Abstract
Purpose
This systematic review aimed to evaluate the effect of transcutaneous auricular vagus nerve stimulation on heart rate variability and baroreflex sensitivity in healthy populations.
Method
PubMed, Scopus, the Cochrane Library, Embase, and Web of Science were systematically searched for controlled trials that examined the effects of transcutaneous auricular vagus nerve stimulation on heart rate variability parameters and baroreflex sensitivity in apparently healthy individuals. Two independent researchers screened the search results, extracted the data, and evaluated the quality of the included studies.
Results
From 2458 screened studies, 21 were included. Compared with baseline measures or the comparison group, significant changes in the standard deviation of NN intervals, the root mean square of successive RR intervals, the proportion of consecutive RR intervals that differ by more than 50 ms, high-frequency power, low-frequency to high-frequency ratio, and low-frequency power were found in 86%, 75%, 69%, 47%, 36%, and 25% of the studies evaluating the effects of transcutaneous auricular vagus nerve stimulation on these indices, respectively. Baroreflex sensitivity was evaluated in six studies, of which a significant change was detected in only one. Some studies have shown that the worse the basic autonomic function, the better the response to transcutaneous auricular vagus nerve stimulation.
Conclusion
The results were mixed, which may be mainly attributable to the heterogeneity of the study designs and stimulation delivery dosages. Thus, future studies with comparable designs are required to determine the optimal stimulation parameters and clarify the significance of autonomic indices as a reliable marker of neuromodulation responsiveness.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite significant breakthroughs in preventive and therapeutic strategies, cardiovascular disease (CVD) continues to be the leading cause of morbidity and mortality worldwide [1, 2]. Prior to a cardiovascular event, risk factors appear in apparently healthy subjects, at which point preventive actions can be effective [3]. The autonomic nervous system (ANS) is responsible for controlling visceral functions to keep up with environmental stimuli and maintain homeostasis. Imbalance in ANS, when persists, is known as a preceding factor for many disorders [4,5,6]. This is also true for CVDs as many studies have shown the association between an imbalance in cardiovascular ANS function and developing hypertension, heart failure, arrhythmias, and acute myocardial infarction [7,8,9,10]. Therefore, regulating cardiovascular autonomic function in apparently healthy subjects seems to be a promising strategy for preventing future CVDs.
Cardiovascular ANS can be modulated by pharmacological and nonpharmacological methods. In recent years, nonpharmacologic approaches to treat CVDs draw more interest because of the limited efficacy, fewer adverse side effects, and the significant costs of pharmacological agents [8, 10, 11]. Nonpharmacological methods are comprised of invasive and noninvasive therapies. Invasive techniques consist of low-level vagus nerve stimulation (VNS) [12], low-level baroreceptor activation therapy [13], spinal cord stimulation [14], ganglionated plexi ablation [15], renal sympathetic denervation [16], and cardiac sympathetic nerve denervation [17]. Noninvasive approaches generally use electrical pulses, electromagnetic field, ultrasound energy, and optogenetics to transcutaneously target cardiovascular ANS [10, 18].
As a safe and noninvasive method to regulate cardiovascular ANS, transcutaneous auricular VNS (ta-VNS) has attracted much attention in recent years. Many clinical trials speculated the effects of ta-VNS on cardiovascular ANS indices in apparently healthy populations [8, 9, 19,20,21]. However, the results are mixed, and there are still many uncertainties on how ta-VNS can effectively modulate the autonomic function and which individuals might benefit the most from this intervention. In this systematic review, we aim to summarize the current evidence of the effect of ta-VNS on two of the most commonly used indicators of cardiovascular autonomic function, heart rate variability (HRV) and baroreflex sensitivity (BRS) in apparently healthy subjects. We also discuss the individual specific determinants of response to ta-VNS and the challenges associated with selecting the optimal stimulation dosage in these subjects.
Methods
This study was undertaken and reported in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standards [22]. The study protocol has been registered in PROSPERO (CRD42022334252).
Search strategy and eligibility criteria
We performed a systematic search in PubMed, Scopus, Web of Science, the Cochrane Library, and Embase databases from inception to February 2023. The search strategy included combinations of keywords related to or describing VNS and cardiac autonomic function indices including HRV and BRS. The details of search strategy are presented in Supplementary Table 1. In addition, reference lists of retrieved studies were searched for additional relevant reports. The search was limited to published English-language studies. Original studies were included in this review if they met the following criteria: (1) Studies included apparently healthy adults; (2) the intervention group received ta-VNS on tragus or concha areas; (3) the comparison group received “no treatment,” “stimulation OFF” on either the tragus or concha, or “stimulation ON” on areas presumed to have no vagal innervation, such as the earlobe and helix; (4) studies whose primary or secondary outcomes were an endpoint measure of HRV or BRS; and (5) double-arm, controlled clinical trials with a parallel or crossover design. Exclusion criteria were: (1) Observational, single-arm noncontrolled interventional studies, case reports, case series, letters, conference paper, and review articles; (2) studies included nonhealthy population.
Study selection and data extraction
The study selection and data extraction were carried out independently by two investigators, with a third being consulted in case of discrepancies. First, titles and abstracts of the selected studies were screened according to eligibility criteria, and then, the full texts of those primarily considered relevant were evaluated in detail. Data on study design, sample size, gender distribution, age, and intervention characteristics in active and sham groups, including stimulation technical parameters, duration of exposure, site of stimulation, and outcome measures were extracted from final included studies.
