Abstract
Purpose
There are only a few epidemiological studies of dry eye syndrome (DES) in populations with a common academic background. in this study, the prevalence of DES and associated factors were evaluated separately in men and women physical education and sports science graduates.
Study design
Cross-sectional survey.
Methods
A questionnaire about the diagnosis of DES and associated factors was mailed to 9507 graduates of the Faculty of Health and Sports Science, Juntendo University. The questions covered subjective DES using Schaumberg et al.’s questionnaire and the prevalence of diagnosed DES. Associated factors, age, sex, smoking, alcohol consumption, body mass index, daily screen viewing time, and contact lens (CL) use were analyzed.
Results
A total of 2048 valid responses were received. The prevalence of diagnosed DES was 2.9% in men and 9.3% in women. For subjective DES, the prevalence was 14.8% in men and 39.8% in women. The odds ratio for DES was high in men and women who used CLs and women whose daily screen viewing time was ≥ 4 h.
Conclusion
Both diagnosed and subjective DES were highly prevalent in men and women of all ages, particularly among those in their 20 and 30s. CL use was associated with DES in both men and women. Measures to deal with the factors that can be corrected might have a positive effect on the ocular health and quality of life of physical education and sports science graduates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dry eye syndrome (DES) is a disorder in which the stability of the tear layer decreases, causing ocular discomfort and visual disturbances, it may be associated with damage to the surface of the eye [1]. The number of DES patients has been increasing in recent years, and it has become a major public health issue that may interfere with daily life [2, 3]. The current Japanese diagnostic criteria for DES emphasize subjective DES causing ocular discomfort, but they also indicate that visual disturbances, such as diminished functional visual acuity, may be present [1]. Against this backdrop, the authors previously conducted a questionnaire survey of undergraduate physical education and sports science students concerning the visual correction methods currently used by university athletes and related issues. We found that a high proportion of university athletes were experiencing problems with visual correction, and that DES was a factor in these problems at a comparatively high frequency [4]. Building on this, we then conducted a questionnaire survey of students studying physical education and sports science at a single four-year university concerning the current status of DES and the problems it caused for undergraduate physical education and sports science students. We found a high prevalence of both subjective and diagnosed DES [5]. Based on our results, in the present study, we conducted a large-scale questionnaire survey of physical education and sports science graduates at a four-year university who had acquired specialist knowledge and skills related to health and physical education and who engaged in ongoing regular exercise by participating in sports.
Previous large-scale epidemiological surveys of DES using questionnaires in Japan have focused, among others, on visual display terminal (VDT) workers [6, 7], high school students [8], residents of a mountainous area [9], and users of smartphone applications [10]. However, there are few previous epidemiological surveys of adult DES in a subject population with a common academic background, and such studies are rare worldwide. Investigating the prevalence of DES and its associated factors and taking measures to counter them may, therefore, be useful for the health and quality of life (QOL) of such populations. Therefore, the epidemiological study described in this report was conducted.
Subjects and methods
Study participants
Questions about the diagnosis of DES and DES-associated factors were prepared for use as survey questions in the lifestyle and health-related questionnaire used in the J-Fit + Study, mailed to 9507 graduates of the Faculty of Physical Education and the Faculty of Health and Sports Science, Juntendo University. The survey was conducted between December 2018 and March 2019. Responses were received from 2141 individuals (22.5%) who consented to take part in the survey, and the analysis population included 2048 of those who completed the question on clinical DES. These included 1716 men and 332 women, of whom 241 were aged 20–29, 331 aged 30–39, 395 aged 40–49, 327 aged 50–59, 411 aged 60–69, 274 aged 70–79, and 69 aged 80–89 years. Because there were only 2 women in the 50–59 year age group and 3 in the 60–69 year age group, these were excluded from the analysis population. The present study was conducted in compliance with the principles of the Declaration of Helsinki and approved by the Ethics Committee of the Faculty of Health and Sports Science, Juntendo University (no. 30 − 29).
Questionnaire form
The questionnaire about DES took account of the Japanese definition of and diagnostic criteria for DES [3], revised in 2016 by the Japan Dry Eye Society to emphasize the presence of subjective symptoms in the diagnosis of DES.
In view of this history, when preparing the DES questionnaire, the Short Dry Eye Questionnaire developed and validated by Schaumberg et al. [11,12,13], which has been regarded as useful for use in screening questionnaires in large-scale epidemiological surveys since the World Dry Eye Workshop (DEWS) [14], was also considered.
