevalence of NCDs among women according to their background characteristics. Further, the model 3 shows the association between prevalence of NCDs and sex of the respondents, after controlling for the other background characteristics.
Results show that women are more likely to suffer from NCDs (OR = 1.02, p < 0.05) as compared to men, irrespective of their other socio-economic characteristics. The age of the respondents is found positively associated with NCDs by sex and is found statistically significant. Respondents of 60 years and above age are found more likely (OR = 8.30, p < 0.001) to suffer from NCDs than the respondents of age below 15 years. The prevalence of NCDs is also found significantly higher among women as compared to men in urban areas (OR = 1.20, p < 0.001); in the richer section of the society (OR = 1.21, p < 0.001); and in the western (OR = 1.59, p < 0.001) and southern (OR = 1.41, p < 0.001) regions. On the other hand, the risk of NCDs is found significantly less among women as compared to men in the scheduled caste (OR = 0.86, p < 0.01) community and in the central region (OR = 0.91, p < 0.05) (Table 4).
Figure 2 represents the difference in the disease-specific prevalence (NCDs) between men and women in India. The cardio-vascular diseases (CVDs) are much more prevalent among women (21 per 1,000) as compared to men (14 per 1,000) in India. Besides, diseases related to respiratory, musculoskeletal and urinary systems are much more prevalent among Indian women than among Indian men. Even though, life-threatening cancer is also highly prevalent among women than among men. Contrarily, the prevalence of metabolic diseases like diabetes, obesity etc. is found higher among men (11) than among women (9). Besides, accident, injuries, burns, fractures, and poisoning are also more prevalent among men than among women.
Discussion
In India, the prevalence of non-communicable diseases (NCDs) largely varies across the states and the regions. The present study shows the regional variation of NCDs in recent time. Further, the northern states represent the highest gap in the prevalence of NCDs between men and women in India. It is evident that men and women have different biological and behavioral characteristics (Case and Paxson 2005). Apart from this, men and women have different exposures to several risk factors (such as smoking, consuming alcohol and tobacco, excessive low and high physical exertion, occupational health threat etc.) of acquiring different NCDs (Mohan et al. 2008; Anish et al. 2013; Bonita and Beaglehole 2014). Hence, the gap in NCD prevalence rate between men and women persists. Further, regional differences in the prevalence of NCDs are also observed. Southern and north-eastern regions show the high and low prevalence of NCDs respectively (Mohan et al. 2008). The study shows that prevalence of smoking is the highest in eastern and southern regions owing to the high prevalence of cardiovascular diseases (Gupta et al. 2012), whereas, the prevalence of overweight/obesity, hypertension and diabetes is the highest in south Indian states (Baruah et al. 2014; Anchala et al. 2014).
Although, previous studies reported that global gender inequality is declining, gender inequality in health still exists (Hassanzadeh et al. 2014). In India, still there is a high volume of excess female deaths at infant and child age (1–4 years) due to discriminatory care at home, discriminatory health-care seeking and selective termination of female fetuses (Bora and Saikia 2015). Socio-cultural differences, related to son-preference, kinship and women’s autonomy, between northern and southern Indian states demonstrate the poor health and higher rate of morbidity and disability in women than in men, but gender difference in disability may not be significant in the context of South India (Sengupta and Agree 2002). The region wise variation in the prevalence of NCDs attributes to regional food habits and harmful dietary practices, consumption of tobacco and sedentary habits (Anchala et al. 2014). Hence, the region specific focus on control of NCDs is important and requires urgent intervention.
Socio-economic conditions can influence people’s exposure and vulnerability to NCDs and can influence health outcomes. The major determinants of NCDs including poverty, illiteracy, poor health infrastructure and social inequality at one side and demographic transition in terms of increasing life expectancy, and urbanization and globalization on the other (Sharma 2013). The study reveals that, in India, the prevalence of NCDs differs according to the socio-economic characteristics of the respondents, irrespective of their sex. Age is consistently associated with all health conditions as an independent risk factor, whereas urban setting is strongly associated with the prevalence of particular diseases (Miszkurka et al. 2012). Similarly, we have found that the prevalence of NCDs is high among the respondents aged above 60 years and among those who residing in urban areas. Further, NCDs are more prevalent among the respondents with high education level and among those who belong to the affluent class (Bhagyalaxmi et al. 2013).
