Summary
Background
The aim of this study was to evaluate the effects of pneumoperitoneum on liver function during and after laparoscopic cholecystectomy.
Methods
This prospective study comprised a total of 165 patients, who were divided into two groups: The first group had low-pressure pneumoperitoneum (12 mm Hg; N = 78) and the second group had high-pressure pneumoperitoneum (14 mm Hg; N = 87). A detailed statistical analysis included sex, age, operation time, and liver function tests including total bilirubin, gamma-glutamyl transferase (GGT), aspartate aminotransferase (AST), alanine aminotransferase (ALT), albumin, fibrinogen, and lactate dehydrogenase (LDH), which were obtained preoperatively and 24 h, 7 days, and 30 days postoperatively. The statistical hypotheses were tested with a t test, Mann–Whitney test, chi-square test, Friedman test, and Wilcoxon’s test.
Results
There was no statistical difference between the two groups considering age, gender, and operation time (p = 0.740, p = 0.255, and p = 0.480, respectively). There was also no statistical difference in the median values of bilirubin, AST, GGT, LDH, albumin, and fibrinogen between the two groups. There was a significant statistical difference between the two groups in the median values of ALT on the 30th postoperative day (p = 0.045). There was a statistical difference for all hematochemical parameters as a function of time, independent of the level of intra-abdominal pressure (IAP).
Conclusion
There were no statistically significant differences in the values of parameters of structural damage to the liver between the two groups, but within the groups themselves. From this we conclude that both values of elevated IAP cause microstructural and functional damage to the liver.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pneumoperitoneum is one of the key elements in laparoscopic surgery that provides visual clarity and space for safe and effective surgery. However, it can cause intraoperative adverse respiratory, cardiovascular, hepatic, and renal effects [1]. Also, high-pressure pneumoperitoneum reduces portal venous flow and causes physiologic alterations in hepatic function [2, 3]. Shorter operation time and lower intra-abdominal pressure (IAP) may reduce the possibility of changes in hepatic function induced by laparoscopic surgery [1, 3].
The aim of this study was to evaluate the effects of pneumoperitoneum on liver function during and after laparoscopic cholecystectomy.
Patients and methods
In this prospective clinical study, we followed up two groups of patients with gallbladder calculosis treated at the University Clinical Center Dr. Dragiša Mišović—Dedinje in Belgrade, Serbia. Patients in both groups were operated on via laparoscopic technique in the period from April 2015 to January 2016. The study was approved by the Bioethics Committee of our hospital.
Patients included in this study had no history of previous liver disease and they exhibited normal values in preoperative liver function tests. Additional exclusion criteria were: specified heart diseases, pulmonary diseases, kidney diseases, and pregnancy. The randomization was based on sealed envelopes containing random groups: The first group had low-pressure pneumoperitoneum (12 mm Hg; n = 78) and the second group had high-pressure pneumoperitoneum (14 mm Hg; n = 87). All patients were hospitalized for 24 h.
A standardized anesthetic technique was used for all the patients with the same medications. Laparoscopic cholecystectomy was performed by using a four-trocar technique with the patient in the reversed Trendelenburg’s position (Figs. 1 and 2). The abdomen was insufflated with CO2 using an automatic insufflator. Pneumoperitoneum was created with an open technique without visual control through a small incision in the umbilical region.
All the patients were seen by the surgeons involved in this study at follow-up visits 7 days and 4 weeks after the operation in the outpatient surgical department. The detailed statistical analysis included sex, age, and operation time. Liver function tests including total bilirubin, gamma-glutamyl transferase (GGT), aspartate aminotransferase (AST), alanine aminotransferase (ALT), albumin, fibrinogen, and lactate dehydrogenase (LDH) were obtained preoperatively and 24 h, 7 days, and 30 days postoperatively. The hematochemical tests were performed at the same laboratory using only one type of device. The normal ranges for each of the aforementioned hematochemical parameters were as follows: bilirubin 3–20 umol/l, GGT 15–85 UI/l, AST 8–40 UI/l, ALT 16–63 UI/l, albumin 33–55 g/l, fibrinogen 2–4 g/l, LDH 81–234 UI/l.
Statistical data analysis was performed using IBM SPSS Statistics 22 (IBM Corporation, Armonk, NY, USA). For the analysis of the primary data, descriptive statistics and statistical methods for testing hypotheses were used. The descriptive statistical methods that were used are measures of central tendency (mean, median), measures of variability (standard deviation), and relative numbers (indices of the structure). The statistical hypotheses were tested with a t test, Mann–Whitney test, chi-square test, Friedman test, and Wilcoxon’s test. A p value of 0.05 was considered as statistically significant.
