Abstract
Objective
To investigate flow-related parameters in pulmonary arteries of patients with pulmonary arterial hypertension (PAH).
Materials and methods
Eleven PAH patients and twelve control participants were recruited. PAH and controls had similar age and gender distribution. 2D phase-contrast MRI (PC-MRI) was performed in the main, right, and left pulmonary artery (MPA, RPA, and LPA). The flow velocity, wall shear stress (WSS), and oscillatory shear index (OSI) were measured.
Results
PAH patients displayed prolonged acceleration time (Tacce) and increased ratio of flow change to acceleration volume in pulmonary arteries (both P < 0.001). The temporally averaged WSS values of MPA, RPA, and LPA in PAH patients were significantly lower than those of control participants (P < 0.001). The OSI in the pulmonary arteries was higher in PAH patients than control participants (P < 0.05). The ROC analysis indicated the ratio of maximum flow change to acceleration volume, WSS, and Tacce exhibited sufficient sensitivity and specificity to detect patients with PAH. The WSS demonstrated strong correlations with Tacce and the ratio value in the two groups (R2 = 0.78–0.96).
Conclusions
We used a clinically feasible 2D PC-MRI sequence with a reasonable scanning time to compute aforementioned indices. The quantitative parameters provided sufficient information to differentiate PAH patients from control participants.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pulmonary arterial hypertension (PAH) is one of the five categories of pulmonary hypertension (PH), and is a progressive condition characterized by progressive obliteration of the pulmonary arterioles, leading to increased pulmonary arterial pressure and eventually to right-ventricular (RV) failure [1]. The underlying mechanism for PAH remains unclear. PAH includes idiopathic PAH (formerly defined as primary PAH) and PAH associated with the other medical conditions, such as connective tissue diseases and congenital heart diseases. PAH is identified when the mean pulmonary arterial pressure is > 25 mmHg at rest or > 30 mmHg during exercise, and when the pulmonary capillary wedge or left-ventricular end-diastolic pressure is < 15 mmHg and the pulmonary vascular resistance (PVR) is > 3 Wood units [1]. Humber et al. reported a novel risk-prediction equation, combining information on patient sex, 6-minute walking distance, and cardiac output, for estimating the survival of PAH patients [2]. Over the past years, several novel treatment options for PAH have been developed. However, despite the improved survival rate of PAH patients, PAH remains a progressive fatal disease [3]. In PAH, increased PVR leads to RV overload, hypertrophy, and dilatation, and eventually to RV failure and death [4].
The previous studies have used noninvasive phase-contrast magnetic resonance imaging (PC-MRI) to estimate several hemodynamic parameters for diagnosing chronic PH patients. Ley et al. have reported lower pulmonary peak velocity, lower blood flow, shorter time-to-peak velocity, and higher pulmonary velocity rise gradient in the main pulmonary artery (MPA) of PAH patients [5]. A previous study measured stroke volume and cardiac output in the MPA by right-heart catheterization (RHC) and PC-MRI, and has shown a strong correlation between these two schemes [6]. In addition, patients with high PVR have been proven to present inhomogeneous velocity profiles, high retrograde flow, and low distensibility in MPA [6, 7]. Besides, the patients were also associated with shorter acceleration time (\(T_{{{\text{acce}}}}\)) of flow rate in the MPA, lower acceleration volume (\(V_{{{\text{acce}}}}\)), and an increased ratio of maximum upslopes of flow rate to \(V_{{{\text{acce}}}}\) [\(\left( {{\text{maximum d}}Q/{\text{d}}t} \right)/V_{{{\text{acce}}}}\)] during ejection [6]. Nevertheless, aforementioned indices in the right pulmonary artery (RPA) and left pulmonary artery (LPA) have not been discussed thoroughly. The altered flow characteristics of RPA and LPA in PAH patients are still not clear.
In animal experiments, Wang et al. used the Windkessel volume (\(V_{{{\text{wk}}}}\)), which accounts for the shape of the arterial pressure waveform, to describe the reservoir in the aorta by calculating \(V_{{{\text{wk}}}}\) as an integration of the measured inflow (\(V_{{{\text{in}}}}\)) and outflow (\(V_{{{\text{out}}}}\)) during a cardiac cycle [8]. Nonetheless, a step toward elucidating the role of \(V_{{{\text{wk}}}}\) in the system of pulmonary arteries is still deficient.