Quality assessment
Two independent researchers assessed the quality of included studies using two different tools, based on the design of the studies: Cochrane Risk of Bias Tool version 2.0 (RoB 2.0) for crossover trials [23] and Cochrane RoB 2.0 for parallel trials [24]. Cochrane RoB 2.0 for crossover studies consists of six domains that assess bias in various methodological steps of studies, such as randomization process, washout period and carryover effects, deviations from the intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result [23]. Cochrane RoB 2.0 for parallel trials is identical to that for crossover studies, with the exception that this tool lacks a domain for evaluating washout period and carryover effects [24]. Cochrane RoB 2.0 classifies studies as follows, based on their overall quality: (1) low risk of bias, which includes studies rated low risk in all domains; (2) some concerns, which includes studies rated of some concern in at least one domain but no high-risk judgement; and (3) high risk of bias, which includes studies rated high risk in at least one domain or have some concerns for multiple domains in a way that significantly reduces confidence in the results [23, 24].
Data synthesis and visualization
We deemed it inappropriate to perform a meta-analysis of study results due to heterogeneity in study design, stimulation delivery protocols, and outcome reporting across studies. Instead, we provided a detailed narrative synthesis of findings in the main text and structured tables, as well as several 3D scatter plots illustrating the distribution of ta-VNS stimulation parameters used in included studies and the effect size of ta-VNS on various HRV indices and BRS in individual studies.
The mean and standard deviation (SD) of HRV indices and BRS measured at three time points—baseline, during stimulation, and recovery—were extracted for the sham and active groups. In the case of reporting other than SD, including standard error (SE) and confidence intervals (CI), they were converted to SD using standard formulas [25]. Due to differences in outcome measures among the included studies, we estimated the effect size of the included studies by calculating the standardized mean difference (SMD) and 95% confidence interval for each within-group and between-group comparison, wherever possible based on the available data. If not, we described the direct findings from the study. An SMD (Cohen’s d) < 0.5 is generally interpreted as a small effect size, 0.5–0.8 as a moderate effect size, and > 0.8 as a large effect size.
Results
Identification and selection of the studies
Figure 1 depicts the study selection process. A total of 2458 papers were retrieved from five databases. After eliminating duplicates and irrelevant research by title and abstract screening, 40 studies were examined for full-text screening. At this step, 19 studies were discarded based on the exclusion criteria, leaving 21 relevant controlled trials for inclusion in this systematic review.
Study characteristics
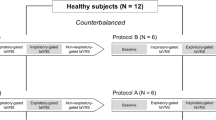
The characteristics of the included studies are summarized in Table 1. Except for four studies that focused only on men [8, 26,27,28], the majority of studies included participants of both sexes. The age ranges of the participants included in studies were as follows: young adults (18–39 years) in 17 studies [8, 9, 19, 21, 26,27,28,29,30,31,32,33,34,35,36,37,38], middle-aged adults (40–59 years) in four studies [34, 39,40,41], and older adults (≥ 60 years) in one study [42]. All studies evaluated the efficacy of ta-VNS, administered either to the tragus [8, 9, 27, 32, 37, 42], cymba concha [21, 26, 28,29,30,31, 34,35,36, 38,39,40,41], or both [19, 33] on HRV parameters [8, 9, 19, 21, 26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41] and/or BRS [8, 27, 34, 40,41,42]. As shown in Figs. 3, 4, 5, 6, 7, 8, and 9, the most used frequency in included studies was 25 Hz in 12 studies [19, 21, 28,29,30,31, 33, 35,36,37,38, 40] followed by 10 Hz in four studies [34, 35, 39, 41], and 20 Hz [26, 27, 32] and 30 Hz [8, 9, 42] each in three studies. The frequencies used in four experiments—2 [35], 5 [26], 100 [35], and 500 Hz [36]—were vastly different from those in other studies. Except for one study that employed a set stimulation of 2 mA [33], the majority of experiments relied on the sensory thresholds of the participants to determine the stimulation intensity. This has been determined using one of two methods: up-titration, which begins at a very low amplitude and gradually rises to the sensory threshold (13 studies) [9, 19, 26, 28, 29, 31, 32, 34, 36, 37, 39,40,41] or down-titration, in which the pain threshold is first detected and then the amplitude is set just below that at the sensory level (two studies) [30, 42]. In addition, the specific procedure for selecting the stimulation intensity was not described in four of the trials [8, 27, 35, 38]. As shown in Figs. 3, 4, 5, 6, 7, 8, and 9, the most frequently employed pulse width in the included studies was 250 µs (five studies) [19, 29, 30, 32, 40], followed by 200 µs [8, 9, 26, 42] and 300 µs [34, 35, 39, 41] each in four studies, 500 µs in two studies [36, 38], and 100 µs [33] and 1000 µs [27] in one study each. Instead of utilizing a fixed number, two investigations reported the pulse width as a range between 200 and 300 µs [21, 31]. Only eight investigations detailed the waveform of the electrical pulses: four used rectangular pulses [27, 29, 35, 36], three of which were monophasic [27, 35, 36]; two used square pulses, one of which was monophasic [30] and the other biphasic [40]; one used a combination of rectangular and square pulses [33]; and one simply stated “biphasic” to describe the waveform [31]. Fifteen trials utilized a continuous stimulation pattern [8, 9, 19, 26, 27, 32, 34,35,36,37, 39,40,41,42] while six studies used an on–off cycle stimulation pattern [21, 28,29,30,31, 38]. As shown in Fig. 2, the following sham or comparison strategies were employed in the included studies: (1) “stimulation ON” on the earlobe (nine trials) [8, 19, 21, 26, 28, 30, 32, 37, 40], (2) “stimulation ON” on the helix (one study) [31], (3) “stimulation OFF” on the tragus (four trials) [8, 27, 33, 42], (4) “stimulation OFF” on the concha (five studies) [29, 33,34,35,36], and (5) “stimulation ON” on the nonauricular region (arm) (one study) [38]. Two studies compared the active groups with “no treatment” groups [39, 41].
ta-VNS and cardiac autonomic nervous system indices
This section evaluates the influence of ta-VNS on HRV frequency-domain (LF, HF, and LF/HF ratio) and time-domain (RMSSD, SDNN, PNN50) parameters, as well as BRS, in the included studies.
