Abstract
Justificative
The relationship between post-exercise heart-rate recovery (HRR) and resting cardiac autonomic modulation is an incompletely explored issue.
Objective
To correlate HRR with resting supine and orthostatic autonomic status.
Method
HRR at the 1st, 3th, and 5th min following maximal treadmill exercise were correlated with 5-min time-domain (CV, pNN50 and rMSSD) and frequency-domain (TP, LF, HF, LFn, HFn, and LF/HF ratio) indices of heart-rate variability (HRV) in both supine and standing positions in 31 healthy physically active non-athletes men. Statistical analysis employed non-parametric tests with two-tailed p value set at 5 %.
Results
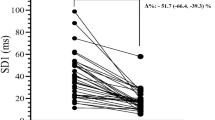
Absolute HRR and Δ %HRR at each post-exercise time did not correlated with HRV in supine position, as well as at 1st min in standing position. At the 3rd min and 5th min, these measures negatively correlated with pNN50, rMSSD, TP, and HF indices, and only in the 5th min, they showed negative correlation with HFn and positive correlation with LF, LFn, and LF/HF ratio in the standing position. Coefficient of HRR (CHRR) at the 1st min negatively correlated with pNN50 and rMSSD and at 3rd and 5th min showed positive correlation with LFn and LF/HF ratio in supine position. With HRV indices in standing position CHRR from the 1st to 5th min showed the same respective negative and positive correlations as the other measures.
Conclusion
HRR from the 1st to 5th min post-exercise negatively correlated with parasympathetic modulation in resting orthostatic, but showed no correlation in supine position. At the 3rd and 5th min, a positive correlation with combined sympathetic-parasympathetic modulation in both positions was observed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Post-exercise heart-rate recovery (HRR) has recently been considered to be a powerful and independent predictor of risk for cardiovascular morbidity and mortality [1, 2]. The short-term post-exercise cardiovascular adaptation is associated with simultaneous rapid increase in parasympathetic and a progressive decrease in sympathetic activity [3, 4]. It is reasonable to expect that these autonomic changes are dependent on the resting autonomic status and that the adaptive heart-rate changes to exercise-induced stress reflect this steady-state autonomic condition.
Time- and frequency-domain analyses of spontaneous heart-rate variability (HRV) based on R–R interval series are a reliable and feasible non-invasive tool for the evaluation of cardiac autonomic modulation in different functional conditions [5–7], which allows indirectly to infer about the parasympathetic and sympatho-vagal balance influence on the sinus node [8–10].
Several studies have examined the relationship between HRR and autonomic modulation by means of HRV focusing the evaluation of HRV only in the resting supine or seat positions prior and after exercise [11–15]. Others studies examined this relationship considering the analysis of HRV prior to exercise only in supine position and HHR in standing position after treadmill test [16–19]. Therefore, by excluding the analysis of HRV in the resting standing position, conflicting results or even erroneous interpretation of data may arise [13, 16–19], because of the discrepancy in evaluating the correlation between HRR and the resting autonomic modulation in different positions. In fact, autonomic status is distinctive in supine and standing positions and the exercise stress test is performed in the standing position with the HRR being measured in this situation [9, 10, 20]. In view that HRR is an adaptive dynamic phenomenon that is dependent on changes in autonomic modulation, it is essential to evaluate the correlation between both functional phenomena considering the different resting autonomic statuses both in the supine and standing positions.
Therefore, we aimed to verify the relationship between 5-min HRR immediately following maximal treadmill exercise stress test and the steady-state cardiac autonomic modulation evaluated by the HRV in both resting supine and standing positions in healthy individuals.
Methods
Study group and protocol
We evaluated 31 healthy physically active male non-athletes subjects aged 28.3 ± 6.4 years (range 21–46 years), with body mass index (BMI) of 24.3 ± 2.6 kg/m2 (range 19.1–29.4 kg/m2). They underwent exercise testing after breakfast, between 8:00 and 10:00 a.m., and they were previously been instructed to abstain from stimulants and alcoholic beverages, medicines, and physical activity for at least 24 h prior. This study was approved by the Ethical Committee on Human Research of the University of Brasília Faculty of Medicine and each volunteer signed an informed written consent.
