Summary
Congenital and acquired conditions presenting with leg length discrepancy, leg deformity or short stature are not only a challenge for paediatric orthopaedic surgeons in terms of treatment options but may also involve a number of medical specialties due to the complex clinical manifestations of the diseases. Various surgical treatment options are available for these rare genetic diseases, including bone lengthening and growth inhibition techniques for lower limb discrepancy, as well as guided growth and other surgical procedures for correction of angular deformities. Surgical techniques may be similar, but the treatment plans and specific multidisciplinary approaches may differ. The present report is focused on paediatric orthopaedic and multidisciplinary aspects of the treatment of rare bone diseases. We address the clinical presentation of these diseases, gait and surgical procedures for conditions such as achondroplasia, X‑linked hypophosphatemia and osteogenesis imperfecta. We also provide a short overview of other rare bone diseases.
Zusammenfassung
Angeborene und erworbene Erkrankungen mit Beinlängendifferenzen, Beindeformitäten oder Kleinwuchs stellen nicht nur eine Herausforderung für Kinderorthopäden dar, sondern können aufgrund der oft komplexen klinischen Manifestationen auch die Expertise verschiedener Fachgebiete erfordern. Verschiedene chirurgische Behandlungsoptionen stehen für diese seltenen Erkrankungen zur Verfügung, darunter Techniken zur Knochenverlängerung und Wachstumshemmung bei Längendiskrepanzen der unteren Extremitäten sowie Wachstumslenkung und invasivere chirurgische Verfahren zur Korrektur von Achsdeformitäten. Die verwendeten Operationstechniken werden entsprechend der knöchernen Deformität, nach Patientenalter, der Grunderkrankung und weiteren Faktoren gewählt. Diese seltenen Knochenerkrankungen verbindet jedoch die Notwendigkeit eines spezifischen multidisziplinären Behandlungsmodus. Die vorliegende Arbeit konzentriert sich auf pädiatrisch-orthopädische und multidisziplinäre Aspekte der Behandlung seltener Knochenerkrankungen. Klinische Manifestation, Gangbild und chirurgische Optionen bei Erkrankungen wie Achondroplasie, X‑chromosomaler Hypophosphatämie und Osteogenesis imperfecta werden dargestellt. Zusätzlich wird ein kurzer Überblick über weitere seltene Knochenerkrankungen gegeben, welche eines multidisziplinären Settings bedürfen.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Leg length discrepancy, leg deformity and short stature occur in a variety of congenital and acquired conditions. Congenital malformation, growth disturbance and local or general bone weakness/fragility are associated with various severity levels of long bone deformities. These conditions pose a challenge for paediatric orthopaedic surgeons in terms of treatment options, and also involve several medical specialties because of their complex clinical manifestations.
Leg length discrepancy of more than 2 cm is suspected to cause long-term pathologies, including back pain, lower extremity pain and degenerative conditions. Compensatory mechanisms impose strain on various parts of the spine and/or lower extremity, require exaggerated motion in these areas and may manifest as gait impairment [1].
Frontal lower limb deformity (valgus/varus) causing partial overload of the hip, knee and ankle, maltorsion of the lower limb, as well as sagittal deformity (procurvatum/recurvatum) may alter the range of motion of the joint and cause gait problems, pain, joint instability, overuse of soft tissue and osteoarthritis.
In paediatric patients, guided growth may serve as a less invasive alternative or an additional procedure to achieve optimal deformity correction. Epiphysiodesis is a minimally invasive option to obtain permanent results, which inhibits the longer extremity by percutaneous drilling/curettage and must therefore be well timed. Temporary hemiepiphysiodesis, a reversible surgical intervention, is achieved by the use of a tension band plate, staples or screws, and may be employed in younger patients because the physis can be untethered upon deformity correction. This intervention may be repeated if necessary and serves as a concept of serial guided growth for both angular deformity correction and deceleration of growth in the longer limb [2] (see Willegger et al., this issue).
