Abstract
Purpose
To measure retinal nerve fiber layer thickness (RNFLT) and ganglion cell complex thickness (GCCT) in eyes with no light perception due to nonglaucomatous optic neuropathy using spectral-domain optical coherence tomography.
Methods
Fourteen eyes of 14 patients (9 women, 5 men; mean age 56.0 ± 16.6 (standard deviation) years] with no light perception due to optic neuropathy were recruited to this retrospective study. Only clinically stable eyes were included. Eyes were imaged at least 6 months after the onset of the disease. Five patients lost light perception due to traumatic optic neuropathy, four patients had ischemic optic neuropathy, two patients had optic neuritis, two patients had compressive optic neuropathy, and one patient had optic nerve atrophy. Global and quadrant RNFLTs were measured with the Cirrus HD-optical coherence tomography (OCT) system; global and hemisphere GCCTs were measured by spectral-domain OCT (RTVue OCT system). Only reliable OCT images were used for further analysis.
Results
Reliable RNFL images were obtained in 12 eyes, and reliable GCC images were obtained in 11 eyes. Global, superior, temporal, inferior, and nasal RNFLT were 57.5 ± 6.7, 60.6 ± 7.6, 54.1 ± 11.2, 59.7 ± 9.5, and 55.6 ± 7.4 µm, respectively. Global, superior, and inferior GCC thicknesses were 68.8 ± 9.6, 70.7 ± 12.2, and 67.8 ± 8.8 µm, respectively.
Conclusions
A considerable proportion of RNFL and GCC remained in eyes with no light perception vision. Clinicians should take this into account when evaluating the severity of optic neuropathy from OCT-measured RNFLT and GCCT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The current standard diagnosis of optic nerve disorders such as glaucoma is based on the presence of typical structural changes with corresponding functional deficits [1]. The measurement of parapapillary retinal nerve fiber layer thickness (RNFLT) with optical coherence tomography (OCT) has been widely used to evaluate structural damage and shown to be a useful, noninvasive, and quantitative alternative marker of optic nerve disorders [2]. Shihota et al. reported the association between RNFLT values measured with OCT and severity of glaucomatous visual field damage (VFD) [3]. However, a number of published studies have found a less than perfect correspondence between structural glaucomatous damage measured with OCT and functional damage measured with VF testing [4–6].
One possible reason for the poor agreement between the structural and functional measures is the floor effect; that is, the minimal value of RNFLT beyond which the RNFLT cannot be reduced even in cases with perfect loss of retinal ganglion cell axons [4, 6–9]. This residual RNFL may consist of a few resistant retinal ganglion cells and nonneuronal components contained in the RNFL, such as blood vessels and glial cells [10, 11]. The residual thickness is an important value for relating structural measures to functional measures, as well as for determining the stage of glaucoma based on structural measures. Several studies have investigated the residual RNFLT [3, 8, 12, 13], but most of these used time-domain OCT (TD-OCT). The newer generation of OCT systems, such as spectral-domain OCT (SD-OCT), is characterized by a vastly improved the scan speed and resolution relative to conventional TD-OCT systems [14–16]. Establishing residual RNFLT measured with SD-OCT is essential for using the SD-OCT device as a structural measure of optic nerve damage because RNFLT values measured with TD-OCT and SD-OCT are not interchangeable [17]. However, there is a paucity of research on residual RNFLT measured with SD-OCT.
In addition to parapapillary RNFLT values, macular ganglion cell complex (GCC) thickness values that can be measured with SD-OCT are also used to assess structural damage of retinal ganglion cells and retinal nerve fibers [18–20]. It is to be expected that there should also be a floor effect for the GCC because the GCC consists of three retinal layers in the macular region: the nerve fiber layer (NFL), the ganglion cell layer (GCL), and the inner plexiform layer (IPL). However, research on the residual GCC thickness has not yet become available.
In this study, we imaged parapapillary RNFL and macular GCC in eyes with no light perception due to nonglaucomatous stable optic neuropathy with SD-OCT to determine the residual thicknesses of these layers.