First, we obtained clinical, anthropometrical and basic physiological data as well as information on lifestyle habits, after which a 12-lead electrocardiogram (ECG) was recorded in supine position, in a quite clinical laboratory room at ambient temperature (21–25 °C).
Continuous R–R interval series were recorded according to a protocol standardized in our laboratory [21]. First, a valid 5-min series was obtained following 10 min of rest in supine position. Subsequently, the subjects were asked to actively adopt the orthostatic posture at bedside, and after 2 min, an additional 5-min R–R interval series was obtained in this position. Prior to orthostatic recording, blood pressure was measured to prove the absence of significant hypotension in this position. During these recording sessions, the individuals breathed spontaneously and regularly and had their respiratory rate counted, and only those with more than 9 rpm were included in the analysis to avoid overlap of the low- and high-frequency spectral band areas.
The cardiopulmonary exercise test (CPX) was applied around 40–60 min after the R–R interval series recording sessions. This was a time previously taken for each new calibration of the O2 and CO2 analysis system according to manufacturer’s recommendations, and instruction of volunteers on how to perform the CPX.
Heart-rate variability analysis
R–R interval series were obtained by the model RS800CX Polar cardiac monitor® at a sampling frequency of 1000 Hz as previously described [21–23]. Then, each series was transferred to a microcomputer for offline data processing and analysis of R–R intervals variability, employing a software (ECGLAB) developed using the MATLAB version 5.3 platform and validated in our laboratory [21–23].
Before analysis of HRV, each R–R interval series was visually verified on a beat-to-beat basis for the validation of sinus rhythm and identification of non-sinus and ectopic beats, artifacts, and reliability of signals. Spurious and eventual outlier beats were occasional and were deleted from the series without adding new intervals. Qualified R–R interval series were highly steady and stationary as estimated by the percent differences of the means and the standard deviations between three divided segments of the series. Variability of R–R intervals series was analyzed in time and frequency domains by means of different established standard indices [5–7, 21–23].
Time-domain indices measured were: (a) mean R–R interval of the series; (b) two indices reflecting the overall autonomic modulation—standard deviation (SDNN) and coefficient of variation (CV: SDNN/mean); (c) percentage of sequential adjacent R–R intervals greater than 50 ms (pNN50) and square root of mean of the square of successive adjacent R–R intervals differences (rMSSD), which reflect the parasympathetic modulation associated with respiratory sinus arrhythmia.
For the frequency-domain analysis, the segments were filtered by the Hanning windowing and then processed by the autoregressive modeling of 16 fixed order for the conversion of the signal-oscillating components into power spectrum, which comprises a very low-frequency (VLF; 0–0.04 Hz), a low-frequency (LF; 0.04–0.15 Hz), and a high-frequency (HF; 0.15–0.50 Hz) spectral bands. Frequency-domain indices calculated included: (a) total power spectral area (0–0.50 Hz) (TP), which indicates the overall autonomic modulation; (b) absolute power areas of low- (LF) and high-frequency (HF) bands; (c) normalized power areas of low-frequency (LFn) and high-frequency (HFn) bands, which were the percentage of absolute power area of each band in relation to the sum of both absolute areas. Low- and high-frequency bands are, respectively, surrogates of combined sympathetic plus parasympathetic and exclusive parasympathetic activities; (d) ratio of low-frequency to high-frequency absolute areas (LF/HF ratio) that estimate the sympatho-vagal balance.
Cardiopulmonary exercise test and heart-rate recovery
The maximal CPX was performed during 8–12 min on a conventional treadmill (ATL, Imbrasport, Brazil). CPX protocol started from a speed of 4 km/h and at a 2.5 % grade of slope; this grade remained fixed throughout the test, and the speed was increased gradually according to the individualized ramp protocol [24].
