Summary
Background
Primary spontaneous pneumothorax (PSP) is a common medical condition in the emergency department. Clinically stable patients with large pneumothoraces usually undergo chest tube drainage. During the course of hospital stay, several chest X-rays are ordered at various time points. Because the number of chest X-rays during diagnosis and management of PSP can be quite high and lung ultrasound has a proven efficacy for the assessment of lung re-expansion, we decided to investigate the use of lung ultrasound for the management and decision-making regarding chest drains for PSP.
Material and methods
A total of 25 patients with PSP were evaluated. A comparison between chest X-rays and lung ultrasound was made at four different time points during patient hospitalization (T1—immediately after drainage, T2–third or fourth post-drainage day, T3—before chest tube removal, T4—after chest tube removal). The rate of agreement between the two investigations was analyzed, as their result impacts decision-making regarding chest tube management and removal.
Results
Overall, positive and negative agreements were high in all time points, except time point 3. Calculated p values using Fisher’s and Barnard’s test were also good for time points 1, 2, and 4 (< 0.05).
Conclusions
For all time points except the third, we can safely reject the null hypothesis, thereby arriving at the conclusion that lung ultrasound can substitute chest X-rays after tube drainage of PSP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Primary spontaneous pneumothorax (PSP) is a collection of air in the pleural space that occurs in patients without an underlying lung disease. It is a common medical condition especially in the emergency department. Its reported incidence is 18–28/100,000 cases per year for men and 1.2–6/100,000 for women [1]. It usually occurs in young, tall, thin male individuals; it rarely occurs after the age of 40 years. Cigarette smoking increases the risk of PSP in a dose-dependent manner, by as much as a factor of 20. Clinically stable patients with large pneumothoraces usually undergo a procedure to re-expand the lung (usually chest tube drainage) and are hospitalized. Although its management accounts for a high health-care cost [2], generally accepted guidelines do not exist, and observational studies show extensive practice variations in management [3]. In addition to diagnostic imaging (chest X-ray or CT), several imaging studies (mostly X-rays) are performed after chest tube drainage. Chest X-rays could be ordered, according to local protocols, for confirming correct positioning of the chest tube, for routine follow-up, after clamping the chest tube, before and after chest tube removal. Prerequisites for a safe chest tube removal are demonstrating by imagery that the lung has re-expanded and that there is no clinical evidence of air leak [4].
There is an increasing interest for the use of ultrasound in diagnosing and managing lung conditions in recent years. Ultrasound presents multiple advantages: it uses no radiation, it is inexpensive, it can be used at the bedside, it is noninvasive and can be repeated as necessary. While it is especially useful for the study of bedridden, critically ill patients, it is a method that is starting to be used by professionals, other than radiologists, with specific clinical questions [5]. Lung ultrasound can be used to evaluate pleural effusions and masses and lung parenchyma. Its learning curve is relatively short compared with that of other sonographic techniques [6]. Lung ultrasound (LUS) is well-suited for the diagnosis of pneumothorax, yielding better results than conventional chest X-ray [7]. Despite its proven efficacy, controversy regarding diagnostic accuracy continues and there seems to be a narrow knowledge base regarding technical aspects of LUS [8].
The aim of this study was to investigate the use of LUS for the management and decision-making regarding chest drains for PSP.
Material and methods
PSP is a relatively common disease in our emergency department. We will describe our current management protocol. After diagnosis by X-ray or computed tomography of a large pneumothorax, as defined by the ACCP [4] as a pneumothorax with a distance from apex to cupola larger or equal to 3 cm, a chest tube of 18 Fr is placed in the pleural space under local anesthesia and attached to a water seal device. A chest X-ray is obtained in the first 30 min after the insertion of the chest tube for confirmation of correct positioning. The patient is then admitted for clinical surveillance until the chest tube can be safely removed. If the patient presents an air leak a few hours after the procedure, the drain is connected to aspiration. If air leaks continue for more than 48 h, patients are proposed for surgery. For the patients that do not present air leaks, a follow-up X-ray is obtained in the third or fourth day following drainage. The tube is clamped on the fifth postoperative day if no air leaks are detected and the previous X-ray showed lung re-expansion or small pneumothorax. Another chest X-ray is obtained on day 6 and, if the lung is expanded, the chest tube is removed. Another X-ray is obtained to rule out recurrence due to potential chest tube removal accidents, and the patient is discharged. We choose to drain for at least 6 days regardless of good clinical course to obtain further pleural apposition.