The translation of this questionnaire has been validated by back translation from Japanese to English, and had been used in previous studies by both Uchino et al. [6, 8, 9] and the authors [5].
In the present study, questions were asked about (1) ocular dryness, (2) foreign body sensation in the eye, and (3) whether the individual had been diagnosed with dry eye. The possible responses to questions (1) and (2) were “Always,” “Often,” “Sometimes,” “Occasionally,” and “Never.” Using these questionnaires, subjective DES was defined as a response of “Always,” “Often,” or “Sometimes” to either question (1) or question (2); diagnosed DES was defined as the response that dry eye had been diagnosed to question (3); and clinical DES was defined as the presence of both subjective and diagnosed DES, and the prevalence of each of them was investigated.
The study participants’ ages (age groups stratified by decade), sex, smoking (current smoker or nonsmoker), alcohol consumption (current habitual alcohol consumption or no alcohol consumption), and body mass index (BMI) calculated as self-reported weight (kg) divided by height squared (m2) were also investigated. The participants were divided into three groups according to their BMI, using the cut-off points recommended by the World Health Organization [15]. Based on Uchino et al.’s previous epidemiological studies [6, 8, 9] and our own previous study [16], the time during which they viewed a computer or smartphone screen each day (< 4 h or ≥ 4 h) and whether they were currently using contact lenses (CLs) were also investigated.
Statistical analysis
First, simple tabulations were performed to determine the prevalence of DES. The prevalence and 95% confidence interval (CI) of DES were calculated by sex and age group (stratified by decade). Then, the associations between lifestyle and the prevalence of DES were investigated using logistic regression analysis to calculate the odds ratios (ORs) and 95% CIs. Significance was determined at the 5% level. All statistical analyses were performed using SPSS version 26.
Results
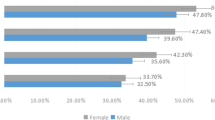
Table 1 shows a comparison of the characteristics of the study participants in men and women. The prevalence of DES in this population is shown in Table 2. In women, the prevalence of diagnosed DES was 9.3%, that of subjective DES was 39.8%, and that of clinical DES was 42.2%, whereas in men, the prevalence of diagnosed DES was 2.9%, that of subjective DES was 14.8%, and that of clinical DES was 15.8%, with both diagnosed and subjective DES clearly more prevalent in women.
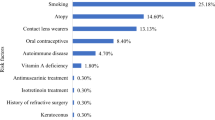
Table 3 shows the prevalence of DES in each age group in men and women and the odds ratios for associated factors. The only factor associated with DES in men was CL use (adjusted OR 2.27, 95% CI 1.59–3.24). The odds ratio for CL use was also high for women (adjusted OR 1.90, 95% CI 1.20–3.02), making it an associated factor for both sexes. In women, VDT use of ≥ 4 h daily also had a high odds ratio (adjusted OR 1.65, 95% CI 0.98–2.78). Both diagnosed DES and subjective DES were present in a high proportion of men and women in a wide range of age groups, from those in their 20s to those in their 80s, with a particularly high prevalence in both men and women in their 20 and 30 s. Additional analysis of DES in all study participants is provided in Online Resource 1 (Supplementary Table 1).
Discussion
According to the DEWS Report [14], the reported prevalence of DES ranges from 5 to 50%, and compared with the prevalence of 4.3–17.9% in the United States, it is, at 12.5–52.4% far higher in Asia. An epidemiological study of DES in Indonesia, located in the tropics, also reports a high DES prevalence of 27.5% [16].
In a comparative study of ethnic differences in DES based on the same diagnostic criteria, an epidemiological survey of 40,000 women in the US that used the same Schaumberg questionnaire [11] also found that the rate was around twice as high among Asians and Hispanics compared with Caucasians, and that many of these patients had severe subjective symptoms. This was consistent with the present results, which identified a high prevalence of subjective DES that was particularly high in women.
