Summary
Background
The purpose of this study was to financially profile four different types of elective colectomy resection in relation to diagnosis and complications.
Methods
A total of 1420 colectomies from three centers within our system were analyzed for diagnostic, complications, financial, length of stay (LOS), and case mix index (CMI) data for four procedure categories: colectomy above peritoneal reflection (AR) with diversion, colectomy AR without diversion, colectomy below peritoneal reflection (BR) with diversion, and colectomy BR without diversion. The incidence of complications and costs were compared between procedure groups. Logit models were used for probabilities of complications and Poisson for rate analysis.
Results
Elective colectomies AR were performed 72% of the time for non-inflammatory diagnoses (benign tumors, polyps, rectal prolapse, malignant tumors), whereas resections BR were performed 64% of the time for inflammatory diagnoses (diverticulitis, Crohn’s, ulcerative colitis, perforation, obstruction, sepsis, fistulae). Thus, diversion was performed in a higher proportion of cases with inflammatory diagnoses and cases requiring diversion had higher complication rates in both AR (16% vs. 5%) and BR (19% vs. 6%) resections.
Conclusion
Inflammatory diagnoses appear to drive the indication for diversion following elective colectomy. Colectomies with diversion have complication rates 1.36 times higher than without diversion, as well as excess LOS and costs. Resections AR with diversion had more than twice the proportion of complications as without diversion. Preoperative mitigation of inflammatory risk factors may decrease the rate of diversion and reduce complications, financial risk, and opportunity cost.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
-
Elective colectomies above the peritoneal reflection (AR) were performed 72% of the time for non-inflammatory diagnoses (benign tumors, polyps, rectal prolapse, malignant tumors), whereas resections below the peritoneal reflection (BR) were performed 64% of the time for inflammatory diagnoses (diverticulitis, Crohn’s, ulcerative colitis, perforation, obstruction, sepsis, fistulae).
-
Inflammatory diagnoses appear to drive the indication for diversion following elective colectomy.
-
Elective colectomies with diversion both above and below the peritoneal reflection have the highest complication rates and costs, with infectious complications being the most common.
-
Elective colectomies with diversion have complication rates 1.36 times higher than without diversion, as well as excess length of stay (LOS) and costs.
-
Preoperative mitigation of inflammatory risk factors may decrease the rate of diversion and reduce complications, financial risk, and opportunity cost.
Introduction
Colon resections are commonly performed procedures but are associated with high postoperative morbidity and mortality [1,2,3,4], and cases with one complication are more likely to have additional complications [5]. Although protocolized perioperative management [6] has led to some improved outcomes by decreasing the time to return of bowel function and length of stay (LOS), they have not been shown to change complication and readmission rates [7].
It has been established that hospitals incur financial penalties for postsurgical complications and that costs are substantially increased in hospitals with high complication rates [8]. In a retrospective study [9] by Eappen et al., 1067 colorectal resections were analyzed and found to have a 13.3% complication rate. Of note, the median LOS increased from 6 to 15 days, and the total margin (revenue minus variable and fixed costs) was shown to decrease by $ 6500 per patient in the setting of complication(s). In a study [10] by Govaert et al., hospital length of stay was shown to increase from 10.29 to 13.97 days in the case of minor complications and to 28.60 days in the case of major complications. Additionally. the cost of primary admission increased from € 7470 ($ 8920) without complications to € 9061 ($10,820) with minor complications and € 23,616 ($ 28,199) with major complications.
However, hospital accounting systems lack accurate complication and complication-dependent readmission data to accurately calculate the full economic impact of post-colectomy complications, and therefore, current financial systems underestimate the financial and opportunity risk profile of operative procedures. By accurately identifying the incidence of complications in specific types of colectomy and initiating quality interventions, financial and opportunity profiles may be improved. The purpose of this multi-institutional study was to financially profile different types of colectomy resections with and without complications using our concurrent complication recording platform. Colectomies above (AR) and below (BR) the peritoneal reflection with and without diversion were chosen because of their complexity, risk, and complication profiles. The financial and opportunity risk profile developed as a function of complication incidence may prove useful in designing quality improvement programs aimed at complication reduction. To our knowledge, these four groups of procedures have not been previously analyzed.