For an uncomplicated clinical course (no air leaks and lung expansion detected by imagery), four chest X-rays are obtained. Considering the use of LUS for the diagnosis of pneumothorax, we asked an independent clinician, trained in lung ultrasound, to evaluate the state of lung expansion by LUS at the four different time points (T1—immediately after drainage, T2—third or fourth post-drainage day, T3—before chest tube removal, T4—after chest tube removal). As decision-making in managing a chest tube takes into account the presence or absence of air leaks, which can be evaluated clinically, and lung re-expansion, LUS was required to determine if the lung was expanded or not, without any attempts of size assessment.
LUS can be performed using any available bi-dimensional scanner. Probe selection is easy and essentially a non-factor, considering that all probes provide sufficient information. However, higher frequency probes and macro probes are better suited for superficial explorations, that is, the pleural surface and its pathologies (and should be preferred for pneumothorax). The maximum effectiveness of the method is best achieved by what is known as “point-of-care ultrasound”, and by a clinically-driven and focused assessment. With the patient in the supine position, the area of interest, the least-dependent part of the chest, is roughly represented by the third-fourth intercostal spaces, between the parasternal and mid-clavicle lines. The probe should be placed perpendicular to the direction of the intercostal space, allowing the visualization of at least two ribs and the corresponding intercostal space. This is important because it allows inexperienced users to quickly identify the main target, the parietal pleura [9]. The parietal pleura appears as a thin echogenic line between and below two adjacent ribs (“the bat sign”, Fig. 1). After the identification of the pleural line, the probe may be rotated as to correspond to the long axis of the intercostal space (the oblique plane). Often, it is necessary to scan more intercostal spaces by moving the probe inferiorly and laterally. This can give an estimate of the extension of the pneumothorax or confirm the diagnosis. At this moment, LUS is not recognized as a method to differentiate between large and small pneumothorax.
A 10 MHz linear probe is used. We selected the probe due to its ability to evaluate the pleural line, which is superficial, better than the convex or micro-convex, lower frequency probes. The patient is placed supine and the area of interest, the least dependent, is the anterior and inferior part of the chest, approximately the third and fourth intercostal spaces between the parasternal and mid-clavicular lines. The examination plane is longitudinal, parallel with the long axis of the body, as this allows easy identification of the pleural line. The probe is then moved laterally and inferiorly on the chest wall. The physician is asked to give one of the following diagnoses: “expanded lung” or “pneumothorax.”
The study population consisted of 25 patients admitted and managed in our department in the period January–December 2014. All patients had a diagnosis of primary spontaneous pneumothorax by X-ray and clinical assessment. All 25 selected patients had a good clinical course. Patients that presented air leaks for more than 48 h or were proposed for surgery, seven cases, were excluded. All patients had chest X-rays and LUS performed at each one of the four time points. The data obtained from X-rays and LUS were compared. Clinical decision-making was based on X-rays and clinical course. All ultrasounds were performed by the same investigator.
The statistical methods available for the comparison of two diagnostic tests were carefully taken into consideration [10, 11]. For each time point overall, positive and negative agreement values were calculated. Overall agreement is the percent in which both the ultrasound and the X-ray found either a collapsed or an expanded lung. Positive agreement is the percent in which both X-ray and ultrasound found an expanded lung. Negative agreement is the percent in which both the X-ray and the ultrasound found a collapsed lung.
Two sets of exact tests were run on the data obtained from clinical practice. The tests assume that the null hypothesis represents complete independence between the variables, that is, there is significant difference between the two methods. A rejection of this hypothesis would therefore entail that both methods can be used interchangeably, there being no statistically significant difference between the two.
