Abstract
Seizures do not occur randomly. They tend to cluster in the majority of men and women with epilepsy. Seizure clusters, in turn, often show a periodicity. When the periodicity of seizure exacerbation aligns itself with that of the menstrual cycle, it is designated as catamenial epilepsy. The neuroactive properties of reproductive steroids and the cyclic variation in their serum concentrations are important pathophysiologic factors. There is evidence for the existence of at least three patterns of catamenial seizure exacerbation: perimenstrual and periovulatory in ovulatory cycles and entire luteal phase in anovulatory cycles. A rational mathematical basis for this categorization of catamenial epilepsy has been developed. It identifies approximately 1/3 of women as having catamenial epilepsy. If seizures show hormonal sensitivity in their occurrence, they may also respond to hormonal treatment. The randomized, double-blind, placebo-controlled NIH Progesterone Trial found that cyclic progesterone supplement is no better than placebo overall but did reduce seizure frequency significantly in the subset of women with perimenstrual seizure exacerbation. There have also been successful open label trials using depomedroxyprogesterone and gonadotropin-releasing hormone analogues.
Zusammenfassung
Anfälle treten nicht zufällig auf, sondern meist gehäuft bei Frauen und Männern mit Epilepsie. Anfallshäufungen wiederum zeigen oft Periodizität und werden als katameniale Epilepsie bezeichnet, wenn sie mit dem Menstruationszyklus zusammentreffen. Als wichtige pathophysiologische Faktoren gelten die neuroaktiven Anteile reproduktiver Steroide und die zyklische Schwankung in ihren Serumkonzentrationen. Mindestens 3 Formen von katamenialer Anfallsverstärkung konnten nachgewiesen werden: perimenstruell und periovulatorisch im ovulatorischen Zyklusteil und in der gesamten Lutealphase im anovulatorischen Zyklusteil. Für diese Kategorisierung wurde eine rationale mathematische Grundlage entwickelt. Sie identifiziert etwa ein Drittel der Frauen als Betroffene von katamenialer Epilepsie. Treten die Anfälle in hormoneller Abhängigkeit auf, könnten sie auf Hormonbehandlung ansprechen. Die randomisierte, doppelblinde, placebokontrollierte Progesteron-Studie des National Institute of Health (NIH) ergab, dass ein periodisch verabreichtes Progesteronpräparat gegenüber Placebo bezüglich der gesamten Studiengruppe keine bessere Wirkung erzielt, jedoch die Anfallshäufigkeit in der Untergruppe der Frauen mit perimenstrueller Anfallsverstärkung signifikant reduziert. Es gab darüber hinaus erfolgreiche markenunabhängige Tests mit depomedroxyprogesteron- und gonadotropin-freisetzenden Hormonanaloga.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Definition, patterns and prevalence
Seizures do not occur randomly in the majority of men and women with epilepsy [1, 2]. They tend to cluster in over 50 % of cases [1, 2]. Seizure clusters, in turn, may occur with temporal rhythmicity in a significant proportion of men (29 %) and women (35 %) with epilepsy [3]. When the periodicity of seizure exacerbation aligns with the menstrual cycle, it is commonly known as catamenial epilepsy [4]. This may be attributable to 1) the neuroactive properties of reproductive steroid hormones and 2) the cyclic variation in their serum levels [4].
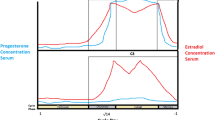
Physiological endocrine secretion during the menstrual cycle influences the occurrence of seizures (Fig. 1). In ovulatory cycles, seizure frequency shows a statistically significant positive correlation with the serum estradiol/progesterone ratio [5]. This ratio is highest during the days prior to ovulation and menstruation and is lowest during the early and mid-luteal phases [5]. The premenstrual exacerbation of seizures has been attributed to the rapid withdrawal of the antiseizure effects of progesterone [4, 5]. Mid-cycle exacerbations may be due to the preovulatory surge of estrogen, unaccompanied by any rise in progesterone until ovulation occurs [4–6]. Seizures are least common during the mid-luteal phase when progesterone levels are highest [4–6], except in anovulatory cycles in which the mid-cycle surge in estrogen still occurs, albeit they are not as high as in ovulatory cycles, but unaccompanied by any substantial increase in progesterone levels [4].
Three patterns of catamenial epilepsy: perimenstrual (C1) and periovulatory (C2) exacerbations during normal ovulatory cycles and entire second half of the cycle (C3) exacerbation during inadequate luteal phase cycles where Day 1 is the first day of menstrual flow and Day −14 is the day of ovulation
Herzog et al. [2, 4, 7] presented statistical evidence to support the concept of catamenial epilepsy and the existence of at least three distinct patterns of seizure exacerbation in relation to the menstrual cycle (Fig. 1):
-
1)
perimenstrual (C1: Day −3 to 3) and
-
2)
periovulatory (C2: Day 10 to −13) in normal cycles, and
-
3)
luteal (C3: Day 10 to 3) in inadequate luteal phase cycles.
In these cycles, Day 1 is the first day of menstrual flow and ovulation is presumed to occur 14 days before the subsequent onset of menses (Day −14). These three patterns can be demonstrated simply by
-
1)
charting menses and seizures and
-
2)
obtaining a mid-luteal phase serum progesterone level to distinguish between normal and inadequate luteal phase cycles (< 5 ng/ml).
