Abstract
Purpose
Hypertension is one of the major causes of cardiovascular morbidity and mortality in the USA and disproportionately affects Black women. Endothelial-derived nitric oxide (eNO) substantially regulates blood pressure in humans, and impaired NO-mediated vasodilation has been reported in the Black population. Previous studies using an NO synthase inhibitor, NG-monomethyl-L-arginine (L-NMMA) did not fully determine the NO contribution to blood pressure because of baroreflex buffering. Therefore, in the present study we used trimethaphan, a ganglionic blocker, to inhibit baroreflex buffering and study NO modulation of blood pressure in Black women during L-NMMA infusion.
Methods
L-NMMA at doses of 250 μg/kg per minute was infused in combination with trimethaphan at doses of 4 mg/min to eliminate baroreflex mechanisms. Heart rate (HR) was obtained with continuous electrocardiogram monitoring, and continuous blood pressure was measured with the volume clamp method. The increase in systolic blood pressure (SBP) during both infusions was used to estimate the contribution of NO to blood pressure.
Results
Ten Black (age range 30–50 years, body mass index [BMI] 30–45 kg/m2), and nine White women (age range 30–50 years, body mass index 30–45 kg/m2) were enrolled in this study. During autonomic blockade, there was no difference in the decrease in SBP between Black and White women (− 20 ± 16.45 vs. − 24 ± 15.49 mm Hg, respectively; P = 0.659). When autonomic blockade was combined with L-NMMA, Black women had a significant increase in SBP compared to White women (54 ± 13.62 vs. 39 ± 09.64 mm Hg, respectively; P = 0.022, respectively).
Conclusion
Autonomic blood pressure regulation was similar between Black and White women. However, NO contribution to blood pressure was significantly greater in Black women compared to White women.
Registration
ClinicalTrials.gov: NCT01122407.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity affects more than 30% of the US population and contributes to cardiovascular mortality, mostly due to diabetes and increased cardiovascular risks [1]. Black women are disproportionately affected by obesity compared with men or White women [2, 3]. Obesity precedes the development of hypertension and insulin resistance [4], both of which contribute to cardiovascular morbidity [5, 6]. The reported annual mortality rate among Black women due to cardiovascular events is 286 per 100,000 Black women [7]. Importantly, hypertension affects Black women at a younger age and is associated with a fivefold increase in coronary heart disease [8].
Obesity is associated with increased sympathetic activity. Microneurography, which directly measures baroreflex-modulated sympathetic traffic to skeletal muscle, is directly associated with body mass index (BMI) and fat mass [9,10,11]. We previously reported that this sympathetic overactivity contributes to obesity-associated hypertension in White women but not in Black women. Hence, other mechanisms may contribute to the pathophysiology of blood pressure regulation in this latter group.
Nitric oxide (NO) plays an important role in blood pressure regulation through its vasodilatory properties [12] and is arguably one of the most important metabolic modulators of blood pressure and vascular tone [13]. This endogenous-formed gas is synthesized in nearly all cell types, tissues, and organs in the human body [14] through three different isoforms of NO synthase enzyme, each with unique functional properties [15]. Endothelial-derived nitric oxide synthase (eNOS) is expressed in endothelial cells, platelets, the human placenta, and myocardial cells [14] and causes vasodilation with a subsequent decrease in blood pressure.
The effect of race on NO-mediated vasodilation has been assessed through the evaluation of vascular reactivity in response to the release of several factors, including NO, endothelium-derived hyperpolarization factor (EDHF), and prostaglandins; taken together, these studies reported an impaired vasodilatory response [16, 21]. Additional studies have also found a blunted endothelium-dependent vasodilation in response to a number of agonists, including acetylcholine [22, 23], methacholine [22, 24, 25], bradykinin [22], isoproterenol [25,26,27], sodium nitroprusside [22], exercise [28], mental stress [29], and, in some studies, also to ischemic stimulus on flow-mediated dilatation [28, 30, 31]. Despite the use of different methodologies and the limitations inherent to these techniques, there is consensus among the authors of these studies that endothelial-dependent vasodilation was abnormal in Blacks.
Importantly, the relative contribution of endothelial-derived NO (eNO) to blood pressure regulation in Black obese women is unknown. Therefore, the purpose of this study was to determine the contribution of NO on blood pressure regulation in Black obese women compared with White obese women. Considering that Black Americans have impaired endothelial-mediated vasodilation, we hypothesized that Black women would have less tonic restraint of blood pressure by NO compared with White women [32].