Because vessels are exposed to various hemodynamics forces, including viscous forces, periodic stretch, and hydrostatic pressure induced by the pulsatile blood flow, several studies have investigated the forces or pressure exerted by the blood flow on the vessel wall to evaluate the specific vascular characteristics of patients. The index of wall shear stress (WSS), which describes the frictional force of the flowing blood on the arterial wall, has attracted increasing attention. Zarins et al. examined postmortem specimens to quantitatively correlate plaque localization with flow velocity profiles and WSS in patients with carotid bifurcation atherosclerosis [9]. The authors concluded that atherosclerosis develops preferentially at branches and curvatures of the arterial tree, which are associated with relatively low WSS, flow separation, and departure from axially aligned, unidirectional flow. Chien et al. indicated that the endothelial cells of vessels bear the majority of the WSS and play a vital role in the remodeling of the vascular wall [10, 11]. Cheng et al. evaluated atherosclerotic lesion size and vulnerability in mouse carotid arteries, observing that reduced shear stress induced larger lesions with a vulnerable plaque phenotype [12]. In addition, Barker et al. calculated the shear range index [13], which is derived from the WSS, to evaluate WSS symmetry along the lumen circumference, observing significant differences in the bicuspid aortic valve between patient and control groups [14]. Stalder et al. used PC-MRI and calculated the oscillatory shear index (OSI) to interpret the temporal oscillation of WSS during the cardiac cycle in healthy volunteers [15].
To date, several schemes have been demonstrated to be able to estimate WSS. Tang et al. developed a combined MRI and computational fluid dynamics (CFD) approach to construct subject-specific pulmonary artery models and to quantify WSS in the MPA of PAH patients [16]. The previous studies reported lower systolic in-plane (i.e., circumferential) WSS values, computed from three-directional velocity-encoding 4D flow data sets, of proximal pulmonary arteries in PAH group [17, 18]. Images acquired with 4D flow MRI may comprise on longer total scanning time and lower spatial resolution for analyzing hemodynamic parameters and WSS.
In this study, we measured blood flow hemodynamic parameters, axial WSS, and WSS-derived OSI in the MPA, RPA, and LPA in PAH patients and control participants using noninvasive time-resolved two-dimensional (2D) PC-MRI. We also investigated the regional distribution of WSS along the circumference of vessel wall. The purpose of this study was to understand the altered flow characteristics of large pulmonary arteries in PAH patients.
Materials and methods
Study cohort
The study population consisted of 11 PAH patients (age 43.0 ± 17.9 years; male/female = 5/6) and 12 control participants without a history of pulmonary disease or pulmonary valve insufficiency (age 38.4 ± 8.9 years; male/female = 5/7). PAH and controls had similar age and gender distribution. Informed consent was obtained from all participants.
MRI acquisition
2D PC-MRI was performed on a 1.5 T clinical scanner (Magnetom Sonata, Siemens, Erlangen, Germany) with a body array coil and prospective ECG triggering. A 2D gradient echo phase-contrast sequence (TR/TE = 11/4.8 ms, flip angle = 15°, temporal resolution = 22 ms, matrix size = 256 × 192, spatial resolution = 1.1 × 1.1 mm2, and slice thickness = 5 mm) with a 150 cm/s through-plane velocity-encoding gradient was acquired, sampling approximately 90% of the cardiac cycle with free-breathing scheme. Magnitude and phase images of the MPA (about 2 cm proximal to bifurcation), RPA (1–1.5 cm distal to bifurcation), and LPA (1–1.5 cm distal to bifurcation) were obtained. All images were acquired in imaging planes perpendicular to the long axes of the vessels.
