Abstract
Purpose
Metaiodobenylguanidine (MIBG) scintigraphy has been shown to enhance the probability of correct diagnosis in patients with parkinsonian syndromes (PS). Thus far, studies of the clinical usefulness of MIBG have been confined to cross-sectional assessments, which are inevitably associated with diagnostic uncertainty during the early stages of these syndromes. In this study, the initial clinical diagnosis was reevaluated longitudinally to assess the sensitivity and specificity of clinical and MIBG parameters in the early diagnosis of PS.
Methods
167 patients with PS (age 67.03 ± 8.92 years (mean ± standard deviation), duration of symptoms 2.48 ± 5.27 years, median Hoehn and Yahr score 2) underwent an initial clinical assessment and MIBG scintigraphy. Eighty seven of those patients (56 with Parkinson’s disease (PD), 1 with multiple system atrophy (MSA), 23 with atypical PS, 7 with tremor syndrome) were clinically reevaluated a mean of 3 years later in order to verify their initial diagnosis.
Results
The use of a lower limit of normal value of 1.74 for the heart-to-mediastinum ratio (HMR) achieved the best discrimination between PD and other PS. The sensitivity of MIBG scintigraphy to PD was 94%; it also had a specificity of 65%, a positive predictive value of 88%, and a negative predictive value of 79%. MIBG scintigraphy was better than initial clinical diagnosis alone (sensitivity 83%, specificity 39%) or levodopa responsiveness (sensitivity 92%, specificity 10%). However, a combination of clinical diagnosis and MIBG scintigraphy was found to be especially clinically useful (specificity 95%, sensitivity 83%, positive predictive value 95%, negative predictive value 83%).
Conclusion
MIBG scintigraphy was demonstrated to be a reliable tool for the diagnosis of early PD. The best diagnostic accuracy was achieved by combining a clinical examination with MIBG scintigraphy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Clinical diagnostic criteria continue to be key to the diagnosis of parkinsonian syndromes [1, 2]. Even when considered over the long term, these criteria are associated with significant uncertainties, with post-mortem studies showing error rates up to 25% [3]. Following the first reports in 1997 [4, 5], evidence has accumulated that the scintigraphically measured myocardial uptake of the norepinephrine analogue metaiodobenzylguanidine (MIBG) is reduced during the early stages of Parkinson’s disease (PD). This phenomenon could aid the diagnosis and differential diagnosis of PD [6,7,8,9,10]. However, data on the sensitivity and specificity of this method have thus far been based on cross-sectional studies.
In the study performed in the present paper, the initial clinical diagnosis was reevaluated later during the course of the disease to improve the accuracy of diagnosis. The diagnostic sensitivity and specificity of the longitudinally verified diagnosis of parkinsonian syndromes (PS) using MIBG scintigraphy, as well as those of a clinical examination and the levodopa-response test, were assessed.
Patient population and methods
Patients
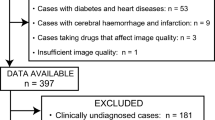
167 patients with PS who underwent MIBG scintigraphy at an early stage of their disease were retrospectively identified in the clinical records of 7 neurological outpatient services in southeast Germany. 80 patients, including 28 deceased patients, were lost to follow-up. 87 were available for clinical reevaluation of their diagnosis at a mean of 3.09 ± 1.72 years after the initial diagnosis. The follow-up population included 56 patients with idiopathic Parkinson’s disease, 1 with multiple system atrophy, 23 with atypical PS, and 7 with essential tremor. After obtaining their informed consent to participate in this study, a complete standardized neurological clinical examination was performed for each patient. Medication and comorbidities were recorded, and specific tests for associated dementia and depression were carried out. Table 1 shows the clinical characteristics of the total population and the follow-up population. Clinical characteristics of the follow-up population were representative of the total population, as no statistically significant differences between the cohorts were found.
Methods
All of the patients in the follow-up population gave their informed consent to participate in this study.