Methods
Study subjects
Subjects were recruited from the Vanderbilt University General Clinical Research Center volunteer database. Eligibility criteria included obesity, defined as BMI between 30 and 45 kg/m2, age range between 30 and 50 years, and Black and White women based on both parents being of the same race. Women who were pregnant or breastfeeding and had a history of coronary artery disease, heart failure, renal or liver failure, and significant weight gain or loss in the past 3 months were excluded. The study was approved by the Vanderbilt University Institutional Review Board, and all participants gave written informed consent before study entry. The study was registered in clinicaltrials.gov (NCT01122407). The data reporting the decrease in blood pressure with trimethaphan (TMT) was previously published as part of a larger cohort [33]; the NG-monomethyl-l-arginine (L-NMMA) data have not been previously published.
Experimental design
All subjects underwent a thorough clinical examination and laboratory analyses (cell blood count, basal metabolic panel, urinalyses, and urinary pregnancy test) prior to enrollment. Subjects were given a weight-maintenance sodium-balanced diet (50% carbohydrates, 30% fat, 20% protein, 150 mEq sodium) 3 days prior to the infusion protocol. They were also told to refrain from all food and beverages containing methylxanthines. The study was conducted in the morning, after a 12-h overnight fast.
The infusion protocol is presented in Fig. 1. Subjects were fitted with two intravenous (IV) catheters, one each in the antecubital vein of each arm. One arm had three infusion ports connected to the IV catheter for TMT (Cambridge Pharmaceuticals, Newcastle upon Tyne, UK), phenylephrine (an alpha-1-adrenergic agonist), and L-NMMA infusion. The opposite arm was used for blood draws and phenylephrine boluses. Heart rate (HR) was obtained with continuous electrocardiogram monitoring, and continuous blood pressure was measured with the volume clamp method (Finapres, Enschede, The Netherlands) and intermittently with automated brachial cuff pressure with standard sphygmomanometry. Cardiac output (CO) was measured at intervals with the inert gas re-breathing method (Innocor CO; COSMED Nordic ApS, Odense, Denmark) [34].
Pictorial depiction of the experiment design. Blood pressure and R-R intervals (red) were measured during ganglionic blockage using trimethaphan infusion with escalating dosages (1, 2, 4, up to 6 mg/min). Trimethaphan infusion was maintained after the establishment of the complete blockade. Baseline BP was restored by titrated Phe infusion. NO was blocked by L-NMMA infusion at 250 µg/kg/min. BP Blood pressure, DBP diastolic BP, ECG electrocardiogram, HR heart rate, L-NMMA NG-monomethyl-L-arginine, NO nitric oxide, Phe phenylephrine, SBP systolic BP
All subjects were allowed to rest in a quiet, thermoneutral environment for 30 min after instrumentation. Baseline hemodynamic parameters were recorded. Phenylephrine boluses were used to confirm abolished baroreflex-mediated prolongation of R-R intervals.
TMT was administered for 15 min, and phenylephrine boluses were repeated, starting at a dose of 2.5 ug until an increase of 25 mm Hg was achieved in systolic blood pressure (SBP) [35, 36]. Autonomic withdrawal can cause a mild decrease in blood pressure due to the low sympathetic tone present in the supine resting position. Therefore, we infused phenylephrine starting at a rate of 0.01 ug/kg/min and titrated to restore blood pressure to baseline levels; the infusion was maintained constant for the duration of the study. Then, L-NMMA was infused at 250 ug/kg per minute for 15 min or until SBP reached 150 mm Hg.
Estimation of autonomic blockade using spectral analysis of blood pressure and heart rate
All the of physiological data were recorded through a WINDAQ data acquisition system. The recordings were digitized with 14-bit resolution and 500-Hz sample frequency. An offline custom-written software program for data analysis in PV-Wave language (PV-wave; Visual Numerics Inc., Houston, TX, USA) was used to analyze data (DIANA, AD, Vanderbilt University, Nashville, TN, USA). A QRS detection algorithm, modified from Pan and Tompkins [37], generated beat-to-beat values. Beat-to-beat values of the RR interval and blood pressure were interposed, low pass filtered (cutoff: 2 Hz), and resampled (4 Hz).
Data segments of interest were used for the spectral analysis. Linear trends were removed, and power spectral density was estimated with a Fast Fourier Transform (FFT)-based algorithm using Welch’s method, using at least three segments of 256 data points with 50% overlapping and a Hanning window. According to task force recommendations, the power in the frequency ranges for very low frequencies (0.003 to < 0.04 Hz), low frequencies (LF: 0.04 to < 0.15 Hz), and high frequencies (HF: 0.15 to < 0.40 Hz) were calculated for each interval [38].