External fixators have been used as the primary means of addressing limb deformity and limb length discrepancy because they permit simultaneous multiplanar deformity correction. Ilizarov perfected the concept of safe and efficient lengthening, suggesting a 5-day latency period after osteotomy as well as a distraction rate of 1 mm per day in four increments, thus activating bone metabolism and inducing bone regeneration [3]. Nowadays, hexapod circular external fixators are paired with a software program which guides surgeons through the process of deformity correction. This is especially useful for paediatric patients who present with concomitant angular and/or rotational lower leg deformities [4]. The surgeon must be thoroughly familiar with deformity analysis and correction in order to perform these procedures.
Intramedullary lengthening devices constitute a milestone in limb lengthening. Their advantages are manifold: a familiar surgical technique, controlled rate and rhythm of lengthening, and protection of deformation or fracture. The use of external fixators may be completely avoided in some cases while still providing rotational correction and angular correction by the use of blocking screws [4]. However, the use of nails for intramedullary lengthening nails is often complicated, sometimes rendered impossible in the patients described in the present report. The reasons are small or short bones, reduced bone quality/stability and/or severe deformity.
In addition to lengthening and deformity correction, preventive intramedullary stabilisation of paediatric bone is a frequently used approach. Surgical procedures vary depending on the patient’s age, local bone and growth plate status, the type of deformity, and underlying conditions. Implants used in these settings include K‑wires, static (special-sized paediatric) nails and telescopic nails.
Complication rates depend on many factors such as the type of surgery, deformity parameters and underlying medical conditions. Intensive postoperative follow-up is crucial for all of these surgical procedures.
The patient’s growth potential and bone quality as a result of the underlying medical condition, as well as the patient’s desired outcome, determine the choice of the surgical procedure and must be analysed individually. Although leg lengthening procedures are quite straightforward for a large majority of congenital lower limb discrepancies (LLD), some of these deformities are associated with syndromes that require a multidisciplinary or even multicentre approach for optimal patient care (see Walleczek et al., this issue). Achondroplasia, X‑linked hypophosphatemia and osteogenesis imperfecta are some of the diseases that call for a multidisciplinary approach in ambulatory, preoperative, perioperative and postoperative care. Although the aforementioned diseases differ regarding their underlying aetiology as well as associated conditions, they are similar in that their treatment requires close collaboration between various medical specialists.
Achondroplasia
Lower limb deformity/gait
Achondroplasia (ORPHA:15, OMIM #100800) is the most common form of congenital disproportionately short stature, associated with a prospective final height averaging about 132 cm in males and 124 cm in females. Pathognomic skeletal changes on radiographs and lower limb deformities such as varus knee or ankle deformities are common clinical manifestations. Other orthopaedic presentations include impaired gait due to intoeing, frequently occurring as a result of reduced external tibial torsion, genu recurvatum caused by a reduced tibial slope, and soft tissue hyperlaxity.
Furthermore, disease-specific gait deviations have been described in children [5] and adults [6] with achondroplasia. Short stature may cause limitations in activities of daily living and impair the patient’s quality of life [7].
Orthopaedic treatment: aims and options
Lower limb alignment is the main goal of treatment in the orthopaedic management of achondroplasia in children. Guided growth with temporary hemiepiphysiodesis may be used successfully for the treatment of a varus knee deformity. However, reduced growth potential must be considered because it requires early intervention. Reduced external tibial torsion (intoeing) and bony genu recurvatum (knee hyperextension) to a clinically relevant extent must be addressed by performing osteotomies. If bone lengthening is favoured, the aforementioned bone deformities can be corrected during lengthening surgery.
Despite the possibility of extensive bone lengthening due to soft tissue availability, proportions should be kept in mind. Proportioning may start at a younger age and be performed in stages. This allows the attainment of the final height of a short normal individual [7, 8].
Lengthening procedures can be performed by the use of a unilateral external fixator, a circular hexapod fixator (Fig. 1) or an intramedullary nail, which are nowadays gaining popularity.