While the precise definition of catamenial epilepsy remains arbitrary, one may maximize the efficiency of distinguishing between women whose seizure occurrence shows a high versus low degree of hormonal sensitivity by using the points of inflection of the S-shaped distribution curves that define the relationship between the severity of seizure exacerbation and the number of women who have exacerbation [4, 7]. These points are calculated to be in the vicinity of a twofold increase in average daily seizure frequency during the phases of exacerbation relative to the baseline phases for all three types of catamenial exacerbation. We propose the use of these points of inflection values in seizure frequency for the designation of catamenial epilepsy. By this criterion, approximately one third of women with intractable partial epilepsy would qualify for the designation of having catamenial epilepsy [4, 7] The adoption of a standard albeit arbitrary nomenclature may provide greater uniformity to study designs for the investigation of the pathogenesis and treatment of catamenial seizure exacerbation.
Pathophysiology
There is considerable scientific evidence at molecular biological, neuronal, experimental animal and clinical levels to indicate that reproductive steroids have neuroactive properties that play an important role in the pathophysiology of epilepsy and the pattern of seizure occurrence. Steroids act in the brain by direct membrane-mediated (short latency) effects as well as intracellular receptor-genomically-mediated (long latency) effects [8–10].
Reproductive hormonal effects on epilepsy
Estradiol
The potential importance of estradiol in the regulation of temporolimbic function is highlighted by the presence of the estradiol synthesizing enzymes, cytochromes P45017a and P450 aromatases, which are localized in neurons in the hippocampus and the measurement of hippocampal estradiol levels that can surpass serum levels [11, 12]. Estradiol has complex effects that vary with estradiol concentration, mode and site of administration, blood–brain barrier and epileptic substrate [13]. The contradictory effects of estrogen in the brain have been reviewed in detail by Veliskova et al [14].
Most adult animal experimental investigations have led to the prevailing opinion that estradiol has neuroexcitatory effects that can lower seizure thresholds. The thresholds of limbic seizures in female rats fluctuate during the estrus cycle inversely to estradiol levels [15]. Physiological doses of estradiol activate spike discharges [13, 16–18] and lower the thresholds of seizures induced by electroshock, kindling, pentylenetetrazol, kainic acid, ethyl chloride and other agents and procedures [13, 18–22]. In fact, topical brain application, as well as intravenous systemic administration, of estradiol in rabbits produces a significant increase in spontaneous electrically recorded paroxysmal spike discharges [13]. The increase is seen within a few seconds of application to suggest a direct membrane rather than a genomic effect and is more dramatic in animals with pre-existent cortical lesions and estradiol priming [13, 16, 18].
With regard to mechanisms of action, estradiol may act on CA1 hippocampal pyramidal neurons via convergent mechanisms that combine the effects of estradiol priming on hippocampal plasticity with subsequent direct potentiation of excitatory postsynaptic potentials (EPSPs) [16]. More specifically, estradiol priming via subcutaneous estradiol injection may act over 2 days to increase dendritic spines and excitatory synapses as well as NMDA binding [23, 24] to increase EPSP durations and repetitive firing response to stimulation of Schaeffer collaterals [16]. Of note is that estradiol priming also increases GABA binding [25]. Direct application of estradiol to primed CA1 hippocampal slices increases membrane-mediated EPSP response to Schaffer collateral stimulation or glutamate application within a couple of minutes [16]. The estradiol application potentiates kainate, and quisqualate-mediated neurotransmission, thereby implicating non-NMDA receptors in the short-term action of estradiol [16]. It can be blocked by non-NMDA, but not NMDA, antagonists [16]. A non-NMDA mechanism of action is supported by a more recent preclinical model which suggests that E2 binds ERβR to increase glutamatergic AMPAR-mediated EPSPs [26] and binds ERαR to acutely suppress presynaptic GABA release and IPSPs via a mGluR1-endocannabinoid mechanism [27]. The complex role of estrogen, however, is illustrated by evidence in some models that estradiol can raise seizure thresholds in the hippocampal region and provide neuroprotection against seizure induced injury [14]. In summary, the combination of estradiol priming effects and direct membrane effects may converge on CA1 hippocampal neurons to exert the neuroexcitatory effects of estradiol.
Estrogen receptor-containing neurons co-localize with other neurotransmitters such as acetyl choline and growth factors such as brain derived neurotrophic factors to modulate neuronal excitability and seizure thresholds [28, 29].
Logothetis et al. [30] clinically showed that intravenously administered conjugated estrogen clearly activated epileptiform discharges in 11 of 16 women and was associated with clinical seizures in 4 cases.
Progesterone
Progesterone and particularly some of its neuroactive metabolites, most notably allopregnanolone, exert direct membrane-mediated inhibitory effects by potentiating GABAA-mediated chloride conductance [9, 31, 32]. It also potentiates the action of the powerful endogenous inhibitory substance adenosine [33]. Progesterone itself also substantially diminishes nicotinic acetylcholine receptor-mediated conductance, which may be relevant to autosomal dominant nocturnal frontal lobe epilepsy [34].
