Summary
Background
Microvascular invasion (MVI) is currently only confirmed by histopathological studies of surgical specimens. Preoperative diagnosis of MVI combined with clinical treatment is still a research problem and direction in hepatocellular carcinoma (HCC). How to assess the presence of MVI early and give appropriate treatment has become a research hotspot.
Methods
This review focuses on recent advances in MVI-related research, including the use of serum markers, tumor tissue markers, and new imaging techniques to predict MVI, as well as the molecular biology mechanisms and therapeutic advances in MVI.
Results
The emergence of MVI may be caused by the interaction of many complex biological processes and various pathogenic factors. We need to try to select several risk factors and establish a systematic evaluation method to solve their respective deficiencies, so as to provide more practical applications for the preoperative prediction of MVI program. Simultaneously, the preoperative, intraoperative, and postoperative comprehensive treatment strategies for MVI are particularly important.
Conclusion
The presence of MVI is thought to reflect increased capacity for local infiltration and distant metastases and affects the prognosis of HCC patients. To accurately assess MVI early based on some biomarkers prior to surgery, we need to work hard to explore and integrate various treatments to create a personalized treatment plan for MVI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
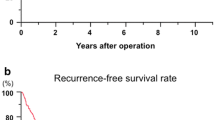
Hepatocellular carcinoma (HCC) ranks among the most common malignancies worldwide [1]. Hepatectomy and liver transplantation (LT) are the most important HCC treatments [2]. The 5-year recurrence rate were as high as 70% and 35%, respectively [3]. MVI significantly increased the risk of recurrence and extrahepatic metastasis after hepatectomy or LT in patients with HCC [4, 5]. But it can only be diagnosed by postoperative histopathology [6] with significant hysteresis. It is very important to diagnose MVI before surgery [7]. The possible mechanism of MVI is that hepatoma cells destroy vascular endothelial cells through receptor-mediated necroptosis [8], leading to cancer cells invading blood vessels and distant metastasis [9]. MVI can be found in tumor stroma, tumor cyst and paracancerous tissues [10]. Small vein branches are connected with the small branches of the peripheral portal vein of HCC, which can become the main metastatic pathway of HCC. If the diagnosis of MVI is difficult, immunohistochemical staining is feasible, such as CD34, CD31, SMA, D2-40, etc. [11]. The incidence of MVI in HCC was high (15–57.1%) [12]. There have been many studies in the world, including predicting MVI with serum markers, tumor tissue markers, and new imaging technologies, and trying to carry out a variety of treatment studies on MVI.
Preoperative diagnosis of MVI
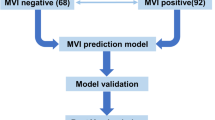
Many researchers have devoted themselves to searching for a method for preoperative detection of MVI, so that we can better assess the patient’s tumor invasion. Table 1 shows some of the current studies on preoperative prediction of the risk of MVI in HCC.
Correlation between clinical factors and MVI
MVI was one of the independent risk factors for tumor recurrence after hepatectomy in HCC patients who meet the Milan criteria [13]. Some studies have pointed out that MVI was closely related to the size, number, morphology, and degree of differentiation of hepatic neoplasms [14,15,16]. In patients with small HCC, long-term survival was not affected by MVI (p = 0.8), whereas in patients with larger HCC, significantly worse survival was observed in patients with MVI (p < 0.001) [17]. According to a study by Eguchi et al. [18], the average diameter of tumors in the MVI group was 5.2 cm and 3 cm in the non-MVI group. Yamashita et al. [19] reported that 28.9% of patients with tumor diameter <2 cm developed MVI. Gouw et al. [20] reported that when the tumor diameter is >4 cm, the probability of developing MVI is twice that of a tumor with <4 cm. Total tumor diameter >8 cm and tumor number >3 were also preoperative predictors of MVI in patients with multinodular HCC [21]. Different MVI types also affected post-hepatectomy survival [22]. Esnaola et al. [23] reported that 12% of patients with well-differentiated HCC developed MVI, and the incidence of MVI in moderately differentiated cases was 29%, while the incidence of MVI in low differentiation cases was up to 50%. Fujita et al. [24] classify the following risks for MVI: M0 level: no MVI was found; M1 (low-risk group): ≤5 MVI and occurred in the near-cancer area (≤1 cm); M2 (high-risk group): >5 MVI or MVI occurred in the distant cancer area (>1 cm). The higher the MVI group, the worse the prognosis. In addition, local nodal metastasis, body mass index, and other tumor characteristics have been reported to be significant predictors of MVI [25].
Predicting MVI with serum markers
Detection of the expression of certain HCC-specific antigens in serum can predict the occurrence of MVI. Studies have shown that MVI was correlated with the levels of aspartate aminotransferase (AST); gamma glutamyl transpeptidase (GGT); and lactate dehydrogenase (LDH) [26]; Li-cadherin [27]; alkaline phosphatase (ALP) [28]; preoperative neutrophil-to-lymphocyte ratio (NLR) [29] and DES-γ-carboxyprothrombin (DCP) [30] can predict the presence of MVI at a definite level. Patients with non-AFP-producing tumors had fewer MVI (P < 0.001) [31]. Studies suggested that elevated AFP was an independent risk factor for MVI [15, 32]. Zhang et al. found that a lower level of albumin, a higher level of AFP, and a larger tumor on preoperative imaging were independently associated with MVI [33]. However, some studies have found no significant correlation between AFP and MVI [7, 34]. Miyaaki et al. believed that AFP mainly reflects the differentiation of tumors and is not specific to HCC vascular invasion [35]. Some studies suggest that preoperative serum DCP levels are associated with the development of MVI [18, 36], but similar high levels of DCP and AFP are also present in the serum of patients with chronic hepatitis and cirrhosis, indicating that DCP expression is not specific [37]. miR-125b is the post-transcriptional regulation factor of HOTTIP [38] and can be used to predict MVI of HCC patients before hepatectomy [39]. The multivariate analysis showed that serum HSP70 and Eno-1 were potential biomarkers for preoperative prediction of MVI [40]. Paraoxonase 1 (PON1) is a hepatic-induced glycoprotein [41] and Huang et al. data indicated that serum PON1 was a novel diagnostic biomarker for MVI [42]. The second-generation sequencing technology has made great progress, and the application of blood as a material to detect tumor mutations has become more and more widespread. This has provided a more in-depth understanding of the occurrence and development of HCC from a genetic perspective, and provides an effective means for the diagnosis, prediction, and prevention of MVI.
