Abstract
Purpose
The aim of this study was to compare the efficacy of the topical regimens of iodine/steroids vs. antibiotics/steroids in acute to subacute adenoviral keratoconjunctivitis.
Study design
A prospective open-label study.
Patients and methods
Nineteen patients diagnosed with unilateral or bilateral adenoviral conjunctivitis at less than 1 week from onset were enrolled in this study. Patients were divided randomly into two groups; group 1 was treated with 1.5% levofloxacin with 0.1% fluorometholone administered four times a day and group 2 was treated with a sixfold dilution of polyvinyl alcohol iodine (PAI) solution with 0.1% fluorometholone four times a day. Conjunctival samples from all affected eyes were obtained for real-time PCR. The total scores of acute signs (i.e., eyelid edema, conjunctival injecton, conjunctival discharge, follicules, pseudomembranes, subconjunctival hemorrhage) and symptoms, HAdV DNA copy number, and the presence of multiple subepithelial corneal infiltrates (MSI) were evaluated every 5 visits up to Day 30 after diagnosis.
Results
Comparing the total scores of acute signs and symptoms and viral load, we observed no significant differences between the two groups. At day 15 after diagnosis the proportion of patients with MSI in group 2 (35.7%) was significantly lower than in group 1 (0%).
Conclusions
The impact of topical iodine/steroid therapy on acute signs and symptoms associated with adenoviral conjunctivitis is limited and not substantially different in the responses to antibiotics/steroids. However, this regimen results in a significant decrease in the incidence of MSI during the subacute phase of infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human adenoviruses (HAdVs) are among the most frequent causes of epidemic keratoconjunctivitis (EKC). No established antiviral medications are available for the treatment of HAdVs conjunctivitis, and usual treatment is mostly supportive. In Japan, corticosteroids together with antibiotics are often prescribed in order to suppress local inflammation and prevent bacterial superinfection [1]. Although corticosteroids may offer symptomatic relief in the acute phase, this treatment regimen has no effect on viral replication. In fact, a study that featured adenovirus type 5 in a New Zealand rabbit model revealed that corticosteroids alone resulted in an increase in viral replication and prolonged duration of viral shedding [2]. In contrast, povidone iodine (polyvinylpyrrolidone-iodine;PVP-I) has shown antiviral activity in vitro [3]. Some reports indicate that povidone iodine alone or combination with dexamethasone may be effective at eradicating HAdV leading to rapid clinical resolution [4,5,6,7,8]. Other reports indicate that iodine had no substantial effect on the clinical course and outcome of viral conjunctivitis [9, 10]. Collectively, use of povidone iodine and corticosteroids for HAdV conjunctivitis remains controversial.
HAdV conjunctivitis is associated with significant discomfort and can lead to complications due to the immune/inflammatory response that emerges in the subacute to chronic phase of infection. The multiple subepithelial corneal infiltrates (MSI) lesions are believed to represent a cellular immune reaction against viral antigens, deposited in the corneal stroma under Bowman`s membrane [11].
The patients frequently complain of irritation, photophobia, and visual impairment which may last from a few months to several years. However, most reports describing the use of iodine for HAdV conjunctivitis evaluate clinical signs and symptoms during the acute phase (i.e., the first 1 – 2 weeks). In this study, we compared the therapeutic impact of two specific regimens, iodine/corticosteroids vs. antibiotics/corticosteroids instillation, and examined the outcomes up to 4 weeks from the onset of infection.
Methods
Patient enrollment
Twenty-seven eyes of 19 patients with the symptoms of acute conjunctivitis at the first appearance were enrolled in this prospective, open-label study that was conducted at the Nojima Hospital between September 2017 and March 2019. Eligibility criteria included a new diagnosis of acute unilateral or bilateral viral conjunctivitis, with characteristics including follicular involvement, serous discharge, hyperemia, and chemosis for less than one week and confirmed by an immunochromatography test (Adenocheck, Santen) at the first visit. Exclusion criteria included pregnancy, age less than 18 years, presence of an ocular infection or inflammation other than adenoviral conjunctivitis, and previous treatment for HAdV infection or a related condition. Eyes diagnosed after second visit were not included. The study consisted of five or more clinic visits up to 30 days with the following schedule: visit 1: Day 1, visit 2: Day 4, visit 3: Day 8, visit 4: Day 15, and visit 5: Day 30. For practical reasons, 1 day divergence was permitted on visits 2–4, and 2 day divergence was permitted on visit 5.