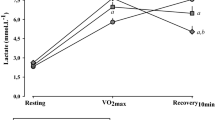
Pulmonary gas exchange was measured using the Cortex device (Biophysik, Leipzig, Germany) for the calculation of maximal oxygen uptake (VO2max) and maximal oxygen pulse defined as the ratio of VO2max by the HR peak (O2 pulse) achieved during the test [24].
Immediately after the test, volunteers were engaged in a post-exercise active cool-down at a speed reduced to 2.4 km/h and keeping of a grade of treadmill slope of 2.5 %, as described by Cole et al. [1]. This recovery cool-down procedure was employed considering their technical feasibility and reproducibility and usual application in the clinical setting.
In standing position, the HRR was obtained, in absolute and relative terms, as the HR decrement from the HR peak to the HR at 1st, 3rd, and 5th min during the 5-min period of active recovery. To normalize the post-exercise HRR for individual differences in orthostatic heart rate immediately before the exercise (HRinitial) and maximal heart rate attained during exercise (HRpeak), we created a coefficient of relative HRR (CHRR), expressed in percent terms, which describes how much the heart rate recovered in each minute after exercise towards the expected total recovery (HRpeak minus HRinitial). Thus, this coefficient is the relation of the absolute values of HRR at each minute post-exercise by the total heart-rate increment from the HRinitial to the HRpeak (chronotropic reserve), being represented by the equation \({\text{CHRR}} = \left( {{{{\text{HRR}}_{{{\text{at}}\, 1 {\text{st,}}\, 3 {\text{rd,}}\, 5 {\text{th}}\,{ \hbox{min} }}} } \mathord{\left/ {\vphantom {{{\text{HRR}}_{{{\text{at}}\, 1 {\text{st,}}\, 3 {\text{rd,}}\, 5 {\text{th}}\,{ \hbox{min} }}} } {{\text{HR}}_{\text{peak}} {-}{\text{HR}}_{\text{initial}} }}} \right. \kern-0pt} {{\text{HR}}_{\text{peak}} {-}{\text{HR}}_{\text{initial}} }}} \right) \times 100.\)
Statistical analysis
Most tested sample variables proved to be non-normally distributed by the Kolmogorov–Smirnov test. Therefore, statistical analysis uniformly employed non-parametric tests, and the variables were reported as median, quartile and extreme values.
The Wilcoxon signed-rank test was used to compare the HRV indices in supine and standing position and the Spearman’s correlation test was employed for all correlation analysis. Spearman’s correlation was also employed to test the influences of confounding variables on HRR, and the finding of a non-significant correlation resulted in no adjustment of HRR for these potentially confounding variables.
The significance level for differences and correlations was set as a two-tailed p value <0.05. Statistical analysis employed the Prism® 4 for the Windows software (GraphPad Software, Inc., USA, 2005).
Results
Baseline physiological, exercise and HRV data
The basic physiological variables were within the normal range in all subjects. Medians (extremes) of arterial blood pressure were 102/65 (82–130/50–80) mmHg in the supine position and 106/70 (82–122/50–90) mmHg in standing position (p = 0.03). HR was, respectively, 58 (43–86) bpm and 75 (53–102) bpm (p < 0.01) in supine and standing positions. Table 1 shows the functional variables before and during the exercise. The measures of HRR are shown in Table 2, where a progressive decrement of HR from the 1st to 5th min post-exercise can be observed.
In testing the influence of independent and confounding variables (age, arterial blood pressure, BMI, resting supine and orthostatic HR, peak HR during exercise, VO2 max, and O2 pulse) on HRR, only the age showed a positive correlation at post-exercise times (r s = 0.36–0.51; p ≤ 0.01–0.05). However, univariate Spearman’s correlation of age with HRV indices showed no significance in either the supine or standing positions (p = 0.06–0.98). Therefore, no confounding variable influenced the correlation between HRR and HRV indices.