Progesterone may act via genomic mechanisms to influence the enzymatic activity controlling the synthesis and release of various neurotransmitters and neuromodulators produced by progesterone receptor containing neurons [8]. Progesterone binds specific cytosolic receptors not only to produce its own characteristic effects but also to lower estrogen receptor numbers and, thereby, antagonize estrogen actions [35].
Chronic progesterone decreases the number of hippocampal CA1 dendritic spines and excitatory synapses faster than the simple withdrawal of estrogen, counteracting the stimulatory effects of estradiol [23]. Progesterone and allopregnanolone have also been shown to have neuroprotective effects on hippocampal neurons in kainic acid induced seizure models [36].
In most adult female animal models, progesterone depresses neuronal firing, [37] and lessens spontaneous and induced epileptiform discharges [20–22, 36–38]. It retards kindling and decreases seizure occurrence [20–22, 36–38].
Backstrom et al. [39] found that intravenous infusion of progesterone, sufficient to produce luteal phase serum levels, was associated with a significant decrease in interictal spike frequency in four of seven women with partial epilepsy.
Neurosteroids
Most of the membrane effect of progesterone is due to the action of its 3α-hydroxylated (i. e. A-ring-reduced) metabolite, 3α-hydroxy-5α-pregnane-20-one or allopregnanolone (AP) [9, 32]. AP and the 3,5-hydroxylated natural metabolite of the mineralocorticoid deoxycorticosterone, allotetrahydro-deoxycorticosterone (allo-THDOC) are among the most potent of a number of endogenous neuroactive steroids with a direct membrane effect on neuronal excitability [9, 31, 32]. AP, but not allo-THDOC, is devoid of hormonal effects and may, together with other related neuroactive steroids, be thought of as an endogenous regulator of brain excitability with anxiolytic, sedative-hypnotic and anticonvulsant properties [9, 31, 32]. AP and allo-THDOC hyperpolarize hippocampal and other neurons by potentiating GABAA-mediated inhibition [9, 32]. At physiological (nanogram) with an extrasynaptic steroid-specific site near the synaptic receptor to facilitate chloride channel opening and prolong the inhibitory action of GABA on neurons [9, 31, 32, 40, 41]. At higher pharmacological (micromolar) concentrations, AP also has a direct effect at the synaptic GABAA receptor to induce chloride currents [9, 32]. AP is one of the most potent ligands of GABAA receptors in the CNS, with affinities similar to those of the potent benzodiazepine, flunitrazepam, and approximately a thousand times higher than pentobarbital [9, 32]. The parent steroid, progesterone, enhances GABA-induced chloride currents only weakly and only in high concentrations [9, 41]. Plasma and brain levels of AP parallel those of progesterone in rats. In women, plasma levels of AP correlate with progesterone levels during the menstrual cycle and pregnancy [9]. However, the brain activity of progesterone and AP is not dependent solely on ovarian and adrenal production, as they are both synthesized de novo in the brain [42]. Their synthesis is region-specific and includes the cortex and the hippocampus [42]. By contrast, allo-THDOC is only synthesized by the adrenal gland and not in the brain [9].
AP, allo-THDOC and a number of other endogenous and synthetic pregnane steroids have a potent anticonvulsant effect in bicuculline-, metrazol-, picrotoxin-, pentylenetetrazol-, pilocarpine- and kainic acid-induced seizures and against status epilepticus, but are ineffective against electroshock and strychnine-induced seizures [31, 43–45]. The anticonvulsant properties of allopregnanolone resemble those of the benzodiazepine, clonazepam [31, 45]. AP is less potent than clonazepam but may have lower relative toxicity [44, 45]. The anticonvulsant effect of AP is greater in female rats in the diestrus 1 part of the ovulatory cycle (equivalent to human mid-luteal phase when progesterone levels are high) than in estrus (equivalent to ovulation when estrogen levels are high) or in the male [40]. Enhanced mid-luteal efficacy at the GABAA receptor may be related to a progesterone induced enhanced formation of the δ GABAA receptor subtype [40]. Rapid withdrawal of progesterone in late diestrus makes the GABAA receptor insensitive to benzodiazepine, but not AP, perhaps as the result of a decrease in the benzodiazepine sensitive synaptic GABAA receptors [46]. This effect can be blocked by inhibiting the formation of the α4 subunit of the GABAA receptor [40, 46].
By contrast, some sulfated neuroactive steroids have excitatory neuronal effects. They include pregnenolone sulfate and dehydroepiandrosterone sulfate (DHEAS), the naturally occurring sulfated esters of the progesterone precursor pregnenolone and progesterone metabolite DHEA [9]. They increase neuronal firing when directly applied to neurons by negatively modulating the GABAA receptor [9] and by facilitating glutamate-induced excitation at the NMDA receptor [47]. In animal seizure models, pregnenolone sulfate and DHEAS have a proconvulsant effect [48]. It is to be noted that serum DHEAS levels are substantially reduced by enzyme inducing antiepileptic drugs such as phenytoin and carbamazepine [49, 50].