Correlation between imaging techniques and MVI
In the preoperative imaging diagnosis, some breakthroughs have also been made in recent years. A non-smooth tumor margin on imaging was independently associated with the presence of MVI [43,44,45]. Chou et al. [46] performed a comparative analysis of preoperative CT images and postoperative disease specimens in 102 patients with HCC. The borders of non-smooth tumors revealed by CT were significantly associated with MVI (P < 0.001), sensitivity was 81.7%, and specificity was 88.1%. Cheung et al. reported that 18F-FDG-labeled PET can better predict MVI [47], and pointed out that the imaging agent 11C-acetate (11C-AC) can increase the sensitivity of the prediction effect. Tumor FDG avidity measured by tumor-to-normal liver standardized uptake value ratio (TLR) on FDG PET/CT was a preoperative imaging biomarker for the prediction of MVI in patients with HCC [48]. Xu et al. used diffusion-weighted MRI and found the sensitivity and specificity of low diffusion coefficient plus irregular peripheral enhancement for prediction of the presence of MVI to be 66.7 and 78.6%, respectively [49]. A recent magnetic imaging study showed that disproportionately weighted imaging of HCC and T2-weighted imaging mismatch were independent predictors of MVI with a high specificity (95.65%) [50]. Higher mean kurtosis values in combination with irregular circumferential enhancement were also potential predictive biomarkers for MVI [51]. RVI is a noninvasive radiogenomic biomarker that accurately predicts histological MVI in HCC surgical candidates. This accurately predicts preoperative tissue MVI in patients undergoing HCC surgery and helps identify whether patients can benefit from surgical treatment [3]. The radiomics nomogram, as a noninvasive preoperative prediction method, can show a favorable predictive accuracy for MVI status in patients with HBV-related HCC [52]. A recent study found histogram analysis of intravoxel incoherent motion (IVIM) based on whole tumor volume can be useful for predicting MVI [53]. Preoperative IVIM DW imaging and Gd-EOB-DTPA-enhanced MRI (DCE-MRI) of 51 patients who were analyzed, Zhao et al. found that an irregular shape and D value ≤1.16 × 10−3 mm2/s may suggest the presence of MVI in HCC [54]. Unfortunately, these imaging features depend primarily on the personal experience of the imaging physician. At the same time, there is a lack of prospective studies and it is currently not available for preoperative screening of MVI [50].
Predict MVI with HCC signaling pathway protein or mRNA
The emergence of MVI may be caused by the interaction of many complex biological processes and various pathogenic factors, which may involve many signaling pathways [55]. Tumor cells in the microenvironment can produce a variety of cytokines that affect the tumor progression [56]. HBV infection and active HBV replication were associated with vascular invasion [57]. HBV infection in the liver microenvironment increased the activity of TGF-β signaling and induced Treg cell recruitment and promoted venous metastasis of HCC [58]. Treg cells can help cancer cells escape immune surveillance, while tumor blood vessels provided the necessary nutrient supply and immune microenvironment for tumor growth to accelerate the malignant progression of the tumor [12]. Table 2 shows some MVI-related biomarkers and their biological functions in HCC studies.
By detecting pathological samples, genes or proteins closely related to MVI were found. Yuan et al. found that lncRNA MVIH was overexpressed in MVI-related HCC patients by microarray analysis [59]. MVIH activates tumor-induced angiogenesis by inhibiting the secretion of phosphoglycerate kinase 1 (PGK1) to promote tumor growth and intrahepatic metastasis. At the same time, MVIH expression was positively correlated with microvessel density [59]. Poté et al. [60] used mass spectrometry to find that histone H4 modifications (H4K16ac and H4K20me2) were highly expressed in the MVI-positive group. The expression of ciRS-7 in HCC tissues with concurrent MVI was inversely correlated with that of miR-7 and positively related to that of two miR-7-targeted genes (PIK3CD and p70S6K) [61]. Xu et al. [62] identified the epithelial–mesenchymal transition (EMT) as an important part of MVI. By inhibiting the transcription factor FOXC1, which plays an important role in EMT, EMT can be reversed and the probability of metastasis can be reduced. Fransvea et al. [63] found that B1 integrin was indispensable in the MVI course of HCC patients. Inhibition of TGF-β1 receptors can inhibit the phosphorylation of B1 integrin, thereby cutting off the vascular invasion path of cancer cells. Mínguez et al. [64] found that 35 gene markers were associated with vascular invasion and the accuracy of MVI prediction was 69%.
In addition to the above studies, there are many studies on MVI biomarkers [65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82]. However, despite the success of these approaches in preclinical translational studies, the clinical application of gene expression profiling is still immature [83]. The sensitivity and specificity of these biological markers are not very satisfactory [84, 85], making it difficult to translate basic research into clinical applications.
Integrating multiple factors to predict MVI
A single tumor feature cannot accurately predict whether MVI has occurred. The researchers proposed to predict MVI by integrating multiple biomarkers. Small HCC (≤3 cm) were generally considered to have low malignant potential; however, matching at least one factor among three (tumor diameter ≥2 cm, AFP ≥200 ng/mL, or DCP ≥40 mAU/mL) can predict pathological MVI in small HCC [86]. A prediction scoring system for MVI was built up according to three independent predictors (tumor size >3.5 cm, AFP >200 ng/mL, and GGT >53 U/L). The prevalence of MVI in HCC patients with predictive score ≥2 was 58.3%, which was obviously higher than in patients with predictive score <2 (20.8%) [87]. Serum AFP level >400 μg/L, serum GGT level >130 U/L, total tumor diameter >8 cm, and tumor number >3 were also preoperative predictors of MVI in patients with multinodular HCC [21]. Cucchetti et al. established an artificial neural network (ANN) model using noninvasive parameters, which included preoperative AFP level, tumor number, and size to predict the occurrence of MVI [88]. Lei et al. developed a nomogram score that patients who had a nomogram score of less than 200 or 200 or greater were considered to have low or high risks of MVI presence, respectively [89]. Lai et al. [90] proposed that “Time-Radiological-response-Alpha-fetoprotein-Inflammation” (TRAIN) score was the best predictor of MVI. A TRAIN score ≥1.0 excellently stratified both the investigated populations in terms of intention-to-treat (ITT) and recurrence survivals. Poté et al. developed an original virtual biopsy to evaluate the immunohistochemical performance of three MVI biomarkers (H4K16ac, H4K20me2, DCP) for predicting MVI in HCC core needle biopsy (CNB). Studies have shown that DCP/H4K16ac performed best in predicting MVI and paved the way for future development of prognostic biomarkers of HCC that can guide treatment strategies [91].
Many of the factors in the above studies were closely related to the occurrence and appearance of MVI, but all factors have different deficiencies. We need to try to select several risk factors and establish a systematic evaluation method to solve their respective deficiencies, so as to provide more practical applications for the preoperative prediction of MVI program.