Table 3 shows the HRV data in supine and standing positions. Predominant parasympathetic modulation in the supine position, and both prominent parasympathetic withdrawal and sympathetic enhancement in standing position were observed.
Heart-rate recovery and heart-rate variability correlation
In the supine position, it was only observed a positive correlation of CHRR at 3rd and 5th min with LF, LFn, and LF/HF ratio (r s = 0.30–0.34; p = 0.03–0.04).
Table 4 shows data for significant correlations between HRR measures at different post-exercise times and HRV indices in the standing position. At 1st min post-exercise, absolute HRR, and Δ %HRR showed no correlation with HRV in this position. At 3rd min, they showed negative correlation with pNN50, rMSSD, TP, and HF indices of HRV. At 5th min, also a negative correlation with pNN50 and rMSSD was observed, as well as with the HF and HFn indices. Instead, only at the 5th min, HRR measures positively correlated with LF, LFn, and LF/HF ratio. For the CHRR, at 1st min, this measure was negatively correlated with pNN50, rMSSD, and HF. At both 3rd and 5th min, CHRR also showed negative correlation with these indices and with TP and HFn and positive correlation with LFn and LF/HF indices.
Therefore, measures of HRR at 3rd and 5th min post-exercise correlated negatively with HRV indices reflecting parasympathetic (pNN50, rMSSD, HF, and HFn) and overall (TP and CV) autonomic activity in the standing position. On the other hand, these measures positively correlated with indices of combined sympathetic-parasympathetic activity (LF, LFn, and LF/HF ratio) from the 3rd to 5th min in both supine and standing positions.
Discussion
New and relevant findings were observed in our work regarding the correlation between post-exercise HRR and HRV at supine and orthostatic resting positions. However, these findings should be considered in the context of complex relationship between HRR and cardiac autonomic modulation at resting evaluated by the HRV, as well as of still conflicting comprehension about this issue [25].
In this study, we observed that correlations of absolute and relative measures of HRR and CHRR with HRV indices were dependent on time following the exercise during the 5-min period examined and on the postural position at resting.
No correlations of absolute HRR and Δ %HRR at 1st min post-exercise with HRV parameters in both postural positions were observed. This finding, in absolute terms, may simply reflect the bias of the relatively small number of individuals examined or, alternatively, to result of the peculiar state of probable yet very higher level of sympathetic activity in association with increasing parasympathetic discharge, which determines a transitory counterbalanced autonomic modulation. Although these possibilities, it may have potential relevance considering that this post-exercise timepoints is usually considered to be reference for clinical evaluation of HRR following the treadmill exercise stress test [1, 26]. On the other hand, that measures of HRR at 3rd and 5th min correlated negatively with parasympathetic and positively with sympathetic-parasympathetic combined modulation indices of HRV in the standing position. When corrected by the chronotropic reserve (CHRR), HRR also now at 1st min in addition to 3rd and 5th min post-exercise negatively correlated with parasympathetic indices, and only at the 3rd and 5th min positively correlated with combined sympathetic-parasympathetic activity, but exclusively in the standing position.
Taken together, these findings suggest that the 1st min following exercise, although established in literature as the standardized time, probably might not be the most appropriate post-exercise time for clinical practice evaluation of HRR as usually measured. Alternatively, it is possible that the HRR at this standardized time should be corrected for the chronotropic reserve as presently stated for a more precise interpretation, which might be a promising new tool for such evaluation in the clinical setting. In this context, we can also to conjecture that the 1st min may not be the ideal post-exercise time for more accurate assessment of HRR, but another time inside the 5 min or even all the 5 min following the exercise.
Therefore, as to nature of correlations between all measures of HRR and indices of HRV, we observed that the higher the parasympathetic indices in the resting standing position, the lower was the HRR at 1st, 3rd, and 5th min, and vice versa. In contrast, the higher the indices that reflects predominance of combined sympathetic–parasympathetic modulation in both resting supine and standing positions, the greater the post-exercise HRR at 3rd and 5th min post-exercise. Apparently, these correlations may seem paradoxical, considering that the post-exercise changes of HR back to baseline values are considered dependent of fast and progressive parasympathetic reactivation and simultaneous slow sympathetic withdrawal [3, 4, 8–10]. However, this may not be that simple so, and our observations can explain some controversial findings in literature regarding to the possible influence of resting cardiac autonomic modulation on post-exercise HRR in the context of the complexity of relationship between HRR and resting HRV.