Methods
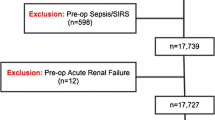
A total of 1420 elective colectomy cases were collected from three major medical centers within our 16-hospital health system between January 1, 2017, and December 31, 2019. ICD-10 codes were categorized into two diagnostic groups: elective resections for (1) inflammatory diagnoses: diverticulitis, Crohn’s, ulcerative colitis, obstruction, etc., and elective resections for (2) non-inflammatory diseases: benign disease (polyps, rectal prolapse) and malignant tumors. Administrative data were evaluated by secondary diagnosis codes for the number of colectomy cases with complications and the number of readmissions within 30 days, and compared to data from our concurrent complication reporting system. In addition, because secondary ICD-10 coding was not sufficiently detailed, we used a proprietary heuristic Natural Language Processing subsystem to further analyze surgical procedures based on a textual analysis of operative procedure descriptions in order to better define operative procedures as described below. Data from our concurrent complication reporting system (Morbidity & Mortality Adverse Event Reporting System, MARS; Outcome Management Systems, LLC, Greenwich, CT, USA) and cost-accounting (Sunrise Decision Support, Allscripts Healthcare, Chicago, IL, USA) systems were analyzed. Financial and LOS cost was evaluated in cases with and without complications in four elective procedure categories: colectomy above the peritoneal reflection (AR) with diversion, colectomy AR without diversion, colectomy below the peritoneal reflection (BR) with diversion, and colectomy BR without diversion. Diversion included both ileostomy and colostomy; however, 98% of diverted cases were either loop or end ileostomies. Ileostomy and colostomy closure cases were excluded from analysis. The incidence of complications for each group was evaluated.
We have previously reported on our concurrent MARS reporting system [11,12,13]. MARS was used to import heterogenous internal and external data sources (clinical EMR, surgical information system, administrative and financial data) into a single view for reporting on surgical activity. Operative data were linked to our concurrent adverse event reporting system within MARS by account number, and complications were identified for the index operation’s primary admission and any readmission within 30 days (Fig. 1). Only elective cases were included in the final dataset. All data were PHI protected and HIPAA compliant, and built on an SQL platform with data repositories maintained within a secured network protected by firewalls and a virtual private network (VPN).
Evaluation of financial and length of stay data
Financial data including adjusted net revenue, direct fixed costs, and contribution margins were evaluated in cases with and without postoperative complications. These cases were further divided into previously described categories as elective or emergency cases. Only elective cases were used for this study. Expense by accounting category was evaluated per case. The number and accuracy of complications reported from our concurrent reporting system was compared to administrative secondary diagnosis codes to assess the accurate identification of complications following colectomy, and to evaluate financial, CMI, and LOS impact.
The data were further examined to determine whether the probability of complications or the rate among those with complications depended on whether the operation was above or below PR, and whether there was or was not diversion. The analyses were done using the generalized linear models (GLM) procedure in R (R Core Team, R Foundation for Statistical Computing, Vienna, Austria). Models for probabilities of complication were analyzed as logit models, while rates were analyzed as Poisson models for the number of complications, using the logarithm of number of cases with complications as the offset.
This project was not a human subject study and was conducted under the umbrella of ongoing quality review. A “Human Subjects Research Determination Request” was filed with our IRB committee and IRB approval was not required.
Results
A total of 1420 elective colectomy cases were evaluated. The distribution of cases by diagnosis group is shown in Table 1. Elective colectomies AR were performed 72% of the time for non-inflammatory diagnoses (benign tumors, polyps, rectal prolapse, malignant tumors), whereas resections BR were performed 64% of the time for inflammatory diagnoses (diverticulitis, Crohn’s, ulcerative colitis, perforation, obstruction, sepsis, fistulae). Resections AR with diversion and BR with diversion were performed for inflammatory diagnoses 65 and 63% of the time, respectively. In contrast, resections BR without diversion were performed in 64% of cases for inflammatory diagnoses vs. 26% for AR resections without diversion. Thus, diversion was associated with predominantly inflammatory diagnoses and not with non-inflammatory diagnoses. Seven percent of all elective cases (99/1420; 7%) sustained complications. There were 278 total complications with an average of 2.81 (278/99) complications per case. When administrative secondary diagnosis data were compared to our concurrent complication reporting system, the number of complications reported in administrative data was only 38.5% of the number reported in our weekly concurrent reporting system. Therefore, our concurrent dataset was used. Complication data are summarized in Table 2.
