Abstract
Purpose
To determine factors predictive of visual outcomes in eyes treated with intravitreal aflibercept injections (IAIs) for typical neovascular age-related macular degeneration (AMD) or polypoidal choroidal vasculopathy (PCV).
Study design
Retrospective, multicenter, institutional, consecutive, interventional case series.
Methods
One hundred nine eyes (107 patients) with treatment-naïve neovascular AMD at 3 university hospitals were studied. After a loading phase of 3 monthly 2.0-mg IAIs, injections were administered every 2 months. The baseline clinical characteristics were investigated in relation to the 12-month visual outcomes. Changes in the mean best-corrected visual acuity (BCVA) were measured at 12 months after initiation of aflibercept therapy.
Results
Forty-five eyes (41.3%) had typical neovascular AMD, and 64 eyes (58.7%) had PCV. The changes in the mean BCVA at 12 months compared with baseline did not differ significantly (P = .737) between the 2 groups. Stepwise analysis showed that larger gains in the BCVA at 12 months were associated with poor BCVA (P < .001), no pigment epithelial detachment (P = .004), and subretinal fluid (P = .039) at baseline in eyes with typical neovascular AMD; larger gains in the BCVA were associated with poorer BCVA (P < .001), presence of choroidal vascular hyperpermeability (CVH) (P = .013), and subretinal fluid (P = .044) at baseline in eyes with PCV.
Conclusions
Although poorer BCVA and the presence of subretinal fluid predicted larger gains in BCVA in both subtypes treated with aflibercept, eyes with typical neovascular AMD had greater improvement if no pigment epithelial detachment was present, while eyes with PCV had greater improvement if CVH was present.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Age-related macular degeneration (AMD) is the leading cause of legal blindness in North America, Europe, Australia, and recently in Asia [1]. However, neovascular AMD in Asian patients has different demographic features from those in white patients. Notably, polypoidal choroidal vasculopathy (PCV) is predominant in Asian patients with AMD [2]. PCV is thought to be a variant of neovascular AMD [3, 4]. On the basis of the distinct funduscopic and angiographic features of PCV, some investigators have speculated that the biologic mechanisms driving neovascularization in PCV might differ from those of typical neovascular AMD. However, the detailed pathophysiology of PCV is not fully understood.
In the previous decade, treatment paradigms for neovascular AMD have shifted to the use of intravitreal vascular endothelial growth factor (VEGF) therapies. Aflibercept (Eylea; Regeneron Pharmaceuticals and Bayer AG), a relatively new anti-VEGF agent, binds to all isoforms of VEGF-A, VEGF-B, and placental growth factor. In the VEGF Trap-Eye: Investigation of Efficacy and Safety in Wet AMD (VIEW) 1 and VIEW 2 trials, intravitreal aflibercept injections (IAIs) dosed monthly or every other month after 3 initial monthly doses had efficacy and safety profiles similar to those of monthly intravitreal ranibizumab (Lucentis; Genentech) injections [5]. Recently, some investigators and we have reported that aflibercept was also effective for treating PCV [6]. Several prognostic factors in neovascular AMD after anti-VEGF injections have been reported, such as patient age [7], greatest linear dimension (GLD) [8], intraretinal fluid (IRF) [9], and pigment epithelial detachment (PED) [10]. Because aflibercept seems to have superior effects on sub-RPE [11] and choroidal lesions [12], the prognostic factors might differ from those reported previously, particularly for PCV. In the current study, we compared the 1-year outcomes for typical neovascular AMD and PCV. We then analyzed the prognostic factors at baseline and the loading phase to predict visual improvement at 1 year.
