Abstract
Racial and ethnic differences in cardiovascular morbidity and mortality persist despite advances in risk factor identification and implementation of evidence-based treatment strategies. African American men and women are disproportionately affected by cardiovascular risk factors, particularly hypertension. In this context, previous studies have identified sex and racial differences in autonomic cardiovascular regulation which may contribute to the development of hypertension and its high morbidity burden among African Americans. In this review, we provide a comprehensive evaluation of the potential pathophysiological mechanisms of blood pressure control and their differences based on sex and race. These mechanisms include obesity-induced sympathetic activation, sympatho-vascular transduction, baroreflex sensitivity and adrenoreceptor vascular sensitivity, which have been the subjects of prior investigation in this field. Understanding the racial differences in the pathophysiology of hypertension and its co-morbid conditions would allow us to implement better treatment strategies tailored to African Americans, with the ultimate goal of reducing cardiovascular mortality in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the widespread use of evidence-based strategies to treat cardiovascular disease (CVD), racial disparities in cardiovascular (CV) morbidity and mortality persist in the United States [1,2,3]. African Americans (AAs) are 20–30% more likely to die from CVD when compared with non-Hispanic whites [1], with the highest estimated age-adjusted ischemic heart disease death rate of any racial group (95.5 deaths per 100,000 people in non-Hispanic whites compared to 107.2 deaths per 100,000 people in AAs) [4]. Estimates for age-adjusted stroke prevalence among AA adults age 20 and older is 2.5% for AA men and 3.2% for AA women [5].
The high prevalence of co-morbid conditions such as hypertension (HTN), obesity, and type 2 diabetes mellitus (T2DM) among AA is at least partially responsible for the high CVD-associated mortality rates in this group [2, 6]. Estimates from the National Health and Nutrition Examination Survey indicate that just under half (44%) of AAs have HTN [6]. In both AA men and women, HTN manifests earlier, has a more rapid progression to end organ damage (particularly renal failure), and results in worse prognoses compared to non-Hispanic whites [7]. Among adults age 20 and over, T2DM prevalence is more than twice as high among AAs compared to non-Hispanic whites (14.5% among AAs compared to 6.7% among non-Hispanic whites) [6]. Obesity estimates among adult AAs range from 70 to 80%, comparable to non-Hispanic white men, and higher than non-Hispanic white women (non-Hispanic white males 72.3% compared to non-Hispanic white females 59.3%) [6].
There are multiple factors that contribute to these health disparities such as individual patient behaviors (smoking, diet, physical activity, and excessive alcohol consumption), healthcare access, insurance coverage, genetics, bias and cultural competency among health care workers, community characteristics, and health system infrastructure [8,9,10,11]. Previous studies have shed light on racial differences in the pathophysiology of atherosclerosis as well as neurohormonal control of blood pressure; these biological dissimilarities may indicate that AAs may have unique pathophysiological mechanisms that predispose them to HTN [1, 12].
Among AA populations, AA women have significantly high prevalence of CV risk factors such as obesity and hypertension (HTN) (prevalence of obesity estimated at 80%, prevalence of HTN estimated at 56%, and largest annual increase in incidence of T2DM of any group) [13]. These risk factors likely predispose them to CVD. Among women 35–74 years old, the CVD-associated age-adjusted death rate for AA women is over 70% higher than in non-Hispanic white women [5]. A 2017 study from the National Health and Nutrition Examination Surveys data from 1999/2000 through 2011/2012 demonstrated persistence of significantly worse age-adjusted mean cardiovascular health scores among AA women compared to white women, while AA and white men scored similarly [14]. Projections from the American Heart Association predicts the most dramatic increase in CVD among AAs (to 50% by the year 2035) and women (to 45% in 2035), placing AA women at the intersection of these two high risk groups [15].
This review article examines differences in the cardiovascular autonomic nervous system that may predispose AA women to CVD. For this purpose, we performed a comprehensive search in PubMed for peer-reviewed articles, case series, cross-sectional studies and review manuscripts on race and sex-based differences in the autonomic regulation of the cardiovascular system [16]. These studies provide an overall assessment of the cardiovascular autonomic regulation in AAs, and in AA women in particular.
Obesity, African Americans, and sympathetic modulation of blood pressure
Obesity in African Americans
Obesity (BMI > 30 kg/m2) is highly prevalent among AAs. The onset of obesity occurs earlier in AAs, exposing them to greater cumulative obesity-associated health risks across the lifespan [1, 7]. Among AAs, AA women are particularly affected by overweight and obesity, with 80% of AA women estimated to have BMI > 25 [13, 17].