Complications occurred in 8% (62/777) of elective resections BR compared to 6% (37/643) of resections AR, with an average of 3 vs. 2.49 complications per case, respectively. Resections requiring diversion had higher complication rates in both AR (16% vs. 5%) and BR (19% vs. 6%) resections (Table 2). The types of complications were grouped into five categories: infectious, readmission, hemorrhage, DVT/PE, and death. Infectious complications were predominant among the complication groups and were associated with diversion compared to without diversion (AR 27% vs. 4.1% and BR 31% vs. 5.1%; p < 0.00001; Table 3). Average case mix indices (CMI) among the groups were equivalent (Table 4). The models for probabilities of complications showed that these probabilities varied with both AR with diversion and BR with diversion, but there was no interaction. The model with main effects had a likelihood ratio chi-square of 0.52 with 1 df, which was not statistically significant. Operations BR (at each level of diversion) had about twice the proportion of complications as AR. Operations with diversion (both above and below the peritoneal reflection) had more than twice the proportion of complications as those without diversion. The models for rates of complications among those with complications showed that the rate of complication depended only on diversion. The model with only the effect of diversion fit extremely well: the deviance was 0.91 with 2 degrees of freedom. Operations with diversion had a rate of complications that was 1.36 times higher than operations without diversion. Thus, diversion was associated with predominantly inflammatory diagnoses, higher complication rates, and higher infectious rates in particular.
Detailed revenue and cost analyses for colectomy AR (with and without diversion) and BR (with and without diversion) are shown in Tables 5 and 6, respectively. AR and BR cases with complications demonstrated higher adjusted net revenues than AR and BR cases without complications and were between 29 and 47% higher in cases without diversion, respectively. Adjusted net revenues with diversion were substantially lower. Direct costs were between 50 and 77% higher for AR and BR procedures with complications and contribution margins for AR and BR cases with complications and with diversion were reduced from 50 to 78%. The LOS for all AR and BR cases with complications was increased from 62 to 108%, with the greatest excess LOS associated with AR resections with diversion. Similarly, ICU costs were from 80 to >200% higher for cases with complications, and generally, ICU costs, room and board, and labor accounted for the increased costs (Table 7). All category costs were ultimately related to the LOS. Cases with complications represent 5.5 and 18% of colectomy volume without and with diversion, respectively. However, complication-related hospital day utilization represents 10.6 and 28% of days, respectively, or 38.6% of total utilization (Table 8).
In summary, for the elective colectomy cases described, the increase in LOS and higher direct costs account for the negative financial and opportunity impact associated with colectomy complications. Cases with diversion both above and below the peritoneal reflection have the highst percentageof inflammatory diagnoses, highest complication rates and highest infection rates. Interestingly, the incidence of infection in BR without diversion is 5.7% compared to BR with diversion at 31%. Therefore, infection was a less common complication in this instance and the contribution margin was highest among the groups with complications. The mere occurrence of complications across all procedure types results in a 1.6–2.1-times increase in LOS. Resections AR with diversion had the highest excess LOS, percentage reduction in contribution margin, and more than twice the proportion of complications as those without diversion. Excess LOS is a measure of increased costs as an indicator of resource consumption related to room and board, ICU stay, labor, and supplies. Colectomies with or without diversion performed without complications all have positive contribution margins. However, contribution margins are significantly reduced for all colectomies with complications with the exception of BR without diversion. In this case, higher adjusted net revenues, lower direct costs, a lower excess LOS, and lower infectious complications may be responsible.
Since diversion appears to be an important factor impacting LOS and cost, we wondered whether operative approaches might be more often associated with diversion. Thus, we analyzed 2172 elective colectomies (Table 9) with respect to open vs. minimally invasive (MIS: laparoscopic/robotic) approaches. Odds ratio (OR) analysis confirms that resections AR have a greater likelihood of diversion than resections BR (OR: 3.5, p < 0.0001) and further, the difference between open and MIS procedures is larger for AR than for BR (OR: 4.07, p < 0.0005). Open procedures are done 82% of the time for AR with diversion and 57% of the time for BR with diversion. For both AR and BR without diversion, MIS procedures were used for 70–75% of cases. These data are consistent with the relationship between inflammatory diagnoses and diversion.