In addition to distraction osteogenesis of the lower extremity, which is used to improve a patient’s quality of life and functional outcome, humeral lengthening is employed in some cases of rhizomelia. Due to a disproportionally short humerus and the lack of elbow extension, basic activities of daily living such as anal hygiene may be impaired [9].
The lateral collateral ligament (LCL) is an important primary restraint to the knee joint against the varus moment during single-leg stance. In achondroplasia, laxity of the LCL is caused by overgrowth of the fibula in relation to the tibia and may lead to an additional dynamic varus deformity [10].
Intraoperative stability of bone is one of the positive aspects of achondroplasia. Bone healing typically occurs fast. However, premature bone healing during the lengthening procedure must be taken into account, especially in younger children.
Degenerative symptoms of the knee in adults with achondroplasia can be addressed with knee replacement. However, the surgeon should keep challenging technical details such as ligamentous balancing, intramedullary instrumentation as a result of varus deformities and substantial femoral bowing in mind [11].
Significant comorbidities and higher infection rates have been reported after joint replacement procedures in patients with musculoskeletal dysplasia [12].
Multidisciplinary approach
Patients with achondroplasia require a multidisciplinary approach, including preoperative discussions to determine the best perioperative strategy. The many challenging situations include the presence of a large head compared to a short neck, thickened vocal cords, spinal or foramen magnum stenosis and fragile articulation of the atlantoaxial joint. The latter might cause neurological deterioration due to spinal cord injury during intubation and positioning for surgery. Recommendations for anaesthesia in achondroplasia have been published online (https://www.orpha.net/data/patho/Ans/en/Achondroplasia.pdf). The prevalence of obstructive sleep apnoea limits the use of narcotics during surgery and requires close postoperative observation [13].
Achondroplasia is associated with a high predisposition to obesity. Obesity in patients with achondroplasia is believed to aggravate complications such as joint pain, leg deformities and increased lumbar canal stenosis, which may cause neurological and orthopaedic problems. Furthermore, a risk and deterioration of sleep apnoea and early cardiovascular mortality have been reported [14].
Children with achondroplasia should undergo yearly physical examinations at specialised centres. The investigations must include growth assessment based on specific percentiles for height, weight and head circumference.
X-linked hypophosphatemia
Lower limb deformity/gait
X‑linked hypophosphatemia (XLH; ORPHA: 89936, OMIM #307800) is a congenital disease caused by loss of function of the phosphate-regulating gene, with homology to endopeptidases on the X chromosome (PHEX), resulting in a dysregulation of fibroblast-like growth factor 23 (FGF23). This dysregulation is associated with increased systemic levels, which induce chronic renal phosphate wasting and impaired activation of 25(OH) vitamin D [15] (see Raimann et al., this issue).
Orthopaedic problems of the lower limb are quite common in children and adults and worsen quality of life in patients with XLH. Musculoskeletal symptoms, reduced growth potential, insufficient bone quality and a high recurrence rate of bone deformities are frequent challenges in the paediatric orthopaedic treatment of XLH. Lower limb malalignment is associated with decreased quality of life. These patients frequently present with a valgus or varus deformity as well as increased external torsion of the femur and reduced external torsion of the tibia/fibula.
Deformities of the lower limb contribute significantly to the burden of disease [16] and are associated with gait impairment [17].
In adults, musculoskeletal pain, lower limb deformity, chronic pseudofractures, reduced joint range of motion, gait deviations, enthesopathies and early osteoarthritis may contribute to the burden of disease [15, 16, 18].
Orthopaedic treatment: aims and options
Children with lower limb deformities should undergo yearly clinical examinations at paediatric orthopaedic centres. Radiographic assessment is advisable in patients with axis deviation or a reduced joint range of motion.
Common paediatric orthopaedic surgical procedures such as guided growth may be used for deformity correction in children with XLH. However, reduced growth potential, incomplete correction and higher recurrence rates are some of the obstacles faced by surgeons in this setting [2].
