Abstract
Objective
The current study aimed to investigate autonomic dysfunction in Guillain–Barré syndrome (GBS) patients and describe the results of computational heart rate variability (HRV)/baroreflex sensitivity (BRS) and autonomic challenge tests.
Methods
GBS patients were consecutively recruited and the results were compared to age- and gender-matched healthy controls. A series of autonomic function tests including computation-dependent tests (power spectrum analysis of HRV and BRS at rest) and challenge maneuvers (deep breathing, eyeball compression, active standing, the Valsalva maneuver, sustained handgrip, and the cold pressor test) were performed.
Results
Ten GBS patients (six men; mean age = 40.1 ± 13.9 years) and ten gender- and age-matched healthy controls were recruited. The mean GBS functional grading scale at disease plateau was 3.4 ± 1.0. No patients required intensive care unit admission or mechanical ventilation. Low-frequency HRV (p = 0.027), high-frequency HRV (p = 0.008), and the total power spectral density of HRV (p = 0.015) were significantly reduced in patients compared to controls. The mean up slope (p = 0.034), down slope (p = 0.011), and total slope (p = 0.024) BRS were significantly lower in GBS patients. The diastolic rise in blood pressure in the cold pressor test was significantly lower in GBS patients compared to controls (p = 0.008).
Interpretation
Computation-dependent tests (HRV and BRS) were more useful for detecting autonomic dysfunction in GBS patients, whereas the cold pressor test was the only reliable challenge test, making it useful as a bedside measure of autonomic function in GBS patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Guillain–Barré syndrome (GBS) is an immune-mediated disease of the peripheral nerves characterized by acute or subacute onset of weakness with areflexia and sensory deficits [1]. Besides motor and sensory deficits, GBS is often associated with autonomic involvement such as cardiovascular, vasomotor, sudomotor, or gastrointestinal dysfunction in both the sympathetic and parasympathetic nervous systems. Signs of sympathetic and parasympathetic failure may be present, as well as overactivity of the sympathetic and parasympathetic nervous systems. Various studies have reported the mortality rate in cases of GBS to be 3–13%, usually due to respiratory, cardiovascular, or autonomic complications [2,3,4]. Approximately 50% of the mortality due to GBS can be attributed to autonomic dysfunction [5, 6]. Serious autonomic complications may present as cardiac arrhythmias, sustained or episodic hypertension, pronounced blood pressure (BP) fluctuations, or orthostatic hypotension. Advances in mechanical ventilation and critical care along with immunotherapy have led to a reduction in the mortality associated with GBS to 2.8%, or approximately 3.9% in patients with extended follow-up at 12 months [4]. Given that half of the mortality rate associated with GBS is related to autonomic dysfunction, it is crucial to identify and address symptoms such as cardiac arrhythmias earlier. The use of autonomic function tests (AFT) is crucial to identifying and monitoring autonomic disturbances in GBS patients, as autonomic dysfunction may occur subclinically [7].
The assessment of autonomic nervous system function using classical challenge maneuvers is often difficult, as severely disabled and mechanically ventilated GBS patients are unable to perform such maneuvers [8]. Up to 30–56% of patients with GBS require mechanical ventilation in an intensive care unit [9, 10]. Newer methods of assessment using computation-dependent methods such as heart rate variability (HRV) and baroreflex sensitivity (BRS) offer a solution to this issue, as they require minimal patient cooperation. HRV is a measure of the fluctuations in the heart rate (HR) over time and can be determined at rest. It can be determined using either time- or frequency-domain analysis. Time-domain analysis using a simple statistical formula such as the standard deviation is simpler than frequency-domain analysis, in which oscillations in HR are measured at different frequencies [11]. However, frequency-domain analysis has the advantage of being able to differentiate sympathetic and parasympathetic function. HR oscillations at different frequencies can be measured by different methods, which can be classified into nonparametric methods (e.g., the fast Fourier transform) and the parametric autoregressive method [11]. Oscillations within the high-frequency range are a measure of parasympathetic function, whereas oscillations within the low-frequency range are attributed to sympathetic control, although a parasympathetic influence can also be observed. Autonomic function can also be determined at rest by assessing baroreflex sensitivity. The autonomic balance that maintains the BP is delicately regulated by baroreceptors in the carotid sinuses and aortic arch [12]. Defects in baroreceptor reflex sensitivity occur when these receptors no longer respond optimally. BRS is typically measured noninvasively using synchronized continuous BP measurement and HR measurement [13].