It has been well studied that obesity increases sympathetic nervous system (SNS) activity, which in turns increases blood pressure, contributing to HTN. Resting SNS activity as measured by muscle sympathetic nerve activity (MSNA) positively correlates with body mass index (BMI), and particularly with other measures of adiposity (visceral fat mass and subcutaneous fat mass) [18,19,20,21,22,23].
The effect of weight gain on SNS activity seems to vary between AA men and women; Victor et al. measured MSNA and 24-h blood pressure in AA men and women and evaluated associations with BMI. In young, normotensive AA women, elevated BMI was weakly associated with increased MSNA (r = 0.045, P = 0.0009) [22]. This study demonstrated that overweight AA women who appeared otherwise healthy had increased sympathetic drive, which may contribute to the development of HTN later in life. Notably, AA women have less visceral fat mass for a given unit of BMI compared with white women, which may explain the poor correlation between MSNA and BMI in this population.
Another study by the same group reported that AA men had elevated MSNA activity regardless of their body weight [24]. Weight loss has been associated with decreased SNS activity in obese subjects, however this association was true only among AA women, not among AA men. Abbas et al. reported that the reduction in visceral adiposity after a hypocaloric diet decreased MSNA by ~ 40% in AA women, but had no effect in AA men despite a reduction in leptin, insulin, and visceral fat adiposity, factors known to increase SNS activity [24]. In this study, the authors concluded that SNS activity in AA men is adiposity-independent [24]. It would be important to identify any relationship between sympathetic overactivity and HTN in AAs.
Sympathetic nervous system modulation of BP
Sympathetic control of blood pressure varies significantly throughout the body, with dramatic differences between certain organs or vascular beds [25]. The SNS may increase peripheral vascular resistance (TPR) or cardiac output to drive changes in blood pressure. A prior study from our group demonstrated that obesity-induced sympathetic activity contributed to HTN in a cohort of non-Hispanic white subjects by increasing total peripheral resistance [26]. Acute autonomic withdrawal with a ganglionic blocker disproportionately reduced systolic blood pressure in obese subjects due to a greater reduction in TPR, while cardiac output remained unchanged [26]. While obesity-associated SNS overactivity likely contributes to the development of HTN in obese white individuals, there are no studies that address sex differences within racial groups.
Considering that obese AA women have obesity-induced SNS activity, our group used a similar experimental approach to determine whether sympathetic overactivity contributes to HTN [27]. We studied four groups of patients: obese AA women with (1) hypertension and (2) normotension and obese white women with (3) hypertension and (4) normotension. In obese normotensive AA women, trimethaphan normalized blood pressure, but this effect was not observed in obese AA women with HTN (Fig. 1) [27]. In contrast, trimethaphan normalized blood pressure in obese white women with HTN and mean arterial pressure values were similar to those of obese white women with normotension [27]. These results indicated that obesity-induced HTN in AA women does not depend on the sympathetic regulation of total peripheral resistance [27]. It could be possible that the elevated SNS activity in AA with HTN raises blood pressure through modulation of renin release.
Ganglionic blockade does not normalize blood pressure in obese African American women with hypertension. a Mean arterial pressure in obese African American and non-Hispanic white women with hypertension and normotension at baseline. b Change in mean arterial pressure during trimethaphan infusion and the MAP deprived of acute autonomic modulation in those with hypertension, African Americans with normotension, and white obese women [27]. MAP Mean arterial pressure, AAs African Americans, Whites non-Hispanic whites, HTN hypertension, NTN normotension, Δ indicates change, NS not significant
Racial differences in adrenoreceptor sensitivity
The SNS mediates vascular changes through alpha-1 adrenoreceptor (AR)-mediated signaling. For this reason, studies on racial differences in vascular AR sensitivity have focused on responses to alpha-1 AR agonists or antagonists [28,29,30,31,32]. Prior studies reported racial differences in the arterial pressure response to systemic administration of phenylephrine, a selective alpha-1 AR agonist, with AAs experiencing a disproportionately greater rise in arterial blood pressure than non-Hispanic whites [29, 31]. However, extrapolation of the effects of systemic infusion of vasoactive drug on blood pressure to measure vascular sensitivity is complicated by the modulating effect of baroreflex activation. Work by another group showed higher rates of blood flow in forearm vasculature of AA men compared with non-Hispanic white males in response to phenylephrine (an alpha-1 vasoconstrictor) infusion in the brachial artery [32]. In a follow-up study, the same group found augmented alpha-1 AR-mediated venoconstriction in the dorsal hand veins of young AA men compared to non-Hispanic white men [30]. These studies demonstrate that AR hypersensitivity occurs without both arterial and venous systems [30, 32]. Furthermore, differences in genetic variation of the alpha-1B adrenoceptor, particularly one variant (rs10070745), present in 14 AA subjects but not in non-Hispanic whites, associated with lower phenylephrine ED50 and greater increase in mean arterial pressure during the cold pressor test [33]. These results suggest that this variant, enriched in AA populations, leads to greater adrenergic-mediated vasoconstriction.
