Abstract
Purpose
Urban, minority communities are disproportionately affected by the chronic diseases associated with autonomic neuropathy; however validated measures of autonomic symptoms have not been studied in these complex populations. We sought to validate the Autonomic Symptom Profile (ASP) in a low income, medically complex, urban patient population.
Methods
Ninety-seven adults were recruited from the outpatient neurology clinic of an academic medical center serving the East Harlem neighborhood of New York City. Participants completed the ASP, and underwent a comprehensive neurologic examination, and a standardized battery of autonomic function tests (quantitative sweat testing, heart rate response to deep breathing (HRDB), Valsalva maneuver, and tilt table). Burden of chronic disease was summarized using the Charlson co-morbidity index (CCI), and detailed medication history was obtained.
Results
The ASP displayed good internal consistency (Cronbach’s α = .88), even among lower literacy participants. In univariate analyses, the ASP was correlated with HRDB (r = −.301, p = .002), a marker of cardiac autonomic neuropathy, with the CCI (r = .37, p < .001), and with use of medications with autonomic effects [t(95) = −2.13, p = .036]. However, in multivariate analysis, only the CCI remained significant.
Conclusions
In this urban, predominantly minority patient population, the symptoms captured by the ASP were more closely associated with burden of medical disease than with autonomic dysfunction. Due to this lack of specificity, it is essential that results from autonomic questionnaires be interpreted in the context of the neurologic history and exam, burden of co-morbid illness and medications, and most importantly autonomic function tests.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autonomic dysfunction frequently accompanies common medical illnesses. For example, it is estimated that milder forms autonomic neuropathy may affect as many as 90 % of some diabetic populations and 61 % of people living with HIV [1, 2]. Quantifying autonomic symptoms and distinguishing them from symptoms of medical illness is a challenge. The Autonomic Symptom Profile (ASP) quantifies autonomic symptoms in nine domains (orthostatic intolerance, reflex syncope, vasomotor, secretomotor, gastrointestinal, urinary, male sexual function, pupillomotor, sleep) [3]. Its validity was established based on its correlation with the results of autonomic function tests summarized as the Composite Autonomic Severity Score (CASS) in patients with autonomic failure, peripheral neuropathy, and normal controls [4]. However studies in more diverse patient populations, and in diseases that cause milder autonomic dysfunction (e.g., diabetes and Sjogren syndrome) have not consistently shown a correlation between the ASP and autonomic function tests [5, 6]. Furthermore, the ASP has been correlated with symptom scales designed for other diseases, such as Sjogren syndrome and fibromyalgia, suggesting that in medically complex populations, particularly those without overt neurologic disease, autonomic symptoms may be difficult to isolate from symptoms of other disorders [7, 8].
In the study described herein, we sought to validate the ASP in a diverse, low income, medically complex, urban, general neurology population, with the rationale that: (1) such populations have a high prevalence of medical illnesses linked to autonomic neuropathy (e.g., diabetes and HIV), and so a valid autonomic questionnaire would be useful, and (2) the ASP has not previously been validated in such a population [9, 10]. We foresaw two potential challenges to the use of the ASP in this setting. First, low income populations may have an overrepresentation of members with low literacy who may experience difficulty interpreting lengthy questionnaires. Second, medical disease typically causes milder autonomic dysfunction, and is often accompanied by non-specific systemic symptoms, which may impede attempts to isolate and quantify autonomic symptoms.
Methods
Design and recruitment
This was a cross-sectional study in which we sought to validate the ASP by correlating it with the results of autonomic testing summarized as the Composite Autonomic Severity Score (CASS). Participants were recruited from the outpatient general neurology clinics of an urban academic medical center in the East Harlem neighborhood of New York City. Patients who expressed willingness to meet with study staff when asked by their neurologist, were screened consecutively. The clinics serve a predominantly minority (African-American and Hispanic/Latino), low income, urban population. Inclusion criteria were: 18 years of age or greater, English speaking, and able to tolerate the autonomic testing (e.g., able to stand, able to perform Valsalva maneuver). Exclusion criteria were conditions for which the Valsalva maneuver is relatively contraindicated: untreated proliferative diabetic retinopathy, uncontrolled glaucoma, aortic stenosis, myocardial infarction in the last 6 months, other retinopathy, or unclipped cerebral aneurysm. All procedures were performed according to a protocol approved by the Icahn School of Medicine at Mount Sinai Institutional Review Board, and are in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participants provided written informed consent.