Compared with the findings of the previous study (Upadhyay 2012), the present study has shown that cardiovascular diseases (CVD), respiratory diseases and musculoskeletal diseases are more prevalent among Indian population, and women are found at the higher risk of these NCDs than men are; therefore, women are disproportionately affected by NCDs as compared to men in India. The prevalence of NCDs is found increasing with the increase in age of women as compared to men. Even though the prevalence of NCDs is found higher in urban areas than in rural areas, urban women are at the greater risk of NCDs as compared to urban men. The sedentary lifestyle of the urban population mostly exposes them to the higher risk of NCDs (Mohan et al. 2008). Although improved health of women and girls is a key to sustainable development (PAHO 2011), to date, the global response to the NCD epidemic has missed the significance of girls and women in its approaches and programs (Alliance NCD 2011). Further, underdeveloped health systems and mal-distribution of health care facilities are also the important determinants of health; hence, underdeveloped and under-resourced health care systems worsen the impact of the NCD epidemic (Sharma 2013). Differences in the health needs of men and women must be addressed through appropriate policy effort. Not only the sex-specific health conditions but sex-specific needs in health conditions that affect both must be considered so that treatment can be assessed by both men and women without bias (Sen and Östlin 2007).
Further, in the developing countries, women report more about the symptoms of their illness as compared to men, owing to the higher prevalence rate of self-reported diseases among women (Miszkurka et al. 2012). For the similar reason, reporting of symptoms of NCDs by women is found more in urban areas and among those who are highly educated and aware; however, it is also evident that in many societies, women lack control over resources and, hence, cannot afford quality care for NCDs. Women face sociocultural, geographic, and economic barriers to access health care services (Alliance NCD 2011); hence, the integration of NCD prevention activities into maternal and women-centric health programs has considerable potential, since there is generally poor access to care for women, girls, and other vulnerable groups affected by NCDs (Maina 2011). There is an increasing recognition of the importance of a life-course approach to the prevention of NCDs beginning with the health of girls and young women before and during pregnancy (Bonita and Beaglehole 2014). Research has shown that when mothers are granted greater control over resources, they allocate more to food, children’s health and nutrition, and education (PAHO 2011); hence, consideration of and reduction in gender inequity are the fundamental components of good health and improvement in this areas will help to move India up the gender-equity health ranking (Raj 2011). The transformation of United Nations’ goal of ‘promoting gender equality and women empowerment’ (Millenium Development Goal-3 or MDG-3) to ‘achieve gender equality’ (Sustainable Development Goals or SDG-5) in the next 15 years emphasizes the importance of gender equality in every aspect of our life. Nevertheless, meeting the NCD targets in the SDGs with respect to gender equality, along with nutrition, food, and other health challenges will require an exhaustive level of focus and political will to do so (Hawkes and Popkin 2015).
Strengths and limitations
The present study has its own strengths and limitations. The study has attempted to fill the literature gap and research on non-communicable diseases in India, conducted simultaneously in the state as well as at the national level. It contributes to the estimation of the current prevalence rate of NCDs in India based on recent cross-sectional data. Further, the study is the first of its kind to represent the regional variation in the prevalence of NCDs in India and to focus on the difference in disease prevalence from a gender perspective, which may be useful in planning and rolling out NCDs initiatives by the government (Wandera et al. 2015).
Despite its strengths, this study has few limitations. The findings of the study should be interpreted with the consideration that self-reported diseases and conditions might underestimate the actual prevalence of different NCDs, as self-reported diseases prevalence is subjected to recall bias and affected by respondents’ level of knowledge and willingness to report their health condition (Van Minh et al. 2008; Muggah et al. 2013). Further, estimation of the prevalence rate of any disease based on any multi-purposive sample survey may not always provide an accurate rate of prevalence for the entire population. Again, the cross-sectional nature of NSS does not allow for proper ascribing of causality and associations between explanatory variables and NCDs; hence, disease-specific longitudinal or cohort studies will be more expedient to understand current magnitude and trend of NCDs prevalence (Wandera et al. 2015). Further, there is a dearth of rigorously analyzed sex-disaggregated data related to NCDs in LMICs, which makes it difficult to accurately determine the influence of gender-related factors on NCD morbidity and mortality (Silva et al. 2014).