In the current study, we consecutively investigated the autonomic dysfunction of patients with GBS by administering quantitative computational and challenge tests. We examined the results of HRV/BRS and autonomic challenge tests and determined bedside measures that best reflect autonomic dysfunction in patients with GBS.
Methods
All consecutive patients who fulfilled the diagnostic criteria for GBS or a variant of it [15] and presented to the University of Malaya Medical Center from September 2015 to February 2017 were recruited. Subjects with pre-existing conditions that could involve the autonomic nervous system were excluded, such as (1) those known to have cardiac arrhythmias (other than atrial fibrillation), (2) those with diabetes mellitus/impaired glucose tolerance who had shown symptoms of autonomic dysfunction, (3) those on medications with known effects on autonomic function. Age- and gender-matched healthy controls were also recruited for comparison. The study was approved by the local ethics committee (MECID no: 20158-1544) and all patients provided written informed consent.
Routine assessments of patients, such as the Medical Research Council (MRC) sum score [16], the GBS disability scale [17], lumbar puncture and nerve conduction studies (NCSs) [18], were performed as per the standard protocol before subjecting the patients to AFTs. The MRC sum score is defined as the sum of the MRC scores of six muscle groups bilaterally, which results in a sum score ranging from 0 (paralysis) to 60 (normal strength). The GBS disability scores (GDS) were: 0, healthy, no signs or symptoms of GBS; 1, minor symptoms or signs and able to run; 2, able to walk 5 m without assistance; 3, able to walk 5 m with assistance; 4, chairbound/bedbound; 5, requiring assisted ventilation; and 6, dead [17]. NCSs were performed as described elsewhere [18]. At least two limbs were assessed, including four motor nerves and three sensory nerves, as well as F-wave latencies. Reference values were derived from NCSs performed on normal subjects at our laboratory. An electrodiagnosis of acute inflammatory demyelinating polyneuropathy (AIDP) or axonal GBS was made based on Ho’s and Hadden’s electrodiagnostic criteria [19, 20]. According to these criteria, patients were classified based on the results of their electrophysiology studies as AIDP, axonal, unclassified, or normal.
Together with the NCS, sympathetic skin response (SSR) was performed using the same electromyography machine. SSR was recorded according to a previously described method using surface electrodes [21]. The active electrode was attached to the palm or sole, and the reference electrode to the dorsum of the hand or foot, respectively. Electrical stimulation of intensity 30 mA and duration 0.2 ms was delivered to the wrist contralateral to the recording side. An amplification sensitivity of 100 µV/division and a sweep speed of 500 ms/division were used. The low-frequency filter setting was 0.2 Hz. The responses were recorded as either absent or present. SSR was considered absent if no response was recorded after at least three attempts to provide unexpected stimuli at irregular intervals.
Autonomic function tests were performed on all patients soon after the diagnosis of GBS was made and before the start of treatment. Prior to the AFTs, patients were assessed at the bedside for any evidence of clinically overt autonomic dysfunction based on HR and BP monitoring, a 12-lead electrocardiogram (ECG), sweating abnormalities, or sphincter disturbances.
Autonomic function tests were performed in the laboratory whenever possible, and at the bedside whenever patients were medically unstable or unable to transfer to a wheelchair. Standardized conditions were maintained as follows. The temperature was maintained at 24–27 °C. Each subject lay quietly for at least 10 min before testing. Continuous beat-to-beat BP measurements were obtained using the vascular unloading method from the index or ring finger using the Task ForceTM Monitor (CNSystems, Austria). The vascular unloading method involves obtaining the blood pressure using a small pressurized cuff positioned over a finger in conjunction with a photoplethysmograph. A synchronized continuous ECG signal was obtained with the standard limb leads. Patients were asked to avoid caffeinated drinks at least 6 h prior to testing.