Study procedures
Neurological diagnoses and medical co-morbidity were collected via participant self-report and review of the electronic medical record (EMR). The Charlson co-morbidity index (CCI), a validated predictor of burden of illness and 5-year mortality, was calculated using these data [11]. The CCI assigns points for the following conditions: myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic obstructive pulmonary disease (COPD), connective tissue disease, peptic ulcer disease, diabetes mellitus, chronic kidney disease, hemiplegia, leukemia, malignant lymphoma, solid tumor, liver disease, and HIV/AIDS. Comprehensive medication use data, with particular attention to medications with the potential to affect the autonomic nervous system (ANS), referred to hereafter as “ANS-relevant medications,” was collected by reviewing the EMR. An inventory of ANS-relevant medications is maintained for this purpose and includes (but is not limited to): all anti-hypertensives (e.g., alpha-blockers, beta-blockers, diuretics); sympathomimetics and levodopa; medications with vasodilatory properties (e.g., nitrates, sildenafil); and medications with anticholinergic properties (e.g., antidepressants). In addition, the Anticholinergic Risk Score (ARS), a validated measure of anticholinergic side effects of medications, was also calculated for each participant [12].
The reading recognition subtest of the Wide Range Achievement Test—3rd Edition (WRAT-3) was administered in order to assess literacy in English [13]. The ASP was administered to all participants by the same investigator, who read the questions aloud and recorded the participant’s response. The participant was free to read along in the ASP and to ask questions. A standardized neurologic examination including the motor portion (part 3) of the United Parkinson’s Disease Rating Scale (UPDRS), and the walking subscale of the Amyotrophic Lateral Sclerosis Severity Scale (Hillel scale) was performed [14, 15].
Prior to autonomic testing, participants were provided with standardized instructions which included refraining from use of caffeine, nicotine, and medications with significant anticholinergic side effects on the day of testing, maintaining normal hydration, and avoiding consumption of a large meal within 3 h of testing. Autonomic function was assessed using a standardized battery of four tests (WR Medical Electronics): quantitative sweat testing (QSweat), heart rate response to deep breathing (HRDB), Valsalva maneuver (VM), and tilt table testing. QSweat is a commercially available version of quantitative sudomotor axon reflex testing (QSART) which involves measurement of sweat volume evoked by iontophoresis of acetyl choline into the skin. Following the QSweat, a non-invasive continuous beat-to-beat blood pressure monitoring device is attached to the participant’s finger (Nexfin system; www.bmeye.com) and a 3-lead surface electrocardiogram is attached to the chest in order to record continuous blood pressure (BP) and heart rate (HR). To assess HRDB, the participant takes eight slow deep breaths in rhythm with a visual cue, and the average change in HR from peak inspiration to expiration is calculated for the 5 consecutive cycles of breath which yield the largest average change. The participant then performs a standardized VM (forced exhalation to a pressure of 40 mmHg for 15 s). The maximum HR during the VM is divided by the minimum HR after the VM to obtain the Valsalva ratio. In addition, the morphology of the continuous BP curve during and immediately after the VM is analyzed according to the criteria set forth in the CASS. The final test is head up tilt (HUT). Prior to HUT 5 min of baseline HR and BP is recorded to ensure stability of values, the participant is then tilted to the upright position for 10 min as tolerated. The results of these tests are used to calculate the CASS [4].
Statistical analysis
Categorical variables were summarized using frequency and proportion, whereas continuous variables were summarized using mean and standard deviation if normally distributed, and using median and interquartile range otherwise. The internal consistency of the ASP was assessed using Cronbach’s α. The construct validity of the ASP was examined by Spearman’s rank correlation of the resultant score with the results of the autonomic function testing, including the individual tests and the summary score (CASS). Multivariate linear regression and independent samples t-tests were used to study relationships between the ASP and other factors (e.g., burden of medical disease and neurological examination findings). All statistical tests were two-tailed and conducted at the α = 0.05 level using SPSS version 22.