Results
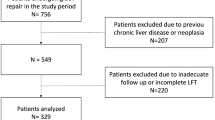
Between April 2015 and January 2016, 273 patients were admitted to the Department of Surgery, University Clinical Center Dr. Dragiša Mišović—Dedinje, Belgrade, for laparoscopic treatment of gallbladder calculosis and polyposis. Of these 273 patients, 108 (39.56%) were excluded from the study for comorbidities and for refusing participation in the study.
Low-pressure pneumoperitoneum was used in 78 patients (17 males and 61 females, age range: 28–85 years, mean age: 54.4 years) and high-pressure pneumoperitoneum was used in 87 patients (13 males and 74 females, age range: 26–76, mean age: 53.7 years). The average operation time in the low-pressure group was 59.6 min (time range: 25–330 min) and 50.3 min (time range: 20–130 min) in the high-pressure group with no statistical difference between these two groups considering age, gender, and operation time (p = 0.740, p = 0.255, and p = 0.480, respectively). Results were descriptively evaluated and are presented in Table 1 with the hematochemical characteristics of all operated patients in the aforementioned period.
When comparing the low-pressure and the high-pressure group, there was no statistical difference considering the median values of bilirubin, AST, GGT, LDH, albumin, and fibrinogen between the groups. There was a significant statistical difference between the two groups for the median values of ALT on the 30th postoperative day (0.045; Fig. 3), while the median preoperative, 24-h postoperative, and 7‑day postoperative values showed no significant difference for ALT.
There was a statistical difference for all hematochemical parameters in function of time, independent of the level of (Table 2).
Discussion
The views on the level of intra-abdominal pressure (IAP) in laparoscopic operations are not clearly defined. The range of the most frequently used IAP in gynecological laparoscopic surgery is 12–16 mm Hg [4, 5], while in urology these values are 8–20 mm Hg [6]. In abdominal laparoscopic surgery, there is no consensus on the optimal level of IAP, which ranges between 8 and 15 mm Hg [7]. Ishizaki and coauthors stated in their study that an IAP value of 16 mm Hg does not significantly reduce the blood flow through the hepatic artery; however, it diminishes the flow through the portal vein and the upper mesenteric artery, which results in a significant decrease of the total hepatic flow, while no significant changes were observed in these parameters at IAP values between 8 and 12 mm Hg [8]. In an experimental study with pigs, Blobner and coworkers used air and CO2 to create pneumoperitoneum and examined their effects on splanchnic circulation [9]. Unlike pneumoperitoneum created by insufflation of air, insufflation of CO2 led to moderate splanchnic hyperemia at IAP levels equal to or less than 12 mm Hg, while at higher IAP values, pressure-induced changes become more important than the type of gas that generates pneumoperitoneum [9].
In another experimental survey on rats, Richter and coworkers showed that higher IAP values reduce portal venous flow without compensatory increase of hepatic arterial flow, resulting in reduced hepatic pCO2 and increased ratios of ALT and AST [3].
In our study we monitored the influence of elevated IAP during laparoscopic cholecystectomy on the function and structure of the liver. Parameters indicating structural liver damage (bilirubin, AST, ALT, GGT, and LDH) with elevated IAP in laparoscopic surgery showed statistically significant differences in parameter values during the observation time for both groups, while only ALT measurement showed a statistically significant difference in median values in relation to different IAP values. By measuring ALT, we found that there is a statistically significant difference in ALT median values compared with different IAP values postoperatively after 30 days (U = 2778.5, p = 0.045). Considering functional liver damage, the albumin values obtained showed that there was no statistically significant difference in the median values compared with different IAP levels in the observation period; however, in both groups there was a statistically significant difference in albumin values in the observation time for patients operated on with an IAP of 12 mm Hg (chi-square test = 130.146; df = 3; p < 0.001) and for those operated on with an IAP of 14 mm Hg (chi-square test = 156.526; df = 3; p < 0.001). The results were identical for the fibrinogen values, which did not show a statistically significant difference in relation to different IAP levels; however, both groups showed statistically significant differences in fibrinogen values in the observation time for subjects with an IAP of 12 mm Hg (chi-square test = 69.725; df = 3; p < 0.001), and for subjects with an IAP of 14 mm Hg (chi i-square test = 44.075; df = 3; p < 0.001).