Comprehensive treatment strategy for MVI of HCC
MVI is currently considered to be closely related to the recurrence of HCC after surgery [92]. Similar results were obtained in patients with metastatic HCC [93], and the rate of extrahepatic recurrence in patients with MVI was higher than in patients without MVI [94]. The preoperative, intraoperative, and postoperative comprehensive treatment strategies for MVI are particularly important. Table 3 shows MVI treatment-related research in the reported studies.
Preoperative treatment strategy of MVI
Preoperative early prediction of MVI can help guide surgery and adjuvant therapy. A systematic retrospective analysis indicated that the correlation coefficient between MVI and the 3‑year disease-free survival (DFS) reduction after LT and hepatectomy was 3.4 and 1.8, respectively. This showed that the prognosis of HCC patients with LT was more closely related to MVI [12]. Pre-transplant prediction of high-risk MVI using both morphological and biological tumor characteristics prior to LT is also a prerequisite to ensure proper allocation of liver sources [95]. Mazzaferro et al. [96] established an MVI-related LT prognostic assessment system—the Up7 criteria—and the 5‑year survival rates of MVI-negative patients meeting this criterion were close to the Milan standard of 71.2%. The results of this study showed that MVI can be used as a new LT selection criterion. Vitale et al. found that patients with a model-based end-stage liver disease (MELD) score greater than 10 and MVI-negativity had a better survival rate when selected for LT, while with a score <10 points or in MVI-positive patients, surgical resection may be the better choice [97]. Primary HCC tumor size <2 cm had a good prognosis after LT and was not affected by MVI or tumor differentiation [98]. However, the medical resources and costs required for LT far exceed liver resection, so it cannot be used as the preferred treatment for HCC. Hepatectomy was more preferred for patients with MVI because of similar 5‑year survival rates in these two procedures [99].
Currently, neoadjuvant therapy with systemic chemotherapy or TACE for resectable HCC is not recommended [100]. Due to its poor therapeutic effect, the optimal timing of surgical treatment may be delayed, resulting in the resectable HCC becoming unresectable. The therapeutic effect of preoperative TACE can only be obtained after treatment. TACE-treated patients were divided into TACE responders and non-responders. TACE responders had better survival outcomes and MVI positivity was a poor prognostic factor for these patients [101, 102]. Whether or not neoadjuvant TACE provides a good prognosis deserves further investigation in patients at a high risk of MVI [37]. In HCV cirrhosis, patients HCC developed soon after DAA therapy [103]. A high preoperative HBV DNA level was an independent risk factor of MVI. Antiviral treatment administered more than 90 days before surgery was associated with reduced incidences of MVI and early tumor recurrence after partial hepatectomy for HBV-related HCC [104].
Intraoperative treatment strategy of MVI
Liver surgery has become the standard of care for HCC [105]. The choice of surgical approach and margins was of great importance to MVI-positive patients. An adequate incisal margin can be used to completely remove the micrometastatic lesion, prevent recurrence, and prolong long-term survival. If the surgical margin reaches a distance of more than 5 cm from the tumor margin, the 5‑year DFS rate of patients after surgery can increase from 21 to 33%. Nevertheless, most of the HCC patients were accompanied by basic diseases such as hepatocirrhosis and hepatocirrhosis. Extended resection may easily cause liver dysfunction and other complications [106]. In patients with a high risk of MVI and well-preserved liver function, anatomic resection (AR) may be worth considering [21].
It remains controversial as to whether AR really confers a survival advantage over non-anatomical resection (NAR) for HCC [107, 108]. A recent study showed that AR reduced early recurrence in patients with poorly differentiated tumor or with MVI [109]. In the high MVI group, the prognosis of patients undergoing AR was significantly better than for NAR [110], and the incidence of MVI was higher in the AR group (P = 0.048). This suggested that AR can more completely remove the MVI [111]. However, using the propensity score matching analysis found no significant difference in the early recurrence of the tumor after AR and NAR in both MVI-positive and MVI-negative patients [111]. In view of the higher frequency of MVI in the portal vein system, Hasegawa et al. recommend AR to slow recurrence and prolong survival [112]. When the surgical margin of MVI-positive patients is >1 cm, the patient’s DFS rate is significantly better than that of MVI-positive patients with surgical margin <1 cm [113]. In MVI-positive patients relapsed after hepatectomy for the first time, a second repeat operation can significantly prolong the overall survival. This study suggested that the biology of MVI may change after secondary liver resection [114]. LT replaced the entire diseased liver, i.e., not only removed the tumor but also replaced the soil upon which the tumor relies. It was a more thorough surgical method for patients with MVI [115]. A study on 1024 patients with early stage HCC who underwent hepatectomy or LT, the emergence of MVI had a more significant impact on LT patients [99]. MVI was a relevant factor for the recurrence of HCC patients after LT, MVI patients did not benefit from LT [37]. Liver congestion may promote the recurrence of HCC after living-donor LT [116]. Liver congestion should be reduced during surgery. In addition, preoperative puncture for HCC was difficult to reflect the overall condition of the tumor because of the small number of specimens, and the operation itself has been proved to significantly increase the risk of metastasis. However, intraoperative liver puncture may help the choice of cutting margins of HCC.
Postoperative treatment strategy of MVI
Although postoperative pathological diagnosis of MVI is lagging, it can help predict the risk of recurrence and metastasis and guide postoperative anti-relapse therapy [117].
Sun et al. retrospectively analyzed data from 322 patients with MVI, suggesting that postoperative adjuvant TACE (PA-TACE) can improve the long-term prognosis of these patients [117]. MVI-positive patients with well-tolerated liver function who underwent PA-TACE after R0 hepatectomy (RH) or RH alone were studied retrospectively. This study showed that PA-TACE may be beneficial for HCC patients with MVI [117]. TACE may be the more effective treatment option for recurrent HCC of BCLC stage 0 or A than surgery/RFA in MVI-positive patients, especially in those who recur early after curative resection [118], while in the MVI-negative group there was no significant difference. Adjuvant TACE (twice or thrice) after radical resection was beneficial for HCC patients with poor differentiation and MVI, especially for those with a tumor diameter of >5 cm [119]. Adjuvant radiotherapy after hepatectomy had a better survival prognosis for HCC patients with MVI than TACE or conservative treatment [120]. However, it is also reported in the literature that PA-TACE can not only reduce the tumor recurrence rate of HCC patients but may also cause more extrahepatic metastases. It has been confirmed that the microvessel density (MVD) of HCC patients after TACE was significantly increased, and vascular endothelial growth factor was also significantly increased. These unfavorable factors increased the invasiveness of tumor cells within the microvessel and accelerated the recurrence and metastasis of HCC [121]. Therefore, the effect of PA-TACE still requires a clear multicenter meta-analysis.