Data processing and statistical analysis
Regions of interest (ROIs) were determined manually on magnitude images using a custom-built analysis program written in Matlab (The Mathworks, Natick, USA) [15], and were applied to phase images for calculating the flow velocity (Figure S1). Several parameters including the peak flow rate, the mean flow rate during the cardiac cycle, and the net flow volume were calculated. Figure 1a shows the acceleration time (\(T_{{{\text{acce}}}}\)) of flow rate and the acceleration flow volume (\(V_{{{\text{acce}}}}\)) in a 32-year-old female PAH patient. The \(T_{{{\text{acce}}}}\) was defined as the time from the ECG R-wave to the peak flow rate [6], i.e., the time-to-peak of the flow rate. The integrated flow rate during \(T_{{{\text{acce}}}}\) was defined as \(V_{{{\text{acce}}}}\) [6], as illustrated by the hatched area in Fig. 1a. The \({\max}. {\text{d}}Q/{\text{d}}t\) was the maximum change in the flow rate during ejection, defined by the maximum upslope of the flow rate during systolic phases [6]. We defined a ratio of the two aforementioned parameters to obtain a physical parameter of force exerted by the heart during ejection phases:
a Several indices derived from the flow profiles are displayed. The \(T_{{{\text{acce}}}}\) was defined as the time duration from the onset of flow to the peak flow rate. The \(V_{{{\text{acce}}}}\) (hatched area) was evaluated by integrating the profile of the flow rate during the \(T_{{{\text{acce}}}}\). The \({\max}. {\text{d}}Q/{\text{d}}t\) during the systolic phase was evaluated as the maximum slope of the flow rate curve (thick solid line). b Integrals of pulmonary aerial inflow (\(V_{{{\text{in}}}}\)) and outflow (\(V_{{{\text{out}}}}\)) in a 45-year-old female PAH patient. The integral of the differences between the inflow (MPA) and outflow (RPA and LPA) represents the instantaneous change in the \(V_{{{\text{wk}}}}\) (hatched area) during a cardiac cycle
To determine the instantaneous change in the windkessel volume (\(V_{{{\text{wk}}}}\)) of the pulmonary system, the integral of the differences between inflow and outflow was calculated, as indicated by the hatched area in Fig. 1b [8].
Several other flow-derived indices were quantified to investigate the hemodynamic differences between the PAH patients and the control participants. The regurgitation fraction was defined as the ratio of the retrograde to antegrade flow volumes [19]. Pulmonary vascular strain was evaluated from magnitude images using the following equation [19]:
where Amax and Amin are maximum cross-sectional area and minimum cross-sectional area of the vessel during a cardiac cycle, respectively.
Because PAH patients can exhibit abnormal shear stress in the pulmonary arteries, axial WSS estimations (or \(\overset{\lower0.5em\hbox{$\smash{\scriptscriptstyle\rightharpoonup}$}} {\tau }\)), i.e., the WSS along the main flow direction, were performed. As described in the previous study [15], if a 1D problem is considered, the estimations of \(\overset{\lower0.5em\hbox{$\smash{\scriptscriptstyle\rightharpoonup}$}} {\tau }\) can be simplified to the following:
where \(\eta\) denotes the dynamic viscosity and was assumed as 4.5 cP [15], v denotes the blood flow velocity, and h denotes the height of boundary. As described by Stalder et al., this calculation combines Green’s theorem and B-spline interpolation to provide an optimal quantification of several blood flow and vessel wall parameters [15].
To determine the temporal oscillation in WSS during a cardiac cycle, the OSI was calculated as follows:
where T is the duration of the cardiac cycle and \(\overset{\lower0.5em\hbox{$\smash{\scriptscriptstyle\rightharpoonup}$}} {\tau }\) is the instantaneous WSS vector as given by Eq. (3) [15].
The unpaired Student’s t test (two-tailed) was used to evaluate the significance of differences between the PAH patients and the control participants. We also analyzed the receiver-operating characteristic (ROC) curves of several quantified indices by the software of SPSS 12 (SPSS, Chicago, IL). The area under the ROC curve (AUC), cut-off value, specificity, sensitivity, and accuracy were determined to perform the diagnostic performance of each index. The Pearson’s correlation analysis was performed to correlate WSS with peak flow rate, Tacce, and the ratio. A P value < 0.05 was considered statistically significant.
