Summary
Background
Although there are numerous modalities to evaluate perianal fistula, there is still a need to determine the most sensitive, specific, and accurate modality. This study was conducted to determine the performance characteristics of magnetic resonance imaging (MRI) and contrast-enhanced three-dimensional endoanal ultrasonography (C-3DEAUS) considering surgery as the gold standard.
Methods
A total of 36 patients who were diagnosed of having anal fistula with 10-MHz hydrogen peroxide-enhanced three-dimensional EAUS underwent MRI followed by surgery. Both of tests were done the day before surgery. Fistula classification was determined with each modality according to Parks’ criteria as inter-sphincteric, trans-sphincteric, extra-sphincteric, or supra-sphincteric and was compared with the surgical findings in all patients. If the accuracy of each modality was at least 85 % compared with the surgery, it was considered as clinically useful.
Results
Agreement for the classification of the primary fistula tract was 94.3 % for C-3DEAUS and surgery, 97.1 % for MRI and surgery. Considering a clock face, C-3DEAUS and surgery agreed in location of internal opening in 88.6 % of cases while MRI and surgery agreed in 97.1 %. In detection a collection, agreement between C-3DEAUS and surgery was 82.9 %, and 97.1 % between MRI and surgery.
Conclusions
Both methods had almost perfect agreement with surgical findings in the classification of the primary fistula tract but MRI had more agreement in distinguishing other aspects of a fistula and it can be used as the most reliable method for preoperative evaluation of perianal fistulas.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An anal fistula is a hollow tract that connects two epithelial surfaces with an internal anorectal and an external opening in the perianal area. Crohn’s disease, pelvic infection, tuberculosis, diverticulitis, trauma during childbirth, pelvic malignancy, and radiation therapy or cryptoglandular infection arising from perianal abscess are common reasons of fistulas. However, most are idiopathic representing the chronic phase of intramuscular anal gland sepsis [1, 2]. Symptoms ranging from minor discomfort and drainage generally affect quality of life significantly [2]. Considering the Parks’ classification, fistulas are classified into four groups: intersphincteric, trans-sphincteric, supra-sphincteric, and extra-sphincteric [2].
The anal fistula prevalence has approximately 0.01 % worldwide affecting young adults predominantly [3], with a male-to-female ratio of approximately 2:1 [1].
Surgery is the typical management of fistula related with various complications such as postoperative incontinence and recurrence [4]. Accurate preoperative definition of the anatomy of the tract and the location of any extension or abscesses are required to have a successful surgery [1, 5].
Radiologic studies are performed to evaluate fistula when the primary opening is difficult to identify or for recurrent or persistent disease. Several imaging diagnostic modalities such as fistulography, barium enema, computed tomography (CT)-scan, endoscopic ultrasonogpahy, and magnetic resonance imaging (MRI) are available to evaluate anal fistulas. Imaging with fistulography, barium enema, and CT scan is not sufficiently accurate to be clinically useful while endoscopic ultrasonography and MRI has been shown to be more accurate in evaluation of perianal fistulas [6–9]. Although MRI has superseded endoscopic ultarsonogrphy [1], a relatively low accessibility and high price of MRI limit its common use as a diagnostic method [10].This study was performed to evaluate the diagnostic accuracy of MRI and hydrogen peroxide contrast-enhanced endoanal ultrasonography (C-EAUS) in detection and characterization of perianal fistulas in comparison to surgery as the gold standard. Although the numerous papers were previously published on this topic, we used updated MRI and endoanal ultrasound techniques in our study to improve diagnostic accuracy of these tests.