Heart rate variability frequency-domain parameters
The effect of ta-VNS on LF-HRV was assessed in a total of 17 experiments from 12 studies including 323 healthy subjects [8, 9, 26, 29, 31,32,33,34, 36, 38, 40, 41]. The majority of studies found no substantial change in LF-HRV with ta-VNS compared with the sham group or baseline levels. Forte et al. [31] observed a substantial increase in LF during ta-VNS compared with baseline levels. Shen et al. [36] identified responders to ta-VNS based on a 20% decrease in the LF/HF ratio; in this group of subjects, there was a substantial decrease in LF during burst stimulation relative to the baseline level. Only Zhu et al. [38] observed a significant decrease in LF-HRV during ta-VNS compared with the sham group.
HF-HRV has been assessed in 21 experiments from 15 studies involving 441 healthy volunteers [8, 9, 19, 26, 29, 31,32,33,34,35,36,37,38, 40, 41]. The results of eight studies did not demonstrate a statistically significant change with ta-VNS when compared with sham or baseline levels [8, 9, 26, 29, 34, 35, 37, 40]. Three studies have revealed a significant rise in HF-HRV during ta-VNS compared with the sham group [31, 32, 38]. In addition, Keute et al. [33] and Forte et al. [31] and Borges et al. [19] reported a significant increase in HF-HRV during stimulation relative to baseline levels. Furthermore, Borges et al. [19] and Kania et al. [41] showed a significant increase in HF during recovery relative to baseline levels. Similarly, Shen et al. [36] observed a significant increase in this parameter among responders to both stimulation patterns (burst and continuous) during stimulation and recovery relative to baseline levels.
Nineteen experiments from 15 studies assessed the influence of ta-VNS on the LF/HF ratio in 380 healthy participants [8, 9, 26,27,28,29, 31,32,33,34, 36,37,38, 40]. Seven studies did not find a substantial difference between the ta-VNS group and the sham or baseline levels [27,28,29, 32, 33, 37, 40]. Compared with baseline values, Antonino et al. [8] and Clancy et al. [9] observed a substantial decrease in the LF/HF ratio during ta-VNS; Shen et al. [36] observed a significant decrease in this parameter during stimulation in responders to burst ta-VNS; and Gauthey et al. [26] observed a significant increase in the LF/HF ratio during ta-VNS with a frequency of 5 Hz. compared with the sham group. Only Zhu et al.[38] detected a substantial reduction in the LF/HF ratio during stimulation. In addition, two investigations found a substantial rise in the LF/HF ratio in the sham group compared with the baseline values [31, 34].
Heart rate variability time-domain parameters
Eighteen experiments from 13 studies involving 450 healthy adults assessed the effect of ta-VNS on RMSSD [19, 21, 26, 28,29,30,31,32,33,34, 36, 39, 41]. The results of four trials did not indicate a significant change in the ta-VNS group compared with sham or baseline levels [26, 28, 29, 34]. Three studies demonstrated a statistically significant rise in RMSSD during ta-VNS versus the sham group [31, 32, 36]. In three investigations [30, 39, 41], although there was no significant difference between the active and sham groups, there was a substantial rise in RMSSD during recovery relative to baseline values. In addition, Borges et al. [21] separated the stimulation session into first and second halves and compared them with sham and baseline levels; although, there was no significant difference between the active and sham groups, a significant increase was identified in the second half of the stimulation compared with baseline. In another study, Borges et al. [19] also found a significant increase in RMSSD during stimulation and recovery compared with baseline levels. In addition, Shen et al. [36] showed a substantial rise in RMSSD during stimulation with both patterns relative to baseline; moreover, a significant increase in this parameter was found during recovery in the burst stimulation responders relative to baseline.
The effects of ta-VNS on SDNN have been investigated in 11 experiments from 7 studies including 212 healthy participants [26, 29, 31,32,33,34, 36]. Gauthey et al. [26] found no significant change in SDNN in the active group compared with the sham group or baseline values. Two studies detected a significant increase in SDNN in during stimulation compared with the sham group [31, 32]. Also, De Couck et al. [29] and Keute et al. [33] did not identify a significant difference between the ta-VNS group and the sham group, but they did note a substantial rise in SDNN during stimulation relative to their baseline levels. In addition, Shen et al. [36] observed a significant increase in SDNN during recovery compared with baseline values for both stimulation patterns, as well as a significant increase during stimulation among responders to both stimulation patterns. Kozorosky et al. [34] found no significant difference between the active group and the sham group or baseline values in any of their experiments; however, the sham group in their first experiment demonstrated a substantial rise in SDNN from baseline.
The effect of ta-VNS on PNN50 has been evaluated in six experiments from four studies [32,33,34, 36].The results of the experiments conducted by Geng et al.[32], Shen et al. [36], and Keute et al. [33] demonstrated a substantial rise in this parameter during ta-VNS stimulation compared with the sham group. Kozorosky et al. [34] did not observe any significant change in PNN50 in the ta-VNS group compared with the sham group or baseline values.
Baroreflex sensitivity
Eight experiments from six studies [8, 27, 34, 40,41,42] including a total of 97 healthy subjects, investigated the effect of ta-VNS on BRS. Only Bretherton et al. [42] detected a significant rise in BRS during ta-VNS stimulation compared with the sham group. Antonino et al. [8] found no statistically significant difference between the active and sham groups, however, a significant rise in BRS during ta-VNS stimulation relative to baseline values was observed.
