Abstract
The forebrain cerebral network including the insular cortex plays a crucial role in the regulation of the central autonomic nervous system in relation to emotional stress. Numerous studies have recently shown that the insular cortex also has roles as a vestibular area in addition to auditory function. In this review, we summarize the recent literature regarding the relationship between the insular cortex and vestibular function, and we describe our hypothesis that the insular cortex has a pivotal role in vestibular-cardiovascular integration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The insular cortex (Ic; also called the insula) is a large, phylogenetically ancient region of the human brain that comprises several parts involved in aspects of emotion, perceptual self-awareness, interoception, multimodal sensory processing, and autonomic control [1, 2]. The German anatomist Johann Christian Reil named the Ic in 1809 [3], and many other names have since been used for this region including “intralobular gyri,” “intersylvian convolutions,” the “central lobe,” the “fifth lobe of the brain,” and the “island of Reil” [4]. Reil proposed that the Ic’s convolutions were the seat of mental processes [5]. Carl Wernicke indicated that lesions of the Ic were related to conduction aphasia [6], and Sigmund Freud later suggested that the Ic is part of the brain's speech area [7]. A network comprising the Ic, the anterior cingulate gyrus, and the amygdala has crucial functions in the regulation of the body’s central autonomic nervous system (ANS) when stress-related emotions such as fear, anxiety, and sadness are experienced [4].
As illustrated in Fig. 1, the Ic is located deep within the lateral sulcus within each hemisphere of the brain in the region of the middle cerebral arteries (MCAs), and its structure thus tends to be vulnerable to a high risk of cerebrovascular disease [8, 9]. For example, damage to the Ic has been associated with an abnormally increased level of B-type natriuretic peptide (BNP), myocardial injury, and Takotsubo cardiomyopathy [10]. The neural substrate for autonomic control during affective behavior has been suggested to be based on interactions of the Ic, anterior cingulate gyrus, and orbitofrontal cortex [11].
Anterior view of a left cerebral hemisphere including the insular cortex (Ic) after the fronto-orbital and frontoparietal opercula have been removed. The middle cerebral artery (MCA) located in the anterior and superior peri-insular sulci has been severed. From Türe et al. [9]
The processing of vestibular function, musical information, and auditory information also involve the Ic [4, 12, 13]. The Ic was recently demonstrated to play a role as a vestibular area in the perception of verticality and in vestibular disorders of balance [12]. With this background, we review herein the anatomical and functional interconnections between the vestibular system and the ANS in the Ic. The precise functions and importance of vestibular inputs in autonomic regulation remain unknown, in part because of the complexity presented by secondary factors such as affective/emotional responses and cardiovascular responses. We hypothesize that the Ic has a pivotal role in vestibular-cardiovascular integration.
Anatomy of the Ic in vestibular function
The normal human Ic has five major gyri, and some individuals have additional smaller gyral areas [14,15,16]. The major gyri are oriented in the dorsal–ventral direction, with three anterior gyri known as the “short” gyri and two posterior gyri known as the “long” gyri. The short anterior gyri consist of the anterior, mid-, and posterior short gyri: ASG, MSG, and PSG. The long gyri consist of the anterior and posterior long insular gyri: ALG and PLG. All five anterior gyri converge at the insular apex, which is the most ventral portion of the superficial Ic [14,15,16].