Patients and methods
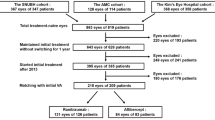
This study was a retrospective and interventional case series that included 172 consecutive patients with treatment-naïve neovascular AMD who were initially examined at the Macula Services of Fukushima Medical University, Tokyo Women’s Medical University, or Kyorin University School of Medicine from December 2012 through October 2013. The institutional review board of each university hospital approved the study protocol, which followed the tenets of the Declaration of Helsinki. Of the 172 patients, 109 eyes of 107 patients were eligible for the current study. To evaluate the visual improvement at 12 months, eyes with a baseline best-corrected visual acuity (BCVA) between 0.06 and 0.8 Japanese standard decimal VA (20/320–20/25 Snellen equivalent) were selected for analysis, according to the criteria of the Comparison of Age-Related Macular Degeneration Treatments Trials (CATT study) [13]. Other inclusion criteria included patient age of 50 years or older, more than 12 months of follow-up, imaging data available from each visit, and the presence of previously untreated active choroidal neovascularization (CNV) secondary to neovascular AMD, either typical neovascular AMD or PCV. Four eyes with retinal angiomatous proliferation were excluded because the number of eyes was too small for statistical analysis. Typical neovascular AMD was characterized by exudative changes due to the presence of CNV as confirmed by fluorescein angiography (FA) and indocyanine green angiography (ICGA). The diagnosis of PCV was based on the ICGA finding of polypoidal structures at the border of a branching choroidal vascular network. In some cases, orange–red protrusions under the RPE were observed biomicroscopically that corresponded to the polypoidal lesions on ICGA. Patients were also excluded if the treated eye had a spherical equivalent of -6 D or less and/or chorioretinal atrophic changes secondary to pathologic myopia; a history of intraocular surgery within 6 months of entrance into the study; non-AMD macular disorders, such as angioid streaks; a history of pars plana vitrectomy; or systemic contraindication for IAIs.
At baseline, all 109 eyes underwent a comprehensive ophthalmic examination including measurement of refraction, VA testing with Landolt C charts, slit-lamp biomicroscopy with contact or noncontact lenses, color fundus photography, FA and ICGA using confocal scanning laser ophthalmoscopy (Heidelberg Retina Angiograph [HRA-2]; Heidelberg Engineering), and optical coherence tomography (OCT). At each monthly visit over the 12-month period, all the patients underwent BCVA testing, slit-lamp biomicroscopy, color fundus photography, and OCT. All 109 eyes were treated with a 2.0-mg IAI monthly for 3 months during a loading phase at baseline and at 1 and 2 months. Thereafter, the patients received IAIs every 2 months—at 6, 8, and 10 months. Between the fixed every-2-month treatments, rescue injections were administered if there was worsening of the subretinal fluid (SRF) and/or IRF seen on the OCT images, a new macular hemorrhage, an expanding PED, or decreased VA greater than the equivalent of 10 Early Treatment Diabetic Retinopathy Study (ETDRS) letters in the presence of retinal fluid on OCT images.
The OCT images were graded for the presence of IRF, SRF, PED (defined as >1 disc diameter and containing hemorrhagic PED), and fibrovascular PED and were used to measure the central retinal thickness (CRT) and subfoveal choroidal thickness (SFCT). The CRT and SFCT were measured using either swept-source (SS)-OCT (DRI-OCT; Topcon) (at Tokyo Women’s Medical University) or enhanced-depth imaging (EDI)-OCT (Heidelberg Spectralis; Heidelberg Engineering) (at Fukushima Medical University and Kyorin University). A high intersystem correlation between these 2 OCT systems was reported previously [14], and the same OCT instrument was always used for all measurements for a patient. With SS-OCT, 12-mm horizontal and vertical scans through the foveal center were obtained. With EDI-OCT, 9-mm horizontal and vertical scans through the foveal center were obtained using the previously reported method [14]. All the images were obtained using an eye-tracking system, and 100 scans were averaged. The CRT was defined as the distance between the surface of the internal limiting membrane and the surface of the RPE at the fovea center. SFCT was defined as the distance between the hyperreflective line corresponding to the Bruch membrane beneath the RPE and the inner scleral surface at the foveal center. CRT and SFCT were measured manually using the OCT caliper function. Independent investigators at each institution who were masked to all patient information including treatment status performed all OCT measurements and gradings. A macula was judged to be dry when there was complete resolution of the SRF and IRF on the OCT images.