The initial early clinical evaluation and diagnostic classification were performed by the treating neurologist at a mean of 2.48 ± 5.27 years after the onset of symptoms. The results and diagnosis were documented in medical records and letters to the patient’s general physicians. MIBG scintigraphy was performed at this time as a routine diagnostic method and the heart-to-mediastinum ratio (HMR) was calculated to quantify cardiac MIBG uptake. The mean time difference between the initial and follow-up visit was 3.09 ± 1.72 years. The follow-up evaluation included a semi-structured interview to obtain clinical information on medical and drug history and the course of the disease, as well as a neurological examination. The neurological examination probed the cranial nerves; the motor system, including rigidity, tapping tests of fingers and feet, abnormal movements, and deep tendon reflexes; sensation, including stereognosis and two-point-discrimination; cerebellar function; postural stability and gait; and clinical symptoms of autonomic nervous system function such as bladder function, orthostatic tolerance, and sweating. The Hoehn and Yahr stage was determined. The “Test zur Früherkennung von Demenzen und Depression” (TFDD, a test for the early detection of dementia and depression) was performed, which studied the patient’s immediate and delayed memory function, orientation in time, ability during the clock-drawing test, and verbal fluency, and checked for signs and symptoms of depression.
Diagnostic criteria for the follow-up diagnosis of PD were based on the criteria published by Gelb et al. [1], based on the second consensus statement on the diagnosis of MSA [11, 12]. Patients who did not fulfill the criteria for PD or MSA were diagnosed with atypical PS. Essential tremor was diagnosed based on typical clinical characteristics in the absence of other signs or symptoms.
MIBG scintigraphy
MIBG is a norepinephrine analogue that is actively transported into noradrenaline granules of sympathetic nerve terminals by the noradrenaline transporter and released upon stimulation by acetylcholine [13, 14]. Radioactive iodine (131I/123I) is used to visualize the uptake and storage of MIBG in noradrenergic postganglionic neurons. Thus, cardiac MIBG uptake reflects not only the localization but also the functionality of these neurons. None of the patients was on any medication that interfered with MIBG uptake [15] or suffered from any other cardiac or neurological disorders that impaired MIBG uptake. The thyroid gland was blocked with potassium iodide. Four hours after the intravenous injection of 111 MBq of MIBG, anterior planar images of the chest were obtained using a dual-head gamma camera system (Siemens e.cam Dual Head). To quantify cardiac MIBG uptake, regions of interest were manually defined that covered the heart and a representative rectangle over the upper mediastinum as reference. Cardiac MIBG uptake counts per pixel in these two areas were measured, and HMR was calculated (Fig. 1). Estorch et al. empirically demonstrated a physiological reduction in MIBG uptake with age in their study of 39 cancer patients [16]. However, this potential confounder of the MIBG results can be neglected in our patient cohorts due to the homogeneous age distribution.
Examples of the cardiac uptake of MIBG. Left image shows a patient with MSA and the right image shows a patient with idiopathic PD. Regions of interest are shown as a rectangular region (mediastinum) and a circle (heart). There is similar uptake in the lungs and liver (bottom left), whereas the uptake of the heart differs considerably
A receiver operating characteristic curve (ROC) (Table 2) was calculated to obtain the best discrimination threshold for cardiac MIBG uptake. A HMR of 1.74 achieved the highest sum of sensitivity and specificity and therefore discriminated most accurately between normal results and a reduced uptake in the images taken 4 h after injection.
The calculated lower limit for a normal HMR (1.74) is in line with the value of 1.75 suggested by Takatsu et al. [9] and Braune [8]. Using HMR limits of 1.48 to include patients with Lewy body dementia [17] or 1.43 to distinguish normal subjects [18] would modestly increase the specificity from 65 to 78% but would markedly reduce the sensitivity from 94 to 68%, leading to an overall reduction in the sum of sensitivity and specificity from 1.59 to 1.45.
Results
Sensitivity and specificity of early clinical diagnostic examination
The sensitivity and specificity of the early clinical diagnostic examination were assessed using the results of the follow-up examination as a reference. With this protocol, the initial clinical examination reached a sensitivity of 83%, a specificity of 39%, a positive predictive value (PPV) of 79%, and a negative predictive value (NPV) of 45% (Table 3).
Sensitivity and specificity of MIBG scintigraphy
The sensitivity and specificity of MIBG scintigraphy in the early stages of the disease were calculated assuming that the diagnosis made at the follow-up examination was the “true” diagnosis. MIBG scintigraphy with a lower limit for a normal HMR of 1.74 was found to to be a reliable early indicator of Parkinson’s disease with a sensitivity of 94% and a specificity of 65%. The positive predictive value (PPV) was 88% and the negative predictive value (NPV) was 79%.