Treatment protocol
The 19 study participants were divided at random into two groups. All patients in group 1 were treated with 1.5% levofloxacin (LVFX; Santen) with 0.1% fluorometholone to be administered four times per day; the instillation was gradually decreased after visit 4. Patients in group 2 were treated with a sixfold diluted polyvinyl alcohol iodine (PAI; Nitten) solution with 0.1% fluorometholone also to be administered four times a day until visit 4; then PAI was switched to 1.5% LVFX, and the instillations were gradually tapered. A sixfold dilution of PAI has an equivalent iodine concentration to 30-fold (0.33%) PVP-I.
Clinical signs including bulbar and palpebral conjunctival injection were scored on a four-point scale (0 = absence/normal, 1 = mild, 2 = moderate, and 3 = severe); clinical signs including conjunctival discharge, and follicles were scored on a three-point scale (0 = absence/normal, 1 = mild, and 2 = severe); the presence of pseudomembranes and subconjunctival hemorrhage were scored on a two-point scale (0 = absence/normal, 1 = presence). Clinical symptoms including foreign body sensation and epiphora were also scored on a four-point scale (0 = absence/normal, 1 = mild, 2 = moderate, and 3 = severe) (Table1). Presence or absence of MSI was also recorded.
Sample collection
Scrapings from the conjunctival sac were collected after anesthetizing the conjunctiva with oxybuprocaine hydrochloride 0.4% ophthalmic solution by inserting sterile absorbent sponges (Medical Quick Absorber) moistened with sterile physiological saline into the fornix of the lower eyelid. Conjunctival samples OU were obtained at every visit. Samples were stored at − 40 °C immediately after the collection prior to evaluation by real-time PCR.
Real-time PCR of adenovirus DNA
DNA was extracted from the samples using a QIAamp DNA mini kit (Qiagen). The extracted DNA was amplified using PrimeSTAR GXL DNA polymerase (Takara) with the following primers targeting the adenovirus hexon loop1, fiber code, and penton base and directly sequenced.
Hexon protein Loop 1 [12]
CACATCGCCGGACAGGATGCTTCGGAGTA
GTGTTGTGAGCCATGGGGAAGAAGGTGGC
Fiber [13]
GATGTCAAATTCCTGGTCCAC
TACCCGTGCTGGTGTAAAAATC
Penton [14]
CARAAYGAYCACAGCAACTT
GCRGGMACGTTTTCACTRACGGT
The resulting sequences were used to identify the type of adenovirus using a basic local alignment search tool (BLAST).
The total score of acute clinical signs, symptoms, and HAdV DNA copy numbers was evaluated at each visit. Clinical resolution was defined as a total score of clinical signs at 0 or 1 with the absence (score = 0) of symptoms.
Statistical analysis
Wilcoxon test was used for the comparisons of signs and symptoms between the two groups, and for the comparison of viral amount between the eyes with and without MSI. Student`s t-test was used for the comparison of viral amounts between the two groups. Fisher`s exact test was used to compare the proportion of eyes that exhibited resolution of acute clinical signs and the proportion of eyes with MSI; p < 0.05 was considered to be statistically significant.
The study protocol conformed to the tenets of the Declaration of Helsinki and was approved by the Ethics Review Committee of Nojima Hospital. Written informed consent was obtained from all patients. The study was registered on the International Clinical Trial Registry Platform (UMIN Clinical Trials Registry, UMIN000036821, https://www.umin.ac.jp/ctr/index-j.htm).
Results
Nineteen patients with either bilateral or unilateral HAdV conjunctivitis (a total of 27 affected eyes) were assessed. Group1 (LVFX/fluorometholone) included 10 patients (5 men, 5 women) with 14 eyes infected with HAdV. Group 2 (iodine/fliorometholone) included 9 patients (5 men, 4 women) with 13 eyes infected with HAdV. The mean age of the patients was (mean ± SD) was 53.3 ± 4.5 in Groups 1 and and 54.4 ± 5.9 in group 2. HAdV-54 DNA was detected in all affected eyes at least once during the evaluation period.
