Abstract
Purpose
To evaluate the progression and risk factors of diabetic retinopathy during and after pregnancy in patients with diabetes.
Methods
We checked the medical records of the patients with diabetes who were referred to the Diabetes Center, Tokyo Women’s Medical University Hospital (Tokyo, Japan), and were pregnant between August 2004 and September 2010. The patients whose ophthalmic examinations records could not be found (n = 15) were excluded, and thus 93 patients (type 1 = 68, type 2 = 25) were included in the analyses. Data were obtained from the medical record and evaluated.
Results
The mean pre-pregnancy HbA1c was 7.1 ± 0.8 %. All patients were encouraged to maintain HbA1c level of under 7.4 % before pregnancy. At baseline, the percentage of patients with no retinopathy was 78 %, with nonproliferative retinopathy 14 %, and with proliferative retinopathy, 8 %. Progression of retinopathy occurred in 16 (17 %) patients. Two (2 %) had loss of visual acuity and 1 (1 %) underwent laser treatment due to progression of retinopathy. Compared with patients who did not show progression, the patients with progression were characterized by longer duration of diabetes (p < 0.00001), presence of diabetic retinopathy before pregnancy (p < 0.00001) and higher blood pressure in the second trimester (p < 0.05).
Conclusions
Frequent ophthalmic examination, especially in patients with a long history of diabetes, is recommended, as well as for patients with presence of diabetic retinopathy before pregnancy. In contrast to previous reports, the progression of retinopathy in this study was lower. This is probably due to our patients’ pre-pregnancy tight glucose control and the high ratio of patients with no retinopathy at baseline.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
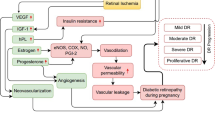
The influence of pregnancy is an important concern for patients with diabetes mellitus as it is known that pregnancy is a major risk factor in the progression of diabetic retinopathy [1, 2] and that this progression varies widely during pregnancy. Poor glucose control, longer duration of diabetes mellitus and high blood pressure are known risk factors for progression of diabetic retinopathy during pregnancy [3–7]. Implications of pregnancy for diabetic retinopathy also continue for the 1st year after delivery [2]. The objective of this study was to evaluate the progression and risk factors of diabetic retinopathy during pregnancy and 12 months following delivery in a group of patients with diabetes mellitus.
Methods
Study design, participants and outcomes
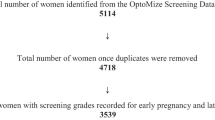
We checked the medical records of patients with diabetes mellitus, who were referred to the Diabetes Center, Tokyo Women’s Medical University Hospital (Tokyo, Japan) and were pregnant between August 2004 and September 2010.
The patients whose ophthalmic examinations records could not be found (n = 15) were excluded, and thus 93 patients (68 type 1 diabetes patients, 25 type 2 diabetes patients) were included in the analyses.
Data obtained from medical records included the patients’ age, height, weight, type of diabetes mellitus, duration of diabetes mellitus, stage of diabetic retinopathy, history of ophthalmic treatment, pre-pregnancy glucose-lowering treatment, glycemic control [HbA1c levels; National Glycohemoglobin Standardization Program (NGSP)], blood pressure, serum creatinine levels and delivery type. The gestational age and birth weight of the newborn were also noted. Landolt visual acuities were converted into a logMAR score.
All patients underwent at least 1 examination each trimester of pregnancy. Dilated funduscopy was performed by ophthalmologists specializing in diabetic retinopathy, and these findings were classified into 6 stages (Table 1). Progression was defined as the worsening of retinopathy by at least 1 stage in at least 1 eye.
NGSP HbA1c levels were measured using column chromatography with a range of 4.3–5.8 % considered normal. Blood pressure was measured using a digital blood pressure monitor with the patient in a sitting position at rest. The degree of nephropathy was evaluated using serum creatinine levels, with a range of 0.48–0.79 mg/dl considered normal.
The study protocol followed the guidelines of the Declaration of Helsinki for research involving human subjects and the Tokyo Women’s Medical University Hospital’s institutional review board approved the study protocol.
Statistical analysis
Data are presented as mean (±SD) or as numbers (%). Statistical analyses were performed using unpaired t-tests and Fisher’s exact test, as appropriate.
Statistical significance was defined at a 2-tailed p value of <0.05.
