Abstract
Purpose
To investigate patterns of change in cerebral perfusion during head-up tilt testing (HUTT) in children and young adults with autonomic dysfunction.
Methods
We utilized near-infrared spectroscopy (NIRS) to estimate bilateral cerebral perfusion patterns during HUTT in 71 adolescents and young adults with a diagnosis of autonomic dysfunction. In addition, we used transthoracic impedance to measure cardiac stroke volume and thus infer autonomic tone, heart rate, and blood pressure during the test. Cerebral blood-flow wave-patterns were then visually analyzed and associated with clinical symptoms and measures of cardiovascular and autonomic function.
Results
Visual analysis of contour changes in head NIRS values during phases of HUTT revealed variable patterns of cerebral blood flow, some specifically associated with severe symptomatology (i.e., syncope). We also observed an inequality in blood flow of the cerebral hemispheres in many patients. Finally, we observed changes in cardiac stroke volume during HUTT, as previously reported, that related to changes in head NIRS.
Conclusion
These results confirm a decrease in cerebral blood flow during HUTT as assessed by head NIRS in patients with autonomic dysfunction. Specifically, we have profiled the cerebral blood flow contours throughout the phases of HUTT, which add insight into the clinical spectrum of the disorder and may correlate with clinical severity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Orthostatic intolerance (OI) with neurocardiogenic syncope (NCS) due to autonomic dysfunction is characterized by symptoms of dizziness, weakness, blurred vision, decreased concentration, and loss of consciousness in the setting of postural changes [1–5]. The proposed mechanism is an inability to maintain adequate venous return to the heart due to venous pooling, primarily in the lower body, during upright posture [5, 6]. Decreased cardiac preload and stroke volume (SV) occurs with decreased multi-organ perfusion, including decreased brain perfusion [7]. Investigation of this phenomenon has been dependent on reproducing the environment that elicits signs and symptoms of impaired organ perfusion.
With the advent of formal head-up tilt testing (HUTT) [8], both physiologists and clinicians realized that many of the clinical manifestations in neurocardiogenic syncope were indicative of ischemia to multiple organ systems. Most investigators have assumed a lack of blood flow to the brain as the basis for the neurologic clinical manifestations [1, 4, 9]. Methods to quantitate cerebral blood flow, such as transcranial Doppler ultrasonography (TCD) and near-infrared spectroscopy (NIRS), have demonstrated that disturbances in brain function are in fact due to decreased perfusion from impaired cerebral blood flow [10, 11].
Decreases in cerebral blood flow have been reported during HUTT in patients with neurocardiogenic syncope using both TCD and NIRS [12, 13]. Transcranial Doppler ultrasonography has been utilized to quantify the changes in blood flow during different phases of the HUTT, namely, the dynamic, static, and post-tilt phases [12, 14]. There has been increasing experience with NIRS as a method of measuring cerebral blood flow since NIRS has the advantage of being less affected by patient movement and has a more robust reproducibility [15, 16]. The objective of this study was to perform an initial assessment of wave-patterns of cerebral blood-flow (via head NIRS) during the three phases of HUTT correlated to clinical severity.
Materials and methods
At our Dysautonomia Center at The University of Texas, Houston, we have investigated children and adolescents with symptoms of OI utilizing HUTT and continuous measurement of cardiac SV, systolic and diastolic blood pressure (BP), and heart rate (HR). Patients were referred to our center for neurologic or cardiologic consultation with complaints of syncope and/or presyncope. Additional, posturally related symptoms included palpitations, abdominal, back and leg pain, chronic fatigue, acrodysesthesias, headaches, and seizures.