Combined sensitivity and specificity values of clinical examination, MIBG scintigraphy, and levodopa response
The combined sensitivity and specificity values of clinical examination, MIBG scintigraphy, and levodopa response during the early stages of PS were calculated using the diagnosis made during the follow-up clinical evaluation as reference. The combination of an early clinical examination and early MIBG scintigraphy showed a sensitivity of 95% and a specificity of 83%. The PPV was 95% and the NPV was 83%.
The combination of an early clinical examination, early MIBG scintigraphy, and early levodopa response presented a sensitivity of 100%, but its specificity was as low as 50%. The PPV was 98% and the NPV was 100% (Table 4).
Discussion
The accurate diagnosis of PS at an early stage provides the basis for making appropriate decisions regarding patient management and treatment, and is becoming increasingly important given that new therapies targeting intracellular pathomechanisms are on the horizon. Thus, diagnostic tools that have been shown to provide high accuracy in the differential diagnosis of PS during the early stages of the disease are needed.
In this study, the initial clinical diagnosis was reevaluated an average of 3 years later to enhance the probability of correct diagnostic classification. This period of time is seen as sufficient to detect changes in clinical symptomatology that may conflict with the initial diagnosis. Using the follow-up diagnosis as reference, the accuracy of the initial clinical examination alone at an early stage of the disease was found to be disappointing, based on its sensitivity (83%), specificity (39%), PPV (79%), and NPV (45%)—a result that is in line with other representative studies [3, 19, 20]. The sensitivity of the levodopa response (a frequently used diagnostic tool) alone was 92%, but its specificity was just 10% or lower during the early stages of the disease (mean H&Y 1.8, PPV 83%, NPV 20%). The combination of a clinical examination fulfilling the clinical criteria for PD and the levodopa response showed enhanced sensitivity (100%) but an unacceptably low specificity (50%). The short-term levodopa response was reported to have even lower accuracy [21].
The accuracy and validity of various technical diagnostic tools for the differential diagnosis of extrapyramidal neurodegenerative disorders have been investigated in previous studies. Routine magnetic resonance imaging (MRI) analysis of 32 patients with PD, 28 with multiple system atrophy (MSA), 30 with progressive supranuclear palsy (PSP), and 26 with corticobasal degeneration (CBD) showed a specificity for PD of 91% and a sensitivity of 71% (MSA), 70% (PSP), and 92% (CBD), respectively; it should be noted, however, that the disease stage of each patient is not known [22]. Brain MRI apparent diffusion coefficient values of the putamen and cerebellum showed similar area under the curve values to those in MIBG scintigraphy for small patient groups [22,23,24]. However, MRI techniques currently require further standardization and validation in bigger patient cohorts and at early disease stages.
Different radioligands have been employed to quantify presynaptic ([123I]N-ω-fluoropropyl-2β-carbomethoxy-3β-(4-iodophenyl)nortropane single photon emission computed tomography, FP-CIT-SPECT; L-6-[18F]fluoro-3,4-dihydroxyphenylalanine positron emission tomography, 18F DOPA-PET) and postsynaptic (123I-iodobenzamide single photon emission computed tomography, IBZM-SPECT;11C raclopride positron emission tomography, raclopride-PET) dopaminergic receptors. Their usefulness in the early stages of PS remains unclear, as some patients were only diagnosed in the late stages of the disease (n = 659 for FP-CIT-SPECT, n = 249 for 18F DOPA-PET, n = 39 for IBZM-SPECT, n = 128 for raclopride-PET) [25]. FP-CIT-SPECT was reported to discriminate between presynaptic parkinsonian syndromes (Parkinson’s disease or atypical parkinsonism) and essential tremor (sensitivity: 80%, specificity: 95%) or vascular parkinsonism (sensitivity: 80%, specificity: 100%) and healthy individuals [26]. Both of the SPECT methods showed poor abilities to differentiate between PD and atypical parkinsonism (FP-CIT-SPECT: sensitivity 80%, specificity 24%; IBZM-SPECT: sensitivity 69%, specificity 57%) [27]. Even using a combination of both SPECT techniques did not significantly improve diagnostic accuracy [28]. When they used automated image-based classification of18F DOPA-PET, Tang et al. [29] reported a sensitivity of 84%, a specificity of 97%, a PPV of 98%, and a NPV of 82% for PD identification (MSA: sensitivity 85%, specificity 96%, PPV 97%, NPV 82%; PSP: sensitivity 88%, specificity 94%, PPV 91%, NPV 92%; N = 167 (PD: 96), H&Y: 2.4). Nevertheless, PET is still a relatively expensive technique that is not widely available. Its value during the early stages of the disease is unknown. Hence, additional cerebral imaging is necessary to exclude vascular parkinsonism before using SPECT or PET.