Uchino et al.’s DES survey of residents aged ≥40 years in a Japanese mountainous area [9], which used the Japanese translation of Schaumberg’s questionnaire, found that the rate of diagnosed DES was 2.0% in men and 7.9% in women, and that of subjective DES was 11.5% in men and 18.7% in women, whereas the rate of clinical DES in which both were present was 12.5% in men and 21.6% in women. The present study is the first DES survey based on a large-scale population with a common academic qualification in Japan, and the survey found that the rate of diagnosed DES was 3.7% in men and 12.5% in women, and that of subjective DES was 16.5% in men and 45.0% in women, whereas the rate of clinical DES in which both were present was 17.5% in men and 47.5% in women. In comparison with the survey conducted in a mountainous area that used the same questionnaire [9], the prevalence in the present survey was far higher, being 1.4 times higher in men and approximately 2.2 times higher in women. This may be because, as physical education and sports science graduates, the present subject population had acquired specialist knowledge and skills concerning health and physical education, unlike the population of the survey conducted in the mountainous area, and may, therefore, tend to possess greater awareness of health issues, including DES. It was also thought that knowledge and awareness of DES may have become more widespread in Japan during the period between the survey conducted in a mountainous area [9] and the present study.
In the present study, DES was particularly prevalent in both men and women 20–39 years of age. In our previous study of undergraduates studying sports-related subjects [5], we found that, in men, the prevalence of diagnosed DES was 7.0%, and that of subjective DES was 56.2%, whereas, in women, the prevalence of diagnosed DES was 13.5%, and that of subjective DES was 69.4%. Taken together, both studies suggest that there is a consistent trend for a high prevalence of both diagnosed and subjective DES. The reasons may include a tendency for long VDT working time and a high rate of CL use.
The reasons that middle-aged and older men tended to have a lower prevalence of DES may include age-related diminished corneal sensitivity and the underestimation of symptoms, as discussed by Uchino et al. in their study of DES in a mountainous area [9].
In terms of factors associated with DES, in our previous study of DES in university athletes who used a VDT [4], which used the same questionnaire as the present study, the prevalence of DES was 1.8 times higher in both men and women whose VDT working time (daily screen viewing time) was ≥2 h and 7.40 times higher in those who used CLs. These results for associated factors showed a consistent tendency with those identified in the present study.
In the results of an epidemiological survey of 3549 Japanese office workers (2640 men and 909 women) [6], in those engaged in VDT work, subjective DES was present in 26.9% of men and 48% of women, with diagnosed DES in 10.1% of men and 21.5% of women. In terms of factors associated with DES, VDT working time ≥ 4 h increased the risk of DES by 1.7-fold compared with VDT working time <4 h. CL wearers had a 3.6-fold risk of DES compared with non-wearers, a much higher rate.
In the DES survey conducted in a mountainous area [9], CL use was a factor associated with DES in both men and women (3.84-fold risk for men, 3.62-fold risk for women), and VDT use was associated with DES in women (2.34-fold risk).
In the present study as well, CL use was a factor associated with DES in both men and women (2.27-fold risk for men and 1.90-fold risk for women), and for women the daily screen viewing time also had a high odds ratio (1.65-fold). These results are consistent with those of the previous study described above.
CL use was associated with DES in both men and women in both the DES survey of office workers engaged in VDT work and in the present study of physical education and sports science graduates. In general, the frequency of blinking during VDT work is approximately one-third that of normal [17]. This significant decrease in the number of blinks while working on a VDT causes the surface of the eye to be exposed for longer, shortening the breakdown time of the tear layer on the cornea. The decreased blinking caused by the long-term continuation of such VDT work requiring a fixed gaze is reportedly a major cause of evaporative DES [17]. Previous studies report that, in CL users, tears are absorbed from the surface of the eye, meaning that the tear layer on the CL surface is extremely thin and prone to evaporation, leading to the development of evaporative DES [18, 19].
Under these circumstances, in the choice of which CLs to use, soft CLs made of silicone hydrogel are highly permeable to oxygen and have a lower water content, making them less likely than conventional CLs to cause sensations of dryness [20]. They may, therefore, help alleviate DES symptoms in both VDT workers and physical education and sports science graduates.
In light of these results, given that physical education and sports science graduates may be likely to develop symptoms of evaporative DES, they should also be fully informed of the existence of DES as an ophthalmic disorder. Making them aware that the discomfort and visual disturbances due to DES can be improved by improving their habits and continuing treatment with therapeutic eye drops under the care and supervision of an ophthalmologist.