Spectral baroreflex transfer function gain
Bivariate power spectral analysis provided useful information about the temporal fluctuations between different hemodynamic parameters, such as HR and blood pressure. We estimated the power spectra, cross spectra, phase, coherence, and transfer function gain of SBP and R-R interval time series using FFT with a segment length of 256 s resampled with 4 Hz. The baroreflex gain was determined as the mean magnitude value of the transfer function in the low-frequency band with a negative phase and squared coherence value > 0.5.
Endpoints
The primary endpoint was the increase in SBP during combined NO synthase inhibition and autonomic blockade.
Secondary endpoints included the change in DBP and HR during combined NO synthase inhibition and autonomic blockade. Other surrogate measurements of sympathetic activity (low-frequency variability of SBP [LFSBP]), parasympathetic activity (high-frequency variability of HR [HFRRI]), and spontaneous baroreflex sensitivity (BRS) were also measured.
Statistical analysis
Standard graphing and screening techniques were employed to detect outliers and to ensure data accuracy. The data were assessed for normality by the Anderson–Darling test, Shapiro–Wilk test, and Kolmogorov–Smirnov test; all three tests were used to check the normality. If normality was violated, we applied a non-parametric method of analysis. Demographic data were presented as means with standard errors of the mean (SEM). We used a parametric Welch’s Correction test to compare the differences in primary outcomes (Delta SBP) and secondary outcomes as previously defined. All tests were two-tailed, and a P value of < 0.05 was considered to be significant. Analyses were performed using GraphPad Prism statistical software (version 9.5.0; GraphPad Software, San Diego, CA, USA).
Results
Demographic characteristics
A total of 19 (10 Black and 9 White) premenopausal and obese women were enrolled in the study. The enrolled subjects were mostly hypertensive (14 hypertensive and 4 healthy women). Demographic characteristics are shown in Table 1. Total cholesterol levels were lower in the Black women than in the White women (mean ± SD, 141 ± 52.91 vs. 187 ± 25.29 mg/dL, P = 0.051). No significant differences were found in SBP while resting and while upright between the groups. There were no significant differences found in urine analysis of sodium and creatinine levels between Black and White women (139 ± 1.94 vs. 138 ± 1.27 mEq/L, respectively, P = 0.251; 0.81 ± 0.11 vs. 0.71 ± 0.11 mg/dL, respectively, P = 0.070).
Effect of autonomic blockade on cardiovascular parameters
There was no difference between Black and White women in the decrease in SBP (− 20 ± 16.45 vs. − 24 ± 15.49 mmHg, respectively, P = 0.659; Fig. 2a) and DBP (-14 ± 11.53 vs. − 18 ± 10.88 mm Hg, respectively; P = 0.431; Fig. 2b). HR significantly increased more in Black women than in White women (23 ± 11.52 vs. 13 ± 16.54 bpm, respectively, P = 0.043; Fig. 2c).
Effect of autonomic withdrawal induced by the ganglionic blockade on blood pressure and heart rate in Black and White women. a Delta values of SBP at the end of trimethaphan infusion and changes in SBP induced by the autonomic blockade. b Delta values of DBP after the treatment with trimethaphan and resulting changes in DBP. c Delta heart rate values after trimethaphan infusion and any changes in heart rate induced by an autonomic blockade. Data are presented as mean ± standard error of the mean. Statistical analysis was performed using Welch’s Correction test. N = 10 for Black women and N = 9 for White women. P < 0.05 was set for statistical significance. DBP Diastolic blood pressure, SBP systolic blood pressure
There were no significant differences between Black and White women in CO (mean ± SEM, − 1 ± 01.13 vs. − 1 ± 01.07 L/min, respectively, P = 0.446) and systemic vascular resistance (SVR; − 1 ± 01.78 vs. − 1 ± 01.14 dynes/s/cm−5, respectively, P = 0.786)). There was also no difference in the decrease in stroke volume (SV) between the groups (− 30 ± 12.26 vs. − 30 ± 24.57 mL/beat, P = 0.978). The changes in CO, SV, and SVR before and after autonomic blockade are shown in Table 2.