The size of the PCV lesions including the branching vascular networks and polypoidal lesions and the number of polypoidal lesions were evaluated using early-phase ICGA in the eyes with PCV. Choroidal vascular hyperpermeability (CVH) was defined as multifocal hyperfluorescence in the middle and late phases of ICGA. The GLD of lesions was measured on FA using the HRA-2 electronic caliper. Two independent investigators evaluated the PCV and CVH in a masked fashion.
The primary outcome was change in BCVA (in logarithm of the minimum angle of resolution [logMAR] units) in eyes with typical neovascular AMD and PCV at 12 months. We compared the baseline characteristics between the 2 subtypes by univariate and stepwise multivariate analyses.
Statistics
Data obtained from all the patients were analyzed using frequency and descriptive statistics. Qualitative data were compared using the Fisher exact test. The mean values were analyzed using the Wilcoxon signed rank test. The BCVA was converted to logMAR units before the calculations. Univariate and multiple linear regression analyses were performed to determine the associations of change in eyes with typical neovascular AMD and PCV at 12 months (objective variables) with ocular and systemic factors (explanatory variables). We performed stepwise analysis with limitations of the Bayesian information criterion and forward selection for BCVA improvement at 12 months, which included the baseline factors of age, sex, CRT, SFCT, SRF, IRF, SRH, PED, CVH, position of CNV, and baseline BCVA (logMAR). Data were expressed as means ± standard deviations. Probability values less than .05 were considered significant. All tests were 2-sided. Statistical analyses were performed using JMP software version 12.2 (SAS Institute).
Results
This study evaluated 109 eyes of 107 patients with treatment-naive neovascular AMD, of whom 22 were women (20.6%) and 85, men (79.4%) (mean age, 74.9 ± 9.0 years; range, 50–92 years). The distribution of the decimal BCVA was as follows: 0.8–0.5 (20/25–40; Snellen equivalent) in 49 eyes (45.0%), 0.4–0.2 (20/50–100) in 37 eyes (33.9%), and 0.1–0.06 (20/200–320) in 23 eyes (21.1%). Typical neovascular AMD was diagnosed in 45 eyes (41.3%), and PCV, in 64 eyes (58.7%). FA showed that the CNV lesions were subfoveal in 77 eyes (70.6%), juxtafoveal in 23 eyes (21.1%), and extrafoveal in 9 eyes (8.2%). Ten eyes (6 eyes with typical neovascular AMD and 4 eyes with PCV) received rescue IAIs at the monthly visit between the scheduled treatments every other month. The average number of IAIs was 7.09 over the 12 months of the study. No significant (P = .313) difference was found in the number of rescue IAIs between the 2 groups. No patients in this study received photodynamic therapy during the follow-up period.
The baseline factors, sex, GLD, CRT, SFCT, PED (>1 disc area [DA]), IRF, SRF, subretinal hemorrhage (SRH) (>1 DA), and CVH, did not differ significantly between the 2 subtypes. The mean baseline ages between patients with typical neovascular AMD (78.0 ± 10.2 years) and those with PCV (72.7 ± 7.5 years) differed significantly (P < .01). The location of CNV on FA differed between typical neovascular AMD and PCV (P = .04) (Table 1). SFCT was significantly thicker in the eyes with CVH (no CVH:CVH = 248 ± 91 microns:306 ± 100 microns; P = .026) in PCV, whereas it did not differ between the eyes with CVH (249 ± 108 microns) and those without CVH (295 ± 66 microns) in typical neovascular AMD (P = .182).