Discussion
The morbidity of colectomy complications includes financial, LOS, and opportunity costs to health systems as well as clinical morbidity to patients [10, 14,15,16,17]. However, hospital accounting systems lack accurate complication and complication-dependent readmission data to reliably calculate the full economic impact of post-colectomy complications. A recent study [18] suggests that administrative data are insufficient to directly identify or rule out individual-level complications. We have shown that administrative secondary diagnosis data accurately identified only 38% of those complications reported by our weekly complication reporting system and these data confirm that finding. Inaccurate identification of cases with complications would significantly underreport cost and LOS data. Inferences from administrative data should be viewed with caution and concurrent methods of complication reporting should be preferred.
Postoperative complications and, in particular, readmission, intra-abdominal abscess, return to the operating room, dehydration, and return to the interventional suite appear to be the most relevant associated with elective colectomy. Our data suggest that operations with diversion (both above and below the peritoneal reflection) were performed more often for inflammatory diagnoses and had more than twice the proportion of complications as those without diversion. In addition, open approaches are associated with a higher incidence of diversion than MIS approaches. Again, inflammatory diagnoses are associated with open approaches and diversion. The rate of complications depended only on diversion and operations with diversion had a rate of complications that was 1.36 times higher than operations without diversion. Operations BR (both with and without diversion) had about twice the proportion of complications as AR. AR and BR complication rates with diversion compared to without diversion are 0.43 vs. 0.13 and 0.74 vs. 0.13, with 2.67 vs. 2.45 and 4 vs. 2.32 complications per case, respectively (Table 10). In both AR and BR cases with and without diversion, diversion seems to benefit LOS and finances in cases without complications. In fact, patients without diversion who do not sustain complications have the lowest LOS (AR: 5.62 days and BR: 4.54 days), favorable contribution margins (AR: $ 14,404 and BR: $ 20,050), and lowest direct costs (AR: $ 18,722 and BR: $ 17,276).
The increase in LOS and direct costs is associated with decreased contribution margins following elective colectomy with complications. The LOS increase related to complications runs from 77 to 106.5% over cases without complications. The total LOS cost of the 37 AR cases with complications is 509.1 extra days of hospital stay. The total LOS cost of the 62 BR cases with complications is 707 extra days of hospital stay. The number of potential uncomplicated opportunity patients is calculated by dividing the excess days by the uncomplicated LOS for each group, or AR: 509.1/5.62 = 90.6 patients and BR: 707/13.55 = 52.2 patients; total = 142.2 patients. The reduction in cost by eliminating cases with complications and the increased revenue associated by backfilling with uncomplicated cases is calculated from the average reduction in contribution margin ($ 8300 per complication case x 99) and the revenue of performing uncomplicated opportunity cases ($ 18,860 x 142.2). In this case, the total opportunity cost of complications equates to approximately $ 3.5 million dollars ($ 821,700 + $ 2,681,892). LOS is directly related to opportunity cost with a total LOS excess of 6.24 days in colectomies AR and 5.01 days in colectomies BR. If complications could be avoided, more elective cases without complications could be performed. For every one readmission or complication with increased length of primary stay, close to two elective cases without complications (and the associated increased revenue) could be admitted, treated, and discharged.
Clearly this is a multifactorial issue and, although focused on elective colectomy, represents selection bias based on diagnosis, patient factors related to the risk of safe anastomosis, and other comorbid conditions. As such, our results are descriptive of patient risk rather than predictive. Nonetheless, there are distinct differences in diagnostic codes and complication incidence among the types of colectomy evaluated. Diversion alone is related to inflammatory diagnoses, increased complication rates, LOS, and cost, and the rate of complication depended only on diversion. Diversion AR has the highest excess LOS, percentage reduction in contribution margin, and more than twice the proportion of infectious complications as those without diversion. Operations with diversion had a rate of complications that was 1.36 times higher than operations without diversion. Paradoxically, resections BR without diversion and with complications had the lowest excess LOS. However, we have shown that infectious complications were 26% less frequent in BR without diversion, potentially accounting for the reduced LOS.