While most of the studies conducted in AA populations have been composed of small cohorts of young, normotensive patients, results from a larger study of 161 older men and women with variable baseline blood pressure demonstrated an association between decreased beta-1 AR responsiveness, high blood pressure (P < 0.01), male sex (P = 0.04), and increasing BMI (P < 0.01) [28]. A nonsignificant trend was also found between reduced beta-adrenergic receptor responsiveness and AA race (P = 0.07) [28]. This study also reported a significant relationship between increased alpha-1 AR responsiveness and high blood pressure (P < 0.01), female sex (P < 0.01), and AA race (P < 0.01) [28]. These results suggest a pathophysiological mechanism of HTN wherein cardiovascular beta-1 ARs become less sensitive and alpha-1 ARs become more sensitive, especially among AAs, men, and subjects with BMI > 30 kg/m2 [28]. A small study of 16 AA and white men supports this hypothesis; they were given isoproterenol (a nonselective beta-AR agonist) after atropine-induced parasympathetic blockade [34]. The study found that AA men required a two-fold higher dose of isoproterenol to increase heart rate by 25 bpm compared to non-Hispanic white men, suggesting that AA men are less sensitive to beta-agonist stimulation [34]. These changes in AR sensitivity may contribute to the development of HTN and cardiovascular disease.
More studies are needed to characterize AR signaling in a group of AA women.
Racial differences in sympathetic-vascular transduction
A complex relationship exists between SNS activation and the end-organ responses that drive blood pressure elevation. Although SNS activity is higher among AAs, and SNS overactivity is associated with increased blood pressure, the relationship can be weak from subject to subject. Therefore a comprehensive understanding of the mechanisms involved in the regulation of blood pressure by the SNS requires a complete understanding of how the SNS impulses are transduced into hemodynamic changes [35].
An abundance of evidence has reported that AA men demonstrate exaggerated vasoconstriction to sympathoexcitatory stressors [32, 36,37,38,39]. A small study of 9 AA and 10 non-Hispanic white subjects demonstrated greater increase in mean arterial pressure (MAP) and total minute muscle sympathetic nerve activity in AA compared to whites during cold pressor stress (MAP of 33.5 ± 3 mmHg in AAs compared to 22.4 ± 3 mmHg in whites, P < 0.05; MSNA of 416 ± 24% in AAs compared to 243 ± 31% in whites, P < 0.05) [36]. Similarly, a larger study composed of 228 AA and non-Hispanic white men demonstrated greater systolic blood pressure elevation in response to cold pressor tests and a series of competitive, incentivized reaction-time tasks, which was most dramatic among AAs with elevated baseline systolic blood pressure [38].
In addition to cold pressor testing, exercise has also been shown to induce more vasoconstriction in young AA men. Barbosa et al. demonstrated that while healthy, young AA and non-Hispanic white men had similar forearm vascular conductance and blood flow at rest, AA men exhibited lower forearm vascular conductance and blood flow during exercise [40]. This study suggests that blood flow during exercise is more limited in healthy AA males compared to white counterparts. This is consistent with findings of increased vasoconstriction and reduced vasodilation at rest that were previously discussed. A randomized crossover study compared the effect of nebivolol (selectively blocks beta-1 AR and stimulates nitric oxide production) compared to metoprolol (nonselective beta blockade) to assess vasodilation after hand-grip exercises in 19 AA subjects (13 men, 6 women) with HTN [41]. The study demonstrated that nebivolol resulted in greater exercise-induced vasodilation and improved endothelial function compared to metoprolol in AA with HTN [41]. An exercise study in AA women demonstrated greater differences in systemic vascular resistance during recovery after aerobic exercise compared to non-Hispanic white women [42]. The authors suggest peripheral circulation may be more sensitive to renin-mediated vasoconstriction [42].