Results
Blood flow hemodynamic indices
Figure 2 shows the time courses of the pulmonary flow rates in the MPA, RPA, and LPA throughout the cardiac cycles of a control participant (age 32 years, female) and a PAH patient (age 32 years, female). In comparison with the control participants, the PAH patients displayed markedly increased flow rates in the MPA, RPA, and LPA, which indicated that the flow patterns differed between the two groups. However, the mean flow volumes and peak flow rate of PAH patients and control participants showed non-significant difference (Table 1). The measured \(T_{{{\text{acce}}}}\) values of the control participants and the PAH patients were 132.1 ± 14.0 ms and 93.8 ± 22.6 ms in the MPA, 148.4 ± 20.4 ms, and 99.2 ± 19.8 ms in the RPA, and 136.7 ± 28.6 ms and 96.0 ± 17.6 ms in the LPA (all P < 0.001), respectively (Fig. 3a). As shown in Fig. 3b, the \(V_{{{\text{acce}}}}\) differed significantly between the two groups only in the LPA (control participant 6.4 ± 1.5 cm3, PAH patient 4.0 ± 3.4 cm3; P < 0.05). We observed markedly higher systolic \({\max}. {\text{d}}Q/{\text{d}}t\) values (Fig. 3c) in the MPA and RPA in the PAH patients (6.5 ± 3.4 L/s2 and 2.9 ± 1.8 L/s2) than in the control participants (4.0 ± 1.2 L/s2 and 1.7 ± 0.6 L/s2), as reflected by the steeper upslope of the flow rate curves in the PAH patient (Fig. 2b). The defined ratio of normalized maximum systolic increase in the flow rate is a physical parameter that demonstrates the force exerted by the heart during ejection phases. As shown in Fig. 3d, the PAH patients exhibited significantly higher values for this parameter in the MPA, RPA, and LPA than the control participants [MPA: 373.0 ± 101.0 s−2 vs. 189.5 ± 65.7 s−2, RPA: 434.8 ± 139.4 s−2 vs. 195.8 ± 70.3 s−2, and LPA: 553.5 ± 224.5 s−2 vs. 214.9 ± 98.5 s−2 (all P < 0.001)].
WSS, OSI, and other indices
Figure 4 shows the time courses of WSS in the MPA, RPA, and LPA in the control participants and PAH patients. The PAH group exhibited lower WSS values than the control group. The box plots in Fig. 5a, b show the hemodynamic indices of the WSS and WSS-derived OSI in the control participants and PAH patients. The temporally averaged WSS (Fig. 5a) in the MPA of the PAH patients was 0.21 ± 0.06 N/m2, which was considerably lower than that in the control participants (0.28 ± 0.04 N/m2, P < 0.001). We observed the same trend in the RPA and the LPA. The OSI in the RPA (17.7 ± 8.5% vs. 10.2 ± 4.0%, P < 0.01) and LPA (21.9 ± 9.3% vs. 15.3 ± 4.3%, P < 0.05) displayed significantly higher values in PAH patients compared to control participants.
The mean values of vascular strain in the control participants (MPA: 28.4 ± 13.3%; LPA: 34.2 ± 16.4%) were significantly higher than those in the PAH patients (MPA: 13.1 ± 4.7%; LPA: 20.5 ± 9.0%), suggesting that the vessel walls of the control participants were less stiff than those of the PAH patients (Fig. 5c). The PAH patients exhibited a regurgitation fraction of 6.4 ± 6.0% in the MPA, which was higher than that of the control participants (1.5 ± 1.5%, P < 0.05), indicating increased retrograde flow in the patients with PAH compared with the control participants (Fig. 5d). The \(V_{{{\text{wk}}}}\) of the PAH patients and control participants showed non-significant differences (Fig. 5e). Table 1 summarizes the hemodynamic parameters of the MPA, RPA, and LPA in the two groups.