Statistical significance is described for an acceptable level of a type I error α (meaning the probability of rejecting a null hypothesis that is actually true). The confidence level is obtained by subtracting this from unity. The standard confidence level is considered to be 95 % with a corresponding value of 0.05 for α, which are the set values for the two tests.
Fisher’s exact test and Barnard’s test compute a two-tailed p value, which is then compared with the α threshold for each of the four time points. The correct interpretation of the p value is the likelihood that, assuming the null hypothesis were true, an event of equal or greater severity (i.e., improbability) as the one described by the given data would take place [12]. This helps in allowing the null hypothesis to be rejected for p values less than the α set value. It should be noted that p values exceeding the threshold value are held to be inconclusive, not proof of validity of the null hypothesis.
As regards the tests, Barnard is now widely considered to be the more powerful of the two, though it has historically been the less used mainly due to its high computational requirements, which is no longer an issue with the advent of powerful computers.
Results
In all, 25 patients with PSP were included in the study. There were 23 male and 2 female patients with a mean age of 27 years. Average BMI for the studied population was 19.6 kg/m2. In total, 24 patients were smokers at the time of the diagnosis, 22 male and two female patients. A total of 17 patients were from an urban environment. Data comparison will be discussed for the four different time points.
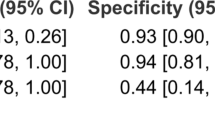
At the first time point, immediately after chest tube insertion, the results were as follows. LUS identified 19 expanded lungs and 6 pneumothoraces. Chest X-ray found 22 expanded lungs and 3 pneumothoraces. The three cases of pneumothorax identified by chest X-ray were also recorded on LUS. Overall agreement was 88 %, positive agreement was 93 %, negative agreement was 67 %, p = 0.004. The cases that showed pneumothorax on chest X-ray were connected to aspiration. Two of the three cases of pneumothorax diagnosed by chest X-ray presented small air leaks that subsided by the fourth post-drainage day. The three additional cases of pneumothorax identified by LUS did not show signs of air leak.
At the second time point, on the third or fourth day after chest tube insertion, the results were as follows. LUS identified 23 expanded lungs and 2 pneumothoraces. Chest X-ray found 22 expanded lungs and 3 pneumothoraces, the same three cases identified at the previous time point, of which LUS missed one. As their size was very small, less than 1 cm from the cupola to apex, their clinical course was unaffected. Overall agreement was 96 %, positive agreement was 98 %, negative agreement was 80 %, p = 0.005.
At the third time point, 24 h after the clamping of the chest tube and on the day of removal, the results were as follows. LUS found 22 expanded lungs and 3 pneumothoraces. Chest X-ray found 24 expanded lungs and 1 pneumothorax. The pneumothorax seen by X-ray was also identified by LUS. Overall agreement was 92 %, positive agreement was 96 %, negative agreement was 50 %, p = 0.06. As the pneumothorax was very small, it did not affect clinical course. The two cases identified by LUS and not by chest X-ray were considered very small, patients were in good clinical condition, so clinical course was not affected.
At the fourth time point, immediately after chest tube removal, the results were as follows. LUS found 22 expanded lungs and 3 pneumothoraces. Chest X-ray found 23 expanded lungs and 2 pneumothoraces, both small in size with patients in good general condition, and their discharge was uneventful. The three cases identified by ultrasound were the same as at the previous time point. Overall agreement was 96 %, positive agreement was 98 %, negative agreement was 80 %, p = 0.005. A summary of the data is presented in Table 1.
All patients returned for follow-up 1 month after discharge. Clinical and radiologic evaluation at this time showed no recurrences and no re-admissions were recorded.
The values obtained for the tests on the four time points of data are listed in Table 2.
Discussion
Standard textbooks state “ultrasound energy is rapidly dissipated by air, ultrasound imaging is not useful for the evaluation of the pulmonary parenchyma” [13]. In effect, for a long time, ultrasound was not deemed useful, and furthermore, not used for the evaluation of lung or pleural diseases. The presence of air causes a complete reflection of the ultrasound beam and prevents the creation of a direct image. However, in the past 2 decades, LUS has emerged as a useful tool and beginning with pleural effusions and masses is now moving steadily toward imaging of the lung parenchyma.