Several recent studies have explored the effect of psychosocial stressors on blood pressure in AA populations. A 2015 study of AA men reported a significant association between perceived control and pulse pressure, suggesting a role for psychosocial factors in influencing CVD risk [43]. A large 2016 study of from the Jackson Heart Study found associations between psychosocial stressors (manifestations of negative affect and stress) and clinically significant increases in blood pressure [44]. Another report from the Jackson Heart Study demonstrated a significant combined effect of certain genetic variants and racial discrimination leading to increased blood pressure [45], confirming the relationship between stressful events and blood pressure as a contributor to the development of HTN.
In addition to enhanced vasoconstriction of microvasculature, Adamopoulos et al. found that among normotensive men, AAs had stiffer arteries at rest (higher carotid-femoral pulse wave velocity) [39]. This trend of greater arterial stiffness in AAs has also been shown in a study of middle-aged adults from the Atherosclerosis Risk in Communities (ARIC) cohort, which found 9% greater beta stiffness index (an indicator of arterial inelasticity) in AAs [46], and among a large cohort of young adults over a 26.5-year follow-up period (greater mean brachial-ankle pulse wave velocity in AA) [47]. These studies suggest that arterial stiffening may occur earlier or at a more accelerated rate among AAs, predisposing them to the development of HTN. Together with the studies showing greater sympathetic transduction to blood pressure among AA men [39, 46, 47], the literature demonstrates differences in vascular health that may contribute to the prevalence of HTN among AAs as they age.
While these studies addressed vascular changes under stressful circumstances, they did not investigate the dynamic regulation of vascular tone and blood pressure by the SNS on a beat-to-beat basis under ordinary circumstances. The mechanisms responsible for modulating sympathetic neurovascular transduction can differ depending on stimulation and nerve firing rates. In this context, using lower-body negative pressure, Ray and Monahan demonstrated enhanced sympathetic vascular transduction for a given change in MSNA in AAs [37]. Studies by Vranish et al. investigated the relationship between changes in leg vascular conductance, total vascular conductance, and mean blood pressure that followed a burst of MSNA measured in the peroneal nerve in healthy young AAs and non-Hispanic men [48]. Changes in leg vascular conductance, total vascular conductance, and mean blood pressure temporally associated with MSNA bursts were larger in AAs versus non-Hispanic whites [48]. These findings suggested that the spontaneous sympathetic neurovascular transduction was more efficient in AA men than in whites [48]. Interestingly, resting MSNA in AAs and whites was not significantly different [48].
Several studies have investigated the effect of age on sympathetic vascular transduction [49,50,51]. One study, which compared sex- and age-related differences in transduction of sympathetic nerve activity into resting vascular tone, demonstrated an increase in sympathetic vascular transduction to blood pressure in post-menopausal women (transduction in post-menopausal women (0.07 ± 0.01 mmHg in older women compared to 0.02 ± 0.01 mmHg in young women, P = 0.001) [49]. These findings suggest that augmented sympathetic-mediated vasoconstriction in post-menopausal women may contribute to the increased population prevalence of HTN women as they age [49]. Interestingly, this same study demonstrated the opposite trend among men, with decreased transduction of sympathetic activity to vascular tone in older men (0.06 ± 0.01 mmHg in older men compared to 0.10 ± 0.01 mmHg in younger men, P = 0.003) [49]. An opposing study that examined age and sex differences in sympathetic transduction reported that older women exhibited reduced transduction compared to men of the same age and compared to younger subjects of either sex (+ 1.20 ± 0.1 mmHg increase in mean arterial pressure in post-menopausal women compared to + 1.72 ± 0.2 mmHg in older men, P < 0.05) [50]. The only study that examined racial difference in sympathetic vascular transduction to blood pressure showed that older AA subjects exhibited a blunted sympathetic neural responsiveness during standing (162 ± 39 in AAs compared to 243 ± 112 in non-Hispanic whites, P = 0.003) with a concomitant increase in pressor response compared to non-Hispanic white subjects (upright diastolic blood pressure of 80 ± 10 mmHg in AA compared to 71 ± 7 mmHg in non-Hispanic whites, P = 0.008) [51]. The authors suggest enhanced sympathetic vascular transduction, angiotensin II-mediated vasoconstriction, or venoarteriolar response as possible mechanisms [51]. In summary, sympathetic-vascular transduction has been shown to vary between AA and non-Hispanic white men, with AA subjects demonstrating greater sympathetic transduction with stress, stimulation, and at rest. There also appears to be variation that is associated with age in a sex-dependent fashion, an effect that may contribute to the prevalence of HTN among women as they age.