The Ic was designated as a vestibular area [17] based on observations in New World and Old World monkeys, i.e., connections from the vestibular thalamic relay nucleus and the ventral posterior inferior nucleus to the dysgranular Ic [18,19,20]. Examinations of the cynomolgus monkey (Macaca fascicularis) revealed neurophysiologically identifiable vestibular neurons in the parieto-insular vestibular cortex (PIVC) (Fig. 2) [21]. The PIVC in humans has not been well described. The PIVC in monkeys is in the upper bank of the lateral sulcus near the posterior end of the Ic, and it includes neurons in the posterior and upper part of the granular Ic [22]. Auditory units were identified in the monkey Ic, the temporal operculum, and the lower bank of the lateral sulcus, although no vestibular neurons were identified in the dysgranular Ic. With a few exceptions, all of the vestibular neurons in the cynomolgus monkey PIVC responded to both visual and somatosensory stimulation and were classified as polymodal vestibular units [23]. In contrast, in squirrel monkeys, it was not possible to identify vestibular neurons in the granular Ic [24], but connections between the retroinsular area and the granular Ic were identified [24]. These connections support the hypothesis that a certain subset of neurons in the granular Ic have a “vestibular” function.
The cortical vestibular network in nonhuman primates (a) and humans (b). In both humans and nonhuman primates, the core of the vestibular cortex (red) is located in the midposterior Sylvian fissure and consists of the parieto-insular vestibular cortex area (PIVC) and the posterior insular cortex area [PIC in humans; visual posterior Sylvian area (VPS) in nonhuman primates]. Areas 3av and 7 in the nonhuman primate brain may be further separated into two portions each (3aNv and 3aHv; 7a and 7b). Some studies have observed activations in the inferior frontal cortex during vestibular stimulation. AI anterior insula, FEF frontal eye fields (in particular the portion that controls smooth pursuit eye movements), MIP/VIP medial/ventral intraparietal area, MST medial superior temporal area, MSTd dorsal portion of the MST, STP/STS polysensory area of the superior temporal sulcus, TPJ portion of the temporoparietal junction bordering the posterior Sylvian fissure. From Frank and Greenlee [21]
Ic stroke and vestibular syndrome
A 1994 study seeking to determine the cortical areas responsible for vestibular function in the roll plane (one of the three major planes of action of the vestibulo-ocular reflex: yaw, pitch, and roll) examined 71 patients who had suffered unilateral supratentorial infarctions [25]. The overlapping area of these infarctions centered on the posterior Ic. In addition, the perception of verticality was affected in 20 of the 52 patients with MCA infarctions. The study’s authors suggested that the posterior Ic is likely homologous to the monkey PIVC and that the PIVC (and therefore the Ic) is the dominant cortical vestibular area, as an integration center of various vestibular areas in the parietal lobe [25]. The patients who had experienced an acute cortical infarction in the MCA territory that affected mostly the posterior Ic and the temporal gyri were reported to exhibit subjective visual vertical deviations of approximately 4–6° [25]. Ocular torsion and skew deviation were not associated with this finding.
The introduction of voxel-based lesion-symptom mapping in magnetic resonance imaging (MRI) enabled the precise localization of infarctions in the posterior Ic (e.g., the long insular gyrus IV) (Fig. 3) [12, 26,27,28]. A cortical site of an infarction causes a misperception of verticality in the acute stage of stroke, which agrees with the imaging data of individuals with acute peripheral vestibular neuritis. In these individuals, subjective visual vertical tilt is positively correlated with the bilateral regional cerebral glucose metabolism for the posterior Ic and retroinsular region (more so in the right than left hemisphere) and bilaterally for the middle temporal gyrus [29].