Autonomic nervous system function was assessed using both computational tests (power spectrum analysis of HRV and BRS) and challenge maneuvers (deep breathing, eyeball compression, active standing, the Valsalva maneuver, isometric exercise, and the cold pressor test), as described in further detail in the Electronic supplementary material (ESM). Parasympathetic function was represented by high-frequency (HF) HRV, heart rate responses to deep breathing, eyeball compression, the Valsalva maneuver, and active standing. Sympathetic function was represented by low-frequency (LF) HRV, blood pressure responses to active standing, the Valsalva maneuver, sustained handgrip, and the cold pressor test through hand immersion in ice water.
The challenge maneuver tests were abandoned if the patients were unable to perform them because of facial weakness (the Valsalva maneuver), lower-limb weakness (active standing), or distal hand weakness (handgrip).
Statistical analysis
The statistical package SPSS was used for statistical analysis. The distributions of all continuous variables were checked using the Kolmogorov–Smirnov normality test. Continuous variables with normal distributions were expressed as the mean ± standard deviation (SD) and were compared using the Student t test. Continuous variables with non-normal distributions were expressed as the median and the interquartile range and were compared using the Mann–Whitney U test. For categorical variables, the chi-square test was used. A p value of < 0.05 was considered statistically significant.
Results
Clinical characteristics of the patients
Ten GBS patients (six men) and ten gender- and age-matched healthy controls were recruited. Nine patients had GBS and one had a variant of GBS, Miller Fisher syndrome (MFS). The mean age was 40.1 ± 13.9 years (range 21–66 years). None of the patients had a prior history of cardiac arrhythmias, diabetes mellitus/impaired glucose tolerance, or were on any adrenergic medications that would affect the autonomic nervous system. Table 1 describes the baseline clinical characteristics and laboratory features of the GBS patients. The mean MRC and disability scores at the time of assessment were 51.0 ± 7.3 and 3.1 ± 1.2, respectively. No patients required intensive care unit admission or mechanical ventilation at presentation or nadir. At disease nadir, the mean MRC and disability scores were 49.6 ± 7.2 and 3.4 ± 1.0, respectively. Electrodiagnosis of the GBS patients indicated that four were axonal, one was AIDP, two were unclassified, and three were normal (Table 2). SSR were absent in five patients (three axonal, one AIDP, and one unclassified patient), and three of those five were older than 50 years old (Table 1). Based on routine bedside monitoring, including ECG recording and BP/HR measurements, no patients displayed overt clinical autonomic dysfunction (i.e., BP fluctuations, sustained tachycardia, tachy–brady arrhythmias, or gastrointestinal or urinary symptoms). All patients were either still in the progressive phase or had reached the neurological nadir (mean = 14.2 ± 9.9 days) when the AFTs were performed. Three cases (patients 4, 5, and 10) presented early with a confirmed diagnosis, so the AFTs were also performed early in these patients (within 5–6 days after onset). The tests were performed promptly after the diagnosis was made and before the initiation of treatment. There was no delay in providing treatment (intravenous immunoglobulin/plasma exchange) to patients.
Autonomic function tests
The results of formal autonomic function testing are shown in Table 3. Ten healthy controls—six men and four women—aged 39.9 ± 14.5 years (range 21–66 years) were studied for comparison. There were no significant differences between the patient and control groups in age and gender distribution. Because some of the patients had motor disability and facial weakness, the complete battery of AFTs could not be effectively applied to every patient. Active standing could not be performed by five patients, the Valsalva maneuver by three patients, and sustained handgrip by one patient.