There are no studies to our knowledge that assess sympathetic-vascular transduction in AA women. While AA women were included in some of the studies previously discussed, the number of AA women were too small to analyze as an independent group. This is a gap in knowledge that should be addressed.
Racial differences in baroreflex responsiveness and arterial blood pressure regulation
The arterial baroreflex is the main short-term modulator of arterial blood pressure in humans. Baroreflex-mediated neural adjustments alter both peripheral vascular resistance and cardiac output (primarily via changes in heart rate) in an effort to maintain arterial blood pressure homeostasis [52, 53].
Race-based differences in baroreflex sensitivity may also contribute to disparities in the development of HTN. Previous studies identified significant dissimilarities in baroreflex sensitivity between normotensive AA and non-Hispanic white men [54,55,56]. Young AA men have a blunted heart rate response to an increase in blood pressure compared to non-Hispanic white men; the compensatory bradycardia among AA men was ~ 9 bpm higher than the value achieved in non-whites [54]. Furthermore, Zion et al. reported differences in arterial compliance and autonomic balance in AA men using the integrated area starting at the nadir of the incisura of the dicrotic notch to the end of the diastole of the radial artery pulse wave, and performed spectral analyses of blood pressure and heart rate; they found that AA men have decreased arterial compliance, parasympathetic activity, and higher sympathovagal balance [55].
Holwerda et al. used a different approach to study carotid baroreflex sensitivity in young healthy AA men; the experimental protocol involved the use of neck suction to simulate hypotension and hypertension [54]. Mean arterial pressure and heart rate were measured to calculate carotid-cardiac stimulus response curves [54]. Results demonstrated an attenuated cardiac response among AA men in all trials of neck suction [54].
Only a few studies that address baroreflex sensitivity in AA women have been published, yet they reported similar alterations in baroreflex sensitivity to those of AA men. Latchman et al. reported that young normotensive AA women demonstrated significant attenuation of resting baroreflex sensitivity in AA women compared to non-Hispanic whites matched for age, BMI, and physical activity [57]. These findings suggest that autonomic regulation of blood pressure exists between AA and non-Hispanic white women beginning in young adulthood [57]. Dysregulation of baroreflex sensitivity function in young AA women may lead to enhanced sympathetic activity and predispose them to the development of HTN as they age [57].
Sex and race differences in parasympathetic modulation of heart rate
Heart rate variability
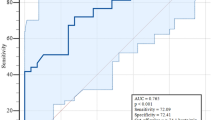
Heart rate variability (HRV) provides a noninvasive and quantitative method of investigating cardiac autonomic modulation [58]. HRV is influenced by anthropomorphic metrics including BMI [59], waist circumference [60], and physical activity [61]. Spectral analysis techniques allow differentiation between sympathetic and parasympathetic sources of HRV by assessing heart rhythm frequencies. There is consensus that the relative power in the high frequency (HFrri) band (> 0.15 Hz) reflects parasympathetic nervous system (PNS) activity, whereas the ratio of low frequency (LFrri) to HFrri wave forms reflects SNS activity (LFrri /HFrri) [38]. Using spectral analysis under controlled clinical conditions, our group demonstrated diminished parasympathetic activity (HFrri > 0.15 Hz) [62] among AA populations and, specifically, among obese AA women compared to non-Hispanic whites (Fig. 2a), consistent with published studies [63]. No differences in sympathetic modulation were observed between AA and non-Hispanic white women (Fig. 2b). Similar studies from another group demonstrated reduced PNS activity among young non-diabetic AA compared to age-matched non-Hispanic white subjects (log HFrri = 3.9 ± 3.2 in AA vs. 5.3 ± 4.7 ms2 in white subjects, P < 0.05), without concomitant changes in sympathetic activity [64]. Reduced PNS activity (as determined by low HFrri) has also been reported in AA independent of differences in physical activity and psychological stressors [65], as well as in young AA women and AA children [66]. A study of healthy adolescents found associations between low HRV and female sex and AA race, suggesting cardiac autonomic changes begin early in life with manifestations as early as adolescence [63]. In another study, decreased HRV was associated with low socioeconomic status (education level, occupation, and income), suggesting that social adversity and financial disadvantage may contribute to dysregulated autonomic cardiovascular regulation [65]. Non-Hispanic white populations exhibit similar reductions in parasympathetic modulation of the cardiovascular system only in old age, suggesting that premature aging of the PNS may occur among AA populations [64]. Young AA men without a diagnosis or family history of HTN exhibited less parasympathetic tone (HFrri) than young non-Hispanic white men (ln HFrri = 8.9 ± 1.1 vs. 9.7 ± 1.1 ms2, respectively; P = 0.006) [55]. Notably, many of these AA populations with reduced PNS activity did not have comorbid HTN.