Current international guidelines for the treatment of HCC recommend sorafenib as a molecularly targeted drug for MVI treatment [122]. A pilot study, patients with MVI can effectively improve DFS after receiving sorafenib for 4 months [123]. The abovementioned clinical trials suggested that certain targeted drugs may inhibit the recurrence and metastasis of HCC patients with MVI. Postoperative adjuvant therapy with sorafenib in patients with MVI can reduce HCC recurrence and improve patient survival [123]. However, Jordi Bruix et al. believed that hepatectomy of HCC patients with adjuvant treatment with sorafenib does not prolong survival [124]. It has also been reported that doxycycline non-selectively inhibits the synthesis of matrix metalloproteinase-9 (MMP-9). MMP-9 can increase the permeability of hepatoma cells. Therefore, doxycycline was considered to inhibit vascular metastasis of HCC [125]. In addition, some new anti-neoplastic vasculogenic drugs such as TNP-470, Flk-1, endostatin, and IFN-α were considered to be able to resist the invasion of HCC and reduce the recurrence and metastasis of tumors [126,127,128].
Fewer studies on other treatments for MVI, such as the efficacy of direct-acting antiviral (DAA) therapy [103], implantation of [125] I particles in the hepatic cut surface [129], and radiofrequency ablation (RFA) [130, 131] are in dispute and need further evaluation.
Conclusion
In summary, MVI is an important marker of tumor invasion behavior and affects the prognosis of HCC patients. How to detect MVI early by some biomarkers before surgery is still a problem worth exploring. At the same time, there is still controversy about the preoperative TACE and drug treatment of HCC with MVI. It is necessary to conduct a multicenter large randomized controlled trial (RCT) study of these controversial treatments. For postoperative adjuvant therapy, TACE or targeted therapy still requires further research. Today, with the rapid development of precision medicine, MVI’s diagnosis and treatment strategies still have no strong evidence-based medicine foundation. Based on an accurate assessment, we need to work hard to explore and integrate various treatments to create a personalized treatment plan.
References
Ringelhan M, Pfister D, O’Connor T, Pikarsky E, Heikenwalder M. The immunology of hepatocellular carcinoma. Nat Immunol. 2018; https://doi.org/10.1038/s41590-018-0044-z.
Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet. 2012;379(9822):1245–55.
Banerjee S, Wang DS, Kim HJ, et al. A computed tomography radiogenomic biomarker predicts microvascular invasion and clinical outcomes in hepatocellular carcinoma. Hepatology. 2015;62(3):792–800.
Zheng J, Chakraborty J, Chapman WC, et al. Preoperative prediction of microvascular invasion in hepatocellular carcinoma using quantitative image analysis. J Am Coll Surg. 2017; https://doi.org/10.1016/j.jamcollsurg.2017.09.003.
Jang SY, Park SY, Lee HW, et al. The combination of periostin overexpression and microvascular invasion is related to a poor prognosis for hepatocellular carcinoma. Gut Liver. 2016;10(6):948–54.
Zhang X, Li J, Shen F. Significance of presence of microvascular invasion in specimens obtained after surgical treatment of hepatocellular carcinoma. 2017.
Pote N, Cauchy F, Albuquerque M, et al. Performance of PIVKA-II for early hepatocellular carcinoma diagnosis and prediction of microvascular invasion. J Hepatol. 2015;62(4):848–54.
Strilic B, Yang L, Albarran-Juarez J, et al. Tumour-cell-induced endothelial cell necroptosis via death receptor 6 promotes metastasis. Nature. 2016;536(7615):215–8.
Ding T, Xu J, Zhang Y, et al. Endothelium-coated tumor clusters are associated with poor prognosis and micrometastasis of hepatocellular carcinoma after resection. Cancer. 2011;117(21):4878–89.
Roayaie S, Blume IN, Thung SN, et al. A system of classifying microvascular invasion to predict outcome after resection in patients with hepatocellular carcinoma. Gastroenterology. 2009;137(3):850–5.
Sumie S, Nakashima O, Okuda K, et al. The significance of classifying microvascular invasion in patients with hepatocellular carcinoma. Ann Surg Oncol. 2014;21(3):1002–9.
Rodriguez-Peralvarez M, Luong TV, Andreana L, Meyer T, Dhillon AP, Burroughs AK. A systematic review of microvascular invasion in hepatocellular carcinoma: diagnostic and prognostic variability. Ann Surg Oncol. 2013;20(1):325–39.
Imura S, Teraoku H, Yoshikawa M, et al. Potential predictive factors for microvascular invasion in hepatocellular carcinoma classified within the Milan criteria. Int J Clin Oncol. 2018;23(1):98–103.
Shirabe K, Toshima T, Kimura K, et al. New scoring system for prediction of microvascular invasion in patients with hepatocellular carcinoma. Liver Int. 2014;34(6):937–41.
McHugh PP, Gilbert J, Vera S, Koch A, Ranjan D, Gedaly R. Alpha-fetoprotein and tumour size are associated with microvascular invasion in explanted livers of patients undergoing transplantation with hepatocellular carcinoma. HPB (Oxford). 2010;12(1):56–61.
Kim BK, Han KH, Park YN, et al. Prediction of microvascular invasion before curative resection of hepatocellular carcinoma. J Surg Oncol. 2008;97(3):246–52.
Shindoh J, Andreou A, Aloia TA, et al. Microvascular invasion does not predict long-term survival in hepatocellular carcinoma up to 2 cm: reappraisal of the staging system for solitary tumors. Ann Surg Oncol. 2013;20(4):1223–9.
Eguchi S, Takatsuki M, Hidaka M, et al. Predictor for histological microvascular invasion of hepatocellular carcinoma: a lesson from 229 consecutive cases of curative liver resection. World J Surg. 2010;34(5):1034–8.
Yamashita Y, Tsuijita E, Takeishi K, et al. Predictors for microinvasion of small hepatocellular carcinoma 〈/= 2 cm. Ann Surg Oncol. 2012;19(6):2027–34.
Gouw AS, Balabaud C, Kusano H, Todo S, Ichida T, Kojiro M. Markers for microvascular invasion in hepatocellular carcinoma: where do we stand? Liver Transplant. 2011;17(Suppl 2):S72–S80.
Zhao WC, Fan LF, Yang N, Zhang HB, Chen BD, Yang GS. Preoperative predictors of microvascular invasion in multinodular hepatocellular carcinoma. Eur J Surg Oncol. 2013;39(8):858–64.
Hou YF, Wei YG, Yang JY, et al. Microvascular invasion patterns affect survival in hepatocellular carcinoma patients after second hepatectomy. J Surg Res. 2016;200(1):82–90.