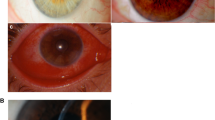
Twenty-four of 27 eyes showed peak symptoms on Day1 or Day4. Three eyes showed a delayed peak on Day 8, while 18 eyes had healed at this point. On Day30, 26 eyes were cured except one with mild symptoms. The total score of signs, symptoms, and amount of viral DNA were not significantly different in a comparison between the two groups at any time during the experimental trial (Figs. 1, 2, and 3). Likewise, the rate of resolution of acute clinical signs did not differ among patients in the two groups (Table2). However, at visit 4 (Day15), there were significantly fewer patients in group 2 who had developed MSI than in group 1 (Fisher’s exact test p < 0.01; Table3). The significant differences were not found in the viral load between the eyes with and without MSI during the observation period (Fig. 4).
Comparison of Human adenovirus DNA copy numbers at each visit between the eyes with and without MSI for group1 (〇: LVFX/FLM) (a) and group2 (●: PAI/FLM) (b). No statistically significant differences were observed. With MSI: patients in which MSI was observed at least once during the observation. Without MSI: patients in which MSI was not observed throughout the observation. MSI: multiple subepithelial corneal infiltrates
No serious adverse effects were reported. There was neither loss of follow-up nor premature discontinuation of drugs in this study.
Discussion
PVP-I is a potent disinfectant that kills extracellular organisms. Previous studies demonstrate that PVP-I was a strong virucidal affecting various types of adenovirus in vitro [3, 15]. However, Isenberg et al. [10] report that PVP-I was ineffective in cases of viral conjunctivitis while PVP-I was as effective as antibiotics in treating bacterial conjunctivitis. Bacteria typically adhere to the surface of infected tissue in biofilms which is accessible to PVP-I; the superficial location of bacteria in the setting of acute conjunctivitis may provide susceptibility to the antibacterial effects of this agent. PVP-I is also highly effective against free virions, including HAdV, but substantially less effective against intracellular viruses; their localization within host cells may protect them from contact with PVP-I [10, 16]. HAdV replication typically peaks during the incubation period and may already be in decline when symptoms appear [17]. Ideally, the PVP-I solution should be administered early enough to limit the acute symptoms and shorten the duration of the disease.
Some clinicians advocate that corticosteroids should be withheld at the early stages of HAdV conjunctivitis, as their administration might result in an increase in the virus replication and prolong the viral shedding [2, 16]. Thus, it has been proposed that corticosteroid treatment should be limited to complicated cases alone. Kovalyuk et al. [16] report that MSI was most frequently observed (44%) in cases treated with steroids alone. By contrast, Asena et al. [18] report that topical corticosteroids have an inhibitory effect on the development of MSI when used as a single therapeutic modality during the acute phase of infection.
Recently, a new topical regimen including povidone iodine combined with corticosteroids has been proposed [4, 6,7,8, 16]. Since antibiotics have no direct impact on virus replication, the results of the present study have been interpreted as a comparison between povidone iodine/corticosteroids combined therapy (Group 2) and corticosteroid therapy alone (Group 1) for the treatment of HAdV conjunctivitis. The results of this study indicate that the iodine/fluorometholone combined therapy has relatively little impact on the course of acute HAdV conjunctivitis within up to 30-days evaluation period. It does, however, significantly decrease the incidence of MSI development at the subacute phase (Day15). These findings are consistent with a previous study [16] that reports that none of the patients receiving combination therapy with iodine/dexamethasone developed MSI.
Steroid administration can add to patient comfort and symptomatic relief. However, even a short course of relatively low-potency corticosteroids (e. g. fluorometholone 0.1%) will increase the duration of viral shedding and prolong the infection of affected patients; this can potentiate a community outbreak [19]. Kovalyuk et al. [16] report that iodine/dexamethasone treatment promoted faster recovery associated with a decrease in the viral amount (PCR) compared to groups treated with dexamethasone alone or with hydroxypropyl methylcellulose. Pepose et al. [4] conclude that iodine/dexamethasone accelerated clinical resolution and promoted eradication of HAdV virions in patients with conjunctivitis more rapidly than iodine or vehicle alone. One interpretation of this finding is that the combination of iodine/dexamethasone administered from an early stage of acute HAdV conjunctivitis can be effective because the corticosteroid component will serve to limit the acute inflammatory symptoms while the iodine prevents prolonged viral shedding resulted by corticosteroid use.
MSI are thought to be the result of delayed immune response to the viral antigens in the corneal stroma [20].
Assuming that the virus that has propagated in the conjunctival cells is released into tears, and spread to the cornea, resulting in antigen deposition, iodine may counteract the side effects of steroid therapy by reducing the viral load and viral antigen in the corneal surface. In the present study, however, reduction in the viral load in the eyes without MSI was not well demonstrated, because of the limitations of PCR, which cannot discern between live and dead viruses.