Infarction sites that cause subjective visual vertical deviations. a Collective presentation of infarcted areas taken from MRI scans and projected onto sections of Duvernoy’s atlas in seven patients with clearly demarcated infarctions of the MCA which caused significant contralateral subjective visual vertical tilts. The overlapping areas of the infarctions (7 of 7 in black) are centered at the posterior part of the Ic, involving the short (blue arrow) and long insular gyri (purple arrow), the transverse temporal gyrus (green arrow), and the superior temporal gyrus (red arrow). b The results of a statistical voxel-wise lesion-behavior mapping (VLBM) analysis comparing 32 patients with acute right-sided infarctions and 22 patients with acute left-sided infarctions with respect to the absolute tilt of subjective visual vertical (t test statistic). Presented are all voxels that survived a correction for multiple comparisons using a 1% false discovery rate cutoff threshold. An overlay of the statistical map from the patients with left-sided infarctions (blue), flipped to the right hemisphere, and the statistical map of the patients with right-sided infarctions (red) is shown. Overlapping regions are indicated by violet arrows. From Baier et al. [27] c Illustration of the affected parts of the insula using Duvernoy’s atlas. Red Right insular lesions. Blue Left insular lesions. The circular insular, central insular, short insular, and long insular gyri were affected. From Dieterich and Brandt [12]
A 2015 assessment of the subjective visual vertical and the haptic vertical in patients at later stages (at mean day 43 during rehabilitation) after having suffered a right hemispheric stroke revealed that their lesions, which occurred more centrally on the temporo-occipital junction and the posterior part of the middle temporal gyrus, were correlated with their subjective visual vertical tilts, and the lesions that correlated with haptic tilts were located more anteriorly in the superior temporal gyrus and sulcus [30]. In contrast, in the same study's patients who had experienced an acute unilateral stroke of the right hemisphere, subjective visual vertical tilts were found to be correlated with lesions in the Ic, the rolandic operculum, the inferior frontal gyrus, and the frontal inferior operculum. Similar lesion sites were also identified in patients with lesions that are associated with tilts of the haptic visual vertical, located in the Ic, rolandic operculum, superior temporal gyrus, pallidum, Heschl's gyrus, superior longitudinal fascicle, and the corona radiata [26].
Vestibular function and the ANS
Parasympathetic nervous hypofunction and significant depression of the sympathetic response due to postural changes from the supine position to standing have been observed in many patients with Meniere's disease at the interval stage, in examinations of heart rate variability based on electrocardiography [31], and sympathetic nervous hypofunction was observed in some of the patients who were at the attack stage [31]. An imbalance of the ANS evaluated by measurements of salivary α-amylase was also observed in individuals with benign paroxysmal positional vertigo, during and after their vertigo attacks [32].
The vestibular system has been shown to modulate the sympathetic outflow to muscle [33], and in that study, the application of low-frequency sinusoidal galvanic vestibular stimulation was associated with sympathetic outflow, which was strongly entrained to vestibular inputs. Since the otolithic organs encode both static positions and linear accelerations of the head in space, these findings indicate that the vestibular apparatus contributes to the control of not only motoneurons that are involved in posture and locomotion, but also sympathetic neurons that are involved in the control of blood pressure. The vestibular modulation of the muscle sympathetic outflow clearly does play a role in the regulation of blood pressure, and the distribution of cardiac output to skeletal muscles must be controlled with the opposing regulatory demands of blood pressure; it therefore makes physiological sense for there to be a mechanism for controlling the blood flow in muscle [33].
The Ic and ANS in relation to vestibular function
Positron emission tomography (PET) was used to determine the differential effects of caloric vestibular stimulation [i.e., irrigation of the right or left ear with warm (44 °C) water] on cortical and subcortical activation in 12 right-handed and 12 left-handed healthy adults [13]. The caloric irrigation induced a direction-specific sensation of rotation and nystagmus, and significant increases in the subjects' regional cerebral blood flow were observed in a network that was present within both hemispheres in the posterior part of the Ic with the adjacent superior temporal gyrus, the inferior parietal lobule, and the precuneus. Together these areas comprise a human homologue of the multisensory vestibular cortex areas identified in monkeys and correspond to the PIVC, the visual temporal sylvian area, and areas 7 and 6. In the same study [13], further cortical activations were observed in the anterior Ic, the anterior cingulum, and the inferior frontal gyrus. The subcortical activation pattern exhibited in the thalamus, putamen, and midbrain is consistent with the manner in which the efferent ocular motor pathways are organized. During the application of monaural stimulation, the cortical and subcortical activations of the described areas were bilateral but predominant in the hemisphere ipsilateral to the stimulated ear; in the right-handed subjects these activations exhibited a significant right hemispheric dominance for vestibular and ocular motor structures. A significant left hemispheric dominance was similarly observed in the left-handed subjects [13].