Segmental WSS
Figure 6 illustrates the regional distribution of WSS along the circumference of the vessel wall. The PAH patients generally exhibited lower segmental WSS in the MPA, RPA, and LPA than the control participants. In the RPA, the WSS in the segments in head–posterior–foot orientation (Fig. 6, middle column) were markedly lower in the PAH patients than in the control participants (P < 0.001). In the LPA, the WSS in all segments were significantly lower in the PAH patients than in the control participants. The segmental WSS values in the RPA and LPA of the PAH patients were approximately 50% of those of the control participants (Fig. 6, middle and right columns).
Both groups exhibited inhomogeneous WSS distribution, particular in control group, which may be attributable to uneven flow velocity profiles. Lower segmental variations of WSS in PAH group indicated reduced asymmetry of WSS along the circumference of the vessel walls.
ROC curve analysis and correlation analysis
Figure 7 presents the ROC curves in MPA, RPA, and LPA for the quantified indices showing significant difference between PAH and control groups. Table 2 summarizes the ROC curve-related parameters. In MPA, the defined ratio, WSS, and Tacce displayed high AUC (all AUC > 0.85) and sufficient sensitivity (70–90.9%) and specificity (91.7–100%), all with P < 0.005. Similar trends can be observed in RPA and LPA.
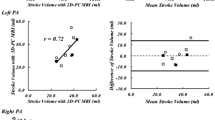
As shown in Fig. 8, either in PAH patients or control participants, WSS demonstrated strong correlations with Tacce (R2 = 0.87–0.96) and the ratio (R2 = 0.78–0.94).
Discussion
In this study, we performed 2D PC-MRI to quantify several flow-derived hemodynamic parameters, WSS, and WSS-derived OSI parameters in MPA, RPA, and LPA, and used them to differentiate the PAH patients from the control participants. The integrated information of abovementioned indices can help to understand the altered flow characteristics of large pulmonary arteries in PAH patients.
The reduced \(T_{{{\text{acce}}}}\) in the MPA, RPA, and LPA of PAH patients demonstrated the effects of high PVR on the pumping function of the right heart. The \(V_{{{\text{acce}}}}\) in the MPA and RPA showed no significant difference between PAH patients and control participants. It may be attributed to a compensatory effect in which the heart provides sufficient \(V_{{{\text{acce}}}}\) during systolic phases, even in the presence of high pressure and resistance in the pulmonary system in PAH patients. Increased maximum \({\text{d}}Q/{\text{d}}t\) values in the PAH group suggested that the flow rate reached a maximum within a shorter period in the PAH patients than in the control participants. The PAH patients also exhibited higher values for the ratio than the control participants, indicating that the right heart might exert a larger force in PAH than in normal condition to resist high-pressure gradient and resistance in the pulmonary system. The high accuracy in the ROC analysis in the defined ratio and Tacce further illustrated their diagnostic powers to demonstrate the abnormality in the large pulmonary arteries of PAH patients.
The PAH patients exhibited lower pulmonary vascular strain in the MPA and LPA compared with the control participants, suggesting that PAH is associated with increased stiffness in the pulmonary arteries, which is consistent with the results of previous histopathological research [20].
Wang et al. indicated that \({} V_{{{\text{wk}}}}\) can be used to estimate aortic arterial compliance [8]. However, in our preliminary results, the \(V_{{{\text{wk}}}}\) values of the control and PAH groups were indistinguishable, which may have resulted from variations in the treatment phases and progression of the PAH patients. Therefore, the \({} V_{{{\text{wk}}}}\) index may not provide a robust parameter for assessing PAH in our present results. In future investigation of the \({} V_{{{\text{wk}}}}\) index, recruiting a larger population of PAH patients and separating the patients subject to various treatment phases and progression into subgroups are necessary.