Baseline HFRRI values were similar between the groups (mean ± SEM, 745 ± 215.90 vs. 845 ± 655.90 ms2, P = 0.114), as were baseline LFRRI values (915 ± 273.80 vs. 792 ± 493.20 ms2, P = 0.167) (Table 3). During the ganglionic blockade, the difference in HFRRI values was significant between Black and White women (2 ± 0.45 vs. 24 ± 19.01 ms2, respectively P = 0.029), while LFRRI in Black and White women decreased to similar values (7 ± 3.50 vs. 30 ± 25.07 ms2, respectively, P = 0.662). The result shows a significant difference in HFRRI HR variability in both groups. The ratio between low- and high-frequency HR variability (LFRRI/HFRRI) was higher in Black women than in White women during the ganglionic blockade (4 ± 7.91 vs. 1 ± 1.32, respectively, P = 0.446).
There was no significant difference in the change in the values of the blood pressure variability parameters when compared at baseline and after autonomic blockade between the groups. LFSBP values at baseline were not significantly different between Black and White women (mean ± SEM, 10 ± 1.94 vs. 8 ± 2.04 mm Hg2, respectively, P = 0.541) (Table 3). LFSBP values decreased after the ganglionic blockade to the same values in both groups (3 ± 1.51 vs. 1 ± 0.29 mm Hg2; P = 0.867). There was no difference in BRS between Black and White women at baseline (9 ± 0.94 vs. 8 ± 2.21 ms/mmHg, P = 0.236). After the autonomic blockade, the baroreflex function decreased in both groups to the same levels (1 ± 0.42 vs. 3 ± 1.23 ms/mm Hg, P = 0.081).
During autonomic blockade, the standard deviation heart rate variability (SDRRI) showed no significant difference in the decrease between Black and White women during blockade (mean ± SEM, 9 ± 02.70 vs. 13 ± 03.28 ms2, respectively, P = 0.424) (Table 3). There were no significant differences in the square root of mean squared successive differences (RMSSD) between the groups during blockade (3 ± 0.53 vs. 6 ± 02.10 ms, P = 0.206). Baroreflex function declined during TMT infusion from baseline values in both Black and White women (9 ± 0.93 to 1 ± 0.42 ms/mmHg [Black women], P = 0.001; 8 ± 2.21 to 3 ± 01.23 ms/mm Hg [White women], P = 0.011).
During the ganglionic blockade, the HFRRI and LFRRI HR variability significantly decreased in both groups. The values at baseline and during autonomic blockade values were also compared in each group. In Black women, high- and low-frequency HR variability significantly decreased during the ganglionic blockade compared to baseline values (745 ± 215.90 to 2 ± 0.45 ms2, P = 0.001; 915 ± 273.80 to 7 ± 3.56 ms2, P = 0.001). In White women, HFRRI and LFRRI HR variability significantly decreased during the ganglionic blockade compared to baseline values (845 ± 655.9 to 24 ± 19.02 ms2, P = 0.001; 792 ± 493.90 to 30 ± 25.07 ms2, P = 0.001).
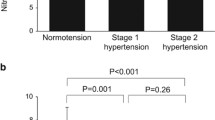
Effect of the L-NMMA on SBP, DBP, and HR of black women compared to white
In each group, the L-NMMA infusion at 250 μg/kg per minute increased SBP and DBP, with the increase significantly greater in Black women than in White women (54 ± 13.62 vs. 39 ± 09.64 mmHg, P = 0.022; 33 ± 03.39 vs. 27 ± 05.30 mmHg, P = 0.016; Fig. 3a, b, respectively). There was no significant change in HR in Black women compared to White women (− 4 ± 2.39 vs. − 3 ± 2.14 bpm, P = 0.469; Fig. 3c).
Effect of L-NMMA on blood pressure and heart rate in the absence of a functional autonomic nervous system in Black and White women, respectively. a Delta values of SBP after infusion of L-NMMA and changes in SBP induced by NOS inhibition. b Delta values of DBP after L-NMMA infusion and resulting changes in DBP. c Delta values of heart rate after L-NMMA infusion and changes in heart rate induced by NOS inhibition. Data are presented as mean ± standard error of the mean. Statistical analysis was performed using Welch’s Correction test. N = 10 for Black women and N = 9 for White women. P < 0.05 was set for statistical significance. DBP Diastolic blood pressure, L-NMMA NG-monomethyl-L-arginine, NOS SBP systolic blood pressure
Discussion
Our main finding was that during NO synthase inhibition in the context of autonomic blockade, the pressor response was more remarkable in Black women than in White women, indicating that endogenous endothelial derived NO significantly contributes to blood pressure modulation to a greater extent in Black women compared with White women.