Conclusions
South Indian states show regional clustering of non-communicable diseases, whereas north Indian states show the highest gap in the NCD prevalence between men and women. These high NCD prevalent states require specific strategy and policy, implemented at the state level to control the particular disease prevalence. In a developing country like India, preventive measures, rather than curative methods of disease control will be cost effective and helpful. Hence, where women are more vulnerable to the certain NCDs, it is imperative to take urgent steps to increase the level of knowledge and awareness of the risk factors for NCDs. In rural areas, programs at the community level can be implemented particularly targeting the women affected by NCDs. Awareness can be spread and diagnosis kit for NCDs can be supplied at affordable prices through trained community health workers among rural women and men. Similarly, in urban areas, programs encouraging healthy lifestyle practices can bring changes in the attitude of urban population by narrowing the gap between men and women in NCD prevalence.
References
Acton KJ, Ríos Burrows N, Moore K, Querec L, Geiss LS, Engelgau MM (2002) Trends in diabetes prevalence among American Indian and Alaska Native children, adolescents, and young adults. Am J Public Health 92:1485–1490. doi:10.2105/AJPH.92.9.1485
Alliance NCD (2011) Communicable diseases: a priority for women’s health and. 1–20.
Alves L, Rodrigues R (2005) Determinants of self-rated health among elderly persons in São Paulo, Brazil. PubMed Commons 17:6–7
Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Angelantonio ED, Prabhakaran D (2014) Hypertension in India. J Hypertens 32:1170–1177. doi:10.1097/HJH.0000000000000146
Anish TS, Shahulhameed S, Vijayakumar K, Joy TM, Shreelakshmi PR, Kuriakose A (2013) Gender difference in blood pressure, blood sugar, and cholesterol in young adults with comparable routine physical exertion. J Family Med Prim Care 2:200–203. doi:10.4103/2249-4863.117424
Baruah MP, Pathak A, Kalra S, Das AK, Zargar AH, Bajaj S, Unnikrishnan AG, Sahay RK (2014) A revisit to prevailing care and challenges of managing diabetes in India: focus on regional disparities. Indian J Endocrinol Metab 18:254–263. doi:10.4103/2230-8210.131113
Bora JK, Saikia N (2015) Gender differentials in self-rated health and self-reported disability among adults in India. PLoS ONE 10(11), e0141953. doi:10.1371/journal.pone.0141953
Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, Baugh V, Bekedam H, Billo N, Casswell S, Cecchini M, Colagiuri R, Colagiuri S, Collins T, Ebrahim S, Engelgau M, Galea G, Gaziano T, Geneau R, Haines A, Hospedales J, Jha P, Keeling A, Leeder S, Lincoln P, McKee M, MacKay J, Magnusson R, Moodie R, Mwatsama M, Nishtar S, Norrving B, Patterson D, Piot P, Ralston J, Rani M, Reddy KS, Sassi F, Sheron N, Stuckler D, Suh I, Torode J, Varghese C, Watt J (2011) Priority actions for the non-communicable disease crisis. Lancet 377:1438–1447. doi:10.1016/S0140-6736(11)60393-0
Bhagyalaxmi A, Atul T, Shikha J (2013) Prevalence of risk factors of non-communicable diseases in a district of Gujarat, India. J Health Popul Nutr 31:78–85
Bonita R, Beaglehole R (2014) Women, and NCDs: overcoming the neglect. Glob Health Action 7:23742. doi:10.3402/gha.v7.23742
Campos ACV, Albala C, Lera L, Sánchez H, Vargas AMDV, Ferreira EF (2015) Gender differences in predictors of self-rated health among older adults in Brazil and Chile. BMC Public Health 15:365. doi:10.1186/s12889-015-1666-9
Case A, Paxson C (2005) Sex differences in morbidity and mortality. Demography 42(2):189–214
Crimmins EM, Kim JK, Solé-Auró A (2011) Gender differences in health: results from SHARE, ELSA and HRS. Eur J Pub Health 21:81–91. doi:10.1093/eurpub/ckq022