Neurophysiological and neuroanatomical investigations using animal models have identified the neurons that mediate vestibulo-sympathetic responses, and these neurons include cells in the caudal aspect of the vestibular nucleus complex, interneurons in the lateral medullary reticular formation, and bulbospinal neurons in the rostral ventrolateral medulla (RVLM) [34]. This 2013 meta-analysis noted that human neuroimaging studies evaluating central autonomic processing identified a set of consistently activated brain regions (the left amygdala, the right anterior and left posterior Ic, and the mid-cingulate cortices) as the core of the central autonomic network. Sympathetic-associated regions were predominant in executive- and salience-processing networks, and parasympathetic regions were predominant in the default mode network [34].
The notion that the cardiovascular system is regulated by a central autonomic network consisting of the Ic, anterior/mid-cingulate cortices, amygdala, hypothalamus, periaqueductal gray matter (PAG), parabrachial complex, nucleus of the tractus solitarius, and RVLM is based on several studies [8, 10, 34, 35]. Taken together, those studies' findings from both animals and human demonstrated that the Ic, hypothalamus, PAG, and RVLM form a functional network that is involved in the regulation of both resting and behavior-coupled changes in muscle sympathetic nerve activity [36].
In individuals with drug-refractory epilepsy, right hemispheric inactivation induced increases in the high-frequency heart rate and blood pressure, and left hemispheric inactivation induced increases in low-frequency heart rate and blood pressure [37]. Importantly, a site of cardiac representation was identified within the human Ic [38]. Tachycardia or pressor effects were significantly common after stimulation of the right Ic, whereas bradycardia or depressor effects were significantly common after stimulation of the left Ic [38]. Thus, the right Ic is associated with sympathetic nervous system activity, and the left Ic is associated with parasympathetic nervous system activity.
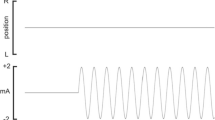
We recently treated a 51-year-old Japanese man diagnosed with herpes encephalitis and a right Ic lesion [39]. Before the diagnosis, he experienced a loss of appetite, hearing impairment, faintness, dizziness, behavior abnormalities, and a persistent high fever. Diffuse left ventricular (LV) hypokinesis was observed at 1 week after his hospital admission. Cardiac 123I-metaiodobenzylguanidine (MIBG) uptake scintigraphy revealed regional reduced uptake in the earlier phase (Fig. 4), and we thus suspected that the patient's LV hypokinesis in encephalitis was derived from reduced sympathetic nervous system activity due to right Ic dysfunction caused by the lesion [39]. This patient’s findings thus support the above-mentioned connection between the right Ic and the sympathetic nervous system.
The brain of a 51-year-old Japanese man diagnosed with herpes encephalitis. a In a diffusion-weighted MRI scan, asymmetric right greater hyperintensity was observed throughout the Ic and cingulate gyrus. b Cardiac 123I-MIBG scintigraphy in the early phase revealed reduced uptake in the inferior and posterior walls compared to thallium-201 scintigraphy. c ECG on admission demonstrated a prolonged QTc interval at 464 ms. From Kikumoto et al. [39]
A functional (f)MRI study revealed that the responses in both the right and left human Ic during the strain phase of the Valsalva maneuver differed among gyri in an anterior–posterior order, with greater responses in the anterior gyri [16]. The strain phase is characterized by a large and rapid increase in sympathetic activity [40,41,42,43]. That study confirmed the anterior location of autonomic control within the Ic, and all three anterior gyri (ASG, MSG, and PSG) responded similarly on the right side. On the left side, the activity was greatest in the ASG, followed by the MSG and then the PSG. In light of the preferential left-sided parasympathetic dominance in the Ic, it is plausible that sympathetic regulation on the left insula was greatest in the most anterior gyrus (i.e., the ASG), whereas the regulation was similar across all three anterior gyri on the right Ic [16].