Resting heart rate variability
All patients had a normal respiratory rate at rest before the test (range: 14–20 breaths per minute) (Table 1). In the time-domain analysis of HRV, AVNN (p = 0.003) and SDNN (p = 0.019) were reduced in GBS patients when compared with controls. In the frequency-domain analysis, low-frequency HRV (p = 0.027), high-frequency HRV (p = 0.008), and the total power spectral density of HRV (p = 0.015) were significantly reduced in GBS patients compared to controls. The three patients who presented early showed a significantly lower AVNN (p = 0.003) and HF-RRI (p = 0.011) when compared with the controls in a subgroup analysis.
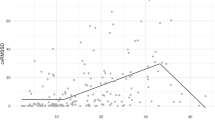
Resting baroreflex sensitivity
Up slope (p = 0.034), down slope (p = 0.011), and total slope (p = 0.024) BRS were significantly lower in the GBS group compared with controls. The three patients who presented early also showed a significantly lower down slope (p = 0.011) and total slope (p = 0.025) BRS when compared to controls in a subgroup analysis.
The HRV and BRS of each patient were analyzed (Table 4) and compared to published normal ranges [26,27,28]. Nine patients were found to have abnormal HRV and seven patients had abnormal BRS. The up slope BRS for patient 7 was undetectable because there were no effective upward ramps.
Challenge tests
Among the challenge AFTs, only the cold pressor test showed statistically significant differences between the groups, with a lower rise in diastolic BP in the GBS group compared to the controls (p = 0.008). Other challenge AFTs (deep breathing, eyeball compression, active standing, the Valsalva maneuver, and sustained handgrip) did not show any significant differences between the groups. However, when individual cases were compared to published normal values, all of the GBS patients (regardless of the electrodiagnosis) showed abnormal responses in some or all of the tests. The CPT was further analyzed in comparison to HRV and BRS using a 2 × 2 “paired contingency” table to evaluate the sensitivity of each test. Generally, the sensitivity of the CPT ranged between 71.4 and 85.7% across all parameters (HRV, BRS) when detecting autonomic dysfunction in GBS (Table 5).
Of the five patients who were able to perform active standing, four had orthostatic hypotension based on the consensus [24]. All four patients showed significant drops in diastolic BP, while one patient presented a significant drop in systolic BP. However, there was no significant difference in mean systolic or diastolic BP drop when compared to control subjects (AS-dSBP: p = 0.717; AS-dDBP: p = 0.996). The difference was marginally significant for heart rate response to active standing (AS-30:15 ratio: p = 0.055) when compared to control subjects. Studies involving a larger sample are warranted to reveal more significant differences.
One patient showed abnormal sensitivity to eyeball pressure compression, with a RRI of 1700 ms and a minimum HR response of 35 bpm (data not shown). However, the HR normalized spontaneously within 1.7 s. No patient developed serious bradyarrhythmias or required administration of atropine or cardiopulmonary resuscitation during the eyeball pressure compression procedure. None of the GBS patients and control subjects developed complications from eyeball compression following the procedure or during subsequent follow-up.
Discussion
There were significant differences in autonomic function between the GBS patients and the control group when using the cold pressor test and in HRV and BRS. No significant differences between the two groups were detected when the other autonomic challenge maneuvers were used. Both parasympathetic and sympathetic function were found to be impaired in our GBS patients based on HRV assessment. We have therefore demonstrated that subclinical autonomic dysfunction can be detected using the cold pressor test, spectral analysis of HRV, and BRS using the sequence method. The HRV and BRS differences were evident even when we performed a subgroup analysis of the patients that presented early (within a week). This implies that subclinical autonomic dysfunction is present at the early stage of the disease, not just at nadir.
Due to the disabilities of the GBS patients, active challenge maneuvers could not always be performed. Eyeball compression and cold pressor tests were included in the study as they are easily administered and do not rely on patient effort. No significant differences were found in HR response with the eyeball compression test between the GBS patients and control group. This contrasts with the results of the study performed by Flachenecker et al. [23], in which 30% (4/13) of the patients with GBS had vagal overreactivity. One possible reason for this discrepancy is the lower disability score in our cohort. This may suggest that muscle power is a potential surrogate for overt autonomic dysfunction in GBS patients. In contrast, the results of the cold pressor test were significantly abnormal in our cohort. This may suggest that the peripheral sensory nerves were preferentially affected at the time of disease presentation compared to the trigeminal nerves. Studies to investigate this further which also incorporate an assessment of trigeminal nerves and peripheral sensory nerves are warranted.