Autonomic regulation of heart rate in obese African Americans and non-Hispanic white females. Continuous cardiac tracings in African Americans and non-Hispanic whites show a decreased PNS activity (HFrri) in African Americans compared to whites and b similar SNS modulation (LFrri/HFrri) between racial groups (Mean ± SEM, N = 28 AA women, N = 12 non-Hispanic white women)
Several studies have shown that high PNS-mediated HRV is cardioprotective [67]; decreased PNS activity, seen in AA populations, is associated with cardiovascular risk, HTN, DM, CHF, stroke, and all-cause mortality [68,69,70,71]. Given the greater prevalence, earlier onset, and worse severity of CVD among AA, as well as low PNS activity and its association with increased cardiovascular risk, it is plausible that impaired parasympathetic function among AAs may predispose them to CVD [18, 48, 60, 72].
Summary
In conclusion, there are sex and race-based differences in autonomic cardiovascular regulation in AAs that predispose them to HTN and CVD (summarized in Table 1). AA males have increased SNS activity independent of weight that did not decrease with weight loss. SNS activity in AA women is positively correlated with BMI, however this correlation is not as strong as it is in non-Hispanic white women and does not contribute to HTN by increasing peripheral vascular resistance.
The abundance of evidence suggests that AA men and women have increased sympathetic-vascular transduction, which contributes to HTN. Baroreflex sensitivity is altered in young AA men and women and begets the development of HTN. The majority of the studies related to alpha-1 AR sensitivity were performed in AA men with only one study [57] performed in AA women. AA men have generalized hypersensitivity in all vascular beds (arteries and veins) resulting in enhanced vasoconstriction; men seem to be more affected compared to women, and this increases sensitivity contributes to HTN. Finally, reduced HRV, which is a known predictor of overall cardiovascular mortality, seems to be reduced in AAs. These autonomic changes in AAs have been found in early adolescence, particularly in women.
References
Carnethon MR et al (2017) Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation 136(21):e393–e423
Safford MM et al (2012) Association of race and sex with risk of incident acute coronary heart disease events. JAMA 308(17):1768–1774
Van Dyke M (2018) Heart disease death rates among blacks and whites aged ≥35 years—United States, 1968–2015. MMWR Surveill Summ 67(5):1–11
Hyattsville MD (2019) National Center for Health Statistics. Health, United States, 2018. Hyattsville, MD
Parmley WW (2001) African American patients and heart disease. J Am Coll Cardiol 38(5):1577
Roger VL et al (2011) Heart disease and stroke statistics–2011 update: a report from the American Heart Association. Circulation 123(4):e18–e209
Mensah GA et al (2005) State of disparities in cardiovascular health in the United States. Circulation 111(10):1233–1241
Howard G et al (2017) Racial differences in the incidence of cardiovascular risk factors in older black and white adults. J Am Geriatr Soc 65(1):83–90
Graham G (2015) Disparities in cardiovascular disease risk in the United States. Curr Cardiol Rev 11(3):238–245
Finkelstein EA et al (2004) Racial/ethnic disparities in coronary heart disease risk factors among WISEWOMAN enrollees. J Womens Health (Larchmt) 13(5):503–518
Angeles H, Somers SA (2007) From Policy to Action: Addressing racial and ethnic disparities at the ground-level
Gupta DK et al (2015) Racial differences in circulating natriuretic peptide levels: the atherosclerosis risk in communities study. J Am Heart Assoc 4(5):e001831
SS V et al, on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee et al (2020) Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation 2020(141):e1–e458
Pool LR et al (2017) Trends in racial/ethnic disparities in cardiovascular health among US adults from 1999–2012. J Am Heart Assoc 6(9):e006027
American Heart Association (2017) Cardiovascular Disease: A Costly Burden for America - Projections Through 2035. 2017, American Heart Association
Liberati A et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100
Ogden CL et al (2006) Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 295(13):1549–1555
Spraul M et al (1993) Reduced sympathetic nervous activity. A potential mechanism predisposing to body weight gain. J Clin Invest 92(4):1730–1735