Hormonal treatment
Progestogen therapy
The term “progestogen” refers to the broad class of progestational agents. These include progesterone, (i. e. naturally occurring progesterone), and progestins (i. e. synthetic progestational agents). Progestogen treatment (Tab. 1 and 2) has taken two forms: 1) cyclic progesterone therapy that supplements progesterone during the luteal phase and withdraws it gradually premenstrually and 2) suppressive therapy in which the goal is to suppress the menstrual cycle, which is generally accomplished using injectable progestins or gonadotropin releasing-hormone analogues.
Cyclic progesterone therapy
In contrast to published cyclic oral progestin investigations that did not result in significant reduction of seizure frequency [51, 52], two open-label trials of adjunctive progesterone therapy for women with catamenial epilepsy resulted in clinically important and statistically significant reductions in seizure occurrence (Tab. 2) [53, 54]. In one investigation of women who had inadequate luteal phase cycles with catamenial exacerbation of intractable complex partial seizures, 6 out of 8 women experienced improved seizure control with a 68 % decline in average monthly seizure frequency over 3 months for the whole group [53]. In a subsequent open trial of adjunctive cyclic progesterone versus the optimal antiseizure medication alone in 25 women (14 with inadequate luteal phase or anovulatory cycles and 11 with normal cycles and perimenstrual seizure exacerbation), 19 (72 %) experienced fewer seizures with an overall average monthly decline of 54 % for complex partial and 58 % for secondary generalized seizures over 3 months [54]. Progesterone was more efficacious when administered during the entire second half of the cycle, rather than just premenstrually, and then tapered and discontinued gradually over 3 or 4 days at the end of the cycle [54]. Failure to taper gradually premenstrually can result in rebound seizure exacerbation. At 3 years, the average daily seizure frequency per patient showed that the 15 women who remained on cyclic progesterone therapy and their original antiepileptic drugs continued to show improved seizure control in comparison to their own baseline (Tab. 2 – 3-year follow-up) [55]. Three women were entirely seizure free. Four had total seizure reductions of 75–99 %. Eight had reductions of 50–74 %. Complex partial seizures in these 15 were lower by a statistically significant 62 % (baseline: 0.328, 3-year follow-up: 0.125; p < 0.01); secondary generalized motor seizures, by 74 % (baseline: 0.148, 3-year follow-up: 0.038; p < 0.01). Antiepileptic drug serum levels continued to show no significant change. The three remaining women who continued on progesterone therapy had 10–50 % improvement at the end of the original investigation at 3 months and were not considered further because they changed antiepileptic drugs.
The NIH Progesterone Trial was a randomized, placebo-controlled, double-blind, clinical trial of progesterone versus placebo therapy in the treatment of intractable seizures in women with and without catamenial epilepsy [56]. The principal outcomes were the proportion of ≥ 50 % responders and the change in seizure frequency between the 3-month baseline and 3-month treatment phases. A sample size of 640 was determined as the enrollment requirement to show a significant difference (p ≤ 0.05) between treatments for ≥ 50 % responders with 80 % power for 35 % progesterone vs 15 % placebo responders in the catamenial stratum. The large sample size was required since only about one-third of the women was expected to show a catamenial pattern of seizure exacerbation. Catamenial designation was based on the demonstration of catameniality in two of three baseline cycles using the 1997 Herzog et al. [54] established points of inflection cutoffs for designation of C1, 2 & 3 patterns. The trial enrolled only 462 women and randomized the 294 subjects who completed the baseline phase. Randomization was carried out separately for the catamenial and non-catamenial strata, 2:1 to progesterone or matching placebo treatment. The treatment regimen consisted of baseline optimal antiepileptic drug treatment plus adjunctive progesterone 200 mg. lozenges or matching placebo. A whole lozenge was taken three times daily on Days 14–25, ½ lozenge three times daily on Days 26–27, ¼ lozenge taken three times daily on Day 28 and then no lozenges until the next Day 14.
The findings of the NIH Progesterone Trial showed that cyclic progesterone is comparable to placebo in the treatment of intractable seizures in women with partial epilepsy [56]. A pre-specified secondary analysis identified a subset of women with perimenstrual seizure exacerbation who were responsive to progesterone treatment. This post-hoc predictor analysis using binary logistic regression analysis (dependent variable being ≥ 50 % progesterone responder: yes or no) found that the level of perimenstrual catameniality (C1 level) is a predictor of the efficacy of progesterone treatment. There was significant interaction between C1 level and treatment. With increasing C1 levels, responder rates increased progressively from 21.3 to 57.1 % for progesterone versus only 19.6 % to 20.0 % with placebo (Fig. 2a). Changes in average daily seizure frequency progressed from −25.5 to −71.0 % for progesterone versus only −25.0 to −26.3 % for placebo (Fig. 2b). There was also significant interaction between C1 level and progesterone treatment for the most severe seizure type, secondary generalized tonic-clonic seizures and complex partial seizures but not simple partial seizures. The separation between responder rates for all seizures combined for progesterone (27.3 %) versus placebo (14.3 %) treatments was not significant at C1 level ≥ 1.69, the C1 cutoff level selected for designation to the catamenial stratum. The separation did achieve statistical significance at C1 level ≥ 2 (28.6 % versus 12.9 %) and at C1 level ≥ 3, the separation (37.8 % versus 11.1 %) was both significant (p = 0.0372) and achieved the anticipated clinically important separation goal of the trial, i. e. ≥ 35 % responder rate for progesterone versus ≤ 15 % responder rate for placebo.