From July 2009 to January 2012, we studied 235 patients with neurocardiogenic symptoms and positive HUTT as demonstrated utilizing the Task Force® monitor (Austria) to assess the autonomic input on heart rate and blood pressure. The sympathetic and parasympathetic tones were calculated by Fourier mathematical analysis of heart rate and diastolic BP variability by software installed on the Task Force® machine. We enhanced our evaluation with the utilization of head NIRS to estimate cerebral perfusion analysis. Of our initial 235 patients, 125 patients underwent cerebral perfusion analysis by head NIRS using a Nonin® monitor (Minneapolis); however, many of these patients only had unilateral NIRS analysis. Thus, 71 consecutive patients (53 female) aged 14–22 years, with bilateral head NIRS were included in this study and those without bilateral head NIRS were excluded. In our cohort, 60 of these 71 patients (85 %) were diagnosed with postural orthostatic tachycardia (POTS) and the remainder had either orthostatic hypotension or neurocardiogenic syncope. This retrospective study was approved by the Institutional Review Board at The University of Texas at Houston and was therefore performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
HUTT protocol
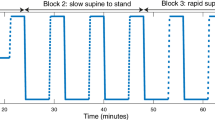
Our HUTT protocol consisted of the application of adhesive electrodes for electrocardiography and transthoracic impedance, as well as bilateral forehead electrodes for head NIRS of each cerebral hemisphere. Following electrode placement and connection to respective Task Force® (Austria) and Nonin® (Minneapolis) monitors, baseline data were collected in the supine position for 10 min. Patients were then tilted upright to an angle of 70° for a period not exceeding 30 min while being observed for hypotension, tachycardia, bradycardia, and changes in neurologic status or other associated signs or symptoms such as sweating, pallor, cyanosis, tingling of the extremities, headaches, nausea, abdominal pain, chest pain, shortness of breath, hot or cold “flashes,” or visual disturbances. Patient manifestations were recorded in a timely manner on the monitor for further analysis. The trends of continuous HR, BP, SV, and sympathetic and parasympathetic tone were recorded and observed during the three phases of HUTT [12, 14]. The test was aborted in patients with severe symptoms such as syncope, significant bradycardia, hypotension, vomiting, change in mental status, or on request of the patient due to inability to tolerate the test. Otherwise, the test continued for the duration of the 30 min, and the patient was slowly returned to the supine position (over 15 s) with continued monitoring of the study parameters and symptoms for a further 10 min.
Wave-pattern analysis
PDF graphs of cerebral NIRS values during HUTT were generated for each patient. These data were analyzed by visualization of contour changes in head NIRS values as graphed patterns during specific phases of the HUTT, allowing for group categorization. We used phases described by previous investigators as dynamic (D) tilt phase (early in the tilt test), as static (S) phase (during the tilt test), and as post-tilt (P) phase (on being returned to the supine position) [12, 14]. During each of these phases, we observed the recurrence of particular patterns similar enough to allow for the formation of specific wave-pattern categories. During the dynamic phase (D): no change (D0), gradual decline (D1), and a steep decremental pattern (D2). During the static phase (S): constant (S1), constant until a steep decline (S2), gradual decrement (S3), gradual decrement until a steep decline (S4), mostly constant with waxing and waning (S5), and mostly gradual decrement with a waxing and waning pattern (S6). During the post-tilt phase (P): mild (P1), moderate (P2), and prominent pattern (P3). Cerebral blood flow in both hemispheres was compared using the head NIRS values for each patient during HUTT by visual analysis. Asymmetry was determined to exist in cases where there was an NIRS value difference of five points or more between the hemispheres. The time to onset of intolerance of HUTT was the period in minutes, up to 30, that the patient could endure HUTT before the onset of clinical manifestations that either caused the patient to discontinue the test or compromised patient safety (i.e., syncope or asystole). Stroke volume (SV) was measured with Task Force® (Austria) monitoring with average values assessed during the baseline phase, tilting phase, and post-tilting phase.
Statistical analysis
Although this study is predominantly descriptive in nature, secondary statistical analyses were performed. These included using ANOVA (with post hoc Tukey test) to compare the mean stroke volume across the different wave-patterns within a specific HUTT phase. Additionally, NIRS from both the right and left cerebral hemispheres from patients were identified as having the same or different wave-patterns on the two sides. Chi-square tests were used to compare evidence of equality in the two hemispheres by the type of wave pattern. Any reperfusion that was evident in the post-tilt phase was compared to the NIRS value before the start of the tilt to calculate the magnitude of the reperfusion. ANOVA and t tests were used to compare this magnitude to different waveforms in the dynamic and static phases and to hemispheric inequality, respectively. All statistical analyses were performed in STATA (v.11, College Station, TX). Statistical significance was assumed at a Type I error rate of 0.05.