Crocetti E, De Angelis R, Buzzoni C, Mariotto A, Storm H, Colonna M, Zanetti R, Serraino D, Michiara M, Cirilli C, Iannelli A, Mazzoleni G, Sechi O, Gonzalez MES, Guzzinati S, Capocaccia R, Maso LD, AIRTUM Working group (2013) Cancer prevalence in United States, Nordic countries, Italy, Australia, and France: an analysis of geographic variability. Br J Cancer 109:219–228. doi:10.1038/bjc.2013.311
Gupta R, Guptha S, Sharma KK, Gupta A, Deedwania P (2012) Regional variations in cardiovascular risk factors in India: India heart watch. World J Cardiol 4:112–120. doi:10.4330/wjc.v4.i4.112
Hassanzadeh J, Moradi N, Esmailnasab N, Rezaeian S, Bagheri P, Armanmehr V (2014) The correlation between gender inequalities and their health related factors in world countries: a global cross-sectional study. Epidemiol Res Int 2014:521569. doi:10.1155/2014/521569, 8 pp
Hawkes C, Popkin BM (2015) Can the sustainable development goals reduce the burden of nutrition-related non-communicable diseases without truly addressing major food system reforms? BMC Med 13:143. doi:10.1186/s12916-015-0383-7
Hosseinpoor AR, Stewart Williams J, Amin A, Araujo de Carvalho I, Beard J, Boerma T, Kowal P, Naidoo N, Chatterji S (2012) Social determinants of self-reported health in women and men: understanding the role of gender in population health. PLoS ONE 7:1–16. doi:10.1371/journal.pone.0034799
Khuwaja AK, Kadir MM (2010) Gender differences and clustering pattern of behavioural risk factors for chronic non-communicable diseases: community-based study from a developing country. Chronic Illn 6:163–170
McDonough P, Walters V (2001) Gender and health: Reassessing patterns and explanations. Soc Sci Med 52 (4):547–559. doi:10.1016/S0277-9536(00)00159-3
Mendoza-Sassi RA, Béria JU (2007) Gender differences in self-reported morbidity: evidence from a population-based study in southern Brazil. Cad. Cad Saude Publica 23(2):341–346
Miszkurka M, Haddad S, Langlois ÉV, Freeman EE, Kouanda S, Zunzunegul MV (2012) Heavy burden of non-communicable diseases at early age and gender disparities in an adult population of Burkina Faso: world health survey. BMC Public Health 12:24. doi:10.1186/1471-2458-12-24
Mohan V, Mathur P, Deepa R, Deepa M, Shukla DK, Menon GR, Anand K, Desai NG, Joshi PP, Mahanta J, Thankappan KR, Shah B (2008) Urban rural differences in prevalence of self-reported diabetes in India: the WHO-ICMR Indian NCD risk factor surveillance. Diabetes Res Clin Pract 80:159–168. doi:10.1016/j.diabres.2007.11.018
Muggah E, Graves E, Bennett C, Manuel DG (2013) Ascertainment of chronic diseases using population health data: a comparison of health administrative data and patient self-report. BMC Public Health 13:16. doi:10.1186/1471-2458-13-16
Maina WK (2011) Integrated non-communicable disease prevention into maternal and child health programs: can it be done and what will it take. Int J Gynaecol Obstet 115:S34–S36
National Sample Survey Organisation (2014) Social consumption in India, Health (NSSO 71st round, January–June 2014). New Delhi: National Sample Survey Organisation, Ministry of Statistics and Programme Implementation, Government of India, New Delhi
Pan American Health Organization (2011) Series: chronic disease issue Brief 2: chronic diseases on global agendas. PAHO, Washington, DC
Patra S, Arokiasamy P, Goli S (2014) Relevance of health knowledge in reporting maternal health complications and use of maternal health care in India. Health Care Women Int 1–19. doi:10.1080/07399332.2014.946509
Raj A (2011) Gender equity and universal health coverage in India. Lancet 377:618–619. doi:10.1016/S0140-6736(10)62112-5