Quality assessment and publication bias
The results of the quality assessment are shown in Supplementary Fig. 1A and B. As previously stated, a total of 17 crossover trials and 4 parallel trials were included in this study. For crossover trials, the risk of bias assessment using Cochrane RoB 2.0 revealed that all of the included studies have some concerns in at least one domain, mainly in those related to the lack of a prespecified analysis plan (14 studies), insufficient washout duration and carryover effect (six studies), and inappropriate randomization process (five studies). Therefore, none of these crossover studies had a low risk of bias, and four of them have been determined to have a high risk. Cochrane RoB 2.0 for parallel randomized controlled trials was utilized to evaluate the four trials conducted using this design. The lack of a prespecified analysis plan was a concern for all of these trials, and two of them also had concerns with randomization.
Discussion
The purpose of this systematic review was to determine whether ta-VNS might significantly influence HRV parameters and BRS, and serve as a preventative strategy to enhance overall health in apparently healthy individuals. ANS imbalance, as revealed by HRV and BRS disturbances, is not only a potent and independent predictor of poor prognosis in patients with CVDs [43,44,45,46], but also a risk factor for death in healthy subjects [47, 48]. The potential of ta-VNS to improve autonomic function in a healthy population is substantial, and it might be used by many individuals where the cardiovascular autonomic balance is changed toward sympathetic predominance [49, 50].
Discussion on main findings
The results generally indicate conflicting conclusions about the effectiveness of ta-VNS on HRV or BRS. As stated previously and illustrated in the graphical abstract, 25%, 47%, and 36% of the studies evaluating LF, HF, and LF/HF, respectively, observed a significant effect of ta-VNS in changing these indices compared with the sham group, the pre-stimulation baseline levels, or both. Regarding time-domain indices, ta-VNS in 69%, 86%, and 75% of the studies has caused a significant change in RMSSD, SDNN, and PNN50, respectively, compared with pre-stimulation baseline levels or comparison groups. Some studies continued the measurement of vagally-mediated indices such as HF, SDNN, and RMSSD in a short period after the cessation of stimulation, and have shown that the level of these indices remains higher than the baseline level during the recovery period [19, 32, 39]. This implies a “carry-over” effect, which is corroborated by earlier research showing greater HF power compared with baseline for at least 1 hour after ceasing auricular VNS with acupuncture (66). Regarding the BRS, only one study (17%) found the benefit of ta-VNS in improving this index compared with the baseline level and comparison group.
LF-HRV power may be generated by both the parasympathetic and sympathetic nervous systems, and slow breathing (i.e., < 8.5 breaths per minute) may influence its measurement [51]. A minimum of 2 min is required for recording LF power [52]. HRV recordings in included studies ranged from 15 to 150 min, which is sufficient for LF analysis, and most studies controlled the respiratory rate of their participants and exclude abnormal respiratory rate from their analysis. The LF/HF ratio is generally considered to be associated with sympathovagal balance, with a high ratio indicating sympathetic dominance and a low ratio indicating parasympathetic dominance [51, 53]. As illustrated in Figs. 3 and 4, exposure to ta-VNS has been associated with a decrease in LF compared with the comparison group in five and nine experiments, but the effect size was only significant in the Zhu et al. study [38] with a near-to-moderate effect size (−0.480) for LF and a moderate effect size for LF/HF (−0.503). The study by Zhu et al. has characteristics that distinguish its design from other studies and that partially explain the significant effect size observed for ta-VNS. This study exposed individuals to cold stress to induce autonomic dysfunction and then investigated the efficacy of ta-VNS on HRV parameters. Some studies have shown that the worse the basic autonomic function, indicated by higher LF/HF, the better the response to ta-VNS [9, 32]. This may partially explain how exposure to ta-VNS led to a higher effect size in the Zhu et al. study, in comparison with other studies that exposed subjects with physiologic baseline autonomic function to intervention. In addition, the study by Zhu et al. was the only one to use bilateral stimulation, which may be more helpful than the unilateral stimulation used in other studies; however, there is no study that compares the two, and this must be investigated in future research. Another difference between the Zhu et al. study and other studies is in their sham groups. The former used arm stimulation as a sham group, which can be superior to a “stimulation OFF” approach on either the tragus or conecha and a “stimulation ON” approach on the earlobe due to proper blinding and a lack of definitive stimulation of the vagus nerve, respectively.
HF, another frequency-domain index, represents parasympathetic activity and could be significantly influenced by respiration [9]. As depicted in Fig. 5, exposure to ta-VNS was associated with an increase in HF compared with the sham group in nine experiments; however, the effect size was only statistically significant in the studies by Geng et al. [32] and Zhu et al. [38], with high (+0.926) and moderate (+0.641) effect sizes, respectively. Despite being adjusted to the same sensory level as other investigations, the mean current intensity in the study by Geng et al. was significantly (up to two to three times) higher than in other studies. According to a recent study, greater ta-VNS intensities may be needed to provide meaningful neuromodulatory effects [54]. Furthermore, while the evidence is conflicting [21], there is some research indicating a positive linear association between ta-VNS intensity and several HRV parameters [55]. This could explain why the Geng et al. study had a considerably larger effect size than other studies evaluating HF-HRV; however, this should be clarified in future studies. Furthermore, the characteristics of the study by Zhu et al. that were described above as possible explanations for the observed substantial impacts on LF and LF/HF indices may also be true for HF.
SDNN is believed to indicate both sympathetic and parasympathetic inputs, whereas RMSSD is supposed to reflect vagally-mediated HRV, and both are less affected by variations in respiratory parameters than frequency-domain indices [43, 56]. Another time-domain HRV parameter is pNN50, which is indicative of parasympathetic nervous system activity and is correlated with HF and RMSSD [56]. As shown in Figs. 6, 7, and 8, Geng et al.’s study [32] found significant increases in all three indices compared with the comparison group, with a high effect size for RMSSD (+1.65), SDNN (+1.924), and pNN50 (+1.842). Above, we described the characteristics of this study, which can be the possible reasons for the higher effect size in this study as compared with other studies.