We also detected a higher proportion of GBS patients (50%) with abnormalities in SSR compared to previous studies (17.0–37.5%) [21, 29, 30]. SSR can be absent in individuals over the age of 60 years [31]; however, only one patient was over the age of 60 years in the current series, suggesting that the abnormal SSRs were likely related to disease. All five patients with abnormal SSRs showed abnormal responses to the cold pressor test. Three patients with normal NCS also showed normal SSRs. However, these patients had autonomic dysfunction according to cardiovascular autonomic function tests. This suggests that the SSR may be insensitive to subclinical autonomic dysfunction in GBS. Our study also showed that all the subtypes of GBS were equally affected in terms of sympathetic and parasympathetic function. This contrasts with a report by Asahina et al. in which they state that AIDP patients show hyperactivity of the cardiosympathetic system and acute motor axonal neuropathy (AMAN) patients have normal cardiovascular autonomic function [32]. However, autopsy reports have provided evidence of inflammatory demyelination of myelinated fibers and degeneration of axons and unmyelinated fibers in the efferent and afferent fibers of the sympathetic and parasympathetic nervous systems [33].
Autonomic dysfunction may present in various ways in GBS patients, including as cardiac arrhythmias, BP fluctuations, sweating disturbances, or genitourinary/gastrointestinal dysfunction [33, 34]. In a GBS patient, both sympathetic and parasympathetic failure can occur along with sympathetic or parasympathetic overactivity [35]. Anandan et al. found that diarrhea and constipation are the most common autonomic symptoms in GBS patients, affecting 15% of the patient population. Urinary retention and bradycardia were found in less than 5% of patients [36].
Bedside clinical signs of autonomic dysfunction such as sustained tachycardia/bradycardia and fluctuating BP are crude and likely to underestimate autonomic dysfunction compared to a quantitative autonomic function examination, especially in cases of mild GBS. Pfeiffer et al. reported that fluctuations in BP can be a sensitive marker of dysautonomia in GBS [37]. However, the authors studied a cohort of patients with severe GBS, as all the patients were mechanically ventilated in the ICU. The traditional clinical autonomic laboratory evaluation of autonomic function involves the assessment of BP and HR changes in response to a series of physical maneuvers, such as active standing, the Valsalva maneuver, and sustained handgrip [8]. This battery of tests requires patient cooperation and thus has poor reproducibility and may be insensitive to small but important changes in autonomic function. As a result, they have limited utility among special patient populations such as young children, the elderly, and those with neurological weakness and cognitive impairment. Fagius et al. subsequently described the cold pressor test, which is a passive assessment of sympathetic function requiring minimal patient cooperation [25]. Newer, more sensitive measures of autonomic function based on spontaneous variations in HR and BP (computation-dependent tests, i.e., HRV and BRS) are now available but remain primarily research tools [11, 14]. HRV and BRS analyses are noninvasive and easily applicable, requiring no active motor tasks, and are therefore feasible, even in severely affected patients. By using quantitative tests of autonomic function, a considerably higher proportion of patients with subclinical involvement of both parasympathetic and sympathetic nervous system disorders can be detected [38].
In the frequency-domain analysis of HRV, the decreases in LF-RRI and HF-RRI as well as total PSD found in this study indicate the involvement of both the parasympathetic and sympathetic nervous systems in GBS. The spectral analysis of HRV in GBS patients has been studied previously. Similar to the current study, Flachenecker et al. [39] found a reduction in HF-RRI, whereas Yerdelen et al. [40] detected reductions in LF-RRI, HF-RRI, and total PSD. They concluded that autonomic dysfunction in GBS involves both the sympathetic and parasympathetic nervous systems. Consistent with this finding, there was also a reduction in BRS in GBS patients, as demonstrated by the significantly lower up slope, down slope, and total slope BRS at rest in this study. One other study has investigated the BRS in GBS patients [41]. The authors found abnormal BRS in four of the seven patients tested. Variation in BP is transmitted by arterial baroreceptors that cause reflex changes in HR and vascular resistance which maintain the BP within the normal range. In GBS, disruption of the sympathetic and parasympathetic nerve fibers along the reflex arc may result in a reduction in BRS. Hence, reduced baroreceptor reflex sensitivity is a marker of autonomic dysfunction in GBS.