The Ic and the model of multimodal integration for vestibular function
Many studies have examined the human posterior Ic and parietal operculum, which together form the core region of a multisensory vestibular cortical network [44, 45]. These two meta-analyses of vestibular function identified the posterior Ic and parietal operculum as the most likely human homologue of the multisensory PIVC in primates [44, 45]. Other investigations of the anterior Ic revealed its specialization for viscero-autonomic responses among areas such as the anterior cingulate gyrus, infralimbic cortex, and thalamus [46, 47]. In addition, several studies indicated that the anterior Ic (which projects to the amygdala, anterior cingulate gyrus, orbitofrontal cortex, dorsal thalamus, and superior temporal sulcus) is specialized for receiving interoceptive information in relation to viscero-autonomic responses [11, 46, 48]. Ic projections have also shown an abundance of local reciprocal intrainsular connections [48]. We thus hypothesize that due to its abundant connections with other association and primary sensory areas, the Ic plays the most important role in the integration for vestibular-autonomic processing among multimodal convergent sites.
Conclusion
In this review, we have summarized the recent research on the Ic and described the integrative roles of this structure in vestibular function. The Ic is thought to be involved in vestibular function and the regulation of the ANS. Based on the accumulated evidence, we hypothesize that the Ic plays an important role in humans' vestibular processing in relation to the ANS. The input from the cochlea to the central vestibular system network in relation to autonomic function would thus be important to this role of the Ic. An in vitro study demonstrated that increased catecholamine levels and inflammatory mediators altered barrier properties of microvascular endothelial cells [49], and we thus speculated that the relationship between the blood–labyrinth barrier and the central vestibular network could be mediated by the autonomic nervous balance. Investigations of the neural substrates including the Ic may obtain important insights into the common pathophysiology of vestibular dysfunction and autonomic instability (as are observed in acute coronary syndrome and arrhythmia).
Abbreviations
- AI:
-
Anterior insula
- ASG:
-
Anterior short gyrus
- FEF:
-
Frontal eye field
- Ic:
-
Insular cortex
- LG:
-
Anterior long gyrus
- MCA:
-
Middle cerebral artery
- MIP/VIP:
-
Medial/ventral intraparietal area
- MSG:
-
Mid-short gyrus
- MST:
-
Medial superior temporal area
- MSTd:
-
Dorsal portion of the MST
- PIVC:
-
Parieto-insular vestibular cortex
- PLG:
-
Posterior long gyrus
- PSG:
-
Posterior short gyrus
- STP/STS:
-
Polysensory area of the superior temporal sulcus
- TPJ:
-
Temporoparietal junction
References
Benarroch EE (2019) Insular cortex: functional complexity and clinical correlations. Neurology 93:932–938
Butti C, Hof PR (2010) The insular cortex: a comparative perspective. Brain Struct Funct 214:477–493
Reil JC (1809) Die sylvische grube. Arch Physiol (Halle) 9:195e208 ((In German))
Nagai M, Kishi K, Kato S (2007) Insular cortex and neuropsychiatric disorders: a review of recent literature. Eur Psychiatry 22:387–394
Clarke E, O’Malley CD (1996) The human brain and spinal cord: a historical study illustrated by writings from antiquity to the twentieth century. Norman Publishing, San Francisco
Wernicke C (1874) Der aphasische symptomencomplex. Cohn and Weigert, Breslau (In German)