HRV: a potential biomarkers for ta-VNS responsiveness
HRV is regarded as a noninvasive tool for assessing autonomic function and may be utilized to assess efferent vagus nerve activity [57]. According to the literature, sympathetic overactivity, the inflammatory response, and oxidative stress are three physiological pathways that contribute autonomic function imbalance to the development of many diseases [58, 59]. Moreover, vagally-mediated indices of HRV are inversely linked to the surrogate markers of these pathways [60,61,62]. Therefore, it is essential to systematically examine how ta-VNS affects HRV. This can not only aid us in finding out the impact of this intervention on autonomic function, but also determine whether HRV could be utilized as a predictive biomarker of ta-VNS responsiveness since it can help in selecting the right individuals, stimulation sites, and stimulation dosage to further optimize neuromodulation therapies. Variations in response to ta-VNS in the aforementioned studies could be explained by differences in study design, stimulation dosage, and individual characteristics. Future research using the same design and stimulation protocol will help to clarify the significance of HRV in predicting treatment response. Using this marker as a response evaluation tool in a ta-VNS closed-loop system can show the response to treatment in real time and aid in optimizing patient selection and stimulation dosage. Furthermore, HRV could be compared with other trustworthy indicators of ta-VNS efficiency, such as somatosensory evoked potentials [63] and skin sympathetic nerve activity [64].
Patient-specific baseline determinants of response to ta-VNS
The heterogeneity of results among studies appears to be influenced by variations in patient-specific baseline factors. Evidence shows that baseline HRV could significantly predict response to ta-VNS, where higher resting LF/HF ratio was associated with greater decreases during ta-VNS [9, 42, 65]. This finding implies that the LF/HF ratio can be utilized to screen individuals who are more likely to benefit from ta-VNS in terms of improved autonomic function. This may make it possible to select ideal individuals for ta-VNS, which is especially important because of the wide range of disorders associated with autonomic imbalance. Bretherton et al. [42] evaluated what baseline HRV threshold can predict response to ta-VNS and found that values greater than 1.5 had a better response to therapy. This issue should be more precisely investigated in future investigations. Furthermore, baseline HRV declines with age [66, 67], and because ta-VNS responds better in individuals with lower baseline HRV [9, 42, 65], ta-VNS may be more effective in older adults than in younger individuals. Importantly, there is a U-shaped link between age and various time-domain indices such RMSSD and pNN50, with a decrease in middle-aged adults and an increase in older ages [68]. Moreover, baseline autonomic function differs significantly between men and women; males exhibited higher LF/HF than women, indicating a higher sympathetic tone in men [69]. Future research should explore the influence of gender on the ta-VNS responsiveness rate.
Considerations in selecting stimulation protocol
The inconsistency of the results reported in the literature may also be due to variation in ta-VNS parameters including intensity, frequency, pulse width, stimulation site (tragus, concha, etc.), and side (right, left, or bilateral). Different stimulation intensity in the same nerve tissue have been shown to yield various clinical results [70]. It has been revealed that ta-VNS can produce vagus somatosensory evoked potentials in brain stem nuclei at stimulation levels lower than those that cause pain perception [71]. In addition, peripheral stimulation with a current adjusted below the pain threshold where Aβ fibers are stimulated provides therapeutic effects [72]. The intensity level in the most studies examined in this review was consistently lower than the pain threshold at the level of sensory perception. Future research should determine whether ta-VNS intensity and HRV variations are linearly related. As shown in Figs. 3, 4, 5, 6, 7, 8, and 9, we calculated another parameter, namely total electrical charge, defined by the mean intensity multiplied by the effective stimulation time, for each individual study and found no linear association between this parameter and calculated effect sizes. Another set of stimulation parameters, such as frequency and pulse width, varied between studies; hence, future dose–response studies are required to find the optimal value for these stimulation parameters. HRV and the other predictive biomarkers of response to ta-VNS can assist in identifying the most effective stimulation parameters once their function as surrogates for neuronal engagement following stimulation is precisely determined.
Conclusions
The results of the included studies were mixed, which may be mainly attributable to the heterogeneity of their study design and stimulation delivery dosage. Thus, future studies with comparable designs are required to determine the optimal stimulation parameters and clarify the significance of autonomic indices as a reliable marker of neuromodulation responsiveness. In addition, it has been shown that the worse the basic autonomic function, the better the response to transcutaneous auricular vagus nerve stimulation, suggesting the importance of patient-specific baseline factors in optimizing neuromodulation.