Results
Evidence of autonomic dysfunction was determined by cardiovascular responses to HUTT as observed by changes in heart rate, blood pressure, and stroke volume measured by Task Force® (Austria) monitoring with evaluation of sympathetic and parasympathetic tone. Clinical manifestations varied from mild symptoms permitting completion of tilt testing to severe complaints leading to cessation of HUTT. Such manifestations included abdominal pain, acrodysesthesias, arrhythmias, seizures, headaches, palpitations, nausea, vomiting, presyncope, and syncope. All patients were diagnosed with dysautonomia based upon the presence of the symptoms mentioned above in association with significant changes in HR (>30 beats above baseline), SBP (decrease more than 20 % of baseline), and/or SV (decrease >30 % of baseline) during HUTT. Actual values recorded from six patients during HUTT (Fig. 1) and schematic representations of values (Fig. 2) are demonstrated. Results are summarized in Table 1.
Cerebral NIRS waveforms in six patients A–F. a baseline, b onset of tilt, c end of tilt; rSO2 regional oxygen saturation (NIRS value). A With onset of tilt, there is a gradual decrement of the cerebral NIRS value with return to baseline after repositioning to supine. B Mild initial drop in cerebral NIRS with steep decline leading to cessation of the test, and after repositioning to supine, there is an overshoot of the pre-test baseline level. Of note, this patient fainted during HUTT. C After no significant change in NIRS during initial 11 min of HUTT, there is a steep decline associated with cessation of the test and, after repositioning, a return to baseline value. D An initial decline in cerebral NIRS, with further decline at 20 min, and a waxing and waning quality before return to baseline after completing HUTT and repositioning to supine. E Waxing and waning quality during entire HUTT. F A gradual decrement in cerebral NIRS during the head-up phase of HUTT, then a gradual return of NIRS to slightly lower than baseline value
Schematic representation of cerebral NIRS waveforms observed during the three phases of HUTT (dynamic, static, and post-tilt). A Dynamic phase: no decrement (D0); gradual decrement (D1); steep decline (D2). B Static phase: waveform with a constant value (S1); waveform with a constant value until a steep decline at the onset of severe symptoms (S2); waveform with a gradual decrement (S3); waveform with a gradual decrement until a steep decline at the onset of severe symptoms (S4); waveform with mostly a constant value with waxing and waning (S5); and waveform with mostly a gradual decrement with waxing and waning (S6). C Post-tilt phase: gradual decrement during HUTT with a return to baseline value when returned to the supine position (P1); steep decline from pre-tilt baseline during HUTT with an increase upon return to the supine position back to pre-tilt baseline value (P2); steep decline from pre-tilt baseline during HUTT with an increase upon return to the supine position above the pre-tilt baseline value (P3)
Dynamic phase (Fig. 2A)
The changes in NIRS during the dynamic tilt phase were compiled and categorized into one of three groups (Fig. 2A): no change (D0), gradual decrement (D1), or a steep decline (D2). During the dynamic phase of the study, five patients (7 %) showed no decrement (D0 waveform) during the initiation of HUTT; 39 of the 71 patients (55 %) had a gradual decrement (D1) in their head NIRS values; and 27 (38 %) had a steep decline (D2). Baseline stroke volume during this phase did not correlate with contiguous changes noted in head NIRS; however, in general, there was a decrease in the SV during this phase. Although the median baseline SV was slightly higher for patients that had a D0 waveform (93 ml; IQR: 88–102 ml), compared to the median baseline SV for patients with D1 (84 ml; IQR: 65–97 ml) or D2 waveforms (70 ml; IQR: 60–92 ml), this trend was not statistically significant (p = 0.077).
Static phase (Fig. 2B)
Data obtained during the static tilt phase were categorized into one of six groups (Fig. 2B) as follows: a waveform with a constant NIRS value (S1); a waveform with a constant NIRS value until a steep decline at the onset of severe symptoms (S2); a waveform with a gradual decrement in NIRS value (S3); a waveform with a gradual decrement in NIRS value until a steep decline at the onset of severe symptoms (S4); a waveform with mostly a constant average NIRS value with both slight increments and declines along the trendline over time—referred to as “waxing and waning” (S5); and a waveform with mostly a gradual decrement in the NIRS value with waxing and waning along the overall trendline (S6).