There are a number of reasons to consider diversion during colectomy and reducing the risk of anastomotic leak [19, 20] and infectious sequelae is a primary consideration. In a Cochrane review of ileostomy and colostomy in the setting of anterior resection for rectal carcinoma, diversion led to significantly decreased anastomotic leaks and urgent reoperations [21]. Of note, however, there was no change in 30-day or long-term mortality. Risk scores can be used to predict which patients are at increased risk for leak and may benefit from diversion [22]. Based on the data presented, future quality studies may best be focused on elective resections for inflammatory diagnosis codes and be designed to thoroughly evaluate the multivariate risk factors associated with anastomotic integrity, source control, adequacy of bowel preparation, antibiotic coverage, efficacy of diversion and drainage, and the resulting potential for infectious complications prompting diversion. Preoperative mitigation of inflammatory risk factors may decrease the rate of diversion and increase the rate of minimally invasive surgical approaches.
There are limitations to this study. These data only include cases within 30 days of readmission. It is likely that follow-up to at least 90 days or 120 days is more appropriate for a truly accurate accounting of increased cost, especially considering that many postoperative complications after colectomy occur after the time of discharge [23]. Similar to a limitation identified among studies of surgical site infections in a 2014 study [24] by Keenan et al., there is heterogeneity in the types of complications included in our study. Healy et al. [15] illustrated that financial data vary significantly by complication type. It could be useful to continue data collection and stratify our data by complication severity and/or type. Additionally, we could analyze complications identified during primary admission and compare these complications with those identified at time of readmission. The study is also limited by the range of different operations included. We addressed this by dividing the study up into AR and BR cases with and without diversion, which allowed us to break the study population down into four categories. In addition, categorizing procedures based on diagnostic indication has helped clarify the clinical situations most at risk for diversion. Findings were similar across categories with increased LOS in the setting of complications based on indication for surgery.
Conclusion
In summary, for the elective colectomy cases studied, excess LOS and higher direct costs and complication rates account for the negative financial and opportunity impact associated with resections. Cases with diversion both above and below the peritoneal reflection have the highest complication rates and costs, with infectious complications being the most common. Cases with diversion are also most often performed for inflammatory diagnosis indications. Resections AR with diversion had the highest percentage of inflammatory diagnoses, highest excess LOS and percentage reduction in contribution margin, and more than twice the proportion of complications as those without diversion. Paradoxically, resections BR without diversion and with complications had the lowest excess LOS and highest contribution margins, but had lower infection rates as a possible explanation.
Administrative data underreported elective colectomy complication incidence by 62% and inferences from administrative data should be viewed with caution. By capturing complication data concurrently, hospitals can better understand the quality and financial impact of complications, and provide appropriate resources for performance improvement efforts. Future quality studies may best be focused on elective resections for inflammatory diagnosis codes and be designed to thoroughly evaluate the multivariate risk factors associated with anastomotic integrity, source control, adequacy of bowel preparation, antibiotic coverage, efficacy of diversion, and the resulting potential for infectious complications prompting diversion. Preoperative mitigation of inflammatory risk factors may decrease the rate of diversion and reduce complications, financial risk, and opportunity cost.
References
Merkow RP, Ju MH, Chung JW, et al. Underlying reasons associated with hospital readmission following surgery in the United States. JAMA. 2015;313(5):483–95.
Artinyan A, Orcutt ST, Anaya DA, Richardson P, Chen GJ, Berger DH. Infectious postoperative complications decrease long-term survival in patients undergoing curative resection for colorectal cancer. ann Surg. 2015;261(3):497–505.
Fry DE, Pine M, Nedza SM, Locke DG, Reband AM, Pine G. Benchmarking hospital outcomes for improvement of care in medicare elective colon surgery. Am J Surg. 2016;212(1):10–5.
Tevis SE, Kennedy GD. Postoperative complications: looking forward to a safer future. Clin Colon Rectal Surg. 2016;29(3):246–52.
Morris AM, Baldwin LM, Matthews B, Dominitz JA, et al. Reoperation as a quality indicator in colorectal surgery: a population-based analysis. ann Surg. 2007;245(1):73–9.
Zhuang CL, Ye XZ, Zhang XD, Chen BC, Yu Z. Enhanced recovery after surgery programs versus traditional care for colorectal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum. 2013;56(5):667–78.
Keane C, Savage S, McFarlane K, et al. Enhanced recovery after surgery versus conventional care in colonic and rectal surgery. ANZ J Surg. 2012;82(10):697–703.