As specific methods of preventing and improving evaporative DES in physical education and sports science graduates, it will be necessary not only to inform them on measures they can take in daily life, such as consciously increasing the number of times they blink and consciously closing their eyes fully to counter the reduced frequency of blinking and shallow, incomplete blinking associated with the fixed gaze entailed by screen use, along with reducing screen time itself, but also to inform people with DES that they should continue to use therapeutic eye drops under the care and supervision of an ophthalmologist. The continued use of artificial tears for hydration and hyaluronate eye drops with a moisturizing action is required to improve DES symptoms [21,22,23]. In recent years, diquafosol sodium eye drops have become widely prescribed as a DES treatment that improves mucin and reduces water loss on the ocular surface. These eye drops are known to encourage fluid secretion in tears on the ocular surface, as well as promote mucin expression, not only improving both dryness and the foreign body sensation in the eyes [24,25,26,27], but also significantly improving functional visual acuity, higher-order aberrations, and corneal backward scattering, stabilizing the tear layer and improving visual disturbances [28]. The continuous use of diquafosol sodium eye drops under normal circumstances, and under the care and supervision of an ophthalmologist, may thus improve DES and enhance visual function of physical education and sports science graduates with DES, and this may help improve their ocular health and QOL.
The present study has a number of limitations. First, the subjects did not undergo objective investigations for clinical DES. Although Schaumberg et al.’s DES questionnaire, used in the present study, has been demonstrated to have high sensitivity and specificity for identifying DES patients [12], the fact that the participants in the present study did not undergo objective investigations for clinical DES, including evaluation of Meibomian gland dysfunction, is a limitation. Second, the DES survey of sports science graduates had a poor response rate compared with other studies, such as Uchino et al.’s DES survey of the residents of a mountainous region, conducted in collaboration with the local government [9], and this may have biased the present results.
Accurate information on the age, sex, and other characteristics of those subjects who did not return the survey could not be obtained, and a comparative investigation with those subjects who did take part is an issue for the future.
Third, data on the status of menopausal symptoms or hormone therapy use, and on the use of medications for systemic conditions such as hypertension, depression, and hay fever were not obtained. Fourth, information on therapeutic eye drops for DES was not obtained, and the use of these medications to alleviate the subjective symptoms of DES requires attention. The subjective symptoms of DES in subjects who use these medications may have been underestimated.
In light of these limitations, further surveys should not only address the details of subjective symptoms in greater depth, but also include larger numbers of patients who have undergone medical studies including objective investigations.
References
Shimazaki J, Yokoi N, Watanabe H, Amano S, Ohashi Y, Kinoshita S, et al. Definition and diagnosis of dry eye in Japan, 2016. Atarashii Ganka. 2017;34:309–13. (in Japanese).
Miljanović B, Dana R, Sullivan DA, Schaumberg DA. Impact of dry eye syndrome on vision-related quality of life. Am J Ophthalmol. 2007;143:409–15.
Management and therapy of dry eye disease: report of the Management and Therapy Subcommittee of the International Dry Eye Workshop (2007). Ocul Surf. 2007;5:163 – 78.
Murakami S, Ohto-Fujita E, Kohmura Y, Shiraishi Y, Aoki K, Sawaki K, et al. Current situation regarding visual correction methods in university athletes and associated issues. Jpn J Clin Sports Med. 2013;21:658–63.
Murakami S, Kohmura Y, Shiraishi Y, Aoki K, Nakata M, Hamano R, et al. Dry eye among undergraduate students studying sports-related subjects: current status and associated issues. Gazz Med Ital. 2019;178:126–31.
Uchino M, Schaumberg DA, Dogru M, Uchino Y, Fukagawa K, Shimmura S, et al. Prevalence of dry eye disease among japanese visual display terminal users. Ophthalmology. 2008;115:1982–8.
Uchino M, Yokoi N, Uchino Y, Dogru M, Kawashima M, Komuro A, et al. Prevalence of dry eye disease and its risk factors in visual display terminal users: the Osaka study. Am J Ophthalmol. 2013;156:759–66.
Uchino M, Dogru M, Uchino Y, Fukagawa K, Shimmura S, Takebayashi T, et al. Japan Ministry of Health study on prevalence of dry eye disease among japanese high school students. Am J Ophthalmol. 2008;146:925–9.
Uchino M, Nishiwaki Y, Michikawa T, Shirakawa K, Kuwahara E, Yamada M, et al. Prevalence and risk factors of dry eye disease in Japan: Koumi study. Ophthalmology. 2011;118:2361–7.
Inomata T, Iwagami M, Nakamura M, Shiang T, Yoshimura Y, Fujimoto K, et al. Characteristics and risk factors associated with diagnosed and undiagnosed symptomatic dry eye using a smartphone application. JAMA Ophthalmol. 2019;138:58–68.
Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136:318–26.