Methods and materials
Study subjects selection
A census of 36 patients with symptomatic diagnosis of anal fistula who referred to the colorectal division, department of surgery of Rasool-Akram hospital, Iran University of Medical Sciences from December 2013 to February 2015 were enrolled in the study. After giving an informed consent, the subjects underwent hydrogen peroxide C-EAUS and gadolinium-contrast MRI studies before surgery. Both tests were done the day before surgery. Exclusion criteria were having contraindication for MRI including claustrophobia, pacemaker, metal pin and having contraindication for use of gadolinium-based contrast: renal failure and liver failure, pregnancy, lactation and severe pain in patients who can not tolerate endoanal ultrasonography. A colorectal surgeon who blind to the results of MRI with about 8 years of experience in endoanal ultrasonography performed all contrast-enhanced endoanal ultrasonographies. In all cases, a second colorectal surgeon performed the surgical operations and categorizations of the fistulae. The radiologist who interpreted the MRIs was blind to the results of C-EAUS and the operating surgeon who described the characteristics of the fistulae was blind to the results of both C-EAUS and MRI too.
The study was approved by the Institutional Review Board of Tehran University of Medical Sciences.
Contrast-enhanced endoanal ultrasonography
The investigation was performed with the patient in sim’s position (left lateral decubitus) without any bowel preparation. A 10-MHz rotating 360 ° ultrasound endoanal probe (type 2052, BK, Pro Focus UltraView 2202, Copenhagen, Denmark) was covered in a latex condom containing degassed gel to obtain maximum image quality.
The procedure was performed in three steps. First, Iodine topical solution was used to identify and clean the perianal fistular openings while the patient was in the left lateral position. For the purpose of contrast solution (hydrogen peroxide) injection, the external fistular opening was cannulated using an 18-gauge plastic cannula and tape-fixed to the skin surface. To locate the external opening when it was not obvious, the soft catheter was firmly probed into the center of a focal elevated erythematous region adjacent to the external fistular opening where the skin was fragile. Then, a conventional ultrasound examination without injection of contrast solution using the rotating endoanal probe was performed. In the next step, without dislodging the cannula, the images were recorded slowly along the entire length of the anal canal with slow pressure injection of 1.0– 2.0 ml of 3 % hydrogen peroxide to visualize the fistula tract, its extension and internal opening and three-dimensional images were obtained after computerized reconstruction.
Fistulae were categorized according to Park’s classification. Hypoechogenic abnormal structures beyond the primary tract were identified as extension or abscess. The categorization of the fistulae was as follows:
The primary tract was classified as inter-sphincteric, trans-sphincteric, supra-sphincteric, or extra-sphincteric according to the Park’s classification system [2].
The position of internal opening was described as clock and level (upper, mid, lower part of the anal canal).
-
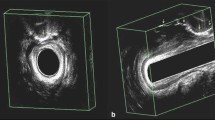
Presence or absence of extension of fistula and/or abscess was also indicated.(Fig. 1)
Contrast-enhanced magnetic resonance imaging
The MRI examinations were performed with 1.5 T MR machine (Avanto, Siemens, Erlongen-Germany) using body phased array coils with no special preparation consisting of the following sequences with 250 field of view before and after gadolinium-based contrast material:
-
Oblique axial T1-weighted fast spin-echo (FSE) sequences with the following parameters: repetition time (tr) msec/echo time (te) msec, 682/10, 3-mm section thickness, 1.4 mm gap, 228 × 256 matrixes.
-
Oblique axial fat suppressed (FS), T1-weighted FSE sequences: tr/te, 655/10, 3-mm section thickness, 2.2 mm gap, 240 × 320 matrixes.
-
Oblique coronal FS T1-weighted FSE sequences: 620/10, 3-mm section thickness, 0.7 mm gap, 205 × 256 matrixes.
-
Oblique axial T1-tirm FSE sequences: 4030/32, 3-mm section thickness, 1.4 mm gap, 228 × 256 matrixes.
-
Oblique axial T2-weighted FSE sequences: 3300/100, 3-mm section thickness, 0.5 mm gap, 205 × 256 matrixes.
-
Oblique coronal T2-weighted FSE sequences: 4860/105, 3.5-mm section thickness, 0.4 mm gap, 207 × 256 matrixes.
-
Sagittal T2-weighted FSE sequences: 5750/101, 3-mm section thickness, 0.7 mm gap, 230 × 256 matrixes.
-
Sagittal FS T2-weighted FSE sequences: 6010/98, 3.5-mm section thickness, 0.7 mm gap, 205 × 256 matrixes.