Birkmeyer JD, Gust C, Dimick JB, Birkmeyer NJO, Skinner JS. Hospital quality and the cost of inpatient surgery in the United States. Ann Surg. 2012;255(1):1–5. https://doi.org/10.1097/SLA.0b013e3182402c17.
Eappen S, Lane BH, Rosenberg B. Relationship between occurrence of surgical complications and hospital finances. JAMA. 2013;309(15):1599–606.
Govaert JA, Fiocco M, van Dijk WA, et al. Costs of complications after colorectal cancer surgery in the Netherlands: building the business case for hospitals. EJSO. 2015;41:1059–67.
Antonacci AC, Lam S, Lavarias V, Homel P, Eavey RD. A morbidity and mortality conference-based classification system for adverse events: surgical outcome analysis: part I. J Surg Res. 2008;147:172–7.
Antonacci AC, Lam S, Lavarias V, Homel P, Eavey RA. A report card system using error profile analysis and concurrent morbidity and mortality review: surgical outcome analysis, part II. J Surg Res. 2009;153:95–104.
Antonacci AC, Dechario S, Husk G, Stoffels G, Antonacci CL, Jarrett M. Analysis of surgical judgment and mortality utilizing a critique algorithm-based database and morbidity/mortality conference (MMC) review. Acad Surg Congr. 2019.
Zogg CK, Najjar P, Rios Diaz AJ, et al. Rethinking priorities: cost of complications after elective colectomy. Ann Surg. 2016;264(2):312–22.
Healy MA, Mullard AJ, Campell DA, Dimick JB. Hospital and payer costs associated with surgical complications. JAMA Surg. 2016;151(9):823–30.
Vonlanthan R, Slankamenac K, Breitenstein, et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg. 2011;254(6):907–13.
Patel AS, Bergman A, Moore BW, Haglund U. The economic burden of complications occurring in major surgical procedures: a systematic review. Appl Health Econ Health Policy. 2013;11(6):577–92.
McIsaac DI, Hamilton GM, Abdulla K, et al. Validation of new ICD-10-based patient safety indicators for identification of in-hospital complications in surgical patients: a study of diagnostic accuracy. BMJ Qual Saf. 2020;29(3):209–16.
Marusch F, Koch A, Schmidt U, et al. Value of a protective stoma in low anterior resections for rectal cancer. Dis Colon Rectum. 2002;45(9):1164–71.
Hüser N, Michalski CW, Erkan M, Schuster T, Rosenberg R, Kleeff J, et al. Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg. 2008;248(1):52–60.
Montedori A, Cirocchi R, Farinella E, Sciannameo F, Abraha I. Covering ileo- or colostomy in anterior resection for rectal carcinoma. Cochrane Database Syst Rev. 2010; https://doi.org/10.1002/14651858.CD006878.pub2.
McKenna NP, Bews KA, Cima RR, Crowson CS, Habermann EB. Development of a risk score to predict anastomotic leak after left-sided colectomy: which patients warrant diversion? J Gastrointest Surg. 2020;24(1):132–43.
Fry DE, Pine M, Nedza SM, et al. Benchmarking hospital outcomes for improvement of care in Medicare elective colon surgery. Am J Surg. 2016;212(1):10–5.
Keenan JE, Speicher PJ, Thacker JKM, et al. The preventative surgical site infection bundle in colorectal surgery: an effective approach to surgical site infection reduction and health care cost savings. JAMA Surg. 2014;149(10):1045–52.
Author information
Authors and Affiliations
Contributions
A. A. conceived of the original idea; A. A., G. H., and S. D. designed the database and implemented the data acquisition model; A. A., C. L. A., and S. D. performed the analytic calculations; D. C. and D. A. provided financial data; A. A., C. L. A., K. C., G. H., G. C., and M. J. contributed to the final version of the manuscript; all authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
A.C. Antonacci, C.L. Antonacci, K. Carsky, S.P. Dechario, G. Husk, D. Caulfield, D. Allinger, G. Coppa, and M. Jarrett declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Antonacci, A.C., Antonacci, C.L., Carsky, K. et al. Elective colectomy financial and opportunity cost analysis: diagnosis, case type, diversion, and complications. Eur Surg 54, 104–112 (2022). https://doi.org/10.1007/s10353-021-00716-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-021-00716-w