In the current study, we found that only one challenge test gave significantly different results in GBS patients compared to healthy controls. GBS patients have motor weakness, so there are a limited number of challenge tests that can be reliably performed [34, 38]. This includes BP and HR changes upon the sustained handgrip and Valsalva maneuver. However, the BP response to the cold pressor test, which assesses sympathetic activity, was significantly lower in GBS patients when compared to controls. The sensitivity of the cold pressor test in detecting autonomic dysfunction ranged between 70 and 85%. Although the HR responses to deep breathing (I-E difference), Valsalva maneuver (Valsalva ratio), and active standing (30:15 ratio) were also decreased in GBS patients in comparison to healthy controls, the differences were not statistically significant. This might be explained, at least in part, by the limited sensitivity and reproducibility of these tests [42].
The main limitation of this study is the small number of patients recruited, as this was a pilot study. As such, we acknowledge that the small sample does not allow solid conclusions to be drawn based on the statistics. The severity of GBS in our cohort was relatively mild, as none of the patients required intensive care admission or mechanical ventilation. This may have impacted our results, as typically between 25% and 44% of GBS patients have been reported to require mechanical ventilation [43]. Although no patients were ventilated, seven of the ten patients were significantly disabled and could not ambulate independently. One of the key findings of this study is the fact that we were able to demonstrate the presence of autonomic dysfunction even in patients who did not have respiratory failure. Some challenge AFTs were limited by the motor deficit of the GBS patients, thus reducing the number of patients available for comparison. Nevertheless, we were still able to demonstrate significant differences in autonomic function between the GBS patients and the healthy controls. The results of this study are consistent with the findings of Flachenecker et al. [44]. Those authors state that serious bradyarrhythmias have long been thought to occur only in severely disabled patients—mainly in those who need mechanical ventilation. These complications may also develop in less severely affected patients who have never needed artificial ventilation, and even in those who were still able to walk more than 5 m [44]. A prospective study evaluating functional outcomes based on autonomic dysfunction detected at baseline is underway. While it is possible that the reductions in HRV and BRS could have occurred due to physical deconditioning, our baseline assessments were conducted as close to the time of diagnosis as possible to avoid this.
In conclusion, our study demonstrated that there is subclinical cardiovascular autonomic dysfunction in GBS patients which would otherwise be undetected on routine bedside testing. Our findings suggest that both computation-dependent tests (HRV and BRS) detected autonomic dysfunction in GBS patients, including patients with mild disease. In contrast, the cold pressor test was the only reliable challenge test, making it potentially useful as a bedside measure of autonomic function in GBS patients. Early recognition of patients with autonomic dysfunction would improve risk stratification to prevent early complications. Future studies utilizing larger cohorts with different GBS subtypes will help to identify the extent of autonomic involvement and its relationship with the underlying GBS pathophysiology.