A previous study [39], using intravenous infusion of L-NMMA doses ranging from 200 to 800 μg/kg per minute, found only a mild increase in blood pressure in healthy volunteers. The authors also reported a mild HR decrease, indicating active baroreflex buffering. To overcome this limitation, our group previously reported that the combined use of L-NMMA and TMT, a ganglionic blocker, helped to measure NO modulation of blood pressure without the confounding effect of baroreflex buffering. Subjects that participated in this study had a moderate increase in SBP with lower doses of L-NMMA [32]. Using this technique, we are currently reporting a similar increase in SBP in White women but a two-fold increase in blood pressure in Black women. Hence, this latter population depends on their endogenous eNO to maintain their blood pressure within normal limits.
Racial differences in NO-induced vasodilation in response to mental stress have been previously studied. Forearm blood flow measurements during intra-arterial infusion of L-NMMA and mental stress were suppressed in Black subjects but not in White subjects [29]. A similar study found attenuated NO-induced vasodilation in Black subjects during resting conditions [40]. Importantly, these studies evaluated NO-induced vasodilation in the microcirculation, which could play a role in the development of future hypertension in these healthy subjects; however, they do not directly measure the tonic contribution of NO to systemic hemodynamics.
In our study, both groups showed a similar decrease in blood pressure during TMT infusion, indicating that sympathetic vasoconstriction activity was equal between groups, as we previously reported in the literature [33]. Importantly, we found a robust increase in HR in Black women during TMT infusion compared with White women, which could indicate an increased sympathetic and cardiovagal regulation of HR. We argue that this difference in HR may not affect blood pressure directly, given that systemic hemodynamic values such as CO, SVR, and SV did not change with TMT.
While our study focused on the acute effects of NO synthase inhibition and autonomic blockade on blood pressure regulation in Black and White obese women, we did not assess for other mechanisms, such as the renin–angiotensin–aldosterone system (RAAS), that may contribute to the differences observed in blood pressure [41]. It is well-documented that Black individuals have higher plasma renin activity than White individuals. This could be, in part, due to the higher prevalence of salt sensitivity. Previous studies demonstrated that salt sensitivity is an independent risk factor for mortality and morbidity due to cardiovascular disease [42,43,44]. Our protocol partially controlled sodium intake by providing subjects with a salt-balanced diet for 3 days before the study day.
Another important consideration is the possibility of differential effects of TMT on the arterial (high-pressure) and venous (low-pressure) systems between Black and White individuals. While our study primarily focused on systemic hemodynamics, including blood pressure and HR, variations in the response of the venous system to autonomic manipulation could impact cardiovascular outcomes differently in different racial groups. Unleashed reflexes of the venous system, such as Bainbridge-like reflexes, triggered by blocking the dominant arterial baroreflexes, may lead to tachycardia as a compensatory response to increased venous return. These reflexes could potentially vary in sensitivity or magnitude between Black and White individuals, thereby influencing overall cardiovascular responses [45].
In conclusion, using a validated approach to determine the contribution of eNO on blood pressure by measuring the effect of systemic NOS inhibition during autonomic blockade, we found that eNO was the most important blood pressure modulator in Black obese women.
Limitations
Our study had several limitations. First our sample size was small; however, we performed in-depth phenotyping of study participants using pharmacological probes that acutely block sympathetic, parasympathetic, and NO function, which controls for differences in these parameters among groups. The other limitation was the use of phenylephrine to restore the blood pressure to baseline level during TMT infusion and before the infusion of L-NMMA. It could be possible that the excessive increase in SBP in Black women was secondary to hypersensitivity to alpha-1 receptors. However, we used the same doses of phenylephrine in both groups to restore the SBP to baseline values, and the increase in SBP with phenylephrine bolus (data not shown) was similar in our Black and White subjects. Further, we enrolled obese women and, therefore, our findings may not extend to the larger population of obese women with cardiometabolic conditions or men.
Additionally, it is important to acknowledge the potential dominance of venous constriction effects of phenylephrine in our experimental protocol. Phenylephrine, an alpha-1 adrenergic agonist used to restore blood pressure to baseline levels during TMT infusion, primarily acts by constricting both arterial and venous vessels. In turn, low-dose alpha-activating drugs like phenylephrine may exert a more pronounced effect on venous constriction and venous return, which could have influenced our observed cardiovascular responses differently in Black and White women. This differential response to phenylephrine administration could potentially confound interpretations of autonomic function and blood pressure regulation [46].