Freud S (1891) Zur auffassung der aphasien. Deutike, Vienna ((in German))
Nagai M, Hoshide S, Kario K (2010) The insular cortex and cardiovascular system: a new insight into the brain-heart axis. J Am Soc Hypertens 4:174–182
Türe U, Yaşargil MG, Al-Mefty O, Yaşargil DC (2000) Arteries of the insula. J Neurosurg 92:676–687
Nagai M, Dote K, Kato M, Sasaki S, Oda N, Kagawa E, Nakano Y, Yamane A, Higashihara T, Miyauchi S, Tsuchiya A, Harada W, Kario K (2017) The insular cortex and Takotsubo cardiomyopathy. Curr Pharm Des 23:879–888
Critchley HD (2005) Neural mechanisms of autonomic, affective, and cognitive integration. J Comp Neurol 493:154–166
Dieterich M, Brandt T (2019) Perception of verticality and vestibular disorders of balance and falls. Front Neurol 10:172
Dieterich M, Bense S, Lutz S, Drzezga A, Stephan T, Bartenstein P, Brandt T (2003) Dominance for vestibular cortical function in the non-dominant hemisphere. Cereb Cortex 13:994–1007
Naidich TP, Kang E, Fatterpekar GM, Delman BN, Gultekin SH, Wolfe D, Ortiz O, Yousry I, Weismann M, Yousry TA (2004) The insula: anatomic study and MR imaging display at 1.5 T. AJNR Am J Neuroradiol 25:222–232
Ture U, Yasargil DC, Al-Mefty O, Yasargil MG (1999) Topographic anatomy of the insular region. J Neurosurg 90:720–733
Macey PM, Wu P, Kumar R, Ogren JA, Richardson HL, Woo MA, Harper RM (2012) Differential responses of the insular cortex gyri to autonomic challenges. Auton Neurosci 168:72–81
Augustine JR (1985) The insular lobe in primates including humans. Neurol Res 7:2–10
Burton H, Jones EG (1976) The posterior thalamic region and its cortical projection in New World and Old World monkeys. J Comp Neurol 168:249–302
Roberts TS, Akert K (1963) 1. Insular and opercular cortex and its thalamic projection in Macaca mulatta. Schweiz. Arch Neurol Neurochir Psychiatry 92:1–43
Deecke L, Schwarz DWF, Fredrickson JM (1974) Nucleus ventroposterior inferior (VPI) as the vestibular thalamic relay in the Rhesus monkey. I. Field potential investigation. Exp Brain Res 20:88–100
Frank SM, Greenlee MW (2018) The parieto-insular vestibular cortex in humans: more than a single area? J Neurophysiol 120:1438–1450
Griisser OJ, Pause M, Schreiter U (1990a) Localization and responses of neurones in the parieto-insular vestibular cortex of awake monkeys (Macaca fascicuhzris). J Physiol 430:537–557
Griisser OJ, Pause M, Schreiter U (1990b) Vestibular neurones in the parieto-insular cortex of monkeys (Macaca fascicularis): visual and neck receptor responses. J Physiol 430:559–583
Guldin WO, Akbarian S, Griisser OJ (1992) Cortico-cortical connections and cytoarchitectonics of the primate vestibular cortex: a study in squirrel monkeys (Saimiri sciureus). J Comp Neurol 326:375–401
Brandt T, Dieterich M, Danek A (1994) Vestibular cortex lesions affect the perception of verticality. Ann Neurol 35:403–412
Baier B, Janzen J, Müller-Forell W, Fechir M, Müller N, Dieterich M (2012) Pusher syndrome: its cortical correlate. J Neurol 259:277–283
Baier B, Suchan J, Karnath HO, Dieterich M (2012) Neural correlates of disturbed perception of verticality. Neurology 78:728–735
Baier B, Zu Eulenburg P, Best C, Geber C, Müller-Forell W, Birklein F, Dieterich M (2013) Posterior insular cortex—a site of vestibular-somatosensory interaction? Brain Behav 3:519–524
Becker-Bense S, Dieterich M, Buchholz HG, Bartenstein P, Schreckenberger M, Brandt T (2014) The differential effects of acute right- vs. left-sided vestibular failure on brain metabolism. Brain Struct Funct 219:1355–1367