References
Weir HK, Anderson RN, Coleman King SM, Soman A, Thompson TD, Hong Y et al (2016) Heart disease and cancer deaths - trends and projections in the United States, 1969–2020. Prev Chronic Dis 13:E157. https://doi.org/10.5888/pcd13.160211
Xu J, Murphy SL, Kochanek KD, Arias E (2015) Mortality in the United States. NCHS Data Brief 2016(267):1–8
Greenland P, Knoll MD, Stamler J, Neaton JD, Dyer AR, Garside DB et al (2003) Major risk factors as antecedents of fatal and nonfatal coronary heart disease events. Jama 290(7):891–7. https://doi.org/10.1001/jama.290.7.891
Kaniusas E, Kampusch S, Tittgemeyer M, Panetsos F, Gines RF, Papa M et al (2019) Current directions in the auricular vagus nerve stimulation i - a physiological perspective. Front Neurosci 13:854. https://doi.org/10.3389/fnins.2019.00854
Beekwilder JP, Beems T (2010) Overview of the clinical applications of vagus nerve stimulation. J Clin Neurophysiol. 27(2):130–8. https://doi.org/10.1097/WNP.0b013e3181d64d8a
Pellissier S, Dantzer C, Canini F, Mathieu N, Bonaz B (2010) Psychological adjustment and autonomic disturbances in inflammatory bowel diseases and irritable bowel syndrome. Psychoneuroendocrinology. 35(5):653–62. https://doi.org/10.1016/j.psyneuen.2009.10.004
Curtis BM, Oeefe JH Jr (2002) Autonomic tone as a cardiovascular risk factor: the dangers of chronic fight or flight. Mayo Clin Proc 77:45–54
Antonino D, Teixeira AL, Maia-Lopes PM, Souza MC, Sabino-Carvalho JL, Murray AR et al (2017) Non-invasive vagus nerve stimulation acutely improves spontaneous cardiac baroreflex sensitivity in healthy young men: a randomized placebo-controlled trial. Brain Stimul 10(5):875–881. https://doi.org/10.1016/j.brs.2017.05.006
Clancy JA, Mary DA, Witte KK, Greenwood JP, Deuchars SA, Deuchars J (2014) Non-invasive vagus nerve stimulation in healthy humans reduces sympathetic nerve activity. Brain Stimul 7(6):871–877. https://doi.org/10.1016/j.brs.2014.07.031
Chen M, Wang S, Li X, Yu L, Yang H, Liu Q et al (2020) Non-invasive autonomic neuromodulation is opening new landscapes for cardiovascular diseases. Front Physiol 11:550578. https://doi.org/10.3389/fphys.2020.550578
Naftchi NE (1990) Mechanism of autonomic dysreflexia. Contributions of catecholamine and peptide neurotransmitters. Ann N Y Acad Sci. 579:133–48. https://doi.org/10.1111/j.1749-6632.1990.tb48356.x
Chen M, Zhou X, Yu L, Liu Q, Sheng X, Wang Z et al (2016) Low-level vagus nerve stimulation attenuates myocardial ischemic reperfusion injury by antioxidative stress and antiapoptosis reactions in canines. J Cardiovasc Electrophysiol 27(2):224–31. https://doi.org/10.1111/jce.12850
Sheng X, Chen M, Huang B, Liu J, Zhou L, Bao M et al (2016) Cardioprotective effects of low-level carotid baroreceptor stimulation against myocardial ischemia-reperfusion injury in canine model. J Interv Card Electrophysiol 45(2):131–40. https://doi.org/10.1007/s10840-015-0094-1
Lopshire JC, Zipes DP (2014) Spinal cord stimulation for heart failure: preclinical studies to determine optimal stimulation parameters for clinical efficacy. J Cardiovasc Transl Res 7(3):321–9. https://doi.org/10.1007/s12265-014-9547-7
Zipes DP (2017) Ablation of atrial gangionated plexi to treat symptomatic sinus bradycardia. JACC Clin Electrophysiol 3(9):960–961. https://doi.org/10.1016/j.jacep.2017.02.010
Böhm M, Linz D, Urban D, Mahfoud F, Ukena C (2013) Renal sympathetic denervation: applications in hypertension and beyond. Nat Rev Cardiol 10(8):465–76. https://doi.org/10.1038/nrcardio.2013.89
Cha YM, Li X, Yang M, Han J, Wu G, Kapa SC et al (2019) Stellate ganglion block and cardiac sympathetic denervation in patients with inappropriate sinus tachycardia. J Cardiovasc Electrophysiol 30(12):2920–2928. https://doi.org/10.1111/jce.14233
Soltani D, Samimi S, Vasheghani-Farahani A, Shariatpanahi SP, Abdolmaleki P, Madjid Ansari A (2023) Electromagnetic field therapy in cardiovascular diseases: a review of patents, clinically effective devices, and mechanism of therapeutic effects. Trends Cardiovasc Med 33(2):72–78. https://doi.org/10.1016/j.tcm.2021.10.006
Borges U, Pfannenstiel M, Tsukahara J, Laborde S, Klatt S, Raab M (2021) Transcutaneous vagus nerve stimulation via tragus or cymba conchae: are its psychophysiological effects dependent on the stimulation area? Int J Psychophysiol 161:64–75. https://doi.org/10.1016/j.ijpsycho.2021.01.003
De Couck M, Cserjesi R, Caers R, Zijlstra WP, Widjaja D, Wolf N et al (2017) Effects of short and prolonged transcutaneous vagus nerve stimulation on heart rate variability in healthy subjects. Auton Neurosci 203:88–96. https://doi.org/10.1016/j.autneu.2016.11.003
Borges U, Laborde S, Raab M (2019) Influence of transcutaneous vagus nerve stimulation on cardiac vagal activity: Not different from sham stimulation and no effect of stimulation intensity. PLoS One 14(10):e0223848. https://doi.org/10.1371/journal.pone.0223848
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj 372:n71. https://doi.org/10.1136/bmj.n71
Higgins JP, Savović J, Page MJ, Sterne JA (2021) Revised Cochrane risk of bias tool for randomized trials (RoB 2) additional considerations for crossover trials. RoB2 Development Group [Internet]
Sterne J A, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. bmj 366
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ et al (2019) Cochrane handbook for systematic reviews of interventions. John Wiley & Sons