Patients and methods
The medical records of consecutive patients with nonglaucomatous optic neuropathy who underwent OCT imaging between September 2010 and December 2014 were retrospectively reviewed. All patients who met the eligibility criteria in either eye were enrolled in the study. Patients with no light perception vision on repeatable (at least 2 consecutive) tests were included if the OCT images were taken at least 6 months after the onset of the disease. Parapapillary RNFL images were scanned with a Cirrus HD OCT system (Carl Zeiss Meditec, Dublin, CA), whereas macular GCC images were taken with an RTVue OCT system (Optoview, Fremont, CA). OCT images were reviewed by an ophthalmologist (AM) who was masked to the patient’s clinical information. Images with noncentered scans, inaccurate segmentation of the RNFL, or a low signal strength index (<6 for Cirrus HD OCT, <40 for RTVue) were excluded from the analysis. Patients with clinical evidence of ocular hypertension, other retinal diseases, inflammation, or edema were also excluded. The clinical data of the eligible patients were collected from the medical charts. These data included age, sex, types of optic neuropathy, intraocular pressure, laterality, and date of onset. This study was approved by the institutional review board of Osaka University Hospital.
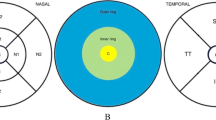
A 6 × 6-mm optic disc cube scan was obtained by Cirrus HD-OCT. The average and quadrant parapapillary RNFL thicknesses on a 3.46-mm-diameter circle were provided by the system’s software. A 7 × 7-mm-square grid scan of the central macula was obtained with the RTVue OCT system. Average and superior and inferior half GCC thickness values were calculated with the system’s software.
Descriptive statistics, including the mean and standard deviation (SD) of the participants’ characteristics and OCT parameters were computed. RNFLT values, both globally and for each sector, as well as GCC thickness values were statistically compared. The correlation between age and OCT parameters were statistically evaluated, as was the correlation between RNFLT and GCC thickness.
Statistical analyses were performed using the statistical programming language R ® Foundation for Statistical Computing, Vienna, Austria).
Results
Thirty eyes of 26 patients fulfilled the eligibility criteria. Of these, 16 eyes of 12 patients were excluded due to poor image quality or poor fixation. Therefore, data from 14 eyes of 14 patients (9 women, 5 men) were used in the analysis. The mean ± SD of the participants’ age was 56.0 ± 16.6 years. These patients had lost light perception because of traumatic optic neuropathy (5 eyes), ischemic optic neuropathy (5 eyes), optic neuritis (2 eyes), and compressive optic neuropathy (2 eyes). The clinical characteristics of the included eyes are summarized in Table 1.
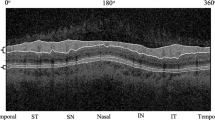
Reliable parapapillary RNFL measurements were obtained in 12 eyes. The mean global RNFLT was 58.1 ± 7.7 µm (Fig. 1). No significant difference was found among the global RNFLT and that of each quadrant (P = 0.6085; Table 2). Reliable GCC measurements were obtained in 11 eyes. The mean average GCC thickness was 65.7 ± 10.2 µm. No significant difference was found among the average, superior half, and inferior half GCC thickness values (P = 0.7889; Table 2).
Images of a representative case. Right eye of a 29-year-old man who had lost light perception owing to traumatic optic neuropathy. Images were taken 218 days after the onset of trauma. a Fundus photograph showing a pale optic disc with no apparent sign of inflammation or edema. b Parapapillary circle scan image showing diffuse loss of the retinal nerve fiber layer (RNFL) in the right eye (left panel) compared to the intact left eye (right panel). Temporal (TEMP)–Superior (SUP)–Nasal (NAS)–Inferior (INF)–Temporal (TEMP) (TSNIT) graph of the affected eye (center panel) showing a flat pattern of the RNFL with no regional difference in thickness. c Macular cube scan image showing diffuse thinning of the ganglion cell complex (GCC) layer
Neither the residual global RNFL thickness nor the GCC thickness significantly correlated with age (P = 0.373 and 0.131, respectively). The global RNFL thickness did not correlate significantly with the average GCC thickness (P = 0.6925).
