Summary
Dorsal pancreatic agenesis is a very rare pancreatic developmental anomaly resulting in missing corpus and cauda of the pancreas. Due to improvements and more widespread use of advanced radiological techniques like CT or MRI, the possibility of finding this disorder is growing. Thus, this rare congenital condition, as well as a pancreas divisum and pseudo-agenesis secondary to chronic pancreatitis, must be considered in the differential diagnosis. Although most of the patients seem to be asymptomatic, abdominal pain and pancreatitis may develop. Moreover, this entity should be known by the treating physician, as these patients are at a high risk of developing diabetes mellitus during their lifetime. Herein, we present the case of a 65-year-old woman with complete agenesis of the dorsal pancreas. The patient was hospitalized due to weight loss, abdominal discomfort, and diabetes mellitus type 2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The pancreas develops by ventral and dorsal endodermal buds. Agenesis of the dorsal pancreas is a very rare congenital disorder, resulting from a failure in the fetal development of the dorsal bud of the pancreas. Only a few cases of dorsal pancreatic agenesis have been reported. Although most of the patients are clinically asymptomatic, abdominal pain and cases of pancreatitis have been reported. In addition, the development of diabetes mellitus may be frequent [1].
We report on a 65-year-old female patient with an incidental finding of agenesis of the dorsal pancreas due to evaluation of insufficiently treatable diabetes mellitus type 2.
Case report
A 65-year-old female patient was hospitalized for treatment optimization of previously diagnosed diabetes mellitus type 2. The patient reported reduced appetite, light abdominal discomfort, and weight loss of 3 kg in the past 4 to 6 weeks. Regarding her diabetes, she was in regular outpatient control and was treated with a combination of sulfonylurea (gliclazide) and a DDP4 inhibitor (vildagliptin). There was reported intolerance of metformin because of diarrhea. The blood sugar level stayed unusually high under this therapy regime, although the patient seemed to be very compliant and followed dietary recommendations.
The initial laboratory findings showed a fasting blood sugar level of 218 mg/dL and an HBA1c (glycated haemoglobin) of 9.6% (81 mmol/mol). The other results were unremarkable. Diabetes-associated antibodies were not detectable, so we could rule out late autoimmune diabetes of adults (LADA).
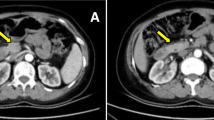
We recommended our patient to start with insulin therapy. Because of the reported weight loss, we performed several examinations to exclude a malignancy. Gastroscopy revealed Helicobacter pylori-associated gastritis. Colonoscopy showed an unremarkable normal colonic mucosa. Abdominal ultrasound showed small renal cysts, without any other pathological findings. The pancreas was not sufficiently describable, due to abdominal gas. Thus, an abdominal CT scan was performed, where the pancreatic corpus and cauda were not detectable (Fig. 1a, b). In a final MRI, the diagnosis of dorsal pancreas agenesis was made. The head of the pancreas showed a normal texture. There was no evidence for an exocrine insufficiency of the pancreas nor a concomitant malignant process or pancreatitis in the ventral fragment.
Discussion
Fetal development of the pancreas is characterized by formation of the tail, body, and upper part of the head, which are drained by the duct of Santorini, by the dorsal bud, while the major part of the head and uncinate process (drained by the Wirsung duct) are formed by the ventral bud [2, 3]. Complete agenesis of the pancreas is an extremely rare disorder with severe intrauterine growth retardation, permanent neonatal diabetes, and pancreatic exocrine dysfunction. High neonatal mortality is reported [4, 5].
Partial agenesis of the pancreas is slightly more frequently and, in this regard, dorsal agenesis is more common than ventral agenesis.
Since the first reports in the early years of the 20th century, around 100 cases have been published in total. Between the first description in 1911 by Kristian Axel Heiberg and 2008, a total number of 53 patients have been reported [6]. A systematic review published in 2016 identified 53 further consecutive patients, reported between 2008 and 2015, with agenesis of the dorsal pancreas [7].
Dorsal agenesis of the pancreas is a congenital malformation caused by a failure of the dorsal bud to form the corpus and cauda in the fetus [8]. Although most cases of dorsal agenesis of the pancreas are sporadic, there are reported associations with an autosomal-dominant mutation of the hepatocyte nuclear factor 1B (HNF1B) gene [9, 10].