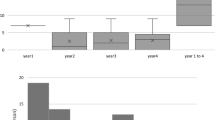
In all the eyes, the mean logMAR BCVA improved significantly (P < .001), from 0.47± 0.32 to 0.27 ± 0.30. In typical neovascular AMD, the mean BCVA improved significantly (P < .001), from 0.52 ± 0.34 at baseline to 0.34 ± 0.32 at 12 months. In PCV, the mean logMAR BCVA improved significantly (P < .001), from 0.43 ± 0.31 at baseline to 0.22 ± 0.29 at 12 months. The mean logMAR BCVA changes at 12 months did not differ significantly (P = .737) between the eyes with typical neovascular AMD (-0.19 ± 0.28) and those with PCV (-0.20 ± 0.28). No significant (P = .559) difference was found in the proportions of eyes with a BCVA gain (-0.3 logMAR units or fewer) by 12 months between the 2 subtypes (22 of 45 eyes [48.9%] with typical neovascular AMD and 36 of 64 eyes [56.3%] with PCV) (Fig. 1). The baseline CRT (typical neovascular AMD, 347 ± 165 microns; PCV, 327 ± 144 microns) decreased significantly (P < .001 for both comparisons) at 12 months in both subtypes (typical neovascular AMD, 205 ± 112 microns; PCV 199 ± 113 microns). No significant (P = .907) difference was found in the changes in the CRT at 12 months between typical neovascular AMD (-142 ± 172 microns) and PCV (-129 ± 147 microns). The BCVA and CRT changes in PCV were similar to those in typical neovascular AMD (Fig. 2). No difference was found in the proportion of eyes with a dry macula between the 2 subtypes: 28 of 45 eyes (62.2%) with typical AMD and 46 of 64 eyes (71.9%) with PCV at 12 months (P = .305).
Mean logarithm of the minimum angle of resolution visual acuity (logMAR VA) in eyes with typical neovascular age-related macular degeneration (AMD) and polypoidal choroidal vasculopathy (PCV) treated with intravitreal aflibercept injections over a 12-month period. No significant differences (P > .05) were seen between the 2 groups at each visit. BCVA best-corrected visual acuity
Mean changes in central retinal thickness in 45 eyes with typical neovascular age-related macular degeneration (AMD) and polypoidal choroidal vasculopathy (PCV) in 64 eyes treated with intravitreal aflibercept injections over a 12-month period. No significant (P > .05) differences were seen between the 2 groups at each visit. The bars indicate the standard errors
Univariate regression analyses showed that together with typical neovascular AMD and PCV, patient age (P = .041), baseline logMAR (P < .001), and baseline CRT (P = .03) contributed to visual improvement at 12 months. Stepwise analysis showed that patient age (P = .005), logMAR units (P < .001) and SRF (P = .007) were prognostic factors at baseline. In typical neovascular AMD, univariate analyses showed that worse BCVA (P < .001) and no PEDs exceeding 1 DA at baseline (P = .03) were associated with BCVA improvement at 12 months; in PCV, patient age (P = .022), poor BCVA (P < .001), CVH (P = .003), and SRF (P = .042) were related to BCVA improvement at 12 months (Table 2). The lesion size of PCV in the ICGA images and number of polypoidal lesions were not significantly correlated with the BCVA improvement (P = .143 and P = .977, respectively).
In typical neovascular AMD, the baseline BCVA (P < .001), PED (P = .004), and SRF (P = .039), and in PCV, the baseline BCVA (P < .001), CVH (P = .013), and SRF (P = .044) were selected as fixed effects. Fixed-effects regression showed significant predictors of VA (R2 = 0.45, P < .001) in typical neovascular AMD and in PCV (R2 = 0.40, P < .001) (Table 2). The pattern of improvement in the BCVA in eyes with CVH was inferior to that in eyes without CVH in typical neovascular AMD, whereas the mean BCVA showed superior improvement in PCV. The eyes with IRF and PED showed similar patterns of improvement in typical neovascular AMD and PCV (Fig. 3).