As established, during the exercise, there is reciprocity between sympathetic hyperactivity and parasympathetic inhibition in the modulation of HR [27]. Following exercise, the sympathetic activity remains at a high level on the 1st min and slowly returns to the baseline level [14, 28], while the rapid restoration of parasympathetic inhibitory activity is beginning to increase [3, 4]. In consequence, hyperactivity of both autonomic branches is present during at least 1 min immediately after exercise. Indeed, when we correct the HRR in relation to baseline HR (CHRR) in standing position immediately prior to exercise, we were able to verify significant negative correlation between HRR at 1st min and parasympathetic indices of HRV at rest, but no correlation with combined sympathetic-parasympathetic indices. Therefore, our findings reinforce the idea that the parasympathetic activity is quickly increasing in the 1st min following exercise in the presence of the still high sympathetic activity at this time by upregulation and, or predominance by the orthostatism, and that the short-term HRR may be simultaneously dependent on parasympathetic reactivation and progressive sympathetic withdrawn [3, 14, 25, 29].
Another aspect to be highlighted in our work is that the correlations observed between HRR and HRV were independent of anthropometrical and physiological confounding variables, including age, BMI, resting supine and orthostatic heart rate, peak HR during exercise, and maximal VO2 and O2 pulse, considering that no correlation was observed between these variables with any of the HRR measures and HRV indices. This observation is in accordance with findings in the literature [9, 29].
The functional basis of the relationships we observed between HRR and HRV is not so easy to explain and can only be conjectured, considering the complexity of the mechanisms involved in one and other manifestation of the heart-rate dynamics. One possibility is that high parasympathetic activity level at resting prevents their full post-exercise reactivation resulting in lower HRR, consequent to exhaustion of their inhibitory capacity by the previous adaptive stimulation, and vice versa for the progressive sympathetic adaptive inhibition. This is in accordance with the concept that the higher the autonomic activity previous to an adaptive functional exigency as the exercise, the more difficult is to increase this activity (parasympathetic activation) in response to the post-exercise excitatory stimulus or more difficult is to decrease this activity (sympathetic inactivation) in response to an inhibitory stimulus [25].
Our results are in accordance with the previous studies that have also detected no relationship between HRR within 1–2 min following maximal or sub-maximal treadmill exercise and resting HRV indices in the supine position in endurance athletes [12] and in male and female non-athletes [11, 17, 18]. Twenty-four-hour HRV also did not correlate with HRR at 1–2 min in a large sample of healthy individuals of both genders [16].
On the other hand, in opposition to our observations, a positive correlation was described of post-exercise HRR at 1–3 min [14, 28] and at 4th min [18] with HRV in resting supine and seat positions, and of HRR at 3rd–4th min, but not at 5th min, with 24-h HRV analysis [16], when parasympathetic indices were considered in healthy non-athletes of broad age range. These discordant results are likely to be mainly due to, for example: (a) inappropriate statistical analysis in some works by employing parametric correlation test without normalization variables, instead of a non-parametric test, when the HRV indices are notoriously non-normally distributed; (b) distinctive age, gender, physical fitness, and functional or clinical conditions of the subjects examined; (c) non-uniformity of the exercise protocols employed; and (d) measurements of HRV made in different postural positions or even in only one position.
It is important to note in our work that the position in which the post-exercise HRR is measured is the orthostatic one, proper of the workload exercise protocol employed, and thus, the more appropriate correlation of HRR measures is with the resting HRV obtained in this position, to eliminate differences in autonomic modulation associated with distinctive positions. Considering that our results are based on the employment of the treadmill exercise stress test, they cannot rigorously be extrapolated for other workload exercises like cyclo ergometry, where the individuals are in the sitting position at the post-exercise recovery phase.