Results
Sample characteristics
Participants (N = 97) were predominantly ethnic minority (African-American and Hispanic/Latino), with a fairly equal distribution of men and women (see Table 1). The mean age was 47 (SD = 12) years. Eighteen percent of participants reported that English was not their first language, however all participants demonstrated adequate English fluency for consent and completion of questionnaires in English. The sample had low-average literacy with a mean standardized WRAT reading score of 90 (SD = 16.2; range = 45–116), which corresponds to a mid-high school grade level. The mean educational attainment was 11.8 (SD = 2.3) years. A variety of neurologic disorders were represented including: headache disorders (35 %), back/neck pain with or without radiculopathy (27 %), neuropathies (20 %), epilepsy (18 %), dizziness and vertigo (12 %), cerebrovascular disease (8 %), other chronic pain syndromes (7 %), movement disorders (4 %), neuromuscular disorders other than neuropathy (3 %), cognitive impairment/dementia (3 %), multiple sclerosis (2 %), and traumatic brain injury (2 %). In keeping with the nature of the neurologic disorders represented, the overall level of physical disability due to neurologic disease was relatively low: 97 % of participants had a UPDRS motor score of less than 15 (a score which correlates with complete independence in activities of daily living) [16], and only 33 % of participants had an abnormal Hillel scale. The majority of participants (62 %) had one or more co-morbid illnesses, the most common of which were liver disease (e.g., Hepatitis C), pulmonary disease (e.g., asthma and chronic obstructive pulmonary disease), and diabetes (see Table 1). The CCI ranged from 0 to 7, with a mean of 1.29 (SD = 1.4). For reference, a CCI of 0 indicates a 98.3 % chance of 10-year survival, 1 corresponds to 95.9 %, 2 corresponds to 90.2 %, and 7 corresponds to 0.01 %. In keeping with the high prevalence of medical illness, only two patients reported taking no daily medications. Regarding ANS-relevant medications, antihypertensives were the most common (32 %), followed by neuropsychiatric medications with anticholinergic side effects such as antidepressants and antiepileptics (31 %). Other medications used by smaller numbers of participants (10 % total) included antihistimines, meclizine, and nitrates all of which were used on an as needed basis only. One patient was prescribed tamulosin.
Results of autonomic testing
Abnormalities on autonomic testing were common, with 49 % of participants having an abnormal CASS (≥3). All autonomic dysfunction was in the mild to moderate range (CASS = 3–6) [6]. With regard to the CASS sub-scores, the sudomotor sub-score was most commonly abnormal with 76 % of participants assigned a non-zero score (representing at least one abnormality on QSweat), followed by adrenergic (65 %), and lastly cardiovagal (30 %) sub-scores. Four percent of participants demonstrated orthostatic hypotension on HUT, 22 % had abnormal HRDB, and 27 % had abnormal Valsalva ratios.
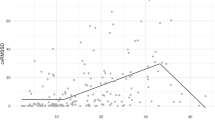
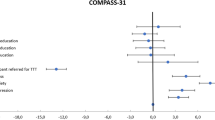
Assessment of the ASP
The ASP had good internal consistency (Cronbach’s α = .88). Analysis of a subset of 33 participants who read at an 8th grade level or below, revealed no significant difference in internal consistency compared to the sample as a whole (Cronbach’s α = .86). The ASP was not significantly correlated with the overall summary score derived from the autonomic testing (CASS). When the tests that contribute to the CASS (Valsalva maneuver, HRDB, tilt table and QSweat) were examined individually, lower (i.e., poorer) HRDB, a marker of cardiac autonomic neuropathy, was correlated with greater autonomic symptomatology on the ASP (r = −.301, p = .002), but the other measures were not. With regard to neurologic examination findings, the ASP was correlated with the Hillel scale (r = −.20, p = .05), but not with the UPDRS (r = −.10, p = .32). With regard to medical co-morbidity and ANS-relevant medications, the ASP was associated with greater burden of medical illness as measured by the CCI (r = .37, p < .001) and there was a trend for higher ASP scores with higher cholinergic burden of medication as measured by the ARS (r = .194, p = .057). The mean ASP was also found to be significantly higher in participants who were taking one or more ANS-relevant medications [31.0 vs. 22.7; t(95) = −2.13, p = .036].
When HRDB, the Hillel scale, ANS-relevant medication use, and the CCI were entered into a linear regression model with ASP as the outcome variable, only the CCI remained significant (standardized Β = .31, p = .002). To determine if particular co-morbidities were responsible for this association, we examined the three most common co-morbidities (diabetes, liver disease and pulmonary disease) independently. Mean ASP scores were higher in participants with each of these co-morbidities, [diabetes (35.4 vs. 25.0), t(95) = −2.3, p = .03; pulmonary (35.2 vs. 25.0), t(95) = −2.3, p = .02]; liver [32.1 vs. 26.1, t(95) = −1.3, p = .20] although the difference was not statistically significant in the case of liver disease.
Discussion
We undertook the present study with the objective of validating the Autonomic Symptom Profile (ASP) in a medically complex, low income, population of patients attending an urban neurology clinic. We demonstrated that the ASP was internally consistent, even in lower literacy participants, and was associated with one of the tests of autonomic function (HRDB), although not with the composite measure of autonomic function (CASS). However, the ASP was most strongly associated with burden of co-morbid chronic disease, and in univariate analysis, also showed an association with ANS-relevant medication use. These findings along with those of previous authors, [7, 8] suggest that measures of autonomic symptoms are likely to be most specific in patients with greater neurologic and lesser medical burden of disease. This does not appear to be a flaw in the ASP, which has sound psychometric properties, but rather a difficulty inherent to the study of autonomic disorders. An important limitation of this study is that all participants were recruited from the neurology clinics of a single academic medical center, which may limit generalizability, and so further research in other settings may be informative.