Logarithm of the minimum angle of resolution visual acuity (logMAR VA) changes in eyes (a) with/without choroidal vascular hyperpermeability (CVH), (b) intraretinal fluid (IRF), (c) a pigment epethelial detachment (SRF) exceeding 1 disc area (DA), and (d) subretinal fluid (PED) at baseline. In eyes with typical neovascular age-related macular degeneration (AMD), 12 eyes had CVH and 33 eyes did not. In eyes with polypoidal choroidal vasculopathy (PCV), 21 eyes had CVH and 43 eyes did not. Nineteen eyes had IRF and 26 eyes did not. In eyes with PCV, 19 eyes had IRF and 45 eyes did not. Forty-one eyes had SRF and 4 eyes did not. In eyes with PCV, 58 eyes had SRF and 6 eyes did not. Eleven eyes had a PED exceeding 1 DA and 34 eyes did not. In eyes with polypoidal choroidal vasculopathy (PCV), 21 eyes had a PED exceeding 1 DA and 43 eyes did not. BCVA best-corrected visual acuity
Discussion
The current study showed that aflibercept therapy for typical neovascular AMD and PCV resulted in equivalent visual outcomes over 12 months of follow-up. Stepwise analysis indicated different prognostic factors for typical neovascular AMD and PCV: for typical neovascular AMD, the specific prognostic factor for an inferior visual outcome was the presence of a PED, and in PCV, the specific prognostic factor for a favorable visual outcome was the presence of CVH.
The efficacy of anti-VEGF therapy for PCV remains uncertain. Previous reports have suggested good visual outcomes in eyes with PCV treated with ranibizumab according to a pro re nata regimen [8, 13]. Because some eyes with PCV were refractory to ranibizumab therapy [15,16,17], some investigators believe that the efficacy of anti-VEGF therapy for treating PCV might be limited when compared with that for treating typical neovascular AMD. The current results found that aflibercept administered according to the 2q8 regimen was equally efficacious for treating typical neovascular AMD and PCV.
The GLDs of PEDs [18,19,20,21] have been suggested to be prognostic factors of anti-VEGF therapy at baseline in PCV, whereas the IRF, SRF, PED [9, 10], and choroidal thickness [22] have been reported to be baseline prognostic factors in studies that included all types of neovascular AMD. Some investigators have suggested that CVH was associated with inferior visual outcomes after ranibizumab or bevacizumab therapy for PCV [16, 23]. Interestingly, the current results indicated that CVH in PCV was a favorable prognostic factor for aflibercept therapy. We speculated that the effects of aflibercept on choroidal exudative changes might have contributed to the results. Recent reports have suggested that aflibercept might suppress choroidal exudative changes. In experimental animal models, aflibercept reduced more fenestrations on the endothelial cells of the choriocapillaris than did ranibizumab [24]. Clinically, aflibercept therapy resulted in markedly decreased choroidal thickness [12], which is associated with CVH [16]. The effects of aflibercept in eyes with CVH might result from the strong affinity to VEGF-A [25] or from inhibition of placental growth factor or VEGF-B, which are other target proteins of aflibercept [26]. CVH in typical neovascular AMD was not a prognostic factor. In addition, the relationship between CHP and choroidal thickness at baseline differs for typical neovascular AMD and PCV. These results suggested that the pathophysiologic mechanisms of CHP in both cases may differ. Further study of the relation between CVH and the morphological findings of PCV is required.
SRF has been reported to be a favorable prognostic factor in PCV and typical neovascular AMD [15, 18]. The visual improvement in PCV after administration of IAIs might be attributed to decreased SRF resulting from improved choroidal exudative changes. Previous multicenter studies have suggested that PED and IRF were inferior prognostic factors in neovascular AMD [9, 10]. Although the current results showed that IRF tended to be related to poorer visual prognosis in typical neovascular AMD, the data did not reach significance (P = .130). In contrast, the trend of visual improvement in eyes with IRF was similar to that in eyes without IRF in PCV. This phenomenon is worth investigating in the future.
The current study had limitations that were related mainly to its retrospective nature, so the difference in the baseline characteristics of age and location of CNV between typical neovascular AMD and PCV must be taken into consideration. A 1-year observation is too short a time to evaluate the efficacy of drugs for neovascular AMD. However, we demonstrated that aflibercept therapy might be equally efficacious for treating typical neovascular AMD and PCV. Eyes with PCV and CVH might be amenable to aflibercept monotherapy, while those that are not might require combination therapy with photodynamic therapy, an area requiring further research.