During this phase, 19 (26.5 %) patients had an S1 waveform, 26 (36.5 %) had an S2 waveform, one (1.5 %) had an S3 waveform, 16 (22.5 %) had an S4 waveform, seven (10 %) had an S5 waveform, and two (3 %) had an S6 waveform. After the initial decline seen during the dynamic phase, SV during this phase in general did not decrease and was maintained at a relatively constant level, which was lower than the baseline value. There was no statistically significant difference in mean SV at baseline (p = 0.612), during the test (p = 0.555), or post-tilt (p = 0.370) between any of the different head NIRS waveforms.
Post-tilting phase (Fig. 2C)
Changes observed after returning to the supine position were categorized into one of three groups (Fig. 2C): mild (P1), moderate (P2), and prominent (P3). Subjects with mild (P1) NIRS changes were able to complete HUTT and, on assuming the supine position, had a return to baseline following an initial decrement in cerebral blood flow during tilt table testing. Patients with moderate (P2) scores had a steep decline during the dynamic or static phase, or both, and had an increase while supine back to the pre-tilt baseline level. A grading of prominent (P3) was applied to patients who had a steep decline in their head NIRS value from the pre-tilt baseline either during the dynamic or static phase, or both, and also had a prominent increase while supine that was above the pre-tilt baseline.
Patients were placed supine at the conclusion of the tilting portion of the study and 14 (20 %) patients showed mild reperfusion (P1), 25 (35 %) patients had moderate reperfusion (P2), and 32 (45 %) patients had prominent reperfusion (P3). Although P3 waveforms were more common with S2 (62 % of S2 patients) than with other waveforms (range 26–43 %), the difference was not statistically significant (p = 0.081). There was no direct correlation between the magnitude of overshoot during the post-tilting phase, the head NIRS, or the SV values.
Analysis of cerebral hemispheres
Head NIRS values were compared between right and left hemispheres. A significant asymmetry, defined as a difference of five points or more between the cerebral hemispheres (Fig. 3), was considered to be present in 22 of our 71 patients (31 %). This difference was present in each phase of HUTT for the 22 patients. No other objective measures were utilized. This inequality was less common among patients with a D1 waveform (20 %) as compared to patients with D0 (60 %) or D2 (52 %) waveforms (p = 0.020). During post-tilt there was a significant trend of likelihood of inequality with increasing magnitude of post-tilt cerebral reperfusion (0 %, 24 %, and 50 %, for P1, P2, and P3 waveforms, respectively; p = 0.001). However no such associations were identified between static phase waveforms and inequality between the cerebral hemispheres.
Time to onset of intolerance of HUTT (Fig. 4)
Approximately half of the patients (32/71; 45 %) completed a full 30 min of HUTT. The test was terminated in the remaining patients with a more or less uniform distribution of time to onset of intolerance (Fig. 4). Most of the patients (38/39; 98 %) that experienced early termination of the HUTT due to onset of severe symptoms had S2 and S4 waveforms. Of the 25 patients (out of 26) with S2 waveforms that had early termination, 13 (52 %) terminated within 15 min of tilt. Thirteen out of 16 (81 %) patients with S4 waveforms terminated early; seven of these (44 %) terminated within 15 min of tilt. All of the patients with other static phase waveforms completed the full HUTT with the exception of one patient with an S1 waveform that terminated between 20 and 24 min. Of the 38 patients (out of 42 overall) with S2 or S4 waveforms who did not tolerate the HUTT, 36 (95 %) fainted. The median time to faint was 10.7 min (IQR: 6.1–19.7 min) in these patients.
Baseline stroke volume and ability to finish HUTT
Nine of 12 patients (75 %) who had a baseline SV <60 ml did not finish HUTT due to onset of severe symptoms and six of these nine (67 %) had symptoms within 10 min. In comparison, 33 of 59 patients (56 %) with a baseline SV of >60 cc had severe symptoms, and 13 of these 33 (39 %) had symptoms within 10 min (p = 0.257).