Numerous authors have documented the useful role of LUS in the diagnosis of pneumothorax [8, 14–16]. The trauma FAST protocol has been recently augmented, e-FAST, and contains an evaluation for pneumothorax. The diagnosis is based on finding and interpreting four basic sonographic signs. Lung sliding is a dynamic sign represented by a bright horizontal movement of the pleural line. In the case of pneumothorax, air separates the two pleural lines and the movement disappears. The absence of lung sliding does not necessarily confirm pneumothorax, as a number of other conditions can cause lack of motion at the pleural line [17]. B lines are horizontal artifacts that arise from the pleural line (should be differentiated from the parallel comet-tail artifacts that arise above the pleural line and can cause false positive results, caused by subcutaneous emphysema), spread vertically, reach the lower edge of the screen without fading, and move synchronously with the lung (Fig. 1). The number and diffusion of the B lines increases with the increase of fluid in the lung [18]. Visualization of even one B line represents a demonstration of the adherence of the visceral pleura to the parietal pleura. B lines rule out pneumothorax with a negative rate of 100 % [19]. Lung pulse is a vertical movement of the pleural line synchronous to the cardiac rhythm. It can appear in the absence of lung sliding and is helpful in differentiating pneumothorax from other conditions characterized by the absence of pleural movement. Visualization of lung pulse rules out pneumothorax. The lung point allows 100 % specificity for confirmation of pneumothorax [20]. It represents a point in which lung sliding and/or B lines are visualized and intermittently replaced by a motionless pleura (Fig. 2). It can be used as an indicator of the size of the pneumothorax, as its location represents the location in which the lung is again in contact with the chest wall. Finding the lung point is achieved by moving the probe toward the lateral-inferior chest areas. M-Mode can also provide a static representation of a dynamic investigation that seeks for movement below the pleural line. The “stratosphere sign” is an indicator of lack of motion, thus an indicator of pneumothorax (Fig. 3), while the “seashore” sign is an indicator of movement below the pleural line and negates the presence of pneumothorax (Fig. 4). The combination of the aforementioned signs can lead to a diagnosis of pneumothorax. While sonographic semiology may appear difficult, several authors have demonstrated that minimal training yields very good results [21]. Lavignia et al. [22] demonstrated that residents trained formally for just 1 h for LUS allowed for safe interpretations and chest tube removals in 61 patients.
For all time points except the third, we can safely reject the null hypothesis, thereby arriving at the conclusion that the two clinical methods can be used interchangeably, as there is no statistically significant difference between them. The third set of p values, although also low, exceeds the limit set for the type I error α. This leads to an inconclusive result that cannot be called statistically significant at the 95 % confidence level.
Our study revealed that, for the evaluation of primary spontaneous pneumothorax, LUS and chest X-ray are interchangeable. LUS compared favorably with chest X-rays for clinical evaluation and chest tube removal. As previously stated, LUS has a short learning curve accessible to all clinicians, including residents and trainees. The expansion of “point-of-care” LUS can provide a quicker diagnosis and can save an important amount of unnecessary radiation. This technique can become standard of care for the management of pneumothorax and other chronic and acute lung and pleural conditions.
Although clinical (air-leaks) decision-making plays a big part in tube management in PSP, imagery is still widely used. Some X-rays offer information that LUS cannot, like the X-ray immediately after insertion that shows correct drain placement. For all other time points, LUS can document lung re-expansion as accurately as chest X-ray. The results of our study have led us to use LUS rather than X-rays for diagnosis and monitoring of the lung state after chest tube removal. Furthermore, follow-up visits required chest X-rays for the documentation of an expanded lung. As our results proved favorable at the fourth time point, we started using LUS for this. With the appearance of electronic suction devices that document air leakage, the role of chest X-ray has decreased. However, electronic devices are not widely available, and clinics where this is the case can use LUS to decrease the number of chest X-rays.