By addressing these limitations, future research can further elucidate the complex interplay between autonomic regulation, vascular physiology, and racial disparities in cardiovascular health.
Abbreviations
- BRS:
-
Baroreflex sensitivity
- DBP:
-
Diastolic blood pressure
- EDHF:
-
Endothelium-derived hyperpolarization factor
- eNO:
-
Endothelial-derived nitric oxide
- eNOS:
-
Endothelial nitric oxide synthase
- HR:
-
Heart rate
- HFRRI :
-
High-frequency variability of HR
- LFRRI :
-
Low-frequency variability of HR
- LFSBP :
-
Low-frequency variability of SBP
- L-NMMA:
-
NG-monomethyl-l-arginine
- NO:
-
Nitric oxide
- RMSSD:
-
Root mean square of successive differences in R-R intervals
- SBP:
-
Systolic blood pressure
- SDRRI :
-
Standard deviation of R-R intervals
- TMT:
-
Trimethaphan
References
Sullivan PW, Morrato EH, Ghushchyan V et al (2005) Obesity, inactivity, and the prevalence of diabetes and diabetes-related cardiovascular comorbidities in the U.S., 2000–2002. Diabetes Care 28:1599–1603. https://doi.org/10.2337/diacare.28.7.1599
Ford ES, Giles WH, Mokdad AH (2004) Increasing prevalence of the metabolic syndrome among U.S. adults. Diabetes Care 27:2444–2449. https://doi.org/10.2337/diacare.27.10.2444
Saleem M (2023) Obesity is associated with increased F2-isoprostanes and IL-6 in black women. Endocrines 4(1):38–54
Choi YS, Klaric JS, Beltran TH (2019) Prediction of insulin resistance with anthropometric and clinical laboratory measures in nondiabetic teenagers. Metab Syndr Relat Disord 17:37–45. https://doi.org/10.1089/met.2018.0072
Reusser ME, DiRienzo DB, Miller GD, McCarron DA (2003) Adequate nutrient intake can reduce cardiovascular disease risk in African Americans. J Natl Med Assoc 95:188–195
Williams RA, Gavin JR, Phillips RA et al (2006) High-risk African Americans with multiple risk factors for cardiovascular disease: challenges in prevention, diagnosis, and treatment. Ethn Dis 16:633–639
Roger VL, Go AS, Lloyd-Jones DM et al (2011) Heart disease and stroke statistics–2011 update: a report from the American Heart Association. Circulation 123:e18–e209. https://doi.org/10.1161/CIR.0b013e3182009701
Jones DW, Chambless LE, Folsom AR et al (2002) Risk factors for coronary heart disease in African Americans: the atherosclerosis risk in communities study, 1987–1997. Arch Intern Med 162:2565–2571. https://doi.org/10.1001/archinte.162.22.2565
Grassi G, Seravalle G, Colombo M et al (1998) Body weight reduction, sympathetic nerve traffic, and arterial baroreflex in obese normotensive humans. Circulation 97:2037–2042. https://doi.org/10.1161/01.cir.97.20.2037
Grassi G, Seravalle G, Cattaneo BM et al (1995) Sympathetic activation in obese normotensive subjects. Hypertension 25:560–563. https://doi.org/10.1161/01.hyp.25.4.560
Alvarez GE, Beske SD, Ballard TP, Davy KP (2002) Sympathetic neural activation in visceral obesity. Circulation 106:2533–2536. https://doi.org/10.1161/01.cir.0000041244.79165.25
Pierini D, Bryan NS (2015) Nitric oxide availability as a marker of oxidative stress. Methods Mol Biol 1208:63–71. https://doi.org/10.1007/978-1-4939-1441-8_5
Cyr AR, Huckaby LV, Shiva SS, Zuckerbraun BS (2020) Nitric oxide and endothelial dysfunction. Crit Care Clin 36:307–321. https://doi.org/10.1016/j.ccc.2019.12.009
Tenopoulou M, Doulias P-T (2020) Endothelial nitric oxide synthase-derived nitric oxide in the regulation of metabolism. F1000Res 9:1000. https://doi.org/10.12688/f1000research.19998.1
Goshi E, Zhou G, He Q (2019) Nitric oxide detection methods in vitro and in vivo. Med Gas Res 9:192–207. https://doi.org/10.4103/2045-9912.273957
Ozkor MA, Murrow JR, Rahman AM et al (2011) Endothelium-derived hyperpolarizing factor determines resting and stimulated forearm vasodilator tone in health and in disease. Circulation 123:2244–2253. https://doi.org/10.1161/CIRCULATIONAHA.110.990317
Mullen MJ, Kharbanda RK, Cross J et al (2001) Heterogenous nature of flow-mediated dilatation in human conduit arteries in vivo: relevance to endothelial dysfunction in hypercholesterolemia. Circ Res 88:145–151. https://doi.org/10.1161/01.res.88.2.145