References
Ropper AH (1992) The Guillain-Barré syndrome. N Eng J Med 326:1130–1136
Alshekhlee A, Hussain Z, Sultan B, Katirji B (2008) Guillain-Barré syndrome: incidence and mortality rates in US hospitals. Neurology 70:1608–1613
Lawn ND, Wijdicks EF (1999) Fatal Guillain-Barré syndrome. Neurology 52:635–638
van den Berg B, Bunschoten C, van Doorn PA, Jacobs BC (2013) Mortality in Guillain-Barré syndrome. Neurology 80:1650–1654
Netto AB, Taly AB, Kulkarni GB, Rao UG, Rao S (2011) Mortality in mechanically ventilated patients of Guillain-Barré syndrome. Ann Indian Acad Neurol 14:262–266
Ishaque T, Islam MB, Ara G, Endtz HP, Mohammad QD, Jacobs BC et al (2017) High mortality from Guillain-Barré syndrome in Bangladesh. J Peripher Nerv Syst 22(2):121–126
Flachenecker P (2007) Autonomic dysfunction in Guillain-Barré syndrome and multiple sclerosis. J Neurol 254:II96–II101
Ewing DJ, Clarke BF (1982) Diagnosis and management of diabetic autonomic neuropathy. Br Med J (Clin Res Ed) 285(6346):916–918
Winer JB, Hughes RA (1988) Identification of patients at risk of arrhythmia in the Guillain-Barré syndrome. Q J Med 68:735–739
Wong AHY, Umapathi T, Shahrizaila N et al (2014) The value of comparing mortality of Guillain-Barré syndrome across different regions. J Neuro Sci 344:60–62
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology (1996) Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation 93:1043–1065
Barret KE, Scott Boitano SMB, Brooks HL (2009) Ganong’s review of medical physiology. McGraw-Hill Medical, London
Steptoe A, Vogele C (1990) Cardiac baroreflex function during postural change assessed using non-invasive spontaneous sequence analysis in young men. Cardiovasc Res 24:627–632
Parati G, Di Rienzo M, Bertinieri G, Pomidossi G, Casadei R, Groppelli A et al (1988) Evaluation of the baroreceptor-heart rate reflex by 24-hour intra-arterial blood pressure monitoring in humans. Hypertension 12:214–222
Asbury AK, Cornblath DR (1990) Assessment of current diagnostic criteria for Guillain-Barré syndrome. Ann Neurol 27(suppl):21–24
Kleyweg RP, van der Meché FG, Schmitz PI (1991) Interobserver agreement in the assessment of muscle strength and functional abilities in Guillain-Barré syndrome. Muscle Nerve 14:1103–1109
Plasma Exchange/Sandoglobulin Guillain-Barré Syndrome Trial Group (1997) Randomized trial of plasma exchange, intravenous immunoglobulin, and combined treatments in Guillain-Barré syndrome. Lancet 349(9047):225–230
Shahrizaila N, Goh KJ, Kokubun N, Abdullah S, Yuki N (2011) Serial nerve conduction studies provide insight into the pathophysiology of Guillain-Barré and Fisher syndromes. J Neurol Sci 309:26–30
Ho TW, Mishu B, Li CY, Gao CY, Cornblath DR, Griffin JW et al (1995) Guillain-Barré syndrome in northern China: relationship to Campylobacter jejuni infection and anti-glycolipid antibodies. Brain 118:597–605
Hadden RDM, Cornblath DR, Hughes RAC, Zilasek J, Hartung HP, Toyka KV et al (1998) Electrophysiological classification of Guillain-Barré syndrome: clinical associations and outcome. Ann Neurol 44:780–788
Shahani BT, Day TJ, Cros D, Khalil N, Kneebone CS (1990) RR interval variation and the sympathetic skin response in the assessment of autonomic function in peripheral neuropathy. Arch Neurol 47:659–664
Wieling W (1992) Non-invasive continuous recording of heart rate and blood pressure in the evaluation of neurocardiovascular control. In: Bannister R, Mathias CJ (eds) Autonomic failure. A textbook of clinical disorders of the autonomic nervous system, 3rd edn. Oxford University Press, New York, pp 291–311
Flachenecker P, Mullges W, Wermuth P, Hartung HP, Reiners K (1996) Eyeball pressure testing in the evaluation of serious bradyarrhythmias in Guillain-Barré syndrome. Neurology 47:102–108