Gauthey A, Morra S, van de Borne P, Deriaz D, Maes N, le Polain JB, de Waroux, (2020) Sympathetic effect of auricular transcutaneous vagus nerve stimulation on healthy subjects: a crossover controlled clinical trial comparing vagally mediated and active control stimulation using microneurography. Front Physiol. https://doi.org/10.3389/fphys.2020.599896
Sinkovec M, Trobec R, Meglic B (2021) Cardiovascular responses to low-level transcutaneous vagus nerve stimulation. Auton Neurosci Basic Clin. https://doi.org/10.1016/j.autneu.2021.102851
Vosseler A, Zhao D, Fritsche L, Lehmann R, Kantartzis K, Small DM et al (2020) No modulation of postprandial metabolism by transcutaneous auricular vagus nerve stimulation: a cross-over study in 15 healthy men. Sci Rep 10(1):20466. https://doi.org/10.1038/s41598-020-77430-2
De Couck M, Cserjesi R, Caers R, Zijlstra WP, Widjaja D, Wolf N et al (2017) Effects of short and prolonged transcutaneous vagus nerve stimulation on heart rate variability in healthy subjects. Auton Neurosci Basic Clin 203:88–96. https://doi.org/10.1016/j.autneu.2016.11.003
De Smet S, Ottaviani C, Verkuil B, Kappen M, Baeken C, Vanderhasselt MA (2023) Effects of non-invasive vagus nerve stimulation on cognitive and autonomic correlates of perseverative cognition. Psychophysiology. https://doi.org/10.1111/psyp.14250
Forte G, Favieri F, Leemhuis E, De Martino ML, Giannini AM, De Gennaro L et al (2022) Ear your heart: transcutaneous auricular vagus nerve stimulation on heart rate variability in healthy young participants. PeerJ 10:e14447. https://doi.org/10.7717/peerj.14447
Geng D, Liu X, Wang Y, Wang J (2022) The effect of transcutaneous auricular vagus nerve stimulation on HRV in healthy young people. PLoS One 17(2):e0263833. https://doi.org/10.1371/journal.pone.0263833
Keute M, Machetanz K, Berelidze L, Guggenberger R, Gharabaghi A (2021) Neuro-cardiac coupling predicts transcutaneous auricular vagus nerve stimulation effects. Brain Stimul 14(2):209–216. https://doi.org/10.1016/j.brs.2021.01.001
Kozorosky EM, Lee CH, Lee JG, Nunez Martinez V, Padayachee LE, Stauss HM (2022) Transcutaneous auricular vagus nerve stimulation augments postprandial inhibition of ghrelin. Physiol Rep. https://doi.org/10.14814/phy2.15253
Sclocco R, Garcia RG, Kettner NW, Fisher HP, Isenburg K, Makarovsky M et al (2020) Stimulus frequency modulates brainstem response to respiratory-gated transcutaneous auricular vagus nerve stimulation. Brain Stimul 13(4):970–978. https://doi.org/10.1016/j.brs.2020.03.011
Shen LL, Sun JB, Yang XJ, Deng H, Qin W, Du MY et al (2022) Reassessment of the effect of transcutaneous auricular vagus nerve stimulation using a novel burst paradigm on cardiac autonomic function in healthy young adults. Neuromodulation 25(3):433–442. https://doi.org/10.1111/ner.13521
Villani V, Tsakiris M, Azevedo R (2019) Transcutaneous vagus nerve stimulation improves interoceptive accuracy. Neuropsychologia 134:107201
Zhu Y, Xu F, Sun C, Xu W, Li M, Gong Y et al (2022) Noninvasive transcutaneous auricular vagal nerve stimulation improves gastric slow waves impaired by cold stress in healthy subjects. Neuromodulation. https://doi.org/10.1016/j.neurom.2022.03.010
Dalgleish AS, Kania AM, Stauss HM, Jelen AZ (2021) Occipitoatlantal decompression and noninvasive vagus nerve stimulation slow conduction velocity through the atrioventricular node in healthy participants. J Osteopath Med 121(4):349–359. https://doi.org/10.1515/jom-2020-0213
Gancheva S, Bierwagen A, Markgraf DF, Bönhof GJ, Murphy KG, Hatziagelaki E et al (2018) Constant hepatic ATP concentrations during prolonged fasting and absence of effects of Cerbomed Nemos® on parasympathetic tone and hepatic energy metabolism. Mol Metab 7:71–79. https://doi.org/10.1016/j.molmet.2017.10.002
Kania AM, Weiler KN, Kurian AP, Opena ML, Orellana JN, Stauss HM (2021) Activation of the cholinergic antiinflammatory reflex by occipitoatlantal decompression and transcutaneous auricular vagus nerve stimulation. J Osteopath Med 121(4):401–415. https://doi.org/10.1515/jom-2020-0071
Bretherton B, Atkinson L, Murray A, Clancy J, Deuchars S, Deuchars J (2019) Effects of transcutaneous vagus nerve stimulation in individuals aged 55 years or above: potential benefits of daily stimulation. Aging (Albany NY) 11(14):4836–4857
Kleiger RE, Miller JP, Bigger JT Jr, Moss AJ (1987) Decreased heart rate variability and its association with increased mortality after acute myocardial infarction. Am J Cardiol 59(4):256–262
Nolan J, Batin PD, Andrews R, Lindsay SJ, Brooksby P, Mullen M et al (1998) Prospective study of heart rate variability and mortality in chronic heart failure: results of the United Kingdom heart failure evaluation and assessment of risk trial (UK-heart). Circulation 98(15):1510–1516
Johansson M, Gao SA, Friberg P, Annerstedt M, Carlström J, Ivarsson T et al (2007) Baroreflex effectiveness index and baroreflex sensitivity predict all-cause mortality and sudden death in hypertensive patients with chronic renal failure. J Hypertens 25(1):163–168
La Rovere MT, Bigger JT, Marcus FI, Mortara A, Schwartz PJ (1998) Baroreflex sensitivity and heart-rate variability in prediction of total cardiac mortality after myocardial infarction. The Lancet 351(9101):478–484
Jouven X, Empana J-P, Schwartz PJ, Desnos M, Courbon D, Ducimetière P (2005) Heart-rate profile during exercise as a predictor of sudden death. N Engl J Med 352(19):1951–1958