Discussion
In this study, we found that our patients retained a considerable proportion of both the RNFL and GCC, even in eyes with no light perception due to old and stable optic neuropathy. This finding is in line with previous histological [10, 11], experimental [21], and in vivo imaging investigations [3, 4, 6–9, 12, 13]. No significant regional difference was found in the residual thickness values of the RNFL and GCC. Residual RNFLT values measured with TD-OCT have been reported in several published studies [3, 8, 12]. The residual RNFLTs measured with SD-OCT in our study were generally thicker than previously reported residual RNFL values measured with TD-OCT. Several studies have reported that RNFLT values measured with different OCT instruments were not interchangeable [17, 22–25]. It is possible that the higher residual RNFLT measurements obtained with SD-OCT systems may be due to the higher resolution and higher scan speed of these systems compared with TD-OCT systems. These properties could result in the detection of very thin retinal layers with SD-OCT that are difficult to detect with TD-OCT. Another possible explanation for the inconsistent measurements between SD-OCT and TD-OCT is the difference in the levels of image smoothing. However, the authors of one published study obtained conflicting results in which the residual RNFLT values measured with SD-OCT were thinner than those measured with TD-OCT [13]. This result may be due to differences in the participant populations, including ethnicity, type of optic neuropathy, and duration of the disease, among the studies. In addition, it is possible that the differences in the SD-OCT instrument used in these studies [Spectralis (Carl Zeiss Meditec) in the previous study, Cirrus in this study] explain the inconsistency. It is understandable that residual RNFL thickness should also be variable among different populations and among different devices. Clinicians should be aware of the residual RNFLT values of their own patient population measured with the OCT device that they are using so as to be able to accurately evaluate the level of glaucomatous structural damage.
In addition to parapapillary RNFLT measurements, macular GCC thickness measurements have been increasingly used in glaucoma practice. The GCC is a combination of the three innermost retinal layers: the NFL, GCL, and IPL. All three layers are affected by glaucoma, and the outer border of the IPL can be relatively easily detected [18]. Therefore, the GCC is commonly used as a parameter for glaucomatous macular damage, and it is critically important to determine the residual thickness of GCC. The residual thickness profile of the GCC may be different from that of parapapillary RNFL because the thickness distributions of the three layers involved in the GCC are quite different from each other [20]. The vulnerability to glaucomatous damage should also be different among these layers. However, no reports have yet been published on the residual thickness of the GCC in human eyes. In our study, we found that a considerable proportion of the GCC also remains in eyes without light perception. When interpreting the measured thickness of GCC in practice, clinicians should also keep in mind that the floor effect also exists for the GCC.
Among the eyes of our patients, both the residual RNFL and GCC thickness values showed significant variability. This finding is in agreement with the results of previous investigations that also showed significant variability in residual RNFLT [3, 12, 13]. Several factors may explain this variability in the residual RNFL and GCC thicknesses. It is well known that there is significant variability in the RNFL and GCC thicknesses of normal eyes [19, 26]. In addition, the vascular component of RNFL has recently been shown to decrease with progression of neuropathy in glaucomatous eyes. Variability may also exist in the thicknesses of the nonneuronal tissues in RNFL and GCC. However, further research is required to clarify more precisely the factors which contribute to residual thickness variability in the RNFL and GCC.
Normal RNFL thickness declines with age [27–34]. We investigated the correlation between age and residual RNFLT in our patients but found no obvious age-related decline in residual RNFLT, possibly indicating that nonneuronal tissues in the RNFL are not as susceptible to age-related damage as the retinal nerve fiber. However, further research is warranted to clarify this issue. Another feature of normal RNFLT is the regional difference: the RNFL is thicker in the inferior and superior quadrants and thinner in the nasal and temporal quadrants [26]. We did not observe any obvious regional difference in residual RNFLT in the eyes of our patients.
There are a number of limitations to our study. First, it was a retrospective study. Secondly, the small number of participants could limit the power to evaluate the effects of each parameter on the residual thicknesses. In addition, the participants were limited to a Japanese population. Both factors limit the direct extrapolation of these results of this study to other populations. Thirdly, as the pattern of optic nerve damage differs among different types of optic neuropathy [35], a difference in residual thickness might exist among the variable pathologies affecting the optic nerve. As a result, it is uncertain whether we can apply the results of this study to other types of optic neuropathy, such as glaucoma. A large-scale, prospective study including various disease types and various populations with an appropriate number of participants to allow subgroup analyses may be the ideal strategy. Such an undertaking, however, will be difficult because the population of patients with no light perception without any other disease or any history of treatments that would influence the measurements is generally small for each particular disease type.