References
Smith W, Assink J, Klein R, Mitchell P, Klaver CC, Klein BE, et al. Risk factors for age-related macular degeneration: pooled findings from three continents. Ophthalmology. 2001;108:697–704.
Maruko I, Iida T, Saito M, Nagayama D, Saito K. Clinical characteristics of exudative age-related macular degeneration in Japanese patients. Am J Ophthalmol. 2007;144:15–22.
Yannuzzi LA, Sorenson J, Spaide RF, Lipson B. Idiopathic polypoidal choroidal vasculopathy (IPCV). Retina. 1990;10:1–8.
Yuzawa M, Mori R, Haruyama M. A study of laser photocoagulation for polypoidal choroidal vasculopathy. Jpn J Ophthalmol. 2003;47:379–84.
Heier JS, Brown DM, Chong V, Korobelnik JF, Kaiser PK, Nguyen QD, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2011;119:2537–48.
Yamamoto A, Okada AA, Koizumi H, Maruko I, Sekiryu T, Iida T, et al. One-year results of intravitreal aflibercept for polypoidal choroidal vasculopathy. Ophthalmology. 2015;122:1866–72.
Kaiser PK, Brown DM, Zhang K, Hudson HL, Holz FG, Shapiro H, et al. Ranibizumab for predominantly classic neovascular age-related macular degeneration: subgroup analysis of first-year ANCHOR results. Am J Ophthalmol. 2007;144:850–7.
Yamashiro K, Tomita K, Tsujikawa A, Nakata I, Akagi-Kurashige Y, Miyake M, et al. Factors associated with the response of age-related macular degeneration to intravitreal ranibizumab treatment. Am J Ophthalmol. 2012;154:125–36.
Simader C, Ritter M, Bolz M, Deak GG, Mayr-Sponer U, Golbaz I, et al. Morphologic parameters relevant for visual outcome during anti-angiogenic therapy of neovascular age-related macular degeneration. Ophthalmology. 2014;121:1237–45.
Schmidt-Erfurth U, Waldstein SM, Deak GG, Kundi M, Simader C. Pigment epithelial detachment followed by retinal cystoid degeneration leads to vision loss in treatment of neovascular age-related macular degeneration. Ophthalmology. 2015;122:822–32.
Broadhead GK, Hong T, Zhu M, Li H, Schlub TE, Wijeyakumar W, et al. Response of pigment epithelial detachments to intravitreal aflibercept among patients with treatment-resistant neovascular age-related macular degeneration. Retina. 2015;35:975–81.
Koizumi H, Yamamoto A, Maruko I, Sekiryu T, Okada AA, Iida T, et al. Subfoveal choroidal thickness during aflibercept therapy for neovascular age-related macular degeneration: twelve-month results. Ophthalmology. 2016;123:617–24.
Jaffe GJ, Martin DF, Toth CA, Daniel E, Maguire MG, Ying GS, et al. Macular morphology and visual acuity in the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2013;120:1860–70.
Ikuno Y, Yasuno Y, Miura M, Sekiryu T, Nishida K, Iida T, et al. Reproducibility of retinal and choroidal thickness measurements in enhanced depth imaging and high-penetration optical coherence tomography. Invest Ophthalmol Vis Sci. 2011;52:5536–40.
Cho M, Barbazetto IA, Freund KB. Refractory neovascular age-related macular degeneration secondary to polypoidal choroidal vasculopathy. Am J Ophthalmol. 2009;148:70–8.
Koizumi H, Yamagishi T, Yamazaki T, Kinoshita S. Relationship between clinical characteristics of polypoidal choroidal vasculopathy and choroidal vascular hyperpermeability. Am J Ophthalmol. 2013;155:305–13.
Saito M, Iida T, Kano M, Itagaki K. Two-year results of intravitreal ranibizumab for polypoidal choroidal vasculopathy with recurrent or residual exudation. Eye (Lond). 2013;27:931–9.