In the trial [56], 38.1 % of the subjects had C1 level ≥ 1.69, 34.4 % had C1 level ≥ 2 and 21.4 % had C1 level ≥ 3 levels of perimenstrual exacerbation (Tab. 3). It is to be noted that 12.2 % had C1 level ≥ 6, which is almost identical to the 12.4 % found in the Duncan study (Tab. 3) [57]. The findings suggest that 21.4 % of women with intractable seizures, i. e. the percent that had C1 level ≥ 3 baseline, might be candidates for cyclic progesterone supplement.
Another tertiary outcome of the trial was to determine whether allopregnanolone (AP) may mediate seizure reduction in progesterone treated women with epilepsy [58]. AP levels were significantly greater in treated cycles than in baseline cycles for women treated with progesterone but not placebos, regardless of the catamenial designation. There was a significant inverse correlation between changes in seizure frequency and changes in AP levels for the subset of subjects who showed a significantly greater responder rate in the post hoc analysis of the trial, i. e. subjects who had a threefold or greater increase in average daily seizure frequency perimenstrually as compared to the mid-follicular and mid-luteal phases (C1 ≥ 3): r = −0.442, p = 0.013 and specifically for C1 ≥ 3 progesterone treated subjects (r = −0.452, p = 0.035), but not other groups (C1 ≥ 3 placebo: r = −0.318, C1 < 3 progesterone: r = 0.099, C1 < 3 placebo: r = 0.131; p = NS). The findings support AP as a mediator of seizure reduction in progesterone treated women who have a substantial level of perimenstrually exacerbated seizures.
Failure of the trial to prove the principal hypothesis may relate to the design that attempted to treat three patterns of catamenial epilepsy which likely differ in pathophysiology with a single treatment regimen [4, 56, 59]. Specifically, cyclic progesterone supplement may have greater efficacy where progesterone withdrawal (C1 pattern), rather than estrogen surge (C2) or high luteal phase estradiol/progesterone serum level ratios (C3 pattern), are causally implicated. The design also assumed that the mathematically determined cutoff for catamenial designation would match the cutoff for a significant progesterone response. The absence of a significant difference between progesterone and placebo responders at the C1 cutoff level of ≥ 1.69 and finding of a significant difference at a clinically important level at C1 level ≥ 3 may suggest that there is a difference between the catamenial level that mathematically best distinguishes hormonally sensitive seizures and the level that distinguishes progesterone responders at a statistically significant and clinically important level. The actual enrollment of a larger sample size might have achieved a significant difference, i. e. 234 progesterone and 117 placebo-treated subjects might show the demonstrated C1 ≥ 1.69 progesterone responder rate of 27.3 % versus placebo rate of 14.2 % with p ≤ .05 and power of 0.80. Even with these larger numbers, however, the responder rate would still not achieve what we consider to be a clinically important response level of ≥ 35 %.
Progestin therapy
Parenteral depomedroxyprogesterone may lower seizure frequency when it is given in sufficient dosage to induce amenorrhea [52, 60]. In one open label study of 14 women with refractory partial seizures and normal ovulatory cycles, parenteral depomedroxyprogesterone administration in doses large enough to induce amenorrhea (i. e. 120–150 mg every 6–12 weeks) resulted in a 39 % seizure reduction [52]. It was unclear whether the effect was due to direct anticonvulsant activity of medroxyprogesterone or to the hormonal consequences of the induced amenorrhea. One patient who had an absence of seizures rather than partial ones did not improve. Side effects included those encountered with natural progesterone. Depot administration, however, is also commonly associated with hot flashes, irregular breakthrough vaginal bleeding and a lengthy delay of 6 to 12 months in the return of regular ovulatory cycles [52]. Long-term hypoestrogenic effects on cardiovascular and emotional status need to be considered with chronic use. Bone density is only partially maintained.
Oral synthetic progestins administered cyclically or continuously have not proven to be an effective therapy for seizures in clinical investigations [51, 52], although individual successes with continuous daily oral use of norethistrone and combination pills have been reported [61].
Gonadotropin-releasing hormone analogue therapy
Bauer et al. [62] used triptorelin, a synthetic gonadotropin-releasing hormone (GnRH) analogue (3.75 mg) in a controlled release depot form intramuscularly every 4 weeks for an average of 11.8 months in 10 women (aged 20–50) with catamenial seizures intractable to high therapeutic doses of carbamazepine, diphenylhydantoin, phenobarbital and valproic acid in monotherapy or combined. They remained on a stable dose of the anticonvulsant throughout the period of treatment with triptorelin. They reported that three patients became seizure free; four showed a decrease in seizure frequency of up to 50 %. In one patient the duration of seizures was shortened; in two patients there was no therapeutic effect. These results were attained within the first two months of starting triptorelin. The study was not a controlled study and longer term follow-up was not available for some of the patients. Serum LH and estrogen were measured in one patient before and during the second month of triptorelin treatment, and as expected showed marked inhibition of LH and estrogen production. All the women became amenorrheic. Eight of the ten patients experienced hot flushes, headache or weight gain.