Freeman R, Wieling W, Axelrod FB et al (2011) Consensus statement on the definition of orthostatic hypotension, neutrally mediated syncope and the postural tachycardia syndrome. Clin Auton Res 21:69–72
Fagius J, Karhuvaara S, Sundlöf G (1989) The cold pressor test: effects on sympathetic nerve activity in human muscle and skin nerve fascicles. Acta Physiol Scand 137(3):325–334
Nunan D, Sandercock GRH, Brodie DA (2010) A quantitative systemic review of normal values for short-term heart rate variability in healthy adults. Pacing Clin Electrophysiol 33:1407–1417
Agelink MW, Malessa R, Baumann B, Majewski T, Akila F, Zeit T et al (2001) Standardized tests of heart rate variability: normal ranges obtained from 309 healthy humans, and effects of age, gender, and heart rate. Clin Auton Res 11:99–108
Kardos A, Watterich G, de Menezes R, Csanády M, Casadei B, Rudas L (2001) Determinants of spontaneous baroreflex sensitivity in a healthy working population. Hypertension 37:911–916
Ropper H, Wijdicks EFM, Shahani BT (1990) Electrodiagnostic abnormalities in 113 consecutive patients with Guillain-Barré syndrome. Arch Neurol 47:881–887
Taly AB, Arunodaya GR, Rao S (1995) Sympathetic skin response in Guillain-Barré syndrome. Clin Auton Res 5:215–220
Drory VE, Korczyn AD (1993) Sympathetic skin response: age effect. Neurology 43:1818–1820
Asahina M, Kuwabara S, Suzuki A, Hattori T (2002) Autonomic function in demyelinating and axonal subtypes of Guillain-Barré syndrome. Acta Neurol Scand 105:44–50
Zochodne DW (1994) Autonomic involvement in Guillain-Barré syndrome: a review. Muscle Nerve 17:1145–1155
Hund EF, Schuchardt V, Ropper AH (1994) Acute inflammatory polyneuropathy (Guillain-Barré syndrome). In: Hacke W (ed) Neurocritical care. Springer, Berlin, pp 774–787
Arnason BG, Soliven B (1993) Acute inflammatory demyelinating polyradiculoneuropathy. In: Dyck PJ, Thomas PK, Griffin JW et al (eds) Peripheral neuropathy, 3rd edn. WB Saunders, Philadelphia, pp 1437–1497
Anandan C, Khuder SA, Koffman BM (2017) Prevalence of autonomic dysfunction in hospitalized patients with Guillain-Barré syndrome. Muscle Nerve 56:331–333
Pfeiffer G, Schiller B, Kruse J, Netzer J (1999) Indicator of dysautonomia in severe Guillain-Barré syndrome. J Neurol 246:1015–1022
Flachenecker P, Wermuth P, Hartung HP, Reiners K (1997) Quantitative assessment of cardiovascular autonomic function in Guillain-Barré syndrome. Ann Neurol 42:171–179
Flachenecker P, Hartung HP, Reiners K (1997) Power spectrum analysis of heart rate variability in Guillain-Barré syndrome. A longitudinal study. Brain 120:1885–1894
Yerdelen D, Erol T, Karatas M (2010) Selective autonomic screening in Guillain-Barré syndrome. Neurol India 58:398–402
Tuck RR, McLeod JG (1981) Autonomic dysfunction in Guillain-Barré syndrome. J Neurol Neurosurg Psychiatry 44:983–990
Therapeutics and Technology Assessment Subcommittee (1996) Clinical autonomic testing report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 46:873–880
Harms M (2011) Inpatient management of Guillain-Barré syndrome. Neurohospitalist 1(2):78–84
Flachenecker P, Lem K, Müllges W, Reiners K (2000) Detection of serious bradyarrhythmias in Guillain-Barré syndrome: sensitivity and specificity of the 24-hour heart rate power spectrum. Clin Auton Res 10:185–191
Funding
This study was funded by a grant from the University of Malaya (Project no. BK074-2017).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tan, CY., Shahrizaila, N., Yeoh, KY. et al. Heart rate variability and baroreflex sensitivity abnormalities in Guillain–Barré syndrome: a pilot study. Clin Auton Res 29, 339–348 (2019). https://doi.org/10.1007/s10286-018-0525-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-018-0525-z