Esnaola NF, Lauwers GY, Mirza NQ, et al. Predictors of microvascular invasion in patients with hepatocellular carcinoma who are candidates for orthotopic liver transplantation. J Gastrointest Surg. 2002;6(2):224–32. discussion 232.
Fujita N, Aishima S, Iguchi T, et al. Histologic classification of microscopic portal venous invasion to predict prognosis in hepatocellular carcinoma. Hum Pathol. 2011;42(10):1531–8.
Siegel AB, Wang S, Jacobson JS, et al. Obesity and microvascular invasion in hepatocellular carcinoma. Cancer Invest. 2010;28(10):1063–9.
Yan X, Fu X, Deng M, et al. Infiltrative hepatocellular carcinoma: assessment of factors associated with outcomes in patients undergoing hepatectomy. Medicine. 2016;95(19):e3589.
Ding ZB, Shi YH, Zhou J, et al. Liver-intestine cadherin predicts microvascular invasion and poor prognosis of hepatitis B virus-positive hepatocellular carcinoma. Cancer. 2009;115(20):4753–65.
Zhu Y, Xu D, Zhang Z, et al. A new laboratory-based algorithm to predict microvascular invasion and survival in patients with hepatocellular carcinoma. Int J Surg. 2018. https://doi.org/10.1016/j.ijsu.2018.07.011
Yu Y, Song J, Zhang R, et al. Preoperative neutrophil-to-lymphocyte ratio and tumor-related factors to predict microvascular invasion in patients with hepatocellular carcinoma. Oncotarget. 2017;8(45):79722–30.
Pote N, Cauchy F, Albuquerque M, et al. Contribution of virtual biopsy to the screening of microvascular invasion in hepatocellular carcinoma: a pilot study. Liver Int. 2018;38(4):687–94.
Agopian VG, Harlander-Locke MP, Markovic D, et al. Evaluation of patients with hepatocellular carcinomas that do not produce alpha-fetoprotein. JAMA Surg. 2017;152(1):55–64.
Imura S, Teraoku H, Yoshikawa M, et al. Potential predictive factors for microvascular invasion in hepatocellular carcinoma classified within the Milan criteria. Int J Clin Oncol. 2017. https://doi.org/10.1007/s10147-017-1189-8
Zheng J, Seier K, Gonen M, et al. Utility of serum inflammatory markers for predicting microvascular invasion and survival for patients with hepatocellular carcinoma. Ann Surg Oncol. 2017;24(12):3706–14.
Kaibori M, Ishizaki M, Matsui K, Kwon AH. Predictors of microvascular invasion before hepatectomy for hepatocellular carcinoma. J Surg Oncol. 2010;102(5):462–8.
Miyaaki H, Nakashima O, Kurogi M, Eguchi K, Kojiro M. Lens culinaris agglutinin-reactive alpha-fetoprotein and protein induced by vitamin K absence II are potential indicators of a poor prognosis: a histopathological study of surgically resected hepatocellular carcinoma. J Gastroenterol. 2007;42(12):962–8.
Iguchi T, Shirabe K, Aishima S, et al. New pathologic stratification of microvascular invasion in Hepatocellular carcinoma: predicting prognosis after living-donor liver transplantation. Transplantation. 2015;99(6):1236–42.
Zhang X, Li J, Shen F, Lau WY. Significance of presence of microvascular invasion in specimens obtained after surgical treatment of hepatocellular carcinoma. J Gastroenterol Hepatol. 2018;33(2):347–54.
Tsang F, Au S, Wei L, et al. Long non-coding RNA HOTTIP is frequently up-regulated in hepatocellular carcinoma and is targeted by tumour suppressive miR-125b. Liver Int. 2015;35(5):1597–606.
Liu M, Wang L, Zhu H, et al. A preoperative measurement of serum microRNA-125b May predict the presence of Microvascular invasion in hepatocellular carcinomas patients. Transl Oncol. 2016;9(3):167–72.
Yu YQ, Wang L, Jin Y, et al. Identification of serologic biomarkers for predicting microvascular invasion in hepatocellular carcinoma. Oncotarget. 2016;7(13):16362–71.
Lao X, Wang X, Liu Y, et al. Association of paraoxonase 1 gene polymorphisms with the risk of hepatitis B virus-related liver diseases in a Guangxi population: a case-control study. Medicine. 2015;94(48):e2179.
Huang C, Wang Y, Liu S, et al. Quantitative proteomic analysis identified paraoxonase 1 as a novel serum biomarker for microvascular invasion in hepatocellular carcinoma. J Proteome Res. 2013;12(4):1838–46.
Lee S, Kim SH, Lee JE, Sinn DH, Park CK. Preoperative gadoxetic acid-enhanced MRI for predicting microvascular invasion in patients with single hepatocellular carcinoma. J Hepatol. 2017;67(3):526–34.
Wu TH, Hatano E, Yamanaka K, et al. A non-smooth tumor margin on preoperative imaging predicts microvascular invasion of hepatocellular carcinoma. Surg Today. 2016;46(11):1275–81.
Chou CT, Chen RC, Lin WC, Ko CJ, Chen CB, Chen YL. Prediction of microvascular invasion of hepatocellular carcinoma: preoperative CT and histopathologic correlation. AJR Am J Roentgenol. 2014;203(3):W253–W9.
Chou CT, Chen RC, Lee CW, Ko CJ, Wu HK, Chen YL. Prediction of microvascular invasion of hepatocellular carcinoma by pre-operative CT imaging. Br J Radiol. 2012;85(1014):778–83.
Cheung TT, Chan SC, Ho CL, et al. Can positron emission tomography with the dual tracers [11 C]acetate and [18 F]fludeoxyglucose predict microvascular invasion in hepatocellular carcinoma? Liver Transplant. 2011;17(10):1218–25.
Hyun SH, Eo JS, Song BI, et al. Preoperative prediction of microvascular invasion of hepatocellular carcinoma using (18)F-FDG PET/CT: a multicenter retrospective cohort study. Eur J Nucl Med Mol Imaging. 2018;45(5):720–6.
Xu P, Zeng M, Liu K, Shan Y, Xu C, Lin J. Microvascular invasion in small hepatocellular carcinoma: is it predictable with preoperative diffusion-weighted imaging? J Gastroenterol Hepatol. 2014;29(2):330–6.
Yang C, Wang H, Sheng R, Ji Y, Rao S, Zeng M. Microvascular invasion in hepatocellular carcinoma: is it predictable with a new, preoperative application of diffusion-weighted imaging? Clin Imaging. 2017;41:101–5.
Wang WT, Yang L, Yang ZX, et al. Assessment of microvascular invasion of hepatocellular carcinoma with diffusion Kurtosis imaging. Radiology. 2018;286(2):571–80.