Haider and Barnett [63] reported on the use of goserelin 3.6 mg subcutaneously every 4 weeks in a 41 year old woman who had had frequent catamenial status epilepticus despite therapeutic anticonvulsant drug levels, which also did not respond to levonorgestrel/ethinyl estradiol. They reported a decrease in frequency from ten admissions for status to three over a similar period.
GnRH analogues basically create a medical oophorectomy. Common side effects are flushing, vaginal dryness and dyspareunia. Serious long-term risks include osteoporosis and cardiovascular disease. Reid and Gangar [64] suggested the addition of medroxyprogesterone acetate and conjugated estrogens to goserelin to prevent this while still abolishing most of the cyclical fluctuations of ovarian hormones. Finkelstein et al. [65] recently discussed the use of parathyroid hormone to prevent bone loss in women treated with GnRH analogues. Although neither Bauer et al. [62] nor Haider and Barrett [63] reported exacerbation of seizures with GnRH analogues, Herzog [66] found that during the first 3 weeks, when there is an initial stimulation of estrogen before its production is inhibited, some women experienced such a marked exacerbation of seizures and auras that they could not tolerate further use of GnRH analogue.
Responder rate and seizure change in relation to C1 level: progesterone vs placebo treatment
This is a plot of ≥ 50 % responders versus the level of perimenstrual seizure exacerbation (C1 level). C1 levels were determined during baseline and are expressed as multiples of the combined mid-follicular and mid-luteal seizure frequencies. Each level includes all women who had seizure exacerbation greater than or equal to that specific level of catameniality. With increasing C1 levels, the rate of ≥ 50 % responders increased from 21.3 % to 57.1 % with progesterone treatment as compared to an increase of only 19.6 % to 20.0 % with placebo treatment. The anticipated primary outcome that 35 % of catamenial progesterone treated versus 15 % of placebo treated women would show a ≥ 50 % reduction in seizure frequency is realized at C1 level ≥ 3 where 37.8 % of progesterone treated as compared to 11.1 % of placebo treated women were ≥ 50 % responders (p = 0.0372). In comparison to the responder rate of the combined placebo group, the progesterone responder rates are significantly greater at each C1 level ≥ 3.
With increasing C1 levels from 1–10, the percent reduction in ADSF (mean ± SEM) progressed from 25.5 % to 71.0 % for progesterone as compared to 25.0 to 26.2 % for placebos. Separation between the treatments reached significance at C1 levels ≥ 4. In comparison to change in ADSF in the combined placebo group, the changes in ADSF in progesterone treated subjects are significant at each C1 level ≥ 3.
Abbreviations
- C1:
-
perimenstrual (Day −3 to +3)
- C2:
-
periovulatory (Day 10 to −13)
- C3:
-
luteal in anovulatory cycles (Day 10 to 3)
- Prog:
-
progesterone
- Plac:
-
placebo
- C1:
-
perimenstrual seizure exacerbation
References
Tauboll E, Lundervold A, Gjerstad L (1991) Temporal distribution of seizures in epilepsy. Epilep Res 8:153–165
Herzog AG, Fowler KM, Sperling MR, Massaro JM, the Progesterone Trial Study Group (2015) Distribution of Seizures Across the Menstrual Cycle. Epilepsia 56(5):e58–e62
Almqvist R (1955) The rhythm of epileptic attacks and its relationship to the menstrual cycle. Acta Psychiatr Neurol Scand 30(suppl 105):1–116
Herzog AG, Klein P, Ransil BJ (1997) Three patterns of catamenial epilepsy. Epilepsia 38:1082–1088
Backstrom T (1976) Epileptic seizures in women related to plasma estrogen and progesterone during the menstrual cycle. Acta Neurol Scand 54:321–347
Laidlaw J (1956) Catamenial epilepsy. Lancet 271:1235–1237
Herzog AG et al (2004) Frequency of catamenial seizure exacerbation in women with localization-related epilepsy. Annals of Neurology 56:431–434
McEwen BS (1994) How do sex and stress hormones affect nerve cells? Annals N Y Acad Sci 743:1–16
Paul SM, Purdy RH (1992) Neuroactive steroids. FASEB Journal 6:2311–2322
Klein P, Herzog AG (1997) Endocrine aspects of epilepsy. In: Pretel S, Knigge KM, Prasad A (Hrsg) Neuroendocrine and neuromolecular aspects of epilepsy and brain disorders. Research Signpost, Trivandrum, India, S 111–140
Hojo Y, Hattori TA, Enami T, Furukawa A, Suzuki K, Ishii H, Mukai H, Morrison JH, Janssen WGM, Kominami S et al (2004) Adult male rat hippocampus synthesizes estradiol from pregnenolone by cytochromes P45017a and P450 aromatase localized in neurons. Proc Natl Acad Sci USA 101:865–870