Kiviniemi AM, Tulppo MP, Hautala AJ, Perkiömäki JS, Ylitalo A, Kesäniemi YA et al (2014) Prognostic significance of impaired baroreflex sensitivity assessed from Phase IV of the Valsalva maneuver in a population-based sample of middle-aged subjects. Am J Cardiol 114(4):571–576
Mischel NA, Mueller PJ (2011) (In)activity-dependent alterations in resting and reflex control of splanchnic sympathetic nerve activity. J Appl Physiol 111(6):1854–1862
Triposkiadis F, Karayannis G, Giamouzis G, Skoularigis J, Louridas G, Butler J (2009) The sympathetic nervous system in heart failure: physiology, pathophysiology, and clinical implications. J Am Coll Cardiol 54(19):1747–1762
Shaffer FM, Ginsberg JP (2017) An overview of heart rate variability metrics and norms. Front Public Health 5:258
Task Force of the European Society of Cardiology the North A Electrophysiology (1996) Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Circulation 93(5):1043–1065
Shaffer F, McCraty R, Zerr CL (2014) A healthy heart is not a metronome: an integrative review of the heart’s anatomy and heart rate variability. Front Psychol 5:1040
Mertens A, Carrette S, Klooster D, Lescrauwaet E, Delbeke J, Wadman WJ et al (2022) Investigating the effect of transcutaneous auricular vagus nerve stimulation on cortical excitability in healthy males. Neuromodulation Technol Neural Interface 5(3):395–406
Machetanz K, Berelidze L, Guggenberger R, Gharabaghi A (2021) Transcutaneous auricular vagus nerve stimulation and heart rate variability: analysis of parameters and targets. Auton Neurosci 236:102894
Umetani K, Singer DH, McCraty R, Atkinson M (1998) Twenty-four hour time domain heart rate variability and heart rate: relations to age and gender over nine decades. J Am Coll Cardiol 31(3):593–601
Messina G, Vicidomini C, Viggiano A, Tafuri D, Cozza V, Cibelli G et al (2012) Enhanced parasympathetic activity of sportive women is paradoxically associated to enhanced resting energy expenditure. Auton Neurosci 169(2):102–106
De Couck M, Mravec B, Gidron Y (2012) You may need the vagus nerve to understand pathophysiology and to treat diseases. Clin Sci 122(7):323–328
Entschladen F, Drell TL, Lang K, Joseph J, Zaenker KS (2004) Tumour-cell migration, invasion, and metastasis: navigation by neurotransmitters. Lancet Oncol 5(4):254–258
Haensel A, Mills PJ, Nelesen RA, Ziegler MG, Dimsdale JE (2008) The relationship between heart rate variability and inflammatory markers in cardiovascular diseases. Psychoneuroendocrinology 33(10):1305–1312
Tsutsumi T, Ide T, Yamato M, Kudou W, Andou M, Hirooka Y et al (2008) Modulation of the myocardial redox state by vagal nerve stimulation after experimental myocardial infarction. Cardiovasc Res 77(4):713–721
Vlcek M, Radikova Z, Penesova A, Kvetnansky R, Imrich R (2008) Heart rate variability and catecholamines during hypoglycemia and orthostasis. Auton Neurosci 143(1–2):53–57
Fallgatter AJ, Neuhauser B, Herrmann MJ, Ehlis AC, Wagener A, Scheuerpflug P et al (2003) Far field potentials from the brain stem after transcutaneous vagus nerve stimulation. J Neural Transm (Vienna) 110(12):1437–43. https://doi.org/10.1007/s00702-003-0087-6
Uradu A, Wan J, Doytchinova A, Wright KC, Lin AYT, Chen LS et al (2017) Skin sympathetic nerve activity precedes the onset and termination of paroxysmal atrial tachycardia and fibrillation. Heart Rhythm 14(7):964–971. https://doi.org/10.1016/j.hrthm.2017.03.030
Shen LL, Sun JB, Yang XJ, Deng H, Qin W, Du MY et al (2021) Reassessment of the effect of transcutaneous auricular vagus nerve stimulation using a novel burst paradigm on cardiac autonomic function in healthy young adults. Neuromodulation 25(3):433–442. https://doi.org/10.1111/ner.13521
Barantke M, Krauss T, Ortak J, Lieb W, Reppel M, Burgdorf C et al (2008) Effects of gender and aging on differential autonomic responses to orthostatic maneuvers. J Cardiovasc Electrophysiol 19(12):1296–1303
Abhishekh HA, Nisarga P, Kisan R, Meghana A, Chandran S, Raju T et al (2013) Influence of age and gender on autonomic regulation of heart. J Clin Monit Comput 27:259–264
Almeida-Santos MA, Barreto-Filho JA, Oliveira JLM, Reis FP, da Cunha Oliveira CC, Sousa ACS (2016) Aging, heart rate variability and patterns of autonomic regulation of the heart. Arch Gerontol Geriatr 63:1–8
Koenig J, Thayer JF (2016) Sex differences in healthy human heart rate variability: a meta-analysis. Neurosci Biobehav Rev 64:288–310
Krames E, Peckham PH, Rezai AR (2018) Neuromodulation: comprehensive textbook of principles, technologies, and therapies. Academic Press
Polak T, Markulin F, Ehlis AC, Langer JB, Ringel TM, Fallgatter AJ (2009) Far field potentials from brain stem after transcutaneous vagus nerve stimulation: optimization of stimulation and recording parameters. J Neural Transm 116:1237–1242
Kaniusas E, Kampusch S, Tittgemeyer M, Panetsos F, Gines RF, Papa M, et al. (2019) Current directions in the auricular vagus nerve stimulation I–a physiological perspective. Frontiers in neuroscience 854
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The manuscript does not contain clinical studies or patient data.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Soltani, D., Azizi, B., Sima, S. et al. A systematic review of the effects of transcutaneous auricular vagus nerve stimulation on baroreflex sensitivity and heart rate variability in healthy subjects. Clin Auton Res 33, 165–189 (2023). https://doi.org/10.1007/s10286-023-00938-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-023-00938-w