Peng J, Zhang J, Zhang Q, Xu Y, Zhou J, Liu L. A radiomics nomogram for preoperative prediction of microvascular invasion risk in hepatitis B virus-related hepatocellular carcinoma. Diagnostic Interv Radiol. 2018;24(3):121–7.
Li H, Zhang J, Zheng Z, et al. Preoperative histogram analysis of intravoxel incoherent motion (IVIM) for predicting microvascular invasion in patients with single hepatocellular carcinoma. Eur J Radiol. 2018;105:65–71.
Zhao W, Liu W, Liu H, et al. Preoperative prediction of microvascular invasion of hepatocellular carcinoma with IVIM diffusion-weighted MR imaging and Gd-EOB-DTPA-enhanced MR imaging. PLoS ONE. 2018;13(5):e197488.
Marquardt JU, Galle PR, Teufel A. Molecular diagnosis and therapy of hepatocellular carcinoma (HCC): an emerging field for advanced technologies. J Hepatol. 2012;56(1):267–75.
Ye J, Wu D, Wu P, Chen Z, Huang J. The cancer stem cell niche: cross talk between cancer stem cells and their microenvironment. Tumour Biol. 2014;35(5):3945–51.
Wei X, Li N, Li S, et al. Hepatitis B virus infection and active replication promote the formation of vascular invasion in hepatocellular carcinoma. BMC Cancer. 2017;17(1):304.
Yang P, Li QJ, Feng Y, et al. TGF-beta-miR-34a-CCL22 signaling-induced Treg cell recruitment promotes venous metastases of HBV-positive hepatocellular carcinoma. Cancer Cell. 2012;22(3):291–303.
Yuan SX, Yang F, Yang Y, et al. Long noncoding RNA associated with microvascular invasion in hepatocellular carcinoma promotes angiogenesis and serves as a predictor for hepatocellular carcinoma patients’ poor recurrence-free survival after hepatectomy. Hepatology. 2012;56(6):2231–41.
Pote N, Alexandrov T, Le Faouder J, et al. Imaging mass spectrometry reveals modified forms of histone H4 as new biomarkers of microvascular invasion in hepatocellular carcinomas. Hepatology. 2013;58(3):983–94.
Xu L, Zhang M, Zheng X, Yi P, Lan C, Xu M. The circular RNA ciRS-7 (Cdr1as) acts as a risk factor of hepatic microvascular invasion in hepatocellular carcinoma. J Cancer Res Clin Oncol. 2017;143(1):17–27.
Xu ZY, Ding SM, Zhou L, et al. FOXC1 contributes to microvascular invasion in primary hepatocellular carcinoma via regulating epithelial-mesenchymal transition. Int J Biol Sci. 2012;8(8):1130–41.
Fransvea E, Mazzocca A, Antonaci S, Giannelli G. Targeting transforming growth factor (TGF)-betaRI inhibits activation of beta1 integrin and blocks vascular invasion in hepatocellular carcinoma. Hepatology. 2009;49(3):839–50.
Minguez B, Hoshida Y, Villanueva A, et al. Gene-expression signature of vascular invasion in hepatocellular carcinoma. J Hepatol. 2011;55(6):1325–31.
Huang KT, Kuo IY, Tsai MC, et al. Factor VII-induced microRNA-135a inhibits autophagy and is associated with poor prognosis in hepatocellular carcinoma. Mol Ther Nucleic Acids. 2017;9:274:283.
Lin J, Lin W, Ye Y, et al. Kindlin-2 promotes hepatocellular carcinoma invasion and metastasis by increasing Wnt/beta-catenin signaling. J Exp Clin Cancer Res. 2017;36(1):134. https://doi.org/10.1186/s13046-017-0603-4
Govaere O, Petz M, Wouters J, et al. The PDGFRalpha-laminin B1-keratin 19 cascade drives tumor progression at the invasive front of human hepatocellular carcinoma. Oncogene. 2017;36(47):6605–16.
Fu L, Chen Q, Yao T, et al. Hsa_circ_0005986 inhibits carcinogenesis by acting as a miR-129-5p sponge and is used as a novel biomarker for hepatocellular carcinoma. Oncotarget. 2017;8(27):43878–88.
Zhu XT, Yuan JH, Zhu TT, Li YY, Cheng XY. Long noncoding RNA glypican 3 (GPC3) antisense transcript 1 promotes hepatocellular carcinoma progression via epigenetically activating GPC3. FEBS J. 2016;283(20):3739–54.
Jeon Y, Kim H, Jang ES, et al. Expression profile and prognostic value of glypican-3 in post-operative South Korean hepatocellular carcinoma patients. APMIS. 2016;124(3):208–15.
Calderaro J, Rousseau B, Amaddeo G, et al. Programmed death ligand 1 expression in hepatocellular carcinoma: relationship with clinical and pathological features. Hepatology. 2016;64(6):2038–46.
Liu WT, Jing YY, Yu GF, et al. Toll like receptor 4 facilitates invasion and migration as a cancer stem cell marker in hepatocellular carcinoma. Cancer Lett. 2015;358(2):136–43.
Cai Z, Zeng Y, Xu B, et al. Galectin-4 serves as a prognostic biomarker for the early recurrence/metastasis of hepatocellular carcinoma. Cancer Sci. 2014;105(11):1510–7.
Govaere O, Komuta M, Berkers J, et al. Keratin 19: a key role player in the invasion of human hepatocellular carcinomas. Gut. 2014;63(4):674–85.
Park Y, Yu E. Expression of metallothionein-1 and metallothionein-2 as a prognostic marker in hepatocellular carcinoma. J Gastroenterol Hepatol. 2013;28(9):1565–72.
Shim JH, Lee HC, Han S, Kang HJ, Yu E, Lee SG. Hepatocyte nuclear factor 1beta is a novel prognostic marker independent of the Milan criteria in transplantable hepatocellular carcinoma: a retrospective analysis based on tissue microarrays. Liver Transplant. 2013;19(3):336–45.
Chung KY, Cheng IK, Ching AK, Chu JH, Lai PB, Wong N. Block of proliferation 1 (BOP1) plays an oncogenic role in hepatocellular carcinoma by promoting epithelial-to-mesenchymal transition. hepatology. 2011;54(1):307–18.
Yang B, Liu Y, Zhao J, et al. Ectopic overexpression of filamin C scaffolds MEK1/2 and ERK1/2 to promote the progression of human hepatocellular carcinoma. Cancer Lett. 2017;388:167–76.
Liu Z, Chang Q, Yang F, et al. Long non-coding RNA NEAT1 overexpression is associated with unfavorable prognosis in patients with hepatocellular carcinoma after hepatectomy: a Chinese population-based study. Eur J Surg Oncol. 2017;43(9):1697–703.