The previous studies have demonstrated that shear stress induced by laminar blood flow plays an essential role in normal vascular functioning, which includes the regulation of the vascular caliber as well as the inhibition of the proliferation, thrombosis, and inflammation of the vessel wall [9, 10, 21,22,23]. Sustained high shear stress can modulate the expression of vascular endothelial cell genes and proteins that protect against atherosclerosis. Butler et al. indicated that the temporal gradient in shear stress is essential for the modulation of signaling and gene expression in vascular endothelial cells and their associated vasodilation function [24]. Because disturbed blood flow and associated low shear stress may upregulate the expression of genes and proteins involved in vessel remodeling, we evaluated the differences in WSS in the large pulmonary arteries of PAH patients, attempting to understand the abnormal WSS in MPA, PRA, and LPA in patient group. In the PAH patients, reduced WSS during systolic phases as well as reduced temporally averaged WSS throughout the cardiac cycle may upregulate the expression of genes involved in vasoconstriction in the pulmonary vascular system. Increased OSI, representing increased oscillations in WSS, can further indicate disturbed flow patterns in the MPA, RPA, and LPA of the PAH patients. A heterogeneous flow velocity may result in heterogeneous direction of the WSS, leading to reduced WSS. Accordingly, the disturbance in flow, the reduction in WSS, and the increase of OSI may, consequently, have integrated impact on vasoconstriction in PAH patients. On the other hand, the high correlations showing between WSS and the defined ratio or Tacce further described the interaction of abnormal vascular characteristics and altered blood flow.
Detailed investigation of the segmental WSS may also provide useful information for assessing PAH. In each segment, the PAH group presented lower WSS compared to the control group, especially at segments 1–2 (posterior-right orientation) in the MPA, segments 6–12 (head–posterior–foot orientation) in the RPA, and segments 6–12 (head–left-foot orientation) in the LPA. The previous studies have indicated that atherosclerotic lesions typically occur in the regions of curvature and bifurcation of the arteries where they are usually with low WSS values [9, 25]. Therefore, in our study, the segments in regions with low WSS might be associated with a high risk of damage to vascular wall. Future investigations of segmental WSS in PAH are warranted to provide sophisticated information for clinical assessment.
There are several limitations in this study. First, to achieve a high temporal resolution and to shorten scanning time, we acquired images using time-resolved 2D PC-MRI and acquired data only on through-plane flow velocity-encoding. Bollache et al. reported that one-directional velocity-encoding technique may present lower flow measurements than that measured by three-directional velocity-encoding scheme [26]. Therefore, acquiring three-directional velocity-encoding flow data can provide additional useful information for PAH assessment, such as circumferential WSS of vessel walls [15] or path lines of pulmonary vascular flow in the case of 4D flow data acquisition [13, 27]. Second, considering the total scanning time, we did not evaluate the routine cardiac function in this study. Obtaining measurements on RV morphology and function to calculate geometry- and function-derived indices [28, 29] may also increase the usefulness of the measured parameters in assessing PAH. Using parallel imaging and navigator-controlled respiration scheme may enable the acquisition of images with higher temporal resolution or spatial resolution, providing subtle details on the temporal and spatial variations between the PAH patients and control participants. Third, the limited numbers of study participants and without correction of momentary situation may not exclude the possible confounding factors of WSS; for example, blood pressure, heart rate, medication, as well as smoking situation. In future studies, the above-mentioned factors and other physiological parameters, such as pulmonary vascular resistance or pulmonary pressure, can be considered altogether to establish a risk-prediction model for PAH patients. Fourth, the lack of catheterization data may limit the understanding of the correlation between computed indices and clinical outcome.
In conclusion, we evaluated several hemodynamic parameters, WSS, and WSS-derived OSI using 2D PC-MRI images in a clinically feasible scanning time and without using complex post-processing procedures. Our results indicated that these indices are of assessing relevance in PAH and enable the differentiation of PAH patients from control participants. The establishment of these indices for PAH may facilitate the long-term follow-up of the treating efficacy and management of PAH patients.