Limitations in our work include exclusion of older subjects and women of any age range, and so, the findings cannot be precisely extrapolated for these groups of peoples. In addition, we performed the evaluation of HRR during a 5-min post-exercise active cool-down phase, which should be tested for possible differences against an evaluation undertaken during a passive recovery phase and others ergometers.
In conclusion, our results suggested that HRR during the initial 1st to 5th min of the recovery period after maximal treadmill exercise is negatively correlated with the parasympathetic cardiac autonomic modulation of HRV in resting orthostatic; in the supine position, no correlation was noted. On the other hand, the measures of HRR, only at 3rd and 5th min, showed positive correlation with combined sympathetic-parasympathetic modulation in both positions. Therefore, analysis of the relationship between HRR and HRV indices should be done obtaining these indices not only in the resting supine, but also and more relevantly in the standing position. HRR in clinical setting appears to be better evaluated doing their correction for the HR prior to and in relation to maximal HR attained during it (chronotropic reserve).
References
Cole CR, Blackstone EH, Pashkow FJ, Snader CE, Lauer MS (1999) Heart-rate recovery immediately after exercise as a predictor of mortality. N Engl J Med 341:1351–1357
Okutucu S, Karakulak UN, Aytemir K, Oto A (2011) Heart rate recovery: a practical clinical indicator of abnormal cardiac autonomic function. Expert Rev Cardiovasc Ther 9:1417–1430
Goldberger JJ, Le FK, Lahiri M, Kannankeril PJ, Ng J, Kadish AH (2006) Assessment of parasympathetic reactivation after exercise. Am J Physiol Heart Circul Physiol 290:H2446–H2452
Tulppo MP, Kiviniemi AM, Hautala AJ, Kallio M, Seppanen T, Tiinanen S, Makikallio TH, Huikuri HV (2011) Sympatho-vagal interaction in the recovery phase of exercise. Clin Physiol Funct Imaging 31:272–281
Task Force (1996) Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task force of the european society of cardiology and north american society of pacing and electrophysiology. Eur Heart J 17:354–381
Pumprla J, Howorka K, Groves D, Chester M, Nolan J (2002) Functional assessment of heart rate variability: physiological basis and practical applications. Int J Cardiol 84:1–14
Kleiger RE, Stein PK, Bigger JT Jr (2005) Heart rate variability: measurement and clinical utility. Ann Noninvasive Electrocardiol 10:88–101
Lombardi F, Malliani A, Pagani M, Cerutti S (1996) Heart rate variability and its sympatho-vagal modulation. Cardiovasc Res 32:208–216
Carnethon MR, Liao D, Evans GW, Cascio WE, Chambless LE, Heiss G (2002) Correlates of the shift in heart rate variability with an active postural change in a healthy population sample: the Atherosclerosis Risk in Communities study. Am Heart J 143:808–813
Carnethon MR, Liao D, Evans GW, Cascio WE, Chambless LE, Rosamond WD, Heiss G (2002) Does the cardiac autonomic response to postural change predict incident coronary heart disease and mortality? The Atherosclerosis Risk in Communities Study. Am J Epidemiol 155:48–56
Javorka M, Zila I, Balharek T, Javorka K (2002) Heart rate recovery after exercise: relations to heart rate variability and complexity. Braz J Med Biol Res 35:991–1000
Bosquet L, Gamelin FX, Berthoin S (2007) Is aerobic endurance a determinant of cardiac autonomic regulation? Eur J Appl Physiol 100:363–369
Jae SY, Heffernan KS, Lee M, Fernhall B (2011) Relation of heart rate recovery to heart rate variability in persons with paraplegia. Clin Auton Res 21:111–116