In summary, The RNFL and GCC in the eyes of our patients which had lost light perception due to optic neuropathy retained a considerable thicknesses as measured with SD-OCT. A significant variability was found in residual RNFL and GCC thickness. No obvious regional difference or obvious influence of age was found in the residual thickness values. These results should be considered when clinicians interpret RNFLT and GCC thickness values to evaluate the severity of optic neuropathy.
References
Weinreb RN, Khaw PT. Primary open-angle glaucoma. Lancet. 2004;363:1711–20.
Gabriele ML, Wollstein G, Ishikawa H, Xu J, Kim J, Kagemann L, et al. Three dimensional optical coherence tomography imaging: advantages and advances. Prog Retin Eye Res. 2011;29:556–79.
Sihota R, Sony P, Gupta V, Dada T, Singh R. Diagnostic capability of optical coherence tomography in evaluating the degree of glaucomatous retinal nerve fiber damage. Invest Ophthalmol Vis Sci. 2006;47:2006–10.
Hood DC, Kardon RH. A framework for comparing structural and functional measures of glaucomatous damage. Prog Retin Eye Res. 2007;26:688–710.
Leung CK, Chong KK-L, Chan W, Yiu CK-F, Tso M, Woo J, et al. Comparative study of retinal nerve fiber layer measurement by Stratus OCT and GDx VCC, II: structure/function regression analysis in glaucoma. Invest Ophthalmol Vis Sci. 2005;46:3702–11.
Medeiros FA, Zangwill L, Bowd C, Mansouri K, Weinreb RN. The structure and function relationship in glaucoma: implications for detection of progression and measurement of rates of change. Invest Ophthalmol Vis Sci. 2012;53:6939–46.
Harwerth RS, Wheat JL, Fredette MJ, Anderson DR. Linking structure and function in glaucoma. Prog Retin Eye Res. 2010;29:249–71.
Hood DC, Anderson S, Rouleau J, Wenick AS, Grover LK, Behrens MM, et al. Retinal nerve fiber structure versus visual field function in patients with ischemic optic neuropathy: a test of a linear model. Ophthalmology. 2008;115:904–10.
Kanamori A, Nakamura M, Yamada Y, Negi A. Longitudinal study of retinal nerve fiber layer thickness and ganglion cell complex in traumatic optic neuropathy. Arch Ophthalmol. 2012;130:1067–9.
Pavlidis M, Stupp T, Nascar R, Cengiz C, Thanos S. Retinal ganglion cells resistant to advanced glaucoma: a postmortem study of human retinas with the carbocyanine dye DiI. Invest Ophthalmol Vis Sci. 2003;44:5196–205.
Radius RL, Anderson DR. The histology of retinal nerve fiber layer bundles and bundle defects. Arch Ophthalmol. 1979;97:948–50.
Chan CKM, Miller NR. Peripapillary nerve fiber layer thickness measured by optical coherence tomography in patients with no light perception from long-standing nonglaucomatous optic neuropathies. J Neuroophthalmol. 2007;27:176–9.
Groth SL, Harrison A, Grajewski AL, Lee MS. Retinal nerve fiber layer thickness using spectral-domain optical coherence tomography in patients with no light perception secondary to optic atrophy. J Neuroophthalmol. 2013;33:37–9.
van Velthoven MEJ, Faber DJ, Verbraak FD, van Leeuwen TG, de Smet MD. Recent developments in optical coherence tomography for imaging the retina. Prog Retin Eye Res. 2007;26:57–77.
Kiernan DF, Mieler WF, Hariprasad SM. Spectral-domain optical coherence tomography: a comparison of modern high-resolution retinal imaging systems. Am J Ophthalmol. 2010;149:18–31.
Savini G, Carbonelli M, Barboni P. Spectral-domain optical coherence tomography for the diagnosis and follow-up of glaucoma. Curr Opin Ophthalmol. 2011;22:115–23.
Knight OJ, Chang RT, Feuer WJ, Budenz DL. Comparison of retinal nerve fiber layer measurements using time domain and spectral domain optical coherent tomography. Ophthalmology. 2009;116:1271–7.
Tan O, Li G, Lu AT-H, Varma R, Huang D. Mapping of macular substructures with optical coherence tomography for glaucoma diagnosis. Ophthalmology. 2008;115:949–56.