MIBG scintigraphy is a well-established and standardized technique that is available in almost any nuclear medicine service center. MIBG scintigraphy distinguishes idiopathic PD from MSA, PSP, and essential tremor, which are the disorders that are most frequently misdiagnosed as idiopathic Parkinson’s disease at an early stage of the disease. The usefulness of MIBG scintigraphy as a diagnostic tool for PS has been demonstrated by cross-sectional studies that included more than 2500 patients [10]. In the last few decades, several studies have reported sensitivities of between 79 and 100% and specificities of between 84 and 89% for the identification of patients with PD [30]. Due to its high accuracy in differentiating between pre- and postganglionic disorders, MIBG scintigraphy is recommended for the diagnosis of PD in the guidelines of the American Academy of Neurology [31], as well as by the European Federation of Neurological Societies (EFNS), as it provides level A evidence [32].
In accordance with previous results [8, 9], a lower limit for a normal HMR of 1.74 in cardiac MIBG uptake was found to provide the best discrimination of PS patients. Also, the sensitivity and specificity of MIBG scintigraphy in our patients were in good accord with the results from a metaanalysis of MIBG diagnostic accuracy in early-stage PD (sensitivity 94.1%, specificity 80.2% [4]; our data: sensitivity 94%, specificity 65%, PPV 88%, NPV 79%). The reduced specificity observed in our study most likely reflects the impact of the longitudinal verification of the diagnosis in this real-world setting versus the one-time diagnosis (with its inevitable inaccuracies) made during an early stage of the disease in previous cross-sectional studies.
The combination of MIBG scintigraphy and a clinical examination fulfilling the diagnostic criteria for PD outperformed the other tests available, yielding a sensitivity of 95%, a specificity of 83%, a PPV of 95%, and a NPV of 83% during the early stages of the disease. The value of MIBG scintigraphy is underlined by comparing patients with identical initial and follow-up clinical diagnoses (n = 62) to patients with diverging clinical diagnoses (n = 25). In the first subgroup, 52 of the 53 PD patients were diagnosed correctly by MIBG scintigraphy (H/M ratio < 1.74) at an early stage of the disease. However, even when the initial clinical diagnosis had to be corrected at the follow-up, PD was initially correctly diagnosed by MIBG scintigraphy in 8 of the 11 patients.
In conclusion, assessing the MIBG cardiac uptake improves the diagnostic accuracy for PD beyond that afforded by a clinical diagnostic examination. In comparison to MRI, PET, and SPECT cerebral imaging, HMR measurement provides higher sensitivity and specificity during the early stages of the disease. Therefore, MIBG scintigraphy is correctly recommended in the current guidelines of the German and American neurological associations and by the EFNS as a well-established and validated diagnostic tool for PS.