Nunan D, Jakovljevic DG, Donovan G, Singleton LD, Sandercock GR, Brodie DA (2010) Resting autonomic modulations and the heart rate response to exercise. Clin Auton Res Off J Clin Auton Res Soc 20:213–221
Cunha FA, Midgley AW, Goncalves T, Soares PP, Farinatti P (2015) Parasympathetic reactivation after maximal CPET depends on exercise modality and resting vagal activity in healthy men. SpringerPlus 4:100
Antelmi I, Chuang EY, Grupi CJ, Latorre Mdo R, Mansur AJ (2008) Heart rate recovery after treadmill electrocardiographic exercise stress test and 24-hour heart rate variability in healthy individuals. Arq Bras Cardiol 90:380–385
Esco MR, Olson MS, Williford HN, Blessing DL, Shannon D, Grandjean P (2010) The relationship between resting heart rate variability and heart rate recovery. Clin Auton Res 20:33–38
Chen JY, Lee YL, Tsai WC, Lee CH, Chen PS, Li YH, Tsai LM, Chen JH, Lin LJ (2011) Cardiac autonomic functions derived from short-term heart rate variability recordings associated with heart rate recovery after treadmill exercise test in young individuals. Heart Vessels 26:282–288
Lee CM, Mendoza A (2012) Dissociation of heart rate variability and heart rate recovery in well-trained athletes. Eur J Appl Physiol 112:2757–2766
Grant CC, Viljoen M, Janse van Rensburg DC, Wood PS (2012) Heart rate variability assessment of the effect of physical training on autonomic cardiac control. Ann Noninvasive Electrocardiol 17:219–229
Porto LG, Junqueira LF Jr (2009) Comparison of time-domain short-term heart interval variability analysis using a wrist-worn heart rate monitor and the conventional electrocardiogram. Pacing Clin Electrophysiol 32:43–51
Carvalho JL, Rocha AF, Nascimento FAO, Souza Neto J, Junqueira LF (2002) Development of matlab software for analysis of heart rate variability. ICSP`Proceeding -6th Internacional Conference os signal Processing 2:1488–1491
Molina GE, Porto LG, Fontana KE, Junqueira LF Jr (2013) Unaltered R–R interval variability and bradycardia in cyclists as compared with non-athletes. Clin Auton Res Off J Clin Auton Res Soc 23:141–148
ACSM (2013) Guidelines for exercise testing and prescription. Lippincott, Philadelphia
Buchheit M, Papelier Y, Laursen PB, Ahmaidi S (2007) Noninvasive assessment of cardiac parasympathetic function: postexercise heart rate recovery or heart rate variability? Am J Physiol Heart Circ Physiol 293:H8–H10
Jouven X, Empana JP, Schwartz PJ, Desnos M, Courbon D, Ducimetiere P (2005) Heart-rate profile during exercise as a predictor of sudden death. N Engl J Med 352:1951–1958
Maciel BC, Gallo L Jr, Marin Neto JA, Lima Filho EC, Martins LE (1986) Autonomic nervous control of the heart rate during dynamic exercise in normal man. Clin Sci 71:457–460
Danieli A, Lusa L, Potocnik N, Meglic B, Grad A, Bajrovic FF (2014) Resting heart rate variability and heart rate recovery after submaximal exercise. Clin Auton Res 24:53–61
Reardon M, Malik M (1996) Changes in heart rate variability with age. Pacing Clin Electrophysiol 19:1863–1866
Acknowledgments
The authors gratefully acknowledge Miss Lúcia Kobayashi from the Exercise Physiology Laboratory of the Faculty of Health Education and Mr. Ronaldo de Andrade Rocha (in memoriam) from the Cardiovascular Laboratory of the Faculty of Medicine, both at the University of Brasilia, by their valuable technical assistance provided.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no financial or others conflicts of interest.
Rights and permissions
About this article
Cite this article
Molina, G.E., Fontana, K.E., Porto, L.G.G. et al. Post-exercise heart-rate recovery correlates to resting heart-rate variability in healthy men. Clin Auton Res 26, 415–421 (2016). https://doi.org/10.1007/s10286-016-0378-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-016-0378-2