There are some limitations to the present study. Among them, an official scoring system for evaluating a clinical course of adenoviral keratoconjunctivitis has yet to be proposed. Uemura et al. evaluated the objective ocular clinical findings of corneal and conjunctival lesions on a 4-point scale grading (0 = none, 1 = mild, 2 = moderate, 3 = severe) [21].
In this study, we attempted a finer evaluation of subjective and objective findings on a 2 to 4-points scale. Due to the variety of clinical symptoms and the limited number of cases, however, detailed evaluation for each symptom was abandoned. Instead, the scores of subjective or objective findings were summed up and evaluated together.
Our study featured a six-fold dilution of PAI as part of the therapeutic regimen, but not universally accepted PVP-I. In Japan, PAI was approved for ophthalmic antiseptic use, but PVP-I has not been approved. Berkerman et al. report that diluted PVP-I was more effective than full-strength PVP-I, and the maximum effect was achieved with a between tenfold (1%) and 100-fold (0.1%) [22].
The six-fold dilution of PAI contains as much free iodine as 30-fold (0.33%) PVP-I. Some studies indicate that PVP-I at concentrations of 0.4%–1.25% together with and 0.1% dexamethasone is safe and well-tolerated. Others indicate that a six-fold dilution of PAI has equivalent antiseptic effects to a 16-fold dilution (0.63%) of PVP-I with reduced toxicity in corneal epithelial cells [23, 24].
Likewise, previous reports which support the effectiveness of PVP-I/corticosteroids used a combined regimen featuring 0.1% dexamethasone, however, the present study used fluorometholone. The therapeutic effect may vary depending on the intensity, frequency, duration, and nature of steroid instillation.
Finally, HAdV-54 was detected in all 19 patients in this study. The antiviral activity of PVP-I is reported to be HAdV type-dependent [13]. Some serotypes of this virus may be associated with either more severe or milder forms of infection than that observed in cases of HAdV-54.
This combination of iodine/corticosteroids topical treatment regimen resulted in a significant decrease in the incidence of MSI during the subacute phase of infection. We conclude that the combination of iodine/corticosteroids may be promising for the treatment of acute to subacute HAdV conjunctivitis. Further clinical investigations are required in order to determine the more effective means of asdministration of this combined therapy.
References
Inoue K. Treatment of viral conjunctivitis. Nippon Ganka Gakkai Zasshi. 2003;107:24–6 ((in Japanese)).
Romanowski EG, Yates KA, Gordon YJ. Topical corticosteroids of limited potency promote adenovirus replication in the Ad5/NZW rabbit ocular model. Cornea. 2002;21:289–91.
Kawana R, Kitamura T, Nakagomi O, Matsumoto I, Arita M, Yoshihara N, et al. Inactivation of human viruses by povidone-iodine in comparison with other antiseptics. Dermatology. 1997;195(Suppl 2):29–35.
Pepose JS, Ahuja A, Liu W, Narvekar A, Haque R. Randomized, controlled, phase 2 trial of povidone-iodine/dexamethasone ophthalmic suspension for treatment of adenoviral conjunctivitis. Am J Ophthalmol. 2018;194:7–15.
Yazar H, Yarbag A, Balci M, Teker B, Tanyeri P. The effects of povidone iodine (pH 4.2) on patients with adenoviral conjunctivitis. J Pak Med Assoc. 2016;66:968–70.
Clement C, Capriotti JA, Kumar M, Hobden JA, Foster TP, Bhattacharjee PS, et al. Clinical and antiviral efficacy of an ophthalmic formulation of dexamethasone povidone-iodine in a rabbit model of adenoviral keratoconjunctivitis. Invest Ophthalmol Vis Sci. 2011;52:339–44.
Pelletier JS, Stewart K, Trattler W, Ritterband DC, Braverman S, Samson CM, et al. A combination povidone-iodine 0.4%/dexamethasone 0.1% ophthalmic suspension in the treatment of adenoviral conjunctivitis. Adv Ther. 2009;26:776–83.
Pinto RDP, Lira RPC, Abe RY, Zacchia RS, Felix JPF, Pereira AVF, et al. Dexamethasone/povidone eye drops versus artificial tears for treatment of presumed viral conjunctivitis: a randomized clinical trial. Curr Eye Res. 2015;40:870–7.