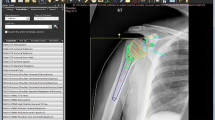
In contrast to other types of skeletal dysplasia, XLH is accompanied by a mild shortening of stature. Therefore, deformity correction of lower limbs is given preference over leg lengthening procedures to improve quality of life. Patients with severe lower limb deformities may require complex correction with multilevel osteotomies and the use of external fixators. Chronic pseudofractures of the lower limbs are common in adults and can be addressed by performing deformity correction with intramedullary stabilisation (Fig. 2a, b).
28-year-old man with X‑linked hypophosphatemia with procurvatum deformity and painful chronic pseudofractures in both femurs after several prior surgeries (a). Deformity correction was achieved by performing an osteotomy and stabilisation with a femoral nail (Expert LFN, DePuy Synthes, Warsaw, USA). Recon screws and an angular stable locking system (ASLS, DePuy Synthes, Warsaw, USA) were used to address weak bone and prevent hardware migration and instability (b, c)
Bone quality may be a challenging issue in patients with XLH. Weak areas of bone and local alterations in bone quality due to prior surgeries may impede osteotomy and osteosynthesis. Close postoperative radiographic monitoring is advised to ensure early detection of complications such as failure of hardware or lack of stabilisation.
In adults with osteoarthritis, adequate limb alignment is crucial for joint replacement surgery. Severe varus or valgus deformities reduce the success rate and implant survival of total knee replacement surgery [19]. In severe cases, bone deformity must be addressed by alignment surgery prior to joint replacement.
Multidisciplinary approach
Multidisciplinary treatment should be established in early infancy because it ensures a better outcome, improves quality of life and reduces the burden of disease. In addition to lower limb deformities, patients with XLH present with a variety of other symptoms which may impair their quality of life as well as social function. Supplementation of phosphate and active vitamin D is believed to reduce musculoskeletal symptoms, including musculoskeletal pain/weakness or joint pain, and lessen lower limb deformity. Supplementation may even prevent deformities and reduce the risk of osteoarthritis. Optimisation of the patient’s growth potential by appropriate metabolic control is especially important in the preoperative setting; increased growth signifies a higher potential for guided growth. Furthermore, adequate supplementation is believed to accelerate bone healing and reduce pseudarthrosis rates.
Therefore, despite side effects such as hyperparathyroidism or nephrocalcinosis, paediatric bone specialists recommend the start of medical treatment in early childhood in order to improve quality of life and optimise surgical orthopaedic care in patients with XLH [15].
Alongside the conventional treatment option of phosphate and vitamin D supplementation, a new treatment option is available for patients with XLH (see Kocijan et al., this issue). Burosumab is a monoclonal antibody that directly binds FGF23 and targets the main pathomechanism of XLH. Treatment with burosumab was found to enhance growth in children [20]. However, the efficacy of burosumab in reducing lower limb deformity is still uncertain. Long-term studies are needed to verify its effects.
Fracture/osteotomy healing, pseudofracture rates, pain, joint stiffness and physical function are the main orthopaedic outcome parameters when using burosumab for the treatment of adults.
In rare cases, patients with increased intracranial pressure or craniosynostosis due to dysregulated ossification may require neurological or neurosurgical assessment.
Despite optimal dental care, endodontic infections may occur in early childhood due to dentin hypomineralisation. Therefore, patients of all ages with XLH should undergo regular dental care [15].
Osteogenesis imperfecta
Lower limb deformity/gait
Osteogenesis imperfecta (OI; ORPHA: 666, OMIM: 166200 166210 166220 166230 259420 259440 610682) is a congenital systemic connective tissue disorder and may be classified into different types depending on the severity of the phenotype. Clinical characteristics include osteopenia, short stature, fragile bones and progressive skeletal deformities. Some cases may be associated with joint laxity, blue sclera, dentinogenesis imperfecta or deafness [21]. The mildest and most common form is OI type I. Limited mobility may be associated with recurrent fractures, muscle weakness, ligament laxity and normal to slightly short stature.