References
Gelb DJ, Oliver E, Gilman S (1999) Diagnostic criteria for Parkinson disease. Arch Neurol 56(1):33–39
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, Obeso J, Marek K, Litvan I, Lang AE, Halliday G, Goetz CG, Gasser T, Dubois B, Chan P, Bloem BR, Adler CH, Deuschl G (2015) MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 30(12):1591–1601
Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55(3):181–184
Satoh A, Serita T, Tsujihata M (1997) Total defect of metaiodobenzylguanidine (MIBG) imaging on heart in Parkinson’s disease: assessment of cardiac sympathetic denervation. Nihon Rinsho 55(1):202–206
Braune S, Reinhardt M, Bathmann J, Krause T, Lehmann M, Lücking CH (1998) Impaired cardiac uptake of meta [123I] iodobenzylguanidine in Parkinson’s disease and autonomic failure. Acta Neurol Scand 97:307–314
Orimo S, Suzuki M, Inaba A, Mizusawa H (2012) 123I-MIBG myocardial scintigraphy for differentiating Parkinson’s disease from other neurodegenerative parkinsonism: a systematic review and meta-analysis. Parkinsonism Relat Disord 18(5):494–500
Yoshita M (1998) Differentiation of idiopathic Parkinson’s disease from striatonigral degeneration and progressive supranuclear palsy using iodine 123 metaiodobenzyl-guanidine myocardial scintigraphy. J Neurol Sci 155:60–67
Braune S (2001) The role of cardiac metaiodobenzylguanidine uptake in the differential diagnosis of parkinsonian syndromes. Clin Auton Res 11(6):351–355
Takatsu H, Nagashima K, Murase M, Fujiwara H, Nishida H, Matsuo H, Watanabe S, Satomi K (2000) Differentiating Parkinson disease from multiple-system atrophy by measuring cardiac iodine-123 metaiodobenzylguanidine accumulation. JAMA 284(1):44–45
Treglia G, Cason E, Stefanelli A, Cocciolillo F, Di Giuda D, Fagioli G, Giordano A (2012) MIBG scintigraphy in differential diagnosis of Parkinsonism: a meta-analysis. Clin Auton Res 22:43–55
Gilman S, Wenning GK, Low PA, Brooks DJ, Mathias CJ, Trojanowski JQ, Wood NW, Colosimo C, Dürr A, Fowler CJ, Kaufmann H, Klockgether T, Lees A, Poewe W, Quinn N, Revesz T, Robertson D, Sandroni P, Seppi K, Vidailhet M (2008) Second consensus statement on the diagnosis of multiple system atrophy. Neurology 71(9):670–676
Osaki YL, Ben-Shlomo Y, Lees AJ, Wenning GK, Quinn NP (2009) A validation exercise on the new consensus criteria for multiple system atrophy. Mov Disord 24(15):2272–2276
Sisson JC, Wieland DM, Sherman P, Mangner TJ, Tobes MC, Jacques S Jr (1987) Metaiodobenzylguanidine as an index of the adrenergic nervous system integrity and function. J Nucl Med 28:1620–1624
Sisson JC, Shapiro B, Meyers L, Mallette S, Mangner TJ, Wieland DM, Glownaik JV, Sherman P, Beierwaltes WH (1987) Metaiodobenzylguanidine to map scintigraphically the adrenergic nervous system in man. J Nucl Med 28:1625–1636
Solanki KK, Bomanji J, Moyes J, Mather SJ, Trainer PJ, Britton KE (1992) A pharmacological guide to medicines which interfere with the biodistribution of radiolabeled meta-iodobenzylguanidine (MIBG). Nucl Med Commun 13:513–521
Estorch M, Carrió I, Berná L, López-Pousa J, Torres G (1995) Myocardial iodine-labeled metaiodobenzylguanidine 123 uptake relates to age. J Nucl Cardiol. 2(2 Pt 1):126–132
Lamotte G, Morello R, Lebasnier A, Agostini D, Defer GL (2015) Accuracy and cutoff values of delayed heart to mediastinum ratio with (123)I-metaiodobenzylguanidine cardiac scintigraphy for Lewy body disease diagnoses. BMC Neurol 15(15):83
Muxí A, Paredes P, Navales I, Valldeoriola F, Gaig C, Lomeña F, de la Cerda A, Solà O, Domenech B, Tolosa E, Pons F (2011) Diagnostic cutoff points for 123I-MIBG myocardial scintigraphy in a Caucasian population with Parkinson’s disease. Eur J Nucl Med Mol Imaging 38(6):1139–1146
Rajput AH, Rozdilsky B (1991) Accuracy of clinical diagnosis in parkinsonism—a prospective study. Can J Neurol Sci 18(3):275–278