Hikichi T, Kitamei H, Shioya S. Prognostic factors of 2-year outcomes of ranibizumab therapy for polypoidal choroidal vasculopathy. Br J Ophthalmol. 2015;99:817–22.
Kang HM, Koh HJ. Long-term visual outcome and prognostic factors after intravitreal ranibizumab injections for polypoidal choroidal vasculopathy. Am J Ophthalmol. 2013;156:652–60.
Koizumi H, Yamagishi T, Yamazaki T, Kinoshita S. Predictive factors of resolved retinal fluid after intravitreal ranibizumab for polypoidal choroidal vasculopathy. Br J Ophthalmol. 2011;95:1555–9.
Hikichi T, Higuchi M, Matsushita T, Kosaka S, Matsushita R, Takami K, et al. Factors predictive of outcomes 1 year after 3 monthly ranibizumab injections and as-needed reinjections for polypoidal choroidal vasculopathy in Japanese patients. Retina. 2013;33:1949–58.
Kang HM, Kwon HJ, Yi JH, Lee CS, Lee SC. Subfoveal choroidal thickness as a potential predictor of visual outcome and treatment response after intravitreal ranibizumab injections for typical exudative age-related macular degeneration. Am J Ophthalmol. 2014;157:1013–21.
Cho HJ, Kim HS, Jang YS, Han JI, Lew YJ, Lee TG, et al. Effects of choroidal vascular hyperpermeability on anti-vascular endothelial growth factor treatment for polypoidal choroidal vasculopathy. Am J Ophthalmol. 2013;156:1192–200.
Julien S, Biesemeier A, Taubitz T, Schraermeyer U. Different effects of intravitreally injected ranibizumab and aflibercept on retinal and choroidal tissues of monkey eyes. Br J Ophthalmol. 2014;98:813–25.
Stewart MW, Rosenfeld PJ. Predicted biological activity of intravitreal VEGF Trap. Br J Ophthalmol. 2008;92:667–8.
Takahashi S. Vascular endothelial growth factor (VEGF), VEGF receptors and their inhibitors for antiangiogenic tumor therapy. Biol Pharm Bull. 2011;34:1785–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
M. Ogasawara, None; Hideki Koizumi, Grant (Novartis Pharma), Moderator fees (Alcon, Bausch & Lomb, Bayer, Canon, HOYA, Kowa, NIDEK, Novartis Pharma, Santen Pharmaceutical, Senju Pharmaceutical, Topcon, Wakamoto Pharmaceutical); A. Yamamoto, Lecture fees (Bayer, Novartis Pharma, Pfizer, Santen Pharmaceutical); K. Itagaki, None; M. Saito, Grant (Bayer, Novartis Pharma, Santen Pharmaceutical), Moderator fees (Alcon, AMO, Bayer, HOYA, Novartis Pharma, Santen Pharmaceutical, Senju Pharmaceutical); I. Maruko, Moderator fees (Alcon, Bayer, NIDEK, Novartis Pharma, Santen Pharmaceutical, Topcon); A. A. Okada, Grant (Bayer, Mitsubishi Tanabe Pharma), Advisory board fee (Bayer), Consultant fee (XOMA), Lecture fees (Bayer, Novartis Pharma, Santen Pharmaceutical), Research funds (Bayer, Mitsubishi Tanabe Pharma); T. Iida, Grant (Bayer, Nidek, Novartis Pharma, Santen Pharmaceutical), Lecture fees (Bayer, Novartis Pharma, Santen Pharmaceutical); T. Sekiryu, None.
Additional information
Corresponding author: Tetsuju Sekiryu
About this article
Cite this article
Ogasawara, M., Koizumi, H., Yamamoto, A. et al. Prognostic factors after aflibercept therapy for typical age-related macular degeneration and polypoidal choroidal vasculopathy. Jpn J Ophthalmol 62, 584–591 (2018). https://doi.org/10.1007/s10384-018-0605-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-018-0605-6