Joannides R, Richard V, Haefeli WE et al (1995) Role of basal and stimulated release of nitric oxide in the regulation of radial artery caliber in humans. Hypertension 26:327–331. https://doi.org/10.1161/01.hyp.26.2.327
Quyyumi AA, Dakak N, Andrews NP et al (1995) Contribution of nitric oxide to metabolic coronary vasodilation in the human heart. Circulation 92:320–326. https://doi.org/10.1161/01.cir.92.3.320
Gilligan DM, Panza JA, Kilcoyne CM et al (1994) Contribution of endothelium-derived nitric oxide to exercise-induced vasodilation. Circulation 90:2853–2858. https://doi.org/10.1161/01.cir.90.6.2853
Panza JA, Casino PR, Kilcoyne CM, Quyyumi AA (1993) Role of endothelium-derived nitric oxide in the abnormal endothelium-dependent vascular relaxation of patients with essential hypertension. Circulation 87:1468–1474. https://doi.org/10.1161/01.cir.87.5.1468
Rosenbaum DA, Pretorius M, Gainer JV et al (2002) Ethnicity affects vasodilation, but not endothelial tissue plasminogen activator release, in response to bradykinin. Arterioscler Thromb Vasc Biol 22:1023–1028. https://doi.org/10.1161/01.atv.0000017704.45007.1d
Jones DS, Andrawis NS, Abernethy DR (1999) Impaired endothelial-dependent forearm vascular relaxation in black Americans. Clin Pharmacol Ther 65:408–412. https://doi.org/10.1016/S0009-9236(99)70135-9
Kahn DF, Duffy SJ, Tomasian D et al (2002) Effects of black race on forearm resistance vessel function. Hypertension 40:195–201. https://doi.org/10.1161/01.hyp.0000024571.69634.ed
Stein CM, Lang CC, Nelson R et al (1997) Vasodilation in black Americans: attenuated nitric oxide-mediated responses. Clin Pharmacol Ther 62:436–443. https://doi.org/10.1016/S0009-9236(97)90122-3
Stein CM, Lang CC, Singh I et al (2000) Increased vascular adrenergic vasoconstriction and decreased vasodilation in blacks. Additive mechanisms leading to enhanced vascular reactivity. Hypertension 36:945–951. https://doi.org/10.1161/01.hyp.36.6.945
Lang CC, Stein CM, Brown RM et al (1995) Attenuation of isoproterenol-mediated vasodilatation in blacks. N Engl J Med 333:155–160. https://doi.org/10.1056/NEJM199507203330304
Bassett DR, Duey WJ, Walker AJ et al (1992) Racial differences in maximal vasodilatory capacity of forearm resistance vessels in normotensive young adults. Am J Hypertens 5:781–786. https://doi.org/10.1093/ajh/5.11.781
Cardillo C, Kilcoyne CM, Cannon RO, Panza JA (1998) Racial differences in nitric oxide-mediated vasodilator response to mental stress in the forearm circulation. Hypertension 31:1235–1239. https://doi.org/10.1161/01.hyp.31.6.1235
Bond V, Thompson GD, Franks BD et al (1996) Racial differences in minimum lower leg vascular resistance in normotensive young adults with positive and negative parental histories of hypertension. J Cardiovasc Risk 3:423–426. https://doi.org/10.1177/174182679600300502
Hinderliter AL, Sager AR, Sherwood A et al (1996) Ethnic differences in forearm vasodilator capacity. Am J Cardiol 78:208–211. https://doi.org/10.1016/s0002-9149(96)90397-5
Gamboa A, Shibao C, Diedrich A et al (2007) Contribution of endothelial nitric oxide to blood pressure in humans. Hypertension 49:170–177. https://doi.org/10.1161/01.HYP.0000252425.06216.26
Marinos A, Gamboa A, Celedonio JE et al (2017) Hypertension in obese Black women is not caused by increased sympathetic vascular tone. J Am Heart Assoc 6:e006971. https://doi.org/10.1161/JAHA.117.006971
Middlemiss JE, Cocks A, Paapstel K et al (2019) Evaluation of inert gas rebreathing for determination of cardiac output: influence of age, gender and body size. Hypertens Res 42:834–844. https://doi.org/10.1038/s41440-018-0179-1
Diedrich A, Jordan J, Tank J et al (2003) The sympathetic nervous system in hypertension: assessment by blood pressure variability and ganglionic blockade. J Hypertens 21:1677–1686. https://doi.org/10.1097/00004872-200309000-00017