-
Oblique axial FS T2-weighted FSE sequences: 5210/98, 3.5-mm section thickness, 0.5 mm gap, and 205 × 256 matrixes.
Intravenous injection of gadobutrol (Gadovist; bayer Schering pharma, Berlin, Germany) was performed with a power injector with a mean dose of 0.1 ml/kg body weight.(Fig. 2)
Magnetic resonance imaging. A 47-year-old man with trans-sphincteric fistula and ischiorectal collection. a coronal contrast-enhanced fat-suppressed T1-weighted MR image and, b axial T1-tirm fast spin-echo show the trans-sphincteric fistula (arrow) crossing the external sphincter and collection (arrow head) in the left ischiorectal fossa
The digital MR images were evaluated by one experienced radiologist who had more than 10 years of experience with pelvic MRI at referral center of anal fistula imaging at the commencement of the study. The same criteria was used to categorize the anatomy of the fistulae as those which were applied for C-EAUS.
Surgery
After mechanical colonic preparation with laxatives for 24 h, surgery was performed. All patients received prophylactic intravenous ceftizoxime (1 g) and metronidazole (500 mg) just before operation. In operating room, the patient was placed in lithotomy position. Under regional or general anesthesia, the proctoscope was inserted. Then, the possible primary tract was palpated; and a special probe was inserted through the external opening to reach the internal opening. In cases where the internal opening was not located, hydrogen peroxide solution was used to visualize the anal canal.
The location of the primary tract, type of the perianal fistula, presence and position of internal opening and presence of extension and/or abscess were determined. Eventually, fistulectomy or fistulotomy was done using a layed open technique.(Fig. 3)
Considering the location of extensions in relation to sphincters, they were either drained or curreted.
Statistical analysis
Statistical analysis was performed using STATA IC version 13.1 for Windows (STATA Corp., TX, USA). Numerical variables were summarized as mean ± standard deviation and categorical variables were summarized as frequency (percentage). Performance characteristics (sensitivity, specificity, positive predictive value, and negative predictive value with 95 % confidence intervals [CIs]) for C-EAUS and MRI in categorizing the anatomy of the fistula and presence or absence of anatomical extension and abscess were evaluated compared with the results of surgery as the gold standard test. Inter-rater agreement analysis for two unique raters was used to evaluate agreement between each of C-EAUS and MRI with surgery. Cohen’s Kappa values with the significance level for its difference from 0 were determined. In fact, Cohen’s Kappa between 0.61 and 0.80 indicates a substantial agreement, and the value between 0.81 and 1.0 demonstrates an almost perfect or perfect agreement [11]. Sensitivity and specificity of C-EAUS and MRI were compared using McNemar’s Chi2 test. p Values less than 0.05 were considered as statistically significant in all analyses.
Results
The subjects’ baseline characteristics are summarized in Table 1. From a total of 36 enrolled patients, 27 had trans-sphincteric fistula and 8 had inter-sphincteric fistulas in their surgery report. The only subject with supra-sphincteric type of fistula was excluded from the analyses. Finally, data from 35 subjects (23 men and 12 women; mean age 39.8 ± 13.5 years) were included in the analyses. From these cases, 11 patients had previous surgeries for fistulas (nine fistula surgery and two for abscess drainage). All fistulae were due to cryptoglandular infection and the patients did not have any other risk factors. In this study there was no patient with horseshoe extension. In all, 14 cases (40.0 %) were reported to have abscess collection around the fistula, and 13 subjects (37.1 %) had an extended fistula tract. The location of the internal opening of the fistulae was determined precisely in 31 cases (88.6 %) with C-EAUS and in 34 subjects (97.1 %) with MRI.
Inter-rater agreement
The results of inter-rater agreement analysis are demonstrated in Table 2. C-EAUS categorized all 27 (100 %) trans-sphincteric and 6 out of 8 (66.7 %) inter-sphincteric fistulas correctly. In fact, C-EAUS showed almost perfect or perfect agreement with surgery in distinguishing trans-sphincteric from inter-sphincteric types of fistulae (agreement: 94.3 %, kappa: 0.82). Categorizing all 27 (100 %) trans-sphincteric and 7 out of 8 (87.5 %) inter-sphincteric fistulae correctly, MRI showed a perfect agreement with surgery (agreement: 97.1 %, kappa: 0.91).