We conclude that due to the lack of specificity of autonomic-type symptoms in medically complicated populations, investigators and clinicians must exercise caution when attempting to measure such symptoms in these patients. It is essential that results from autonomic questionnaires such as the ASP be interpreted in the context of the neurologic history and exam, burden of co-morbid illness and medications. Most importantly, autonomic function tests, which may be quantified by standardized scores such as the CASS, can provide objective evidence of autonomic dysfunction and so may be preferred to symptom-based measures such as the ASP.
References
Kennedy WR, Navarro X, Sutherland DE (1995) Neuropathy profile of diabetic patients in a pancreas transplantation program. Neurology 45(4):773–780
Robinson-Papp J, Sharma S, Simpson DM, Morgello S (2013) Autonomic dysfunction is common in HIV and associated with distal symmetric polyneuropathy. J Neurovirol 19(2):172–180
Suarez GA, Opfer-Gehrking TL, Offord KP, Atkinson EJ, O’Brien PC, Low PA (1999) The Autonomic Symptom Profile: a new instrument to assess autonomic symptoms. Neurology 52(3):523–528
Low PA (1993) Composite autonomic scoring scale for laboratory quantification of generalized autonomic failure. Mayo Clin Proc 68(8):748–752
Cai FZ, Lester S, Lu T et al (2008) Mild autonomic dysfunction in primary Sjogren’s syndrome: a controlled study. Arthritis Res Ther 10(2):R31
Low PA, Benrud-Larson LM, Sletten DM, Opfer-Gehrking TL, Weigand SD, O’Brien PC, Suarez GA, Dyck PJ (2004) Autonomic symptoms and diabetic neuropathy: a population-based study. Diabetes Care 27(12):2942–2947
Newton JL, Frith J, Powell D et al (2012) Autonomic symptoms are common and are associated with overall symptom burden and disease activity in primary Sjogren’s syndrome. Ann Rheum Dis 71(12):1973–1979
Solano C, Martinez A, Becerril L et al (2009) Autonomic dysfunction in fibromyalgia assessed by the composite autonomic symptoms scale (COMPASS). J Clin Rheumatol 15(4):172–176
Carter JS, Pugh JA, Monterrosa A (1996) Non-insulin-dependent diabetes mellitus in minorities in the United States. Ann Intern Med 125(3):221–232
Centers for Disease Control and Prevention. HIV/AIDS surveillance report (2014) http://www.cdc.gov/hiv/topics/surveillance/resources/reports/. Accessed 7 2016
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Rudolph JL, Salow MJ, Angelini MC, McGlinchey RE (2008) The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med 168(5):508–513
Wilkinson G (1993) Wide range achievement test, 3rd ed. administration manual. Delaware: Wide Range Inc., 1993
Fahn S, Elton RL, UPDRS program members. Unified Parkinsons Disease Rating Scale. In: Fahn S, Marsden CD, Goldstein M, Calne DB, eds. Recent developments in Parkinsons Disease. Vol 2. Florham Park, NJ: Macmillan Healthcare Information; 1987:153-153-163
Hillel AD, Miller RM, Yorkston K, McDonald E, Norris FH, Konikow N (1989) Amyotrophic lateral sclerosis severity scale. Neuroepidemiology 8(3):142–150
Shulman LM, Gruber-Baldini AL, Anderson KE, Fishman PS, Reich SG, Weiner WJ (2010) The clinically important difference on the Unified Parkinson’s Disease Rating Scale. Arch Neurol 67(1):64–70
Acknowledgments
The authors thank Dr. Phillip Low, MD and the faculty and staff of the autonomic laboratory at the Mayo Clinic in Rochester, MN for providing the Autonomic Symptom Profile and instruction on its use.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This work was supported in part by a grant from the National Institute of Neurologic Disorders and Stroke (K23 NS066789, PI: Robinson-Papp). The authors have no relevant conflicts of interest to report.
Ethical standards
All procedures were performed according to a protocol approved by the Icahn School of Medicine at Mount Sinai Institutional Review Board, and are in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participants provided written informed consent.
Rights and permissions
About this article
Cite this article
Robinson-Papp, J., Sharma, S.K., George, M.C. et al. Assessment of autonomic symptoms in a medically complex, urban patient population. Clin Auton Res 27, 25–29 (2017). https://doi.org/10.1007/s10286-016-0384-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-016-0384-4