Discussion
Head-up tilt table testing has been validated as an investigational tool to evaluate NCS and signs and symptoms of OI [8]. Hypotension associated with OI leads to decreased perfusion and clinical manifestations in many organ systems [1, 4, 9, 17, 18]. Decreased organ perfusion has been most rigorously investigated in the nervous system by focusing on blood flow to the brain [10]. A decrease in cerebral blood flow has been demonstrated during HUTT in affected patients [13, 19], and this decrease in perfusion is implicated as a cause for neurologic clinical manifestations. Previously, determination of cerebral blood flow during HUTT was achieved through Doppler ultrasonography and, more recently, head NIRS has been used to estimate these changes [13, 20].
Reports have documented a change in cerebral blood flow measured by Doppler ultrasonography in patients with orthostatic hypotension during different phases of HUTT, namely, the dynamic, static, and post-tilt phases [12, 13]; however, no determination has been made regarding the specific patterns in which cerebral blood flow changes. Evaluation of cerebral blood flow changes in response to HUTT with head NIRS has provided an opportunity to further detail specific variations during this imposed orthostatic stress. We sought to categorize cerebral blood flow changes during HUTT through identification of distinct head NIRS patterns in patients with dysautonomia and NCS. We have confirmed previous reports of a decrease in cerebral blood flow during the HUTT and profiled these changes with continuous head NIRS values. We have found variations in these changes in our cohort that allow for categorization into specific groups corresponding to the quality of head NIRS changes during each phase of HUTT. Studies have shown that cerebral hypoperfusion may be associated with differing vascular mechanisms responsible for hypotension [21]. We consider that the presence of these sub-categories may also signify distinct pathologic variations in patients with OI. Furthermore, these variations may correlate with severity, as certain waveforms appear more likely to be associated with severe physiological changes and clinical manifestations than do others. Additionally, patients who had more severe physiologic changes during the static phase of the HUTT were more likely to discontinue the test due to the onset of severe symptoms. The variations in physiologic changes in head NIRS values during HUTT in patients with autonomic dysfunction should stimulate discussion regarding the clinical stratification for diagnosis, management, and prognosis.
We also found a difference between the head NIRS values of the two cerebral hemispheres during the HUTT by way of visual inspection. There was an increased likelihood for this difference as the severity of post-tilt phase hyperperfusion increased. Studies have shown differences in perfusion between the cerebral hemispheres of normal patients [22] and in patients with orthostatic intolerance [23]. Thus, our findings do not necessarily point to specific pathology. However, predisposition to hemispheric asymmetry in the setting of decreased cerebral blood flow may explain hemispheric abnormalities leading to focal findings associated with orthostatic hypotension, such as hemiplegic syndromes and unilateral migraine headaches, and their frequent occurrence after hypotensive events [24].
Finally, our investigation focused on cardiac SV in order to further demonstrate central vascular responses to HUTT and correlate both intracranial (NIRS) with extracranial (SV) blood flow changes in patients with orthostatic hypotension. Studies have shown that in cases of orthostatic intolerance, peripheral blood flow changes may be mirrored in the intracranial vasculature, thus demonstrating an abnormality in the ability to maintain a relatively consistent cerebral blood flow (autoregulation) over a wide range of peripheral blood pressures [12, 25]. The assumption is that the failure of cerebral vascular autoregulation may be associated with orthostatic hypotension and result in the commonly associated neurologic manifestations [25–27]. Therefore, we sought to understand changes in SV during the HUTT in our cohort to determine any relationship to head NIRS value or clinical symptomatology. Overall, SV decreased during the time of tilting (dynamic and static phases) and increased towards baseline during the post-tilt phase. In general, there was a decrease in SV at the onset of the tilting phase and rebound towards baseline SV with conclusion of the tilting phase. This observation was similar to previous reports [28] In some patients, the post-tilt stroke volume was higher than the baseline value, but this was not specifically associated with trends seen in the head NIRS nor a predictor of clinical symptomatology. Thus, there was not a clear demonstration of a lack of cerebral vascular autoregulation in our cohort; however, the fact that the overall changes in the SV appeared similar to those observed in the head NIRS does suggest that strict maintenance of cerebral blood flow did not occur during orthostatic stress.