Test performance characteristics
Table 3 demonstrates test performance characteristics for C-EAUS and MRI and comparison of their sensitivities and specificities. In determining anatomy of the fistular tract, C-EAUS and MRI showed the same level of sensitivity (100 % for both tests). However, MRI had higher specificity although the difference was statistically nonsignificant (87.5 vs. 75.0 %; p = 1.000). Both tests had similar levels of positive and negative predictive values (PPV: 93.1 and 96.4 % for C-EAUS and MRI, respectively; and NPV: 100 % for both tests). In distinguishing other aspects of fistulae, C-EAUS and MRI showed similar levels of performance characteristics except for that MRI showed better specificity than C-EAUS in showing a peri-fistular abscess collection with borderline significance of difference (100 vs. 76.2 %, p = 0.062). Also, sensitivity of MRI in showing the existence of a fistular tract extension was higher although with statistically nonsignificant difference (92.3 vs. 76.9 %; p = 0.625).
Discussion
Mostly all anal fistulas are easily managed surgically [12] while high risk of complications such as recurrence or sphincter damage resulting fecal incontinence always exist for complex and recurrent fistula [13]. Thus, to have a successful surgery the anatomy of the tract and the location of any extension or abscesses should be defined accurately before surgery.
The current study examined the performance characteristics and agreement of C-EAUS and MRI with surgery to determine the most accurate modality to assess perianal fistulas. In this study, the average wait time between C-EAUS, MRI, and surgery was short. Both of tests were done the day before surgery. Finally, the results showed that C-EAUS and MRI exceeded the prespecified threshold of 85 % accuracy compared with surgery. Consistent with the results of meta-analysis that was conducted by Siddiqui et al [14], the current study demonstrated that two diagnostic modalities had comparable accuracy in assessment of perianal fistula; however, all other components of performance characteristics of diagnostic modalities were higher in MRI compared with EAUS.
In this study, the results showed that the agreement of peroxide-enhanced three-dimensional EAUS with surgery for the classification of the primary fistula tract was almost perfect and it had a substantial agreement level in distinguishing other aspects of a fistula; while different studies reported a wide range of accuracy and performance characteristics for EAUS in detection of primary tract, internal opening, and extension [15, 16]. This may be due to differences in the criteria used, differences in operator experience, differences in the complexities of fistulas, and differences in the EAUS techniques. In addition to the use of high-frequency transducers and three-dimensional technology, using H2O2 as a contrast may be the most effective reason to improve the accuracy of EAUS [15]. Many other studies confirmed the superiority of H2O2-enhanced EAUS compared with unenhanced studies [4, 17].
Peroxide-enhanced EAUS improves detection of fistula tract via visualizing the tract more obviously especially in difficult cases such as supra-sphincteric fistula tract and recurrent fistulas in which accurate anatomical assessment is pivotal [15]. Consequently, performing H2O2-enhanced EAUS in difficult cases may be more economical and helpful. Although H2O2 infusion is generally safe, several complications may happen mainly due to large infusion volume or forceful infusion [18, 19]. Of note, no patient in this study complained of symptoms related to H2O2 infusion. Thus, the high accuracy and safety of three-dimensional peroxide-enhanced EAUS may make it a choice in the preoperative assessment of fistula due to its easy use, low cost as well as its usefulness in routine clinical practice. However, different studies used MRI with body coils in assessment and classification of anal fistula [1, 20, 21]. It may provide further information on perianal anatomy and structures of anal fistula as well as active tracts and healed or scar tissue compared with EAUS [22, 23]. The accuracy of MRI was investigated in different studies with reported sensitivities of 86 − 97 % [6, 24, 25]. These results are in line with the current study. Hussain et al. [8] and Lunniss et al. [6] reported a sensitivity of 61–65 % for EAUS and 85–89 % for MRI using a body coils or endoanal coils in two studies comparing EAUS and MRI.