Jordan J, Tank J, Shannon JR et al (2002) Baroreflex buffering and susceptibility to vasoactive drugs. Circulation 105:1459–1464. https://doi.org/10.1161/01.cir.0000012126.56352.fd
Pan J, Tompkins WJ (1985) A real-time QRS detection algorithm. IEEE Trans Biomed Eng 32:230–236. https://doi.org/10.1109/TBME.1985.325532
[No authors listed] (1996) Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 93:1043–1065
Sander M, Chavoshan B, Victor RG (1999) A large blood pressure-raising effect of nitric oxide synthase inhibition in humans. Hypertension 33:937–942. https://doi.org/10.1161/01.hyp.33.4.937
Ozkor MA, Rahman AM, Murrow JR et al (2014) Differences in vascular nitric oxide and endothelium-derived hyperpolarizing factor bioavailability in Blacks and Whites. Arterioscler Thromb Vasc Biol 34:1320–1327. https://doi.org/10.1161/ATVBAHA.113.303136
Kaneko Y, Takeda T, Ikeda T et al (1970) Effect of ganglion-blocking agents on renin release in hypertensive patients. Circ Res 27:97–103. https://doi.org/10.1161/01.res.27.1.97
Pitzer A, Elijovich F, Laffer CL et al (2022) DC ENaC-dependent inflammasome activation contributes to salt-sensitive hypertension. Circ Res 131:328–344. https://doi.org/10.1161/CIRCRESAHA.122.320818
Sahinoz M, Elijovich F, Ertuglu LA et al (2021) Salt sensitivity of blood pressure in blacks and women: a role of inflammation, oxidative stress, and epithelial Na+ channel. Antioxid Redox Signal 35:1477–1493. https://doi.org/10.1089/ars.2021.0212
Richardson SI, Freedman BI, Ellison DH, Rodriguez CJ (2013) Salt sensitivity: a review with a focus on non-hispanic blacks and hispanics. J Am Soc Hypertens 7:170–179. https://doi.org/10.1016/j.jash.2013.01.003
Crystal GJ, Salem MR (2012) The Bainbridge and the “reverse” Bainbridge reflexes: history, physiology, and clinical relevance. Anesth Analg 114:520–532. https://doi.org/10.1213/ANE.0b013e3182312e21
Gelman S (2024) Norepinephrine produces two different haemodynamic effects depending on the dose used. Eur J Anaesthesiol 41:157–160. https://doi.org/10.1097/EJA.0000000000001941
Funding
CAS was supported in part by the National Heart, Lung, and Blood Institute (NHLBI) of the National Institute of Health (NIH) grants R01HL157584 and R01HL159203 and by a grant from the American Heart Association (967054). AK was supported in part by the NIH grant R01HL144941. IB was supported in part by the NIH grant R01HL149386. AD was supported in part by the NIH grant R01HL142583. MS was supported in part by the American Heart Association grant 23CDA1053072. The Vanderbilt Institute for Clinical and Translational Research (VICTR) is funded by the National Center for Advancing Translational Sciences (NCATS), Clinical Translational Science Award (CTSA) Program, Award Number 5UL1TR002243-03. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
Sharla Rahman contributed to the performed literature search, data analysis, manuscript preparation, and editing. Mohammad Saleem contributed to the data analysis. André Diedrich and Surat Kulapatana contributed to the spectral analysis. Annet Kirabo and Cyndya A. Shibao contributed to the review, editing, and approval of the final draft of the manuscript. Cyndya A. Shibao, Alfredo Gamboa, André Diedrich, and Italo Biaggioni contributed to the study planning, data extraction, and completion of the study.
Corresponding authors
Ethics declarations
Conflict of interest
CAS is a consultant for Antag Therapeutics, Theravance Biopharma, and Argenx. AK is a consultant for Argenx. All other authors (SR, AG, MS, SK, AD, IB) have nothing to declare. The author(s) declare that they have no conflict of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rahman, S., Gamboa, A., Saleem, M. et al. Complete autonomic blockade reveals nitric oxide contribution to blood pressure regulation in obese Black women. Clin Auton Res 34, 427–436 (2024). https://doi.org/10.1007/s10286-024-01050-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-024-01050-3