Gait deviations such as reduced walking speed, single support time, stride and step length, as well as increased external hip rotation have been reported [22].
Orthopaedic treatment: aims and options
The aims of surgery vary according to the type of OI. In mild to moderate disease, the goal is to achieve normal gait. In severe disease, the main purpose is to avoid fractures and stabilise weak bones. Intramedullary devices with elongating capacities, such as telescoping rods (Fig. 3), or flexible intramedullary nails are used to enhance the biomechanical load-bearing capacity of bone for verticalisation and walking. In younger patients, simple K‑wires or Rush rods are used to provide fracture protection if the medullary canal is too small for the aforementioned devices. However, these require additional surgery later in life because the protective effect is limited by the length of the implant. Secondary deformities above and below the implanted devices may occur during the growth period. Other disease-related complications and the need for surgical revisions may be attributed to poor bone quality. Such complications include loss of fixation of the distal and proximal anchorage of intramedullary devices, migration of fixating hardware, secondary deformities, bending of nails and delayed consolidation of osteotomies [23].
Telescopic nail (Fassier Duval, Pega Medical, Laval, Canada) in a femur of a 6-year-old girl with osteogenesis imperfecta (type 1). The telescope mechanism is superior to simple nails or rods in preventing fractures over a longer period of time during growth. Note: Deep trochanteric placement of the female part due to multiple prior surgeries
Severe osteoarthritis due to deformities and posttraumatic changes is a frequent phenomenon in adults with OI. Joint replacement and deformity correction are challenging approaches in adults because of the risk of severe bowing, maltorsion and extensive prior surgeries. High complication rates, iatrogenic perioperative fractures, the need for constrained implants and high rates of implant loosening are obstacles in postoperative patient care [24].
Multidisciplinary approach
Osteogenesis imperfecta is best treated by a multidisciplinary approach. Drug therapy, ideally instituted by a paediatric bone specialist, includes intravenous administration of bisphosphonates to reduce fracture rates. Vitamin D and calcium supplements are prescribed to ensure adequate levels. Anaesthesia recommendations for osteogenesis imperfecta are available online (https://www.orpha.net/data/patho/Ans/en/Osteogenesis-imperfecta.pdf). Physical rehabilitation is focused on muscle strength and joint range of motion. Rehabilitation permits the preservation of function and physical independence in patients with severe OI, thus enabling self-care, transfer and domestic skills. Patients with mild OI maintain their physical function at a very high level; the sole prohibited activity is contact sports. Regular follow-up examinations are recommended in order to prevent scoliosis, impairment of pulmonary function and cardiac manifestations. Auditory tests should be started in early childhood because OI is associated with adult-onset hearing loss. Neurosurgical assessments might be necessary in patients with abnormalities of the skull base, such as platybasia, basilar invagination or basilar impression [21].
Other rare bone diseases
Congenital longitudinal deficiency of the lower limb, such as congenital femoral deficiency (CFD) may present with or without fibular hemimelia (FH; ORPHA:93323). Tibial hemimelia (TH; ORPHA:93322, OMIM: 275220) is another rare bone disease. These rare conditions are commonly addressed by bone lengthening and deformity correction in mild to severe cases. Multidisciplinary assessment and care may not be necessary in an otherwise healthy child. However, a multidisciplinary and multicentre approach may be needed when the conditions are associated with other severe syndromes.
Congenital pseudarthrosis of the tibia (CPT; ORPHA:295018), commonly associated with neurofibromatosis (ORPHA:636, ORPHA:637), is the most frequently observed type of congenital pseudarthrosis and may present with fibular abnormalities. This condition, if associated with neurofibromatosis, poses a challenge for the paediatric orthopaedic surgeons as well as for interdisciplinary care. The treatment includes non-surgical treatment, such as orthosis, and surgical procedures ranging from bone grafting, intramedullary rod fixation, external fixators and bone transport to amputation. However, CPT is not the only manifestation that calls for intervention. Neurofibromatosis may be associated with other clinical conditions such as scoliosis, cardiovascular abnormalities including congenital heart disease, vasculopathy and hypertension, tumours of the nervous system and other tumours. These conditions obviously require a multidisciplinary approach.