Many patients with dorsal agenesis of the pancreas are asymptomatic, but up to 50% will develop insulin-dependent diabetes mellitus. The disease seems to be associated with an increased rate of epigastric pain, weight loss due to exocrine insufficiency, polysplenia, and pancreatitis or tumors of the ventral pancreas [2, 11, 12]. Due to improvements in radiological techniques, the possibility of finding this disorder is growing. Pancreas divisum and pseudo-agenesis secondary to chronic pancreatitis must be considered in the differential diagnosis.
A history of previous abdominal pain, former episodes of pancreatitis, CT scanning, and determination of serum lipase might be helpful in the differential diagnosis [13,14,15].
The therapeutic regimen is an individual decision depending on the clinical features of the single patient. At least regular control of blood sugar levels and HbA1c are necessary in asymptomatic patients. Usually, insulin therapy and substitution of pancreatic enzymes is all that is needed.
In our case, the diagnosis of dorsal agenesis of the pancreas was an incidental finding due to evaluation of insufficiently treatable diabetes type 2 with weight loss and mild abdominal discomfort.
In summary, this extremely rare congenital condition should be known by the treating physician when corpus and cauda of the pancreas cannot be visualized by routine examination, as these patients are at a high risk of developing diabetes mellitus during their lifetime, as in our patient.
References
Fukuoka K, et al. Complete agenesis of the dorsal pancreas. J Hepatobiliary Pancreat Surg. 1999;6(1):94–7.
Sakpal SV, Sexcius L, Babel N, Chamberlain RS. Agenesis of the dorsal pancreas and its association with pancreatic tumors. Pancreas. 2009;38(4):367–73.
Shih HP, Wang A, Sander M. Pancreas organogenesis: from lineage determination to morphogenesis. Annu Rev Cell Dev Biol. 2013;29(1):81–105.
Voldsgaard P, Kryger-Baggesen N, Lisse I. Agenesis of pancreas. Acta Paediatr. 1994;83(7):791–3.
Baumeister FAM, Engelsberger I, Schulze A. Pancreatic agenesis as cause for neonatal diabetes mellitus. Klin Padiatr. 2005;217:76–81.
Heiberg KA. Ein Fall von fehlender Cauda pancreatis (bei einem Diabetiker). Zentralbl Allg Pathol. 1911;22:676–7.
Cienfuegos JA, Rotellar F, Salguero J, Benito A, Solórzano JL, Sangro B. Agenesis of the dorsal pancreas: systematic review of a clinical challenge. Rev Esp Enferm Dig. 2016;108(8):479–84.
Joo YE, et al. Agenesis of the dorsal pancreas: a case report and review of the literature. Korean J Intern Med. 2006;21:236–9.
Wildling R, et al. Agenesis of the dorsal pancreas in a woman with diabetes mellitus and in both of her sons. Gastroenterology. 1993;104(4):1182–6.
Body-Bechou D, et al. TCF2/HNF-1beta mutations: 3 cases of fetal severe pancreatic agenesis or hypoplasia and multicystic renal dysplasia. Prenat Diagn. 2014;34(1):90–3.
Schnedl WJ, et al. Agenesis of the dorsal pancreas and associated diseases. Dig Dis Sci. 2009;54(3):481–7.
Sannappa RM, Buragohain J, Sarma D, Saikia UK, Choudhury BK. Agenesis of dorsal pancreas associated with periampullary pancreaticobiliary type adenocarcinoma. J Pancreas. 2014;15(5):489–92.
Gold RP. Agenesis and pseudo-agenesis of the dorsal pancreas. Abdom Imaging. 1993;18(2):141–4.
Balakrishnan V, Narayanan VA, Siyad I, Radhakrishnan L, Nair P. Agenesis of the dorsal pancreas with chronic calcific pancreatitis. Case report, review of the literature and genetic basis. J Pancreas. 2006;7(6):651–9.
Uygur-Bayramiçli O, Dabak R, Kiliçoglu G, Dolapçioglu C, Öztas D. Dorsal pancreatic agenesis. J Pancreas. 2007;8(4):450–2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
P. Dinkhauser, J. Paesold, D. Hubner, V. Steffan, R. Lampl, and H. Hofer declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dinkhauser, P., Paesold, J., Hubner, D. et al. Agenesis of the dorsal pancreas: a very rare entity causing diabetes mellitus. Wien Med Wochenschr 170, 168–170 (2020). https://doi.org/10.1007/s10354-019-00717-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10354-019-00717-1