Scherrer U et al (1994) Body fat and sympathetic nerve activity in healthy subjects. Circulation 89(6):2634–2640
Grassi G et al (1995) Sympathetic activation in obese normotensive subjects. Hypertension 25(4 Pt 1):560–563
Weyer C et al (2000) Ethnic differences in insulinemia and sympathetic tone as links between obesity and blood pressure. Hypertension 36(4):531–537
Abate NI et al (2001) Overweight and sympathetic overactivity in black Americans. Hypertension 38(3):379–383
Alvarez GE et al (2002) Sympathetic neural activation in visceral obesity. Circulation 106(20):2533–2536
Abbas A et al (2010) Adiposity-independent sympathetic activity in black men. J Appl Physiol 108(6):1613–1618
Esler M, Lambert G, Jennings G (1989) Regional norepinephrine turnover in human hypertension. Clin Exp Hypertens A 11(Suppl 1):75–89
Shibao C et al (2007) Autonomic contribution to blood pressure and metabolism in obesity. Hypertension 49(1):27–33
Marinos A et al (2017) Hypertension in obese black women is not caused by increased sympathetic vascular tone. J Am Heart Assoc 6(11):e006971
Sherwood A et al (2017) Race and sex differences in cardiovascular α-adrenergic and β-adrenergic receptor responsiveness in men and women with high blood pressure. J Hypertens 35(5):975–981
Sherwood A, Hinderliter AL (1993) Responsiveness to alpha- and beta-adrenergic receptor agonists. Effects of race in borderline hypertensive compared to normotensive men. Am J Hypertens 6(7 Pt 1):630–635
Adefurin A et al (2013) Blacks have a greater sensitivity to α1-adrenoceptor-mediated venoconstriction compared with whites. Hypertension 61(4):915–920
Thomas KS et al (2006) Ethnicity, perceived discrimination, and vascular reactivity to phenylephrine. Psychosom Med 68(5):692–697
Stein CM et al (2000) Increased vascular adrenergic vasoconstriction and decreased vasodilation in blacks. Additive mechanisms leading to enhanced vascular reactivity. Hypertension 36(6):945–951
Adefurin A et al (2017) Genetic variation in the alpha(1B)-adrenergic receptor and vascular response. Pharmacogenomics J 17(4):366–371
Johnson JA, Burlew BS, Stiles RN (1995) Racial differences in beta-adrenoceptor-mediated responsiveness. J Cardiovasc Pharmacol 25(1):90–96
Shoemaker JK et al (2015) Neural control of vascular function in skeletal muscle. Compr Physiol 6(1):303–329
Calhoun DA et al (1993) Normotensive blacks have heightened sympathetic response to cold pressor test. Hypertension 22(6):801–805
Ray CA, Monahan KD (2002) Sympathetic vascular transduction is augmented in young normotensive blacks. J Appl Physiol 92(2):651–656
Light KC et al (1987) Effects of race and marginally elevated blood pressure on responses to stress. Hypertension 10(6):555–563
Adamopoulos D et al (2009) Intensified large artery and microvascular response to cold adrenergic stimulation in African blacks. Am J Hypertens 22(9):958–963
Barbosa TC et al (2018) Attenuated forearm vascular conductance responses to rhythmic handgrip in young African–American compared with Caucasian–American men. Am J Physiol Heart Circ Physiol 315(5):H1316–h1321
Neuman RB et al (2016) Nitric oxide contributes to vasomotor tone in hypertensive African Americans treated with nebivolol and metoprolol. J Clin Hypertens (Greenwich) 18(3):223–231
Headley SA et al (1998) Renin and hemodynamic responses to exercise in borderline hypertensives. Ethn Dis 8(3):312–318
Hill LK et al (2015) Perceived control predicts pulse pressure in African American men: the Baltimore study of black aging. Ethn Dis 25(3):263–270
Ford CD et al (2016) Psychosocial factors are associated with blood pressure progression among African Americans in the Jackson Heart Study. Am J Hypertens 29(8):913–924
Taylor JY et al (2017) The combined effects of genetic risk and perceived discrimination on blood pressure among African Americans in the Jackson Heart Study. Medicine (Baltimore) 96(43):e8369
Din-Dzietham R et al (2004) Arterial stiffness is greater in African Americans than in whites: evidence from the Forsyth County, North Carolina ARIC cohort. Am J Hypertens 17(4):304–313
Li S et al (2004) Childhood blood pressure as a predictor of arterial stiffness in young adults: the bogalusa heart study. Hypertension 43(3):541–546
Vranish JR et al (2018) Exaggerated vasoconstriction to spontaneous bursts of muscle sympathetic nerve activity in healthy young black men. Hypertension 71(1):192–198