Pepose JS, Narvekar A, Liu W, Haque R. A randomized controlled trial of povidone-iodine/dexamethasone ophthalmic suspension for acute viral conjunctivitis. Clin Ophthalmol. 2019;13:535–44.
Isenberg SJ, Apt L, Valenton M, Signore MD, Leo C, Labrador MA, et al. A controlled trial of povidone-iodine to treat infectious conjunctivitis in children. Am J Ophthalmol. 2002;134:681–8.
Dosso AA, Rungger-Brabdle E. A Clinical course of epidemic keratoconjunctivitis: evaluation by in vivo confocal microscopy. Cornea. 2008;27:263–8.
Takeuchi S, Itoh N, Uchio E, Aoki K, Ohno S. Serotyping of adenoviruses on conjunctival scrapings by PCR and sequence analysis. J Clin Microbiol. 1999;37:1839–45.
Xu W, McDonough MC, Erdman DD. Species-specific identification of human adenoviruses by a multiplex PCR assay (published correction: J Clin Microbiol 2001 Apr; 39(4): 1686). J Clin Microbiol. 2000;38:4114–20.
Fujimoto T, Matsushima Y, Shimizu H, Ishimaru Y, Kano A, Nakajima E, et al. A molecular epidemiologic study of human adenovirus type 8 isolates causing epidemic keratoconjunctivitis in Kawasaki City, Japan in 2011. Jpn J Infect Dis. 2012;65:260–3.
Yates KA, Shanks RMQ, Kowalski RP, Romanowski EG. The in vitro evaluation of povidone-iodine against multiple ocular adenoviral types. J Ocul Pharmacol Ther. 2019;35:132–6.
Kovalyuk N, Kaiserman I, Mimouni M, Cohen O, Levartovsky S, Sherbany H, et al. Treatment of adenoviral keratoconjunctivitis with a combination of povidone-iodine 1.0% and dexamethasone 0.1% drops: a clinical prospective controlled randomized study. Acta Ophthalmol. 2017;95:e686–92.
Galasso GJ, et al. Antiviral drugs. In: Notkins A, et al., editors. Concepts in viral pathogenesis. New York: Spronger-Verlag; 1984. p. 382–8.
Asena L, Şıngar Özdemir E, Burcu A, Ercan E, Çolak M, Altınörs DD. Comparison of clinical outcome with different treatment regimens in acute adenoviral keratoconjunctivitis. Eye (Lond). 2017;31:781–7.
Romanowski EG, Roba LA, Wiley L, Araullo-Cruz T, Gordon YJ. The effects of corticosteroids of adenoviral replication. Arch Ophthalmol. 1996;114:581–5.
Lund OE, Stefani FH. Corneal histology after epidemic keratoconjunctivitis. Arch Ophthalmol. 1978;96:2085–8.
Uemura T, Migita H, Ueno T, Saeki Y, Fujimoto T, et al. Clinical and virological analysis of epidemic keratoconjunctivitis caused by adenovirus type 54 in a regional ophthalmic clinic in Kyushu, Japan. Clin Ophthalmol. 2018;12:511–7.
Berkelman RL, Holland BW, Anderson RL. Increased bactericidal activity of dilute preparations of povidone-iodine solutions. J Clin Microbiol. 1982;15:635–9.
Inoue Y, Usui M, Ohashi Y, Shiota H, Yamazaki T. Preoperative Disinfection Study Group. Preoperative disinfection of the conjunctival sac with antibiotics and iodine compounds: a prospective randomized multicenter study. Jpn J Ophthalmol. 2008;52:151–61.
Shibata Y, Yuta Tanaka Y, Tomita T, Taogoshi T, Kimura Y, Taiichiro Chikama T, et al. Evaluation of corneal damage caused by iodine preparations using human corneal epithelial cells. Jpn J Ophthalmol. 2014;58:522–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
K. Matsuura, None; Y. Terasaka, None; D. Miyazaki, Lecture fee (Santen, Senju, Alcon); Y. Shimizu, None; Y. Inoue, None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Kazuki Matsuura
About this article
Cite this article
Matsuura, K., Terasaka, Y., Miyazaki, D. et al. Comparative study of topical regimen for adenoviral kearoconjunctivitis by 0.1% fluorometholone with and without polyvinyl alcohol iodine. Jpn J Ophthalmol 65, 107–114 (2021). https://doi.org/10.1007/s10384-020-00788-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-020-00788-3