Shakya A, Mishra SR, Giri S, Paudel K, Neupane D (2014) Gender differences and clustering of modifiable risk factors of non-communicable diseases among medical students: a cross sectional study in Nepal. J Community Health 40:147–152. doi:10.1007/s10900-014-9912-0
Sharma K (2013) Burden of non communicable diseases in India: setting priority for action. Int J Med Sci Public Heal 2:7. doi:10.5455/ijmsph.2013.2.7-11
Sen G, Östlin P (2007) Unequal, unfair, ineffective and inefficient gender inequity in health: why it exists and how we can change it. Final report submitted to the WHO Commission on Social Determinants of Health, Women and Gender Equity Knowledge Network, WHO, Geneva, 145 pp
Sengupta M, Agree E (2002) Gender and disability among older adults in North and South India: differences associated with coresidence and marriage. J Cross Cult Gerontol 17:313–336. doi:10.1023/A:1023079219538
Silva ER, Ivankovich M, Jose R, Faramand T (2014) Addressing the unique needs of men and women in non-communicable disease services. USAID Assist Project, USAID, Bethesda, MD
Simpson CR, Sheikh A (2010) Trends in the epidemiology of asthma in England: a national study of 333,294 patients. J R Soc Med 103:98–106. doi:10.1258/jrsm.2009.090348
Teh JKL, Tey NP, Ng ST (2014) Ethnic and gender differentials in non-communicable diseases and self-rated health in Malaysia. PLoS ONE 9, e91328. doi:10.1371/journal.pone.0091328
Upadhyay RP (2012) An overview of the burden of non-communicable diseases in India. Iran J Public Health 41:1–8
Vadrevu L, Kumar V, Kanjilal B, Professor A (2015) Gender differentials in the impact of multi-morbidity on self-rated health in rural West Bengal in India. IOSR J Nurs Health Sci 4:2320–1940. doi:10.9790/1959-04231621
Van Minh H, Ng N, Juvekar S, Razzaque A, Ashraf A, Hadi A, Soonthornthada K, Bich TH, Kanungsukkasem U, Byass P (2008) Self-reported prevalence of chronic diseases and their relation to selected sociodemographic variables: a study in INDEPTH Asian sites, 2005. Prev Chronic Dis 5:A86
Vellakkal S, Subramanian SV, Millett C, Basu S, Stuckler D, Ebrahim S (2013) Socioeconomic inequalities in non-communicable diseases prevalence in India: disparities between self-reported diagnoses and standardized measures. doi:10.1371/journal.pone.0068219
Vlassoff C (2007) Gender differences in determinants and consequences of health and illness. J Heal Popul Nutr 25:47–61
Wandera SO, Kwagala B, Ntozi J (2015) Prevalence and risk factors for self-reported non-communicable diseases among older Ugandans: a cross-sectional study. Glob Health Action 8:1–10. doi:10.3402/gha.v8.27923
World Health Organization (2008) The global burden of disease: 2004 update. Update 2010:146. WHO, Geneva. doi:10.1038/npp.2011.85
World Health Organization (2010) Global status report on noncommunicable diseases. WHO, Geneva
World Health Organization (2015) International classification of diseases, 10th revision. WHO, Geneva
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The data used for this study considered all the ethical issues while collecting information and it is available to all users upon request. This paper is not published previously and not submitted elsewhere.
Funding
The study is not funded by any funding agency.
Conflict of interest
The authors declare that there is no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(JPG 392 kb)
Rights and permissions
About this article
Cite this article
Patra, S., Bhise, M.D. Gender differentials in prevalence of self-reported non-communicable diseases (NCDs) in India: evidence from recent NSSO survey. J Public Health 24, 375–385 (2016). https://doi.org/10.1007/s10389-016-0732-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-016-0732-9