Hojo Y, Higo S, Ishii H, Ooishi Y, Mukai H, Murakami G, Kominami T, Kimoto T, Honma S, Poirier D, Kawato S (2013) Comparison between hippocampus-synthesized and circulation-derived sex steroids in the hippocampus. Endocrinology 150:5106–5112
Marcus EM, Watson CW, Goodman PL (1966) Effects of steroids on cerebral electrical activity. Arch Neurol 15:521–532
Velíšková J, De Jesus G, Kaur R, Velíšek L (2010) Females, their estrogens and seizures. Epilepsia 51(Suppl 3):141–144
Teresawa E, Timiras P (1968) Electrical activity during the estrous cycle of the rat; cyclic changes in limbic structures. Endocrinology 83:207–216
Wong M, Moss R (1992) Long-term and short-term electrophysiological effects of estrogen on the synaptic properties of hippocampal CA1 neurons. J Neurosci 12:3217–3225
Kawakami M, Teresawa E, Ibuki T (1970) Changes in multiple unit activity in the brain during the estrous cycle. Neuroendocrinology 6:30–48
Logothetis J, Harner R (1960) Electrocortical activation by estrogens. Arch Neurol 3:290–297
Hom AC, Buterbaugh GG (1986) Estrogen alters the acquisition of seizures kindled by repeated amygdala stimulation or pentylenetetrazol administration in ovariectomized female rats. Epilepsia 27:103–108
Nicoletti F et al (1985) Comparative effects of estradiol benzoate, the antiestrogen clomiphene citrate, and the progestin medroxyprogesterone acetate on kainic acid-induced seizures in male and female rats. Epilepsia 26:252–257
Spiegel E, Wycis H (1945) Anticonvulsant effects of steroids. J Lab Clin Med 30:947–953
Woolley DE, Timiras PS (1962) The gonad-brain relationship: effects of female sex hormones on electroshock convulsions in the rat. Endocrinology 70:196–209
Woolley CS, McEwen BS (1993) Roles of estradiol and progesterone in regulation of hippocampal dendritic spine density during the estrous cycle in the rat. J Comp Neurol 336:293–306
Woolley CS, McEwen BS (1994) Estradiol regulates hippocampal dendritic spine density via an N-methyl-D-aspartate receptor-dependent mechanism. J Neurosci 14:7680–7687
Schumacher M, Coirini H, McEwen BS (1989) Regulation of high affinity GABA, receptors in the dorsal hippocampus by estradiol and progesterone. Brain Res 487:178–183
Smejkalova T, Woolley CS (2010) Estradiol acutely potentiates hippocampal excitatory synaptic transmission through a presynaptic mechanism. J Neurosci 30:16137–16148
Huang GZ, Woolley CS (2012) Estradiol acutely suppresses inhibition in the hippocampus through a sex-specific endocannabinoid and mGluR-dependent mechanism. Neuron 74:801–808
Luine VN, Renner KJ, McEwen BS (1986) Sex-dependent differences in estrogen regulation of choline acetyltransferase are altered by neonatal treatments. Endocrinology 119:874–878
Harte-Hardgrove L, MacLuskey NL, Scharfman H (2013) Brain-derived neurotrophic factor-estragon interactions in the hippocampal mossy fiber pathway: implications for normal brain function and disease. Neuroscience 239:46–66
Logothetis J, Harner R, Morrell F, Torres F (1959) The role of estrogens in catamenial exacerbation of epilepsy. Neurol (Minneap) 9:352–360
Majewska MD, Harrison NL, Schwartz RD, Barker JL, Paul SM (1986) Steroid hormone metabolites are barbiturate-like modulators of the GABA receptor. Science 232:1004–1007
Gee KW, McCauley LD, Lan NC (1995) A putative receptor for neurosteroids on the GABA receptor complex: the pharmacological properties and therapeutic potential of epalons. Crit Rev Neurobiol 9:207–227
Phyllis JW (1986) Potentiation of the depression by adenosine of rat cerebral cortex neurones by progestational agents. Brit J Pharmacol 89:693–702
Valera S, Ballivet M, Bertrand D (1992) Progesterone modulates a neuronal nicotinic acetylcholine receptor. Proc Nat Acad Sci USA 89:9949–9953
Hsueh AJW, Peck EJ, Clark JH (1976) Control of uterine estrogen receptor levels by progesterone. Endocrinology 98:438–444
Frye CA (1995) The neurosteroid 3a-5a-THP has antiseizure and possible neuroprotective effects in an animal model of epilepsy. Brain Res 696:113–120
Smith SS, Waterhouse BD, Woodward DJ (1987) Sex steroid effects on extrahypothalamic CNS. II. Progesterone, alone and in combination with estrogen, modulates cerebellar responses to amino acid neurotransmitters. Brain Res 422:52–62
Landgren S, Backstrom T, Kalistratov G (1978) The effect of progesterone on the spontaneous interictal spike evoked by the application of penicillin to the cat’s cerebral cortex. J Neurol Sci 36:119–133
Backstrom T, Zetterlund B, Blom S, Romano M (1984) Effects of intravenous progesterone infusions on the epileptic discharge frequency in women with partial epilepsy. Acta Neurol Scand 69:240–248
Maguire JL, Stell BM, Rafizadeh M, Mody I (2005) Ovarian cycle-linked changes in GABAA receptors mediating tonic inhibition alter seizure susceptibility and anxiety. Nat Neurosci 8:797–804