Results
Clinical characteristics
The clinical characteristics before pregnancy for the 93 patients included in this study are summarized in Table 2. Mean age was 33.8 ± 4.2 years with a range of 22–43 years. Mean duration of diabetes mellitus was 13.0 ± 7.0 years with a range of 1–29 years. Mean HbA1c level was 7.1 ± 0.8 % with a range of 4.9–8.5 %, mean blood pressure was 117 ± 14/72 ± 9 mmHg with a range of 53–99/88–181 mmHg, and serum creatinine levels were 0.61 ± 0.13 mg/dl with a range of 0.40–1.11 mg/dl. No patient had hypertension.
All patients were encouraged to keep HbA1c level of under 7.4 % before pregnancy; therefore, the pre-pregnancy HbA1c level of 75 patients (81 %) was under 7.4 %.
Diabetic retinopathy was present in at least 1 eye in 21 (23 %) patients, of these 7 (8 %) had proliferative diabetic retinopathy.
Progression of retinopathy
Sixteen patients (17 %) experienced progression of diabetic retinopathy (Table 3). Two (2 %) had loss of visual acuity, and 1 (1 %) received laser treatment for severe nonproliferative diabetic retinopathy. Two patients developed changes in the first trimester, 5 in the second, 5 in the third, and 4 after delivery.
The 2 patients with loss of visual acuity during pregnancy are briefly described below. Before pregnancy, both patients had bilateral proliferative diabetic retinopathy treated with panretinal photocoagulation. Both patients subsequently developed vitreous hemorrhage in 1 eye during their pregnancies: one at 19 weeks of gestation and the other at 33 weeks of gestation. After delivery, lost vision was regained as the vitreous hemorrhage resolved without vitrectomy. Both patients had normal blood pressure and were under good glycemic control during their pregnancies, and neither had renal dysfunction.
The patient that underwent a laser treatment during pregnancy had bilateral mild nonproliferative diabetic retinopathy before pregnancy. During the second trimester, she developed severe nonproliferative diabetic retinopathy, and a bilateral retinal laser treatment was performed. After treatment, her degree of diabetic retinopathy remained stable.
The percentage of each stage of diabetic retinopathy is described below; stages 1, 2, 3, 4 and 5 at baseline were 78, 14, 0, 8 and 0 %, respectively, and stages 1, 2, 3, 4 and 5 at the last visit were 74, 14, 4, 5 and 2 %, respectively.
Clinical characteristics and progression of retinopathy
The rate of diabetic retinopathy progression was significantly increased in patients who had a longer duration of diabetes mellitus (p < 0.00001) and in patients who had diabetic retinopathy before becoming pregnant (p < 0.00001) (Table 3).
The patients who showed progression had higher HbA1c levels (before pregnancy, first trimester, second trimester, after delivery) and higher systolic blood pressure (second trimester) than patients who did not show progression (p < 0.05, respectively) (Table 4).
Discussion
In our study, the rate of diabetic retinopathy progression was significantly increased in patients who had a longer duration of diabetes mellitus. A longer duration of diabetes mellitus had the highest statistical association with the progression of diabetic retinopathy. No association was found between rates of progression and age. Our result is the same as previous studies [3, 7, 8]. Compared with patients who did not show progression, the patients with progression were characterized by presence of retinopathy before pregnancy. This indicates that patients with a long history of diabetes mellitus need especially strict ophthalmic examination, and those showing presence of diabetic retinopathy before pregnancy need frequent examination.
In the non-pregnant population with diabetes mellitus, high blood pressure has been associated with progression of diabetic retinopathy [8]. This is also true in the pregnant population with diabetes mellitus, as higher blood pressure in pregnancy has been associated with progression of diabetic retinopathy during pregnancy [3, 6, 7]. In our study the patients showing progression had higher systolic blood pressure in the second trimester than those patients who did not show progression.
The patient who had severe nonproliferative diabetic retinopathy received photocoagulation. The ophthalmologist in charge of this patient seems to have considered it unwise to wait until proliferative changes developed, because a previous report showed that a delay in panretinal photocoagulation treatment was a risk factor of poor visual outcome [9]. After treatment, this patient had no further progression of diabetic retinopathy and no loss of visual acuity.