Rousseaux M, Braem B, Honoré J, Saj A (2015) An anatomical and psychophysical comparison of subjective verticals in patients with right brain damage. Cortex 69:60–67
Yamada M, Mizuta K, Ito Y, Furuta M, Sawai S, Miyata H (1999) Autonomic nervous function in patients with Meniere’s disease evaluated by power spectral analysis of heart rate variability. Auris Nasus Larynx 26:419–426
Korkmaz T, Bicer YO, Serin E, Seyhan S, Sanal SK (2018) Salivary α-amylase levels in vertigo: can it be an autonomic dysfunction? Ear Nose Throat J 97:278–282
Hammam E, Macefield VG (2017) Vestibular modulation of sympathetic nerve activity to muscle and skin in humans. Front Neurol 8:334
Beissner F, Meissner K, Bär KJ, Napadow V (2013) The autonomic brain: an activation likelihood estimation meta-analysis for central processing of autonomic function. J Neurosci 33:10503–10511
Benarroch EE (1993) The central autonomic network: functional organization, dysfunction, and perspective. Mayo Clin Proc 68:988–1001
Macefield VG, Henderson LA (2019) Identification of the human sympathetic connectome involved in blood pressure regulation. Neuroimage 202:116119
Hilz MJ, Dutsch M, Perrine K, Nelson PK, Rauhut U, Devinsky O (2001) Hemispheric influence on autonomic modulation and baroreflex sensitivity. Ann Neurol 49:575–584
Oppenheimer SM, Gelb A, Girvin JP, Hachinski VC (1992) Cardiovascular effects of human insular cortex stimulation. Neurology 42:1727–1732
Kikumoto M, Nagai M, Ohshita T, Toko M, Kato M, Dote K, Yamashita H (2018) Insular cortex lesion and autonomic instability in a herpes simplex virus encephalitis patient. J Neurovirol 24:649–651
Benarroch EE (1997) Central autonomic network: functional organization and clinical correlations, 1st edn. Futura Pub. Co., Armonk, New York
Ewing DJ (1993) Noninvasive evaluation of heart rate: the time domain. In: Low PA (ed) Clinical autonomic disorders, 1st edn. Little, Brown & Co, Boston, Toronto, London, pp 297–314
Ewing DJ (1992) Analysis of heart rate variability and other non-invasive tests with special reference to diabetes mellitus. In: Bannister R, Mathias CJ (eds) Autonomic failure a textbook of clinical disorders of the autonomic nervous system. Oxford University Press, Oxford, pp 312–333
Hilz MJ (2002) Quantitative autonomic functional testing in clinical trials. In: Brown R, Bolton C, Aminoff M (eds) Neuromuscular function and disease. W.B. Saunders Company, Philadelphia, pp 1899–1929
Lopez C, Blanke O, Mast FW (2012) The human vestibular cortex revealed by coordinate-based activation likelihood estimation meta-analysis. Neuroscience 212:159–179
zu Eulenburg P, Caspers S, Roski C, Eickhoff SB (2012) Meta-analytical definition and functional connectivity of the human vestibular cortex. Neuroimage 60:162–169
Craig AD (2009) How do you feel—now? The anterior insula and human awareness. Nat Rev Neurosci 10:59–70
Cechetto DF (2014) Cortical control of the autonomic nervous system. Exp Physiol 99:326–331
Augustine JR (1996) Circuitry and functional aspects of the insular lobe in primates including humans. Brain Res Brain Res Rev 22:229–244
Ittner C, Burek M, Störk S, Nagai M, Förster CY (2020) Increased catecholamine levels and inflammatory mediators alter barrier properties of brain microvascular endothelial cells in vitro. Front Cardiovasc Med 7:73
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Nagai, M., Scheper, V., Lenarz, T. et al. The insular cortex as a vestibular area in relation to autonomic function. Clin Auton Res 31, 179–185 (2021). https://doi.org/10.1007/s10286-020-00744-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-020-00744-8