References
Chin KM, Rubin LJ (2008) Pulmonary arterial hypertension. J Am Coll Cardiol 51(16):1527–1538
Humbert M, Sitbon O, Yaici A, Montani D, O'Callaghan DS, Jais X, Parent F, Savale L, Natali D, Gunther S, Chaouat A, Chabot F, Cordier JF, Habib G, Gressin V, Jing ZC, Souza R, Simonneau G (2010) Survival in incident and prevalent cohorts of patients with pulmonary arterial hypertension. Eur Respir J 36(3):549–555
Humbert M, Sitbon O, Chaouat A, Bertocchi M, Habib G, Gressin V, Yaici A, Weitzenblum E, Cordier JF, Chabot F, Dromer C, Pison C, Reynaud-Gaubert M, Haloun A, Laurent M, Hachulla E, Cottin V, Degano B, Jais X, Montani D, Souza R, Simonneau G (2010) Survival in patients with idiopathic, familial, and anorexigen-associated pulmonary arterial hypertension in the modern management era. Circulation 122(2):156–163
Batt J, Shadly Ahmed S, Correa J, Bain A, Granton J (2013) Skeletal muscle dysfunction in idiopathic pulmonary arterial hypertension. Am J Respir Cell Mol Biol
Ley S, Mereles D, Puderbach M, Gruenig E, Schock H, Eichinger M, Ley-Zaporozhan J, Fink C, Kauczor HU (2007) Value of MR phase-contrast flow measurements for functional assessment of pulmonary arterial hypertension. Eur Radiol 17(7):1892–1897
Mousseaux ETJ, Jolivet O, Simonneau G, Bittoun J, Gaux JC (1999) Pulmonary arterial resistance: noninvasive measurement with indexes of pulmonary flow estimated at velocity-encoded MR imaging—preliminary experience1. Radiology 212:896–902
Kondo C, Caputo GR, Masui T, Foster E, O'Sullivan M, Stulbarg MS, Golden J, Catterjee K, Higgins CB (1992) Pulmonary hypertension: pulmonary flow quantification and flow profile analysis with velocity-encoded cine MR imaging. Radiology 183(3):751–758
Wang JJOBA, Shrive NG, Parker KH, Tyberg JV (2003) Time-domain representation of ventricular-arterial coupling as a windkessel and wave system. Am J Physiol Heart Circ Physiol 284(4):H1358–H1368
Zarins CK, Giddens DP, Bharadvaj BK, Sottiurai VS, Mabon RF, Glagov S (1983) Carotid bifurcation atherosclerosis. Quantitative correlation of plaque localization with flow velocity profiles and wall shear stress. Circ Res 53(4):502–514.
Chien S (2007) Mechanotransduction and endothelial cell homeostasis: the wisdom of the cell. Am J Physiol Heart Circ Physiol 292(3):H1209–1224
Chien S, Li S, Shyy YJ (1998) Effects of mechanical forces on signal transduction and gene expression in endothelial cells. Hypertension 31(1 Pt 2):162–169
Cheng C, Tempel D, van Haperen R, van der Baan A, Grosveld F, Daemen MJ, Krams R, de Crom R (2006) Atherosclerotic lesion size and vulnerability are determined by patterns of fluid shear stress. Circulation 113(23):2744–2753
Francois CJ, Srinivasan S, Schiebler ML, Reeder SB, Niespodzany E, Landgraf BR, Wieben O, Frydrychowicz A (2012) 4D cardiovascular magnetic resonance velocity mapping of alterations of right heart flow patterns and main pulmonary artery hemodynamics in tetralogy of Fallot. J Cardiovasc Magn Reson 14:16
Barker AJ, Lanning C, Shandas R (2010) Quantification of hemodynamic wall shear stress in patients with bicuspid aortic valve using phase-contrast MRI. Ann Biomed Eng 38(3):788–800
Stalder AF, Russe MF, Frydrychowicz A, Bock J, Hennig J, Markl M (2008) Quantitative 2D and 3D phase contrast MRI: optimized analysis of blood flow and vessel wall parameters. Magn Reson Med 60(5):1218–1231
Tang BT, Pickard SS, Chan FP, Tsao PS, Taylor CA, Feinstein JA (2012) Wall shear stress is decreased in the pulmonary arteries of patients with pulmonary arterial hypertension: an image-based, computational fluid dynamics study. Pulm Circ 2(4):470–476