In a similar study that was conducted by West et al. [26], three-dimensional EAUS were compared with MRI using endoanal coils. Although the results were comparable in both modalities, the technique of MRI was different from the current study that was MRI with body phased array coils. Considering the study of Halligan et al. [27], MRI with body coils is more accurate and has a larger field of view than MRI with endoanal coils and is tolerated easier. Some other studies compared MRI with EAUS; two studies found MRI superior to EAUS in classification of the primary tracts, localizing the internal opening and detecting collections or extensions [8, 20]; while in a study that was conducted by Orsoni et al., EAUS was more accurate than MRI in diagnosing fistula and in agreement with surgery in 82 % compared with 50 % for MRI [20, 23]. EAUS and MRI, along with various other modalities, can provide valuable diagnostic information. However, MRI is not operator dependent, it is a safe and painless test, and the images can then be examined on a computer monitor, transmitted electronically, printed or copied to a CD [28].
Conclusion
In conclusion, this study showed that peroxide-enhanced three-dimensional EAUS and MRI both had almost perfect agreement with surgical findings in the classification of the primary fistula.
In addition, although C-EAUS showed a substantial agreement level in distinguishing other aspects of a fistula (existence of peri-fistular abscess collection and fistular tract extension), MRI had a perfect agreement with surgery and it can be used as the most reliable methods for preoperative evaluation of perianal fistulas, in complex tracts and when EAUS cannot be tolerated or definitely confirm the diagnosis. EAUS could be considered for simple tracts and in case of any contraindication of doing MRI or lacking expertise in its interpretation.
Limitation
The most important limitation of our study was the small sample size. Therefore, further studies are needed to be conducted with larger sample size to determine the most accurate modality in assessment of perianal fistula. Another limitation of the study was operator-dependent nature of these tests.
Contribution of authors
Designing and implementing of the study protocol, data gathering, analysis, supervising of project and manuscript drafting were performed by Mahyar Ghafoori, Bahar Mahjoubi, Hossein Youseffam, Mina Mollabashi, and Hajar Nikbakht. All authors read and approved the final manuscript.
Funding
This study was part of Mina Mollabashi dissertation supported by Tehran University of Medical Sciences.
Conflict of interest
M. Ghafoori, B. Mahjoubi, H. Youseffam, M. Mollabashi, and H. Nikbakht declare that there are no actual or potential conflicts of interest in relation to this article.
References
de Miguel CJ, del Salto LG, Rivas PF, et al. MR imaging evaluation of perianal fistulas: spectrum of imaging features. Radiographics. 2012;32(1):175–94.
Poggio JL. Fistula-in-Ano. http://emedicine.medscape.com/article/190234-overview. Accessed 25 Nov. 2015.
Sainio P. Fistula-in-ano in a defined population. Incidence and epidemiological aspects. Ann Chir Gynaecol. 1984;73(4):219–24.
Ratto C, Gentile E, Merico M, et al. How can the assessment of fistula-in-ano be improved? Dis Colon Rectum. 2000;43(10):1375–82.
Kruskal JB, Kane RA, Morrin MM. Peroxide-enhanced anal endosonography: technique, image interpretation, and clinical applications. Radiographics. 2001;21(Spec No):173–89.
Lunniss PJ, Barker PG, Sultan AH, et al. Magnetic resonance imaging of fistula-in-ano. Dis Colon Rectum. 1994;37(7):708–18.
Tto T, Mulder C, Wijers O, et al. Endosonography of peri-anal and pericolorectal fistula and/or abscess in Crohn’s disease. Gastrointest Endosc. 1990;36(4):331–36.
Hussain SM, Stoker J, Schouten WR, et al. Fistula in ano: endoanal sonography versus endoanal MR imaging in classification. Radiology. 1996;200(2):475–81.
Chapple MK, Spencer J, Windsor A, et al. Prognostic value of magnetic resonance imaging in the management of fistula-in-ano. Dis Colon Rectum. 2000;43(4):511–16.