Tan O, Chopra V, Lu AT-H, Schuman JS, Ishikawa H, Wollstein G, et al. Detection of macular ganglion cell loss in glaucoma by Fourier-domain optical coherence tomography. Ophthalmology. 2009;116(2305–14):e1–2.
Hood DC, Raza AS, de Moraes CG, Liebmann JM, Ritch R. Glaucomatous damage of the macula. Prog Retin Eye Res. 2013;32:1–21.
Choe TE, Abbott CJ, Piper C, Wang L, Fortune B. Comparison of longitudinal in vivo measurements of retinal nerve fiber layer thickness and retinal ganglion cell density after optic nerve transection in rat. PLoS One. 2014;9:e113011.
Leung CK-S, Cheung CY-L, Weinreb RN, Qiu Q, Liu S, Li H, et al. Retinal nerve fiber layer imaging with spectral-domain optical coherence tomography: a variability and diagnostic performance study. Ophthalmology. 2009;116:1257–63.
Tan BB, Natividad M, Chua K-C, Yip LW. Comparison of retinal nerve fiber layer measurement between 2 spectral domain OCT instruments. J Glaucoma. 2012;21:266–73.
Akashi A, Kanamori A, Nakamura M, Fujihara M, Yamada Y, Negi A. Comparative assessment for the ability of Cirrus, RTVue, and 3D-OCT to diagnose glaucoma. Invest Ophthalmol Vis Sci. 2013;54:4478–84.
Sung KR, Kim DY, Park SB, Kook MS. Comparison of retinal nerve fiber layer thickness measured by Cirrus HD and Stratus optical coherence tomography. Ophthalmology. 2009;116:1264–70.
Seibold LK, Mandava N, Kahook MY. Comparison of retinal nerve fiber layer thickness in normal eyes using time-domain and spectral-domain optical coherence tomography. Am J Ophthalmol. 2010;150:807–14.
Balazsi AG, Rootman J, Drance SM, Schulzer M, Douglas GR. The effect of age on the nerve fiber population of the human optic nerve. Am J Ophthalmol. 1984;97:760–6.
Repka MX, Quigley HA. The effect of age on normal human optic nerve fiber number and diameter. Ophthalmology. 1989;96:26–32.
Poinoosawmy D, Fontana L, Wu JX, Fitzke FW, Hitchings RA. Variation of nerve fibre layer thickness measurements with age and ethnicity by scanning laser polarimetry. Br J Ophthalmol. 1997;81:350–4.
Funaki S, Shirakashi M, Funaki H, Yaoeda K, Abe H. Relationship between age and the thickness of the retinal nerve fiber layer in normal subjects. Jpn J Ophthalmol. 1999;43:180–5.
Alamouti B, Funk J. Retinal thickness decreases with age : an OCT study. Br J Ophthalmol. 2003;87:899–902.
Da Pozzo S, Iacono P, Marchesan R, Minutola D, Ravalico G. The effect of ageing on retinal nerve fibre layer thickness: an evaluation by scanning laser polarimetry with variable corneal compensation. Acta Ophthalmol Scand. 2006;84:375–9.
Hirasawa H, Tomidokoro A, Araie M, Konno S, Saito H, Iwase A, et al. Peripapillary retinal nerve fiber layer thickness determined by spectral-domain optical coherence tomography in ophthalmologically normal eyes. Arch Ophthalmol. 2010;128:1420–6.
Leung CK-S, Yu M, Weinreb RN, Ye C, Liu S, Lai G, et al. Retinal nerve fiber layer imaging with spectral-domain optical coherence tomography: a prospective analysis of age-related loss. Ophthalmology. 2012;119:731–7.
Danesh-Meyer HV, Yap J, Frampton C, Savino PJ. Differentiation of compressive from glaucomatous optic neuropathy with spectral-domain optical coherence tomography. Ophthalmology. 2014;121:1516–23.
Conflicts of interest
A. Miki, None; T. Endo, None; T. Morimoto, None; K. Matsushita, None; T. Fujikado, None; K. Nishida, None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Miki, A., Endo, T., Morimoto, T. et al. Retinal nerve fiber layer and ganglion cell complex thicknesses measured with spectral-domain optical coherence tomography in eyes with no light perception due to nonglaucomatous optic neuropathy. Jpn J Ophthalmol 59, 230–235 (2015). https://doi.org/10.1007/s10384-015-0386-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-015-0386-0