Multiple hereditary exostosis (MHE; ORPHA:321) is characterised by the formation of non-malignant cartilage-capped bone tumours that cause painful impingement of surrounding soft tissue, impairment of the range of motion and, if occurring near growth plates, deformities of the lower or upper limb at several levels. A further cause for concern is the development of spinal osteochondromas. These conditions are clear indications for interdisciplinary treatment.
Rare syndromes such as hemihypertrophy, leg deformity, short stature or overgrowth also require an interdisciplinary approach. Proteus syndrome (PS; ORPHA:744) is associated with a higher risk of perioperative complications such as deep vein thrombosis or pulmonary embolism. Beckwith–Wiedemann syndrome (BWS; ORPHA:116) is a rare genetic disease characterised by the triad of exomphalos, macroglossia and overgrowth. Leg length discrepancy is commonly detected in early childhood in patients with BWS. The latter condition may also be associated with oral abnormalities, cardiac abnormalities, renal malformations, combined immunodeficiency and hypertension, neonatal hypoglycaemia and a high risk of malignant tumours in childhood.
Surgical treatment options for these rare genetic diseases include bone lengthening and growth inhibition techniques for lower limb discrepancies, as well as guided growth and deformity correction for angular deformities. While the surgical techniques used for the treatment of these conditions are similar, the treatment plan and the specific multidisciplinary approach may differ.
The optimal care of patients with rare bone diseases not only requires an interdisciplinary approach—such as that provided by the VBGC (Vienna Bone and Growth Center) with three centres, one each for paediatric bone disease (General Hospital Vienna, Medical University Vienna), adult osteology (Hanusch Hospital) and orthopaedic surgery focused on deformity correction (Orthopaedic Hospital Speising)—but also a local perioperative multidisciplinary setting of physiotherapists, psychologists, paediatricians, anaesthetists and paediatric orthopaedic surgeons.
References
Gordon JE, Davis LE. Leg Length Discrepancy: The Natural History (And What Do We Really Know). J Pediatr Orthop. 2019;39(6):S10–3.
Stevens PM, Klatt JB. Guided growth for pathological physes: radiographic improvement during realignment. J Pediatr Orthop. 2008;28(6):632–9.
Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res. 1990;250:8–26.
Iobst CA. New technologies in pediatric deformity correction. Orthop Clin North Am. 2019;50(1):77–85.
Inan M, Thacker M, Church C, Miller F, Mackenzie WG, Conklin D. Dynamic lower extremity alignment in children with achondroplasia. J Pediatr Orthop. 2006;26(4):526–9.
Sims DT, Burden A, Payton C, Onambélé-Pearson GL, Morse CI. A quantitative description of self-selected walking in adults with Achondroplasia using the gait profile score. Gait Posture. 2019;68:150–4.
Schiedel F, Rödl R. Lower limb lengthening in patients with disproportionate short stature with achondroplasia: a systematic review of the last 20 years. Disabil Rehabil. 2012;34(12):982–7.
Peretti G, Memeo A, Paronzini A, Marzorati S. Staged lengthening in the prevention of dwarfism in achondroplastic children: a preliminary report. J Pediatr Orthop B. 1995;4(1):58–64.
Ginebreda I, Campillo-Recio D, Cárdenas C, Tapiolas J, Rovira P, Isart A. Surgical technique and outcomes for bilateral humeral lengthening for achondroplasia: 26-year experience. Musculoskelet Surg. 2019;103(3):257–62.
Paley D, Bhatnagar J, Herzenberg JE, Bhave A. New procedures for tightening knee collateral ligaments in conjunction with knee realignment osteotomy. Orthop Clin North Am. 1994;25(3):533–55.