Zhou ZJ, Dai Z, Zhou SL, et al. Overexpression of HnRNP A1 promotes tumor invasion through regulating CD44v6 and indicates poor prognosis for hepatocellular carcinoma. Int J Cancer. 2013;132(5):1080–9.
Zhuang LK, Yang YT, Ma X, et al. MicroRNA-92b promotes hepatocellular carcinoma progression by targeting Smad7 and is mediated by long non-coding RNA XIST. Cell Death Dis. 2016;7:e2203.
Xiao C, Wang C, Cheng S, et al. The significance of low levels of LINC RP1130-1 expression in human hepatocellular carcinoma. Biosci Trends. 2016;10(5):378–85.
Nault JC, Galle PR, Marquardt JU. The role of molecular enrichment on future therapies in hepatocellular carcinoma. J Hepatol. 2018;69(1):237–47.
Yamashita Y, Shirabe K, Aishima S, Maehara Y. Predictors of microvascular invasion in hepatocellular carcinoma. Dig Dis. 2015;33(5):655–60.
Agopian VG, Harlander-Locke M, Zarrinpar A, et al. A novel prognostic nomogram accurately predicts hepatocellular carcinoma recurrence after liver transplantation: analysis of 865 consecutive liver transplant recipients. J Am Coll Surg. 2015;220(4):416–27.
Yamashita YI, Imai K, Yusa T, et al. Microvascular invasion of single small hepatocellular carcinoma 〈/=3 cm: Predictors and optimal treatments. Ann Gastroenterol Surg. 2018;2(3):197–203.
Zhao H, Hua Y, Lu Z, et al. Prognostic value and preoperative predictors of microvascular invasion in solitary hepatocellular carcinoma 〈/= 5 cm without macrovascular invasion. Oncotarget. 2017;8(37):61203–14.
Cucchetti A, Piscaglia F, Grigioni AD, et al. Preoperative prediction of hepatocellular carcinoma tumour grade and micro-vascular invasion by means of artificial neural network: a pilot study. J Hepatol. 2010;52(6):880–8.
Lei Z, Li J, Wu D, et al. Nomogram for preoperative estimation of microvascular invasion risk in hepatitis B virus-related hepatocellular carcinoma within the Milan criteria. JAMA Surg. 2016;151(4):356–63.
Lai Q, Nicolini D, Inostroza Nunez M, et al. A novel prognostic index in patients with hepatocellular cancer waiting for liver transplantation: time-radiological-response-alpha-fetoprotein-INflammation (TRAIN) score. Ann Surg. 2016;264(5):787–96.
Pote N, Cauchy F, Albuquerque M, et al. Contribution of virtual biopsy to the screening of microvascular invasion in hepatocellular carcinoma: A pilot study. Liver Int. 2018;38(4):687–94.
Lim KC, Chow PK, Allen JC, et al. Microvascular invasion is a better predictor of tumor recurrence and overall survival following surgical resection for hepatocellular carcinoma compared to the Milan criteria. Ann Surg. 2011;254(1):108–13.
Bockhorn M, Sotiropoulos G, Neuhaus J, et al. Prognostic impact of intrahepatic lymphatic and microvascular involvement in cases of colorectal liver metastases. Int J Colorectal Dis. 2009;24(7):845–50.
Ho CM, Hu RH, Lee PH, Wu YM, Ho MC. Long-term survival in patients with T2 hepatocellular carcinoma after primary curative resection can be further stratified by tumor size. Medicine. 2014;93(27):e203.
Grat M, Stypulkowski J, Patkowski W, et al. Limitations of predicting microvascular invasion in patients with hepatocellular cancer prior to liver transplantation. Sci Rep. 2017;7:39881.
Mazzaferro V, Llovet JM, Miceli R, et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol. 2009;10(1):35–43.
Vitale A, Huo TL, Cucchetti A, et al. Survival benefit of liver transplantation versus resection for Hepatocellular carcinoma: impact of MELD score. Ann Surg Oncol. 2015;22(6):1901–7.
El-Fattah MA. Hepatocellular carcinoma biology predicts survival outcome after liver transplantation in the USA. Indian J Gastroenterol. 2017;36(2):117–25.
Vitale A, Cucchetti A, Qiao GL, et al. Is resectable hepatocellular carcinoma a contraindication to liver transplantation? A novel decision model based on “number of patients needed to transplant” as measure of transplant benefit. J Hepatol. 2014;60(6):1165–71.
Jiang JH, Guo Z, Lu HF, et al. Adjuvant transarterial chemoembolization after curative resection of hepatocellular carcinoma: propensity score analysis. World J Gastroenterol. 2015;21(15):4627–34.
Goh BK, Chow PK, Teo JY, et al. Number of nodules, Child-Pugh status, margin positivity, and microvascular invasion, but not tumor size, are prognostic factors of survival after liver resection for multifocal hepatocellular carcinoma. J Gastrointest Surg. 2014;18(8):1477–85.
Nishikawa H, Arimoto A, Wakasa T, Kita R, Kimura T, Osaki Y. Effect of transcatheter arterial chemoembolization prior to surgical resection for hepatocellular carcinoma. Int J Oncol. 2013;42(1):151–60.
Renzulli M, Buonfiglioli F, Conti F, et al. Imaging features of microvascular invasion in hepatocellular carcinoma developed after direct-acting antiviral therapy in HCV-related cirrhosis. Eur Radiol. 2018;28(2):506–13.
Li Z, Lei Z, Xia Y, et al. Association of preoperative antiviral treatment with Incidences of microvascular invasion and early tumor recurrence in hepatitis B virus-related hepatocellular carcinoma. JAMA Surg. 2018; https://doi.org/10.1001/jamasurg.2018.2721.
Braunwarth E, Stattner S, Fodor M, et al. Surgical techniques and strategies for the treatment of primary liver tumours: hepatocellular and cholangiocellular carcinoma. Eur Surg. 2018;50(3):100–12.
Pereyra D, Starlinger P. Shaping the future of liver surgery: Implementation of experimental insights into liver regeneration. Eur Surg. 2018;50(3):132–6.
Zhou Y, Xu D, Wu L, Li B. Meta-analysis of anatomic resection versus nonanatomic resection for hepatocellular carcinoma. Langenbecks Arch Surg. 2011;396(7):1109–17.
Okamura Y, Ito T, Sugiura T, Mori K, Uesaka K. Anatomic versus nonanatomic hepatectomy for a solitary hepatocellular carcinoma : a case-controlled study with propensity score matching. J Gastrointest Surg. 2014;18(11):1994–2002.