It is important to note that this study was an initial attempt to identify head NIRS wave-patterns that were grossly identifiable. Our aim was to describe our observation of these wave-patterns and stimulate interest in creating quantifiable parameters that can be defined objectively and applied to this diverse population. Furthermore, although we have attempted to statistically identify differences in wave-patterns by stroke volume and other factors, this study was not designed to primarily assess these associations. As such, the differences described above should be viewed as secondary (stroke volume) and post hoc (hemispheric inequality) analyses and need to be validated in future datasets. Nonetheless, we feel that a widely accepted classification of head NIRS changes during HUTT will facilitate a more precise clinical distinction of these patients and also provide a basis for uniformity in further exploration of the pathophysiology that underlies this condition.
Evaluation of cerebral blood flow changes in response to HUTT utilizing head NIRS has provided an opportunity to detail specific variations during this imposed orthostatic stress. We have shown variations in head NIRS patterns in our cohort that allow for categorization into specific groups. Two of these specific patterns were associated with the most severe symptoms during HUTT, including syncope and convulsions. The presence of these groups may underlie differences in clinical manifestations in patients with orthostatic intolerance and imply specific pathophysiologic conditions causing autonomic dysfunction.
We have also shown a difference in the head NIRS values between both hemispheres in some patients during HUTT. This difference may be exacerbated during times of orthostatic stress and may be responsible for lateralizing symptoms that may be observed in these patients, such as unilateral sensory or motor deficits, more specifically those that occur after a hypotensive event.
Finally, we have shown a change in cardiac SV that resembles the change in head NIRS during HUTT. Typically, changes in peripheral blood pressure are not reflected in cerebral blood flow due to autoregulation. Failure of this process may underlie the neurologic manifestations, and understanding this phenomenon may help to identify the pathophysiology of the distinct cerebral blood flow patterns observed in autonomic dysfunction. We believe that inclusion of head NIRS monitoring during HUTT will lead to further understanding and classification of the symptomatology in patients with autonomic dysfunction.
References
Carew S, Connor MO, Cooke J, Conway R, Sheehy C, Costelloe A et al (2009) A review of postural orthostatic tachycardia syndrome. Europace 11:18–25
Kanjwal K, Karabin B, Kanjwal Y, Grubb B (2010) Autonomic dysfunction presenting as postural orthostatic tachycardia syndrome in patients with multiple sclerosis. Int J Med 7:62–67
Kouakam C, Lacroix D, Zghal N, Logier R, Klug D, Le Franc P et al (1999) Inadequate sympathovagal balance in response to orthostatism in patients with unexplained syncope and a positive head up tilt test. Heart 82:312–318
Low PA, Opfer-Gehrking TL, Mcphee BR, Fealey RD, Benarroch EE, Willner CL et al (1995) Prospective evaluation of clinical characteristics of orthostatic hypotension. Mayo Clin Proc 70:617–622
Rowell LB (1993) Orthostatic intolerance. In: Rowell LB (ed) Human cardiovascular control, 1st edn. Oxford University Press, New York, pp 118–161
Stewart JM (2000) Autonomic nervous system dysfunction in adolescents with postural orthostatic tachycardia syndrome and chronic fatigue syndrome is characterized by attenuated vagal baroreflex and potentiated sympathetic vasomotion. Pediatr Res 48:218–226
Podoleanu C, Maggi R, Oddone D, Solano A, Donateo P, Croci F et al (2009) The hemodynamic pattern of the syndrome of delayed orthostatic hypotension. J Interv Card Electrophysiol 26:143–149