Briant LJ et al (2016) Quantifying sympathetic neuro-haemodynamic transduction at rest in humans: insights into sex, ageing and blood pressure control. J Physiol 594(17):4753–4768
Vianna LC et al (2012) Influence of age and sex on the pressor response following a spontaneous burst of muscle sympathetic nerve activity. Am J Physiol Heart Circ Physiol 302(11):H2419–H2427
Okada Y et al (2012) Elderly blacks have a blunted sympathetic neural responsiveness but greater pressor response to orthostasis than elderly whites. Hypertension 60(3):842–848
Ogoh S et al (2005) Autonomic nervous system influence on arterial baroreflex control of heart rate during exercise in humans. J Physiol 566(Pt 2):599–611
Fadel PJ et al (2003) Recent insights into carotid baroreflex function in humans using the variable pressure neck chamber. Exp Physiol 88(6):671–680
Holwerda SW et al (2011) Carotid baroreflex responsiveness is impaired in normotensive African American men. Am J Physiol Heart Circ Physiol 301(4):H1639–H1645
Zion AS et al (2003) Low arterial compliance in young African–American males. Am J Physiol Heart Circ Physiol 285(2):H457–H462
Young BE et al (2020) Augmented resting beat-to-beat blood pressure variability in young, healthy, non-Hispanic black men. Exp Physiol 105:1102–1110
Latchman P et al (2013) Spontaneous baroreflex sensitivity in young normotensive African–American women. Clin Auton Res 23(4):209–213
(1996) Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation 93(5):1043–1065
Koenig J et al (2014) Body mass index is related to autonomic nervous system activity as measured by heart rate variability—a replication using short term measurements. J Nutr Health Aging 18(3):300–302
Windham BG et al (2012) The relationship between heart rate variability and adiposity differs for central and overall adiposity. J Obes 2012:149516
Rennie KL et al (2003) Effects of moderate and vigorous physical activity on heart rate variability in a British study of civil servants. Am J Epidemiol 158(2):135–143
Kaufmann H (1996) Consensus statement on the definition of orthostatic hypotension, pure autonomic failure and multiple system atrophy. Clin Auton Res 6(2):125–126
Faulkner MS, Hathaway D, Tolley B (2003) Cardiovascular autonomic function in healthy adolescents. Heart Lung 32(1):10–22
Choi JB et al (2006) Age and ethnicity differences in short-term heart-rate variability. Psychosom Med 68(3):421–426
Lampert R et al (2005) Depressed autonomic nervous system function in African Americans and individuals of lower social class: a potential mechanism of race- and class-related disparities in health outcomes. Am Heart J 150(1):153–160
Graziano PA et al (2011) Cardiovascular regulation profile predicts developmental trajectory of BMI and pediatric obesity. Obesity (Silver Spring) 19(9):1818–1825
Kemp AH, Quintana DS (2013) The relationship between mental and physical health: insights from the study of heart rate variability. Int J Psychophysiol 89(3):288–296
Thayer JF, Yamamoto SS, Brosschot JF (2010) The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int J Cardiol. 2009:122–131
Binkley PF et al (1991) Parasympathetic withdrawal is an integral component of autonomic imbalance in congestive heart failure: demonstration in human subjects and verification in a paced canine model of ventricular failure. J Am Coll Cardiol 18(2):464–472
Cygankiewicz I, Zareba W (2013) Heart rate variability. Handb Clin Neurol 117:379–393
Thayer JF, Lane RD (2007) The role of vagal function in the risk for cardiovascular disease and mortality. Biol Psychol 74(2):224–242
Calhoun DA et al (1994) Muscle sympathetic nervous system activity in black and Caucasian hypertensive subjects. J Hypertens 12(11):1291–1296
Acknowledgements
The authors have no acknowledgements.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MCF and RJG have no competing interests to declare. CAS received grant support from the Food and Drug Administration Office of Orphan Products Development, Grant #FD-R-04778-01-A3. CAS has received speaker honoraria from Lundbeck Pharmaceuticals. CAS received consulting honoraria from Lundbeck and Theravance Biopharma. CAS is a member of the Board of the American Autonomic Society.
Rights and permissions
About this article
Cite this article
Farrell, M.C., Giza, R.J. & Shibao, C.A. Race and sex differences in cardiovascular autonomic regulation. Clin Auton Res 30, 371–379 (2020). https://doi.org/10.1007/s10286-020-00723-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-020-00723-z