Cucchetti A, Qiao GL, Cescon M, et al. Anatomic versus nonanatomic resection in cirrhotic patients with early hepatocellular carcinoma. Surgery. 2014;155(3):512–21.
Zhao H, Chen C, Fu X, et al. Prognostic value of a novel risk classification of microvascular invasion in patients with hepatocellular carcinoma after resection. Oncotarget. 2017;8(3):5474–86.
Marubashi S, Gotoh K, Akita H, et al. Anatomical versus non-anatomical resection for hepatocellular carcinoma. Br J Surg. 2015;102(7):776–84.
Kishi Y, Hasegawa K, Kaneko J, et al. Resection of segment VIII for hepatocellular carcinoma. Br J Surg. 2012;99(8):1105–12.
Hirokawa F, Hayashi M, Miyamoto Y, et al. Outcomes and predictors of microvascular invasion of solitary hepatocellular carcinoma. Hepatol Res. 2014;44(8):846–53.
Hou YF, Li B, Wei YG, et al. Second Hepatectomy improves survival in patients with microvascular invasive hepatocellular carcinoma meeting the Milan criteria. Medicine. 2015;94(48):e2070.
Mehta N, Heimbach J, Harnois DM, et al. Validation of a risk estimation of tumor recurrence after transplant (RETREAT) score for Hepatocellular carcinoma recurrence after liver transplant. JAMA Oncol. 2017;3(4):493–500.
Suh SW, Lee JM, You T, et al. Hepatic venous congestion in living donor grafts in liver transplantation: is there an effect on hepatocellular carcinoma recurrence? Liver Transplant. 2014;20(7):784–90.
Sun JJ, Wang K, Zhang CZ, et al. Postoperative adjuvant transcatheter arterial chemoembolization after R0 hepatectomy improves outcomes of patients who have hepatocellular carcinoma with Microvascular invasion. Ann Surg Oncol. 2016;23(4):1344–51.
Jin YJ, Lee JW, Lee OH, et al. Transarterial chemoembolization versus surgery/radiofrequency ablation for recurrent hepatocellular carcinoma with or without microvascular invasion. J Gastroenterol Hepatol. 2014;29(5):1056–64.
Gao Z, Du G, Pang Y, et al. Adjuvant transarterial chemoembolization after radical resection contributed to the outcomes of hepatocellular carcinoma patients with high-risk factors. Medicine. 2017;96(33):e7426.
Wang L, Wang W, Yao X, et al. Postoperative adjuvant radiotherapy is associated with improved survival in hepatocellular carcinoma with microvascular invasion. Oncotarget. 2017;8(45):79971–81.
Kadam PD, Chuan HH. Erratum to: rectocutaneous fistula with transmigration of the suture: a rare delayed complication of vault fixation with the sacrospinous ligament. Int Urogynecol J Pelvic Floor Dysfunct. 2016;27(3):505.
Finn RS, Zhu AX, Farah W, et al. Therapies for advanced stage hepatocellular carcinoma with macrovascular invasion or metastatic disease: a systematic review and meta-analysis. Hepatology. 2018;67(1):422–35.
Wang SN, Chuang SC, Lee KT. Efficacy of sorafenib as adjuvant therapy to prevent early recurrence of hepatocellular carcinoma after curative surgery: a pilot study. Hepatol Res. 2014;44(5):523–31.
Bruix J, Takayama T, Mazzaferro V, et al. Adjuvant sorafenib for hepatocellular carcinoma after resection or ablation (STORM): a phase 3, randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2015;16(13):1344–54.
Elewa MA, Al-Gayyar MM, Schaalan MF, Abd El Galil KH, Ebrahim MA, El-Shishtawy MM. Hepatoprotective and anti-tumor effects of targeting MMP-9 in hepatocellular carcinoma and its relation to vascular invasion markers. Clin Exp Metastasis. 2015;32(5):479–93.
Borderud SP, Li Y, Burkhalter JE, Sheffer CE, Ostroff JS. Electronic cigarette use among patients with cancer: characteristics of electronic cigarette users and their smoking cessation outcomes. Cancer. 2014;120(22):3527–35.
Mazzaferro V, Romito R, Schiavo M, et al. Prevention of hepatocellular carcinoma recurrence with alpha-interferon after liver resection in HCV cirrhosis. Hepatology. 2006;44(6):1543–54.
Chen R, Yu H, An Y‑L, Chen H‑J, Teng G‑J. Endothelial progenitor cells combined with cytosine deaminase-endostatin for suppression of liver carcinoma. J Biomed Nanotechnol. 2016;12(6):1174–82.
Chen K, Xia Y, Wang H, Xiao F, Xiang G, Shen F. Adjuvant iodine-125 brachytherapy for hepatocellular carcinoma after complete hepatectomy: a randomized controlled trial. PLoS ONE. 2013;8(2):e57397.
Imai K, Yamashita YI, Yusa T, et al. Microvascular invasion in small-sized hepatocellular carcinoma: significance for outcomes following hepatectomy and radiofrequency ablation. Anticancer Res. 2018;38(2):1053–60.
Meniconi RL, Komatsu S, Perdigao F, Boelle PY, Soubrane O, Scatton O. Recurrent hepatocellular carcinoma: a Western strategy that emphasizes the impact of pathologic profile of the first resection. Surgery. 2015;157(3):454–62.
Funding
This study was supported by The Key Project of Natural Science Foundation of Fujian Province (grant nos. 2016J01585 and 2016J01592) and The Army’s Logistics Medical Research Major Projects Fund Grants for Yi Jiang (grant nos. CNJ15J002 and 14ZX22); Startup Fund for scientific research, Fujian Medical University for Rui-Sheng Ke (2017XQ2048) and NO. 900 Hospital of the Joint Logistics Team Construction Special Funding for Department of Hepatobiliary Surgery (grant nos. 2014CXTD05 and 2018Q06 and 2018J02).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
R.-S. Ke, Q.-c. Cai, Y.-t. Chen, L.-Z. Lv, and Y. Jiang declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
R.-S. Ke, Q.-c. Cai, and Y.-t. Chen contributed equally to the manuscript. Yi Jiang and Li-Zhi Lv proposed ideas and designed the research. Rui-Sheng Ke, Qiu-cheng Cai, and Yong-tai Chen searched and analyzed literature. Yong-tai Chen and Rui-Sheng Ke completed the minor revision. The manuscript was drafted by Rui-Sheng Ke. All authors read and approved the final manuscript.
Rights and permissions
About this article
Cite this article
Ke, RS., Cai, Qc., Chen, Yt. et al. Diagnosis and treatment of microvascular invasion in hepatocellular carcinoma. Eur Surg 52, 55–68 (2020). https://doi.org/10.1007/s10353-019-0573-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-019-0573-1