Kenny RA, Ingram A, Bayliss J, Sutton R (1986) Head-up tilt: a useful test for investigating unexplained syncope. Lancet 1:1352–1355
Stewart JM (2002) Orthostatic intolerance in pediatrics. J Pediatr 140:404–411
Van Lieshout JJ, Wieling W, Karemaker JM, Secher NH (2003) Syncope, cerebral perfusion, and oxygenation. J Appl Physiol 94:833–848
Szufladowicz E, Maniewski R, Kozluk E, Zbiec A, Nosek A, Walczak F (2004) Near-infrared spectroscopy in evaluation of cerebral oxygenation during vasovagal syncope. Physiol Meas 25:823–836
Ocon AJ, Medow MS, Taneja I, Clarke D, Stewart JM (2009) Decreased upright cerebral blood flow and cerebral autoregulation in normocapnic postural tachycardia syndrome. Am J Physiol Heart Circ Physiol 297:H664–H673
Tanaka H, Matsushima R, Tamai H, Kajimoto Y (2002) Impaired postural cerebral hemodynamics in young patients with chronic fatigue with and without orthostatic intolerance. J Pediatr 140:412–417
Ocon AJ, Messer Z, Medow MS, Stewart JM (2011) Increased pulsatile cerebral blood flow, cerebral vasodilatation, and postsyncopal headache in adolescents. J Pediatr 159:656–662
Jobsis FF (1977) Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science 198:1264–1267
Wyatt JS, Cope M, Delpy DT, Richardson CE, Edwards AD, Wray S et al (1990) Quantitation of cerebral blood volume in human infants by near-infrared spectroscopy. J Appl Physiol 68:1086–1091
Stewart JM (2013) Common syndromes of orthostatic intolerance. Pediatrics 131:968–980
Stewart JM (1998) Neurally mediated hypotension and autonomic dysfunction measured by heart rate variability during head-up tilt testing in children with chronic fatigue syndrome. Clin Auton Res 8:221–230
Naquib AN, Winch P, Ro PS, Olshove V, Tobias JD (2011) Changes in near-infrared spectroscopy and the bispectral index during tilt-table examination. Pediatr Cardiol 32:234–236
Rao RP, Danduran MJ, Dixon JE, Frommelt PC, Berger S, Zangwill SD (2010) Near infrared spectroscopy: guided tilt table testing for syncope. Pediatr Cardiol 31:674–679
Thomas KN, Galvin SD, Williams MJ, Willie CK, Ainslie PN (2010) Identical pattern of cerebral hypoperfusion during different types of syncope. J Hum Hypertens 24:458–466
Pfefferbaum A, Chanraud S, Pitel AL, Shankaranarayanan A, Alsop DC, Rohlfing T et al (2010) Volumetric cerebral perfusion imaging in healthy adults: regional distribution, laterality, and repeatability of pulsed continuous arterial spin labeling (PCASL). Psychiatry Res 182:266–273
Kamiyama Y, Fujita Y, Fuchigami T, Kamiyama H, Takahashi S, Sakatani K (2014) Asymmetric changes in cerebral blood oxygenation induced by an active standing test in children with postural tachycardia syndrome. Adv Exp Med Biol 812:271–278
Furlan JC (2011) Headache attributed to autonomic dysreflexia: an underrecognized clinical entity. Neurology 77:792–798
Zhang R, Zuckerman JH, Levine BD (1998) Deterioration of cerebral autoregulation during orthostatic stress: insights from the frequency domain. J Appl Physiol 85:1113–1122
Brothers RM, Zhang R, Wingo JE, Hubing KA, Crandall CG (2009) Effects of heat stress on dynamic cerebral autoregulation during large fluctuations in arterial blood pressure. J Appl Physiol 107:1722–1729
Lin YJ, Po HL, Hsu HY, Chung CP, Sheng WY, Hu HH (2011) Transcranial Doppler studies on cerebral autoregulation suggest prolonged cerebral vasoconstriction in a subgroup of patients with orthostatic intolerance. Ultrasound Med Biol 37:1554–1560
Wyller VB, Due R, Saul JP, Amlie JP, Thaulow E (2007) Usefulness of an abnormal cardiovascular response during low-grade head-up tilt-test for discriminating adolescents with chronic fatigue from healthy controls. Am J Cardiol 99:997–1001
Conflict of interest
On behalf of all of the authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lankford, J., Numan, M., Hashmi, S.S. et al. Cerebral blood flow during HUTT in young patients with orthostatic intolerance. Clin Auton Res 25, 277–284 (2015). https://doi.org/10.1007/s10286-015-0295-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-015-0295-9