Hughes AJ, Daniel SE, Lees AJ (2001) Improved accuracy of clinical diagnosis of Lewy body Parkinson’s disease. Neurology 57(8):1497–1499
Asayama S, Wate R, Kaneko S, Asayama T, Oki M, Tsuge A, Nagashima M, Morita J, Nakamura S, Nakamura M, Nishii M, Fujita K, Saito A, Nakano S, Ito H, Kusaka H (2013) Levodopa challenge test and (123)I-metaiodobenzylguanidine scintigraphy for diagnosing Parkinson’s disease. Acta Neurol Scand 128(3):160–165
Yekhlef F, Ballan G, Macia F, Delmer O, Sourgen C, Tison F (2003) Routine MRI for the differential diagnosis of Parkinson’s disease, MSA, PSP, and CBD. J Neural Transm 110:151–169
Sako W, Abe T, Murakami N, Miyazaki Y, Izumi Y, Harada M, Kaji R (2016) Imaging-based differential diagnosis between multiple system atrophy and Parkinson’s disease. J Neurol Sci 368:104–108
Umemura A, Oeda T, Hayashi R, Tomita S, Kohsaka M, Yamamoto K, Sawada H (2013) Diagnostic accuracy of apparent diffusion coefficient and 123I-metaiodobenzylguanidine for differentiation of multiple system atrophy and Parkinson’s disease. PLoS One 8(4):e61066
Cummings JL, Henchcliffe C, Schaier S, Simuni T, Waxman A, Kemp P (2011) The role of dopaminergic imaging in patients with symptoms of dopaminergic system neurodegeneration. Brain 134:3146–3166
Vlaar AM, de Nijs T, Kessels AG, Vreeling FW, Winogrodzka A, Mess WH, Tromp SC, van Kroonenburgh MJ, Weber WE (2008) Diagnostic value of 123I-ioflupane and 123I-iodobenzamide SPECT scans in 248 patients with Parkinsonian syndromes. Eur Neurol 59:258–266
Pifarré P, Cuberas G, Hernández J, Lorenzo C, Miquel F, Castell-Conesa J (2010) Cortical and subcortical patterns of I-123 iodobenzamide SPECT in striatal D(2) receptor parkinsonisms. Clin Nucl Med 35:228–233
Mo SJ, Linder J, Forsgren L, Larsson A, Johansson L, Riklund K (2010) Pre- and postsynaptic dopamine SPECT in the early phase of idiopathic parkinsonism: a population-based study. Eur J Nucl Med Mol Imaging 37(11):2154–2164
Tang CC, Poston KL, Eckert T, Feigin A, Frucht S, Gudesblatt M, Dhawan V, Lesser M, Vonsattel JP, Fahn S, Eidelber D (2010) Differential diagnosis of parkinsonism: a metabolic imaging study using pattern analysis. Lancet Neurol 9:149–158
Chiaravalloti A, Stefani A, Pierantozzi M, Stanzione P, Schillaci O (2013) Does 123I-MIBG scintigraphy really assist the diagnosis of Parkinson’s disease? Parkinsonism Relat Disord 8:772–773
Montgomery EB Jr (2006) Practice parameter: diagnosis and prognosis of new onset Parkinson disease (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 67(12):2266–2267
Berardelli A, Wenning GK, Antonini A, Berg D, Bloem BR, Bonifati V, Brooks D, Burn DJ, Colosimo C, Fanciulli A, Ferreira J, Gasser T, Grandas F, Kanovsky P, Kostic V, Kulisevsky J, Oertel W, Poewe W, Reese JP, Relja M, Ruzicka E, Schrag A, Seppi K, Taba P, Vidailhet M (2013) EFNS/MDS-ES/ENS recommendations for the diagnosis of Parkinson’s disease. Eur J Neurol 20(1):16–34
Acknowledgments
We wish to thank our patients and neurological colleagues, in particular Wolfgang Klein, Herbert Lehner, Christoph Schormaier, Michael Bauer, allowing us to include their data and examinations into this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest with respect to the research, authorship, and/or publication of the article.
Ethical standards
The authors declare that this study has been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All persons gave their informed consent prior to their inclusion in the study.
Rights and permissions
About this article
Cite this article
Brandl, S.J., Braune, S. Sensitivity and specificity of cardiac metaiodobenzylguanidine scintigraphy in the early diagnosis of Parkinson’s disease. Clin Auton Res 29, 567–574 (2019). https://doi.org/10.1007/s10286-018-0534-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-018-0534-y