Wu FS, Gibbs TT, Farb DH (1990) Inverse modulation of g-aminobutyric acid- and glycine-induced currents by progesterone. Mol Pharmacol 37:597–602
Cheney DL, Uzunov D, Costa E, Guidotti A (1995) Gas chromatographic-mass fragmentographic quantitation of 3a-hydroxy-5a-pragnan-20-one (allopregnanolone) and its precursors in blood and brain of adrenalectomized and castrated rats. J Neurosci 15:4641–4650
Belleli D, Bolger MB, Gee KW (1989) Anticonvulsant profile of the progesterone metabolite 5a-pregnan-3a-ol-20-one. Eur J Pharmacol 166:325–329
Kokate TG, Svensson BE, Rogawski MA (1994) Anticonvulsant activity of neurosteroids: correlation with g-aminobutyric acid-evoked chloride current potentiation. J Pharmacol ExpTher 270:1223–1229
Kokate TG, Cohen AL, Karp E, Rogawski MA (1996) Neuroactive steroids protect against pilocarpine- and kainic acid-induced limbic seizures and status epilepticus in mice. Neuropharmacology 35:1049–1056
Smith SS, Gong QH, Hau F-C, Markowitz RS, ffrench-Mullen JMH, Li X (1998) GABAA receptor α4 subunit suppression prevents withdrawal properties of an endogenous steroid. Nature 392:926–930
Irwin RP, Maragakis NJ, Rogawski MA, Purdy RH, Farb DH, Paul SM (1992) Pregnenolone sulfate augments NMDA receptor mediated increases in intracellular Ca2+ in cultured rat hippocampal neurons. Neurosci Lett 141:30–34
Heuser G, Ling GM, Buchwald NA (1965) Sedation or seizures as dose-dependent effects of steroids. Arch Neurol 13:195–203
Levesque LA, Herzog AG, Seibel MM (1986) The effect of phenytoin and carbamazepine on dehydroepiandrosterone sulfate in men and women who have partial seizures with temporal lobe involvement. J Clin Endocrinol Metab 63:243–245
Herzog AG et al (2004) Differential effects of antiepileptic drugs on serum neuroactive steroid concentrations in men with localization-related epilepsy. Epilepsia 45:122–123
Dana Haeri J, Richens A (1983) Effect of norethistrone on seizures associated with menstruation. Epilepsia 24:377–381
Mattson RH, Cramer JA, Caldwell BV, Siconolfi BC (1984) Treatment of seizures with medroxyprogesterone acetate: preliminary report. Neurol (Clevel) 34:1255–1258
Herzog AG (1986) Intermittent progesterone therapy and frequency of complex partial seizures in women with menstrual disorders. Neurology 36:1607–1610
Herzog AG (1995) Progesterone therapy in complex partial and secondary generalized seizures. Neurology 45:1660–1662
Herzog AG (1999) Progesterone therapy in women with epilepsy: a 3-year follow-up. Neurology 52:1917–1918
Herzog AG, Fowler KM, Smithson SD, Kalayjian LA, Heck CN, Sperling MR, Liporace JD, Harden CL, Dworetzky BA, Pennell PB, Massaro JM, Progesterone Trial Study Group (2012) Progesterone versus placebo therapy for women with epilepsy: a randomized clinical trial. Neurology 78:1959–1966
Duncan S, Read CL, Brodie MJ (1993) How common is catamenial epilepsy? Epilepsia 34:827–831
Herzog AG, Frye CA, Progesterone Trial Study Group (2014) Allopregnanolone levels and seizure frequency in progesterone treated women with epilepsy. Neurology 83:345–348
Herzog AG (2008) Catamenial Epilepsy: definition, prevalence, pathophysiology and treatment. Seizure 17(2):151–159
Zimmerman AW, Holden KR, Reiter EO, Dekaban AS (1973) Medroxyprogesterone acetate in the treatment of seizures associated with menstruation. J Pediatr 83:959–963
Hall SM (1977) Treatment of menstrual epilepsy with a progesterone-only oral contraceptive. Epilepsia 18:235–236
Bauer J, Wildt L, Flugel D, Stefan H (1992) The effect of a synthetic GnRH analogue on catamenial epilepsy: a study in ten patients. J Neurol 239:284–286
Haider Y, Barnett DB (1991) Catamenial epilepsy and goserelin. Lancet 338:1530
Reid B, Gangar KF (1992) Catamenial epilepsy and goserelin. Lancet 339:253
Finkelstein JS, Klibenski A, Schaefer EH, Hornstein MD, Schiff I, Neer RM (1994) Parathyroid hormone for the prevention of bone loss induced by estrogen deficiency. New Engl J Med 331:1618–1623
Herzog AG (1991) Reproductive endocrine considerations and hormonal therapy for women with epilepsy. Epilepsia 32:S27–S33
Acknowledgement
The NIH Progesterone Trial was supported by a grant from the National Institute of Neurological Disorders and Stroke (NIH R01 NS39466).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Andrew G. Herzog states that there are no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Rights and permissions
About this article
Cite this article
Herzog, A.G. Catamenial epilepsy: current concepts of definition, prevalence, pathophysiology and treatment. Z. Epileptol. 28, 295–303 (2015). https://doi.org/10.1007/s10309-015-0005-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10309-015-0005-6