Waniczek D, Adamczyk T, Arendt J, et al. Usefulness assessment of preoperative MRI fistulography in patients with perianal fistulas. Pol J Radiol. 2011;76(4):40–4.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Maier AG, Funovics MA, Kreuzer SH, et al. Evaluation of perianal sepsis: comparison of anal endosonography and magnetic resonance imaging. J Magn Reson Imaging. 2001;14(3):254–60.
Sangwan YP, Rosen L, Riether RD, et al. Is simple fistula-in-ano simple? Dis Colon Rectum. 1994;37(9):885–9.
Siddiqui MR, Ashrafian H, Tozer P, et al. A diagnostic accuracy meta-analysis of endoanal ultrasound and MRI for perianal fistula assessment. Dis Colon Rectum. 2012;55(5):576–85.
Kim Y, Park YJ. Three-dimensional endoanal ultrasonographic assessment of an anal fistula with and without H(2)O(2) enhancement. World J Gastroenterol. 2009;15(38):4810–5.
Navarro-Luna A, García-Domingo MI, Rius-Macías J, et al. Ultrasound study of anal fistulas with hydrogen peroxide enhancement. Dis Colon Rectum. 2004;47(1):108–14.
Poen A, Felt-Bersma R, Eijsbouts Q, et al. Hydrogen peroxide-enhanced transanal ultrasound in the assessment of fistula-in-ano. Dis Colon Rectum. 1998;41(9):1147–52.
Schwab C, Dilworth K. Gas embolism produced by hydrogen peroxide abscess irrigation in an infant. Anaesth Intensive Care. 1999;27(4):418–20.
Tsai SK, Lee TY, Mok MS. Gas embolism produced by hydrogen peroxide irrigation of an anal fistula during anesthesia. Anesthesiology. 1985;63(3):316–7.
Orsoni P, Barthet M, Portier F, et al. Prospective comparison of endosonography, magnetic resonance imaging and surgical findings in anorectal fistula and abscess complicating Crohn’s disease. Br J Surg. 1999;86(3):360–4.
George U, Sahota A, Rathore S. MRI in evaluation of perianal fistula. J Med Imaging Radiat Oncol. 2011;55(4):391–400.
Schwartz DA, Wiersema MJ, Dudiak KM, et al. A comparison of endoscopic ultrasound, magnetic resonance imaging, and exam under anesthesia for evaluation of Crohn’s perianal fistulas. Gastroenterology. 2001;121(5):1064–72.
Gustafsson UM, Kahvecioglu B, Astrom G, et al. Endoanal ultrasound or magnetic resonance imaging for preoperative assessment of anal fistula: a comparative study. Colorectal Dis. 2001;3(3):189–97.
Spencer JA, Ward J, Beckingham I, et al. Dynamic contrast-enhanced MR imaging of perianal fistulas. AJR Am J Roentgenol. 1996;167(3):735–41.
Barker P, Lunniss P, Armstrong P, et al. Magnetic resonance imaging of fistula-in-ano: technique, interpretation and accuracy. Clin Radiol. 1994;49(1):7–13.
West R, Zimmerman D, Dwarkasing S, et al. Prospective comparison of hydrogen peroxide–enhanced three-dimensional endoanal ultrasonography and endoanal magnetic resonance imaging of perianal fistulas. Dis Colon Rectum. 2003;46(10):1407–15.
Halligan S, Bartram C. MR imaging of fistula in ano: are endoanal coils the gold standard? AJR Am J Roentgenol. 1998;171(2):407–12.
Radiological Society of North America. Magnetic Resonance Imaging (MRI). http://www.radiologyinfo.org/en/info.cfm?pg=spinemr. Accessed 4 Nov. 2014.
Author information
Authors and Affiliations
Corresponding author
Additional information
The manuscript has not been a podium or poster meeting presentation.
Rights and permissions
About this article
Cite this article
Ghafoori, M., Mahjoubi, B., Youseffam, H. et al. Magnetic resonance imaging and peroxide-enhanced anal endosonography in assessment of fistula in anus: comparison with surgery. Eur Surg 48, 39–46 (2016). https://doi.org/10.1007/s10353-015-0380-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-015-0380-2