Barker AJ, Roldan-Alzate A, Entezari P, Shah SJ, Chesler NC, Wieben O, Markl M, Francois CJ (2015) Four-dimensional flow assessment of pulmonary artery flow and wall shear stress in adult pulmonary arterial hypertension: results from two institutions. Magn Reson Med 73(5):1904–1913
Schafer M, Kheyfets VO, Schroeder JD, Dunning J, Shandas R, Buckner JK, Browning J, Hertzberg J, Hunter KS, Fenster BE (2016) Main pulmonary arterial wall shear stress correlates with invasive hemodynamics and stiffness in pulmonary hypertension. Pulm Circ 6(1):37–45
Tardivon AA, Mousseaux E, Brenot F, Bittoun J, Jolivet O, Bourroul E, Duroux P (1994) Quantification of hemodynamics in primary pulmonary hypertension with magnetic resonance imaging. Am J Respir Crit Care Med 150(4):1075–1080
Prapa M, McCarthy KP, Dimopoulos K, Sheppard MN, Krexi D, Swan L, Wort SJ, Gatzoulis MA, Ho SY (2013) Histopathology of the great vessels in patients with pulmonary arterial hypertension in association with congenital heart disease: large pulmonary arteries matter too. Int J Cardiol
Chiu JJ, Usami S, Chien S (2009) Vascular endothelial responses to altered shear stress: pathologic implications for atherosclerosis. Ann Med 41(1):19–28
Cunningham KS, Gotlieb AI (2005) The role of shear stress in the pathogenesis of atherosclerosis. Lab Invest 85(1):9–23
Efstathopoulos EP, Patatoukas G, Pantos I, Benekos O, Katritsis D, Kelekis NL (2008) Wall shear stress calculation in ascending aorta using phase contrast magnetic resonance imaging. Investigating effective ways to calculate it in clinical practice. Phys Med 24(4):175–181
Butler PJ, Weinbaum S, Chien S, Lemons DE (2000) Endothelium-dependent, shear-induced vasodilation is rate-sensitive. Microcirculation 7(1):53–65
Shaaban AM, Duerinckx AJ (2000) Wall shear stress and early atherosclerosis: a review. AJR Am J Roentgenol 174(6):1657–1665
Bollache E, van Ooij P, Powell A, Carr J, Markl M, Barker AJ (2016) Comparison of 4D flow and 2D velocity-encoded phase contrast MRI sequences for the evaluation of aortic hemodynamics. Int J Cardiovasc Imaging 32(10):1529–1541
Bachler P, Valverde I, Pinochet N, Nordmeyer S, Kuehne T, Crelier G, Tejos C, Irarrazaval P, Beerbaum P, Uribe S (2013) Caval blood flow distribution in patients with Fontan circulation: quantification by using particle traces from 4D flow MR imaging. Radiology 267(1):67–75
Moral S, Fernandez-Friera L, Stevens G, Guzman G, Garcia-Alvarez A, Nair A, Evangelista A, Fuster V, Garcia MJ, Sanz J (2012) New index alpha improves detection of pulmonary hypertension in comparison with other cardiac magnetic resonance indices. Int J Cardiol 161(1):25–30
Swift AJ, Rajaram S, Hurdman J, Hill C, Davies C, Sproson TW, Morton AC, Capener D, Elliot C, Condliffe R, Wild JM, Kiely DG (2013) Noninvasive estimation of PA pressure, flow, and resistance with CMR imaging: derivation and prospective validation study from the ASPIRE registry. JACC Cardiovasc Imaging
Acknowledgements
This study was funded by the National Science Council, Taiwan (NSC 102-2320-B-007-003-MY3; MOST 106-2314-B-007-006-MY3) and Veterans General Hospitals and University System of Taiwan Joint Research Program (VGHUST103-G3-1-1).
Funding
This study was funded by the Ministry of Science and Technology, Taiwan (NSC 102-2320-B-007-003-MY3; MOST 106-2314-B-007-006-MY3) and Veterans General Hospitals and University System of Taiwan Joint Research Program (VGHUST103-G3-1-1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, HH., Tseng, WY.I., Yu, HY. et al. Phase-contrast magnetic resonance imaging for analyzing hemodynamic parameters and wall shear stress of pulmonary arteries in patients with pulmonary arterial hypertension. Magn Reson Mater Phy 32, 617–627 (2019). https://doi.org/10.1007/s10334-019-00767-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10334-019-00767-x