Hasukic in his study of 50 patients operated on laparoscopically for gallbladder calculoses reported an increase of ALT and AST values postoperatively in the group of patients operated on at IAP levels of 14 mm Hg [10]. Richardson and colleagues described three main determinants of blood flow through the liver: vascular resistance through the hepatic artery, mesenteric vessels, and vascular resistance through intrahepatic portal blood flow. With increased IAP in laparoscopy, vascular resistance in mesenteric blood vessels can be the main determinant of flow through the liver [11]. While most authors report that increased IAP is responsible for hepatic injury [2, 3, 10, 11] some groups claim that liver traction in extensive laparoscopic procedures can lead to hepatocyte damage [12] as well as “squeezing” of the liver tissue, which can free liver enzymes into the blood [13].
Conclusion
Our results show that there were statistically significant differences in the observed parameters of microstructural and functional damage to the liver as a function of time (increase in value for 30 days) in both study groups. There were no statistically significant differences in the values of parameters of structural damage to the liver between the two groups, but within the groups themselves. From this we conclude that both values of elevated IAP cause microstructural and functional damage to the liver.
Patients without comorbidity compensate for changes in perfusion of intra-abdominal organs without reducing their function and structure. However, for patients who have damage to the cardiovascular system, as well as the already existing damage to the function of one of the abdominal cavity organs, the reduction in perfusion due to elevated IAP could have adverse consequences. For these reasons, such patients should be carefully observed and an adequate surgical technique should be selected for solving the primary problem; in the case of laparoscopic surgery, such patients should be operated on by creating a pneumoperitoneum with lower IAP values.
References
Neudecker J, Sauerland S, Neugebauer E, et al. The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. Surg Endosc. 2002;16:1121–43.
Lai H, Mo X, Yang Y, et al. Association between duration of carbon dioxide pneumoperitoneum during laparoscopic abdominal surgery and hepatic injury: a meta-analysis. PLoS ONE. 2014;9(8):e104067.
Richter S, Olinger A, Hildebrandt U, Menger MD, Vollmar B. Loss of physiologic hepatic blood flow control (“hepatic arterial buffer response”) during CO2-pneumoperitoneum in the rat. Anesth Analg. 2001;93(4):872–7.
Singh RK, Saini AM, Goel N, Bisht D, Seth A. Major laparoscopic surgery under regional anesthesia: a prospective feasibility study. Med J Armed Forces India. 2015;71(2):126–31.
Hirvonen EA, Nuutinen LS, Kauko M. Hemodynamic changes due to Trendelenburg positioning and pneumoperitoneum during laparoscopic hysterectomy. Acta Anaesthesiol Scand. 1995;39(7):949–55.
Sassa N, Hattori R, Yamamoto T, et al. Direct visualization of renal hemodynamics affected by carbon dioxide-induced pneumoperitoneum. Urology. 2009;73(2):311–5.
Saber AA, Laraja RD, Nalbandian HI, Pablos-Mendez A, Hanna K. Changes in liver function tests after laparoscopic cholecystectomy: not so rare, not always ominous. Am Surg. 2000;66(7):699–702.
Ishizaki Y, Bandai Y, Shimonura K, Abe H, Ohtomo Y, Idezuki Y. Safe intraabdominal pressure of carbon dioxide pneumoperitoneum during laparoscopic surgery. Surgery. 1993;114(3):549–54.
Blobner M, Bogdanski R, Kochs E, Henke J, Findeis A, Jelen-Esselborn S. Effects of intraabdominally insufflated carbon dioxide and elevated intraabdominal pressure on splanchnic circulation: an experimental study in pigs. Anesthesiology. 1998;89(2):475–82.
Hasukic S. Postoperative changes in liver function tests. Randomized comparison of low- and high-pressure laparoscopic cholecystectomy. Surg Endosc. 2005;19:1451–5.
Richardson PD, Withrington PG. Liver blood flow. Intrinsic and nervous control of liver blood flow. Gastroenterology. 1981;81(1):356–75.
Jeoung GA, Cho GS, Shin EJ, Lee MS, Kim HC, Song OP. Liver function alterations after laparoscopy assisted gastrectomy for gastric cancer and its clinical significance. World J Gastroenterol. 2011;17:372–8.
Tan M, Xu FF, Peng JS, et al. Changes in the level of serum liver enzymes after laparoscopic surgery. World J Gastroenterol. 2003;9:364–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Z. Zagorac, R. Zivic, M. Milanovic, B. Vekic, B. Dakovic, Z. Bukumiric, and D. Radovanovic declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zagorac, Z., Zivic, R., Milanovic, M. et al. Changes in liver function tests after laparoscopic cholecystectomy with low- and high-pressure pneumoperitoneum. Eur Surg 51, 61–65 (2019). https://doi.org/10.1007/s10353-019-0568-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-019-0568-y