Kim RH, Scuderi GR, Dennis DA, Nakano SW. Technical challenges of total knee arthroplasty in skeletal dysplasia. Clin Orthop Relat Res. 2011;469(1):69–75.
Patel H, Cichos KH, Moon AS, McGwin G, Ponce BA, Ghanem ES. Patients with musculoskeletal dysplasia undergoing total joint arthroplasty are at increased risk of surgical site Infection. Orthop Traumatol Surg Res. 2019;105(7):1297–301.
Haldar R, Ambesh P, Kaushal A. Anesthesia for an achondroplastic individual with coexisting atlantoaxial dislocation. Anesth Essays Res. 2015;9(3):443.
Saint-Laurent C, Garde-Etayo L, Gouze E. Obesity in achondroplasia patients: from evidence to medical monitoring. Orphanet J Rare Dis. 2019;14(1):253.
Raimann A, Mindler GT, Kocijan R, Bekes K, Zwerina J, Haeusler G, et al. Multidisciplinary patient care in X‑linked hypophosphatemic rickets: one challenge, many perspectives. Wien Med Wochenschr. 2020;170(5-6):116–23.
Skrinar A, Dvorak-Ewell M, Evins A, Macica C, Linglart A, Imel EA, et al. The lifelong impact of X‑linked hypophosphatemia: results from a burden of disease survey. J Endocr Soc. 2019;3(7):1321–34.
Mindler GT, Kranzl A, Stauffer A, Haeusler G, Ganger R, Raimann A. Disease-specific gait deviations in pediatric patients with X‑linked hypophosphatemia. Gait Posture. 2020;81:78–84.
Steele A, Gonzalez R, Garbalosa JC, Steigbigel K, Grgurich T, Parisi EJ, et al. Osteoarthritis, osteophytes, and enthesophytes affect biomechanical function in adults with X‑linked hypophosphatemia. J Clin Endocrinol Metab. 2020;105(4):1798–814.
Mills ES, Iorio L, Feinn RS, Duignan KM, Macica CM. Joint replacement in X‑linked hypophosphatemia. J Orthop. 2019;16:55–60.
Imel EA, Glorieux FH, Whyte MP, Munns CF, Ward LM, Nilsson O, et al. Burosumab versus conventional therapy in children with X‑linked hypophosphataemia: a randomised, active-controlled, open-label, phase 3 trial. Lancet. 2019;393(10189):2416–27.
Forlino A, Marini JC. Osteogenesis imperfecta. Lancet. 2016;387(10028):1657–71.
Garman CR, Graf A, Krzak J, Caudill A, Smith P, Harris G. Gait deviations in children with osteogenesis Imperfecta type i. J Pediatr Orthop. 2019;39(8):e641–e6.
Wirth T. The orthopaedic management of long bone deformities in genetically and acquired generalized bone weakening conditions. J Child Orthop. 2019;13(1):12–21.
Roberts TT, Cepela DJ, Uhl RL, Lozman J. Orthopaedic considerations for the adult with osteogenesis imperfecta. J Am Acad Orthop Surg. 2016;24(5):298–308.
Author information
Authors and Affiliations
Contributions
All authors contributed to this review article. Gabriel T. Mindler and Rudolf Ganger had the idea for the article, Gabriel T. Mindler and Alexandra Stauffer performed the literature search and drafted the manuscript. Rudolf Ganger critically revised the work.
Corresponding author
Ethics declarations
Conflict of interest
G.T. Mindler and A. Stauffer declare that they have no competing interests. R. Ganger reports personal fees from Smith & Nephew Europe and personal fees from Nuvasive Inc., outside the submitted work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mindler, G.T., Stauffer, A. & Ganger, R. Leg lengthening and deformity correction in rare bone diseases: a multidisciplinary approach. Wien Med Wochenschr 171, 126–132 (2021). https://doi.org/10.1007/s10354-020-00805-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10354-020-00805-7