In comparison with previous studies, the progression of diabetic retinopathy in the present study is lower. Progression of diabetic retinopathy during pregnancy is reported to occur in 17.4–41.5 % of cases [2–4, 6, 7]. In the present study, progression of diabetic retinopathy during pregnancy and up to 1 year after delivery, occurred in 17 % of patients, and few patients had sight-threatening progression. This is probably due to the fact that sudden tight glucose control is associated with worsening of diabetic retinopathy [10, 11]. A previous report suggests that the rapid improvement in glucose control that often occurs in early pregnancy may result in an increased risk for the progression of diabetic retinopathy and that it is important that patients with diabetes who may become pregnant establish good glucose control before conception [4]. In our study, in contrast to previous reports, most patients were in tight glucose control before pregnancy (mean pre-pregnancy HbA1c = 7.1 ± 0.8 %) because our patients were strictly encouraged to maintain HbA1c level under 7.4 % before becoming pregnant. As a result, the pre-pregnancy HbA1c level of 75 patients (81 %) was under 7.4 %. In addition, previous studies show that diabetic retinopathy most often progresses in the second trimester [2, 5] but, in our study, the patients who showed worsening of diabetic retinopathy were evenly distributed in every trimester. This may be related to avoiding the rapid improvement in glucose control in early pregnancy in our study. We tell all patients that it is advisable to conceive a child after maintaining good glucose control. Consequently, the number of patients showing progression of retinopathy was probably relatively small.
In a previous study, Chew et al. reported that “progression of retinopathy was seen in 10.3, 21.1, 18.8 and 54.8 % of patients with no retinopathy, microaneurysm only, mild nonproliferative retinopathy and moderate-to-severe nonproliferative retinopathy at baseline, respectively” [4]. In our study, the percentage of patients with no retinopathy at baseline was 78 %. There is a possibility that this high ratio was related to our low rate of retinopathy progression.
It is important that patients with diabetes mellitus maintain good glucose control before becoming pregnant. Certain cases probably need conception control.
References
Klein BE, Moss SE, Klein R. Effect of pregnancy on progression of diabetic retinopathy. Diabetes Care. 1990;13:34–40.
The Diabetes Control and Complications Trial Research Group. Effect of pregnancy on microvascular complications in the diabetes control and complications trial. Diabetes Care. 2000;23:1084–91.
Axer-Siegel R, Hod M, Fink-Cohen S, Kramer M, Weinberger D, Schindel B, et al. Diabetic retinopathy during pregnancy. Ophthalmology. 1996;103:1815–9.
Chew EY, Mills JL, Metzger BE, Remaley NA, Jovanovic-Peterson L, Knopp RH, et al. Metabolic control and progression of retinopathy. Diabetes Care. 1995;18:631–7.
Temple RC, Aldridge VA, Sampson MJ, Greenwood RH, Heyburn PJ, Glenn A. Impact of pregnancy on the progression of diabetic retinopathy in Type 1 diabetes. Diabet Med. 2001;18:573–7.
Vestgaard M, Ringholm L, Laugesen CS, Rasmussen KL, Damm P, Mathiesen ER. Pregnancy-induced sight-threatening diabetic retinopathy in women with Type 1 diabetes. Diabet Med. 2010;27:431–5.
Rahman W, Rahman FZ, Yassin S, Al-Suleiman SA, Rahman J. Progression of retinopathy during pregnancy in type 1 diabetes mellitus. Clin Exp Ophthalmol. 2007;35(3):231–6.
Matthews DR, Stratton IM, Aldington SJ, Holman RR, Kohner EM. Risks of progression of retinopathy and vision loss related to tight blood pressure control in type 2 diabetes mellitus—UKPDS 69. Arch Ophthalmol. 2004;122:1631–40.
Chan WC, Lim LT, Quinn MJ, Knox FA, McCance D, Best RM. Management and outcome of sight-threatening diabetic retinopathy in pregnancy. Eye. 2004;18:826–32.
The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Eng J Med. 1993;329:977–86.
The Diabetes Control and Complications Trial Research Group. Early worsening of diabetic retinopathy in the Diabetes Control and Complications Trial. Arch Ophthalmol. 1998;116:874–86.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
J. Toda, None; S. Kato, None; M. Sanaka, None; S. Kitano, None.
About this article
Cite this article
Toda, J., Kato, S., Sanaka, M. et al. The effect of pregnancy on the progression of diabetic retinopathy. Jpn J Ophthalmol 60, 454–458 (2016). https://doi.org/10.1007/s10384-016-0464-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-016-0464-y