Compliance with ethical guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. All subjects were required to sign an informed consent prior to admission in the study.
Conflict of interest
Vlad Constantin, Alexandru Carâp, Simona Bobic, Alexandru Ciudin, Elvira Brătilă, Victor Vlădăreanu, and Bogdan Socea declare that they have no conflict of interest.
References
Melton LJ 3rd, Hepper NG, Offord KP. Incidence of spontaneous pneumothorax in Olmsted County, Minnesota: 1950 to 1974. Am Rev Respir Dis. 1979;120:1379–82.
Baumann MH, Strange C. Treatment of spontaneous pneumothorax: a more aggressive approach? Chest. 1997;112:789–804.
Baumann MH, Strange C. The clinician’s perspective on pneumothorax management. Chest. 1997;112:822–8.
Baumann MH, et al. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest. 2001;119:590–602.
Koenig SJ, Narasimhan M, Mayo PH. Thoracic ultrasonography for the pulmonary specialist. Chest. 2011;140(5):1332–41.
Gargani L, Volpicelli G. How I do it: lung ultrasound. Cardiovasc Ultrasound. 2014;12(1):25.
Volpicelli G, Elbarbary M, Blaivas M, et al., International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS) (2012) International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 38:577–91.
Berlet T, Fehr T, Merz TM. Current practice of lung ultrasonography (LUS) in the diagnosis of pneumothorax: a survey of physician sonographers in Germany. Crit Ultrasound J. 2014;6(1):16.
Lichtenstein DA, Menu Y. A bedside ultrasound sign ruling-out pneumothorax in the critically ill. Lung sliding. Chest. 1995;108:1345–8.
Marusteri M, Bacarea V. Comparing groups for statistical differences: how to choose the right statistical test? Biochem Med. 2010;20(1):15–32.
Bipasa B Assessing agreement for diagnostic devices. FDA/Industry Statistics Workshop. 2006.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–10.
Longo D, Fauci A, Kasper D, Hauser S, Jameson J, Loscalzo J. Harrison’s principles of internal medicine. McGraw Hill, New York. 2008.
Jakobson DJ, Iftach S. Merging ultrasound in the intensive care routine. Isr Med Assoc J. 2013;15:688–92.
Chira R, Chira A, Săplăcan R, et al. Pleural ultrasonography. Pictorial essay. Med Ultrason. 2014;16(4):364–71.
Lichtenstein DA, Meziere G, Lascols N, et al. Ultrasound diagnosis of occult pneumothorax. Crit Care Med. 2005;33:1231–8.
Lichtenstein DA, Lascols N, Prin S, et al. The lung pulse: an early ultrasound sign of complete atelectasis. Intensive Care Med. 2003;29:2187–92.
Agricola E, Bove T, Oppizzi M, et al. Ultrasound comet-tail images: a marker of pulmonary edema. A comparative study with wedge pressure and extravascular lung water. Chest. 2005;127:1690–5.
Lichtenstein D, Meziere G, Biderman P, et al. The comet-tail artifact, an ultrasound sign ruling out pneumothorax. Intensive Care Med. 1999;25:383–8.
Lichtenstein DA, Meziere G, Biderman P, et al. The lung point: an ultrasound sign specific to pneumothorax. Intensive Care Med. 2000;26:1434–40.
Monti JD, Younggren B, Blankenship R. Ultrasound detection of pneumothorax with minimally trained sonographers: a preliminary study. J Spec Oper Med. 2009;9:43–6.
Lavingia KS, Soult MC, Collins JN, et al. Basic ultrasound training can replace chest radiography for safe tube thoracostomy removal. Am Surg. 2014;80(8):783–6.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Constantin, V., Carap, A., Zaharia, L. et al. High correlation of lung ultrasound and chest X-ray after tube drainage in patients with primary spontaneous pneumothorax: can we omit X-rays for tube management?. Eur Surg 47, 175–180 (2015). https://doi.org/10.1007/s10353-015-0333-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-015-0333-9