Gulati A, Sullivan R, Buring JE, Sullivan DA, Dana R, Schaumberg DA. Validation and repeatability of a short questionnaire for dry eye syndrome. Am J Opthalmol. 2006;142:125–31.
Schaumberg DA, Buring JE, Sullivan DA, Dana MR. Hormone replacement therapy and dry eye syndrome. JAMA. 2001;286:2114–9.
Stapleton F, Alves M, Bunya VY, Jalbert I, Lekhanont K, Malet F, et al. TFOS DEWS II Epidemiology Report. Ocul Surf. 2017;15:334–65.
Tsugane S, Sasaki S, Tsubono Y. Under- and overweight impact on mortality among middle-aged japanese men and women: a 10-y follow-up of JPHC study cohort I. Int J Obes Relat Metab Disord. 2002;26:529–37.
Lee AJ, Lee J, Saw S-M, Gazzard G, Koh D, Widjaja D, et al. Prevalence and risk factors associated with dry eye symptoms: a population based study in Indonesia. Brit J Ophthalmol. 2002;86:1347–51.
Sato N, Yamada M, Tsubota K. Visual display terminal work and dry eye. Atarashii Ganka. 1992;9:2103–6. (in Japanese).
Nichols JJ, King-Smith PE. Thickness of the pre-and post-contact lens tear film measured in vivo by interferometry. Investig Opthalmol Vis Sci. 2003;44:68–77.
Maruyama K, Yokoi N, Takamata A, Kinoshita S. Effect of environmental conditions on tear dynamics in soft contact lens wearers. Invest Ophthalmol Vis Sci. 2004;45:2563–8.
Chalmers R, Long B, Dillehay S, Begley C. Improving contact-lens related dryness symptoms with silicone hydrogel lenses. Optom Vis Sci. 2008;85:778–84.
Sand BB, Marner K, Norn MS. Sodium hyaluronate in the treatment of keratoconjunctivitis sicca. A double masked clinical trial. Acta Ophthalmol. 1989;67:181–3.
Hori Y, Muramatsu R. Tear supplementation: artificial tear and hyaluronate eye drops. Atarashii Ganka. 2015;32:931–4. (in Japanese).
Nakamura M, Hikida M, Nakano T, Ito S, Hamano T, Kinoshita S. Characterization of water retentive properties of hyaluronan. Cornea. 1993;12:433–6.
Yokoi N, Kato H, Kinoshita S. Facilitation of tear fluid secretion by 3% diquafosol ophthalmic solution in normal human eyes. Am J Ophthalmol. 2014;157:85–92.
Koh S, Ikeda C, Takai T, Watanabe H, Maeda N, Nishida K. Long-term results of treatment with diquafosol ophthalmic solution for aqueous-deficient dry eye. Jpn J Ophthalmol. 2013;57:440–6.
Shimazaki-Den S, Iseda H, Dogru M, Shimazaki J. Effects of diquafosol sodium eye drops on tear film stability in short BUT type of dry eye. Cornea. 2013;32:1120–5.
Yamaguchi M, Ohashi Y. 3% diquafosol ophthalmic solution promotes mucin and tear fluid. Atarashii Ganka. 2015;32:935–42. (in Japanese).
Kaido M, Uchino M, Kojima T, Dogru M, Tsubota K. Effect of diquafosol tetrasodium administration on visual function in short break-up time dry eye. J Ocul Pharmacol Ther. 2013;29:595–603.
Acknowledgements
The authors would like to thank the graduates and the J-Fit + Study for their cooperation.
This work was supported by the Joint Research Program of Juntendo University Faculty of Health and Sports Science and Institute of Health and Sports Science & Medicine, Juntendo University. The authors would also like to thank Forte Science Communications (Tokyo, Japan) for editorial assistance with the preparation of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
S. Murakami, None; Y. Kohmura, None; Y. Someya, None; K. Suzuki, None; K. Inoue, Grants or contracts (Teijin, Otsuka, Wakamoto), Lecture fee (Otsuka, HOYA, Pfizer, Senju, Santen, Allergan, Novartis, ZEISS); S. Amano, Payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events (Santen, AMO, Senju, Alcon, HOYA, Otsuka); K. Aoki, None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Shigeki Murakami
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Murakami, S., Kohmura, Y., Someya, Y. et al. Prevalence of dry eye syndrome and risk factors in physical education and sports science graduates. Jpn J Ophthalmol 67, 175–181 (2023). https://doi.org/10.1007/s10384-022-00973-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-022-00973-6