Abstract
Objective
Daily sessions of slow-breathing (6 breaths/min) significantly reduced 24-h ambulatory blood pressure (ABP) in patients with mild hypertension and this effect persisted at least 6 months after the interruption of sessions. The sequence of changes induced by slow-breathing (SB) daily sessions on the modulation of ambulatory blood pressure, renal resistive index, heart rate variability (HRV), and baroreflex sensitivity (BRS) was thus investigated in a randomized, controlled clinical trial.
Methods
Thirty-seven patients (30–75 years, grade I essential hypertension), untreated with antihypertensive drugs, were randomized to daily sessions (30 min) of music-guided SB (<10 breaths/min) (intervention, n = 24) or simple relaxation (control, n = 13). Office and ambulatory blood pressure monitoring renal Doppler ultrasound, assessment of BRS (sequence method and spectral analysis), and HRV (spectral power in the high- and low-frequency bands) were performed at baseline, and after 1, 4, and 8 weeks. Mixed model analysis was conducted on derived variables given by the difference between each measurement and the baseline value within subjects.
Results
After 1 week, the intervention enhanced the parasympathetic modulation (high-frequency power; at least p < 0.05 vs both control and baseline) and reduced renal vascular resistance (p < 0.05 for both comparisons); after 1 month, the enhancement of BRS (p < 0.05 for both comparisons at both methods) paralleled a significant reduction in 24 h ABP (p < 0.05 for all comparisons).
Interpretation
Repeated daily session of music-guided SB increased parasympathetic modulation and decreased renal resistive index early in the study. These changes were being followed by a positive modulation of BRS and blood pressure reduction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An increase in sympathetic activity, with a possible reduction in parasympathetic tone, is present in borderline hypertension and contributes to the maintenance of sustained hypertension [1]. The reduction of breathing rate from 16 breaths/min to less than 10 breaths/min for at least 2 min enhances parasympathetic tone and/or reduces sympathetic activation [2], being and is followed by increased baroreflex sensitivity (BRS) [3, 4] and BP reduction [3, 5]. Although these changes promptly vanish after the restoration of a normal breathing rate, a reduced chemoreflex sensitivity was observed in pranayama yoga trainees who learned to breathe slowly and deeply, mobilizing in sequence the diaphragm and the lower and upper chest [6]. Electronic devices able to guide breathing rate were thus developed and tested in hypertensive patients with favourable results [7–13], and this approach is now considered among other non-pharmacologic approaches to treat hypertension [14]. However, although there is evidence to suggest that slow breathing (SB) has positive effects on the autonomic nervous system at the acute level [15], it remains unknown whether these effects are long-term when treatment is provided over a number of weeks. In a single study in which patients were assigned to SB daily sessions, this antihypertensive effect was found to cover all of the 24-h period measured by ambulatory blood pressure monitoring and to persist for at least 6 months after the termination of the sessions [13]. Therefore, the present randomized controlled study was performed to investigate whether the voluntary act of performing daily slow-breathing exercises can target the autonomic nervous system inducing chronic changes in the modulation of BP, renal resistive index (RRI), heart rate variability (HRV), and BRS in mild hypertension.
Methods
Subjects
The study protocol was approved by the Review Committee and Ethics Committee of the Azienda Ospedaliera Universitaria Careggi (Prot. n. 2009/0004365), and all subjects gave informed consent. Inclusion criteria were patients 30–75 years old with a previous diagnosis of grade I essential hypertension and not receiving antihypertensive medications [16]. Exclusion criteria included coronary heart disease, heart failure, use of beta-blockers, cerebrovascular disease, diabetes mellitus, chronic respiratory disease, pregnancy, neoplasm, altered night-time sleep pattern due to shift work, and recent weight change. Patients who regularly performed athletic activities were also excluded
Study design and protocol
The study had a controlled, parallel design with a randomization ratio of 2:1 (intervention:control) because of an expected higher drop-out rate in the intervention group. Participants in the control group (n = 15) listened to slow music to provide/encourage a period of relaxation without the the manipulation of breathing. Participants in the intervention group (n = 30) were instructed to perform daily sessions of music-guided slow (<10 breaths/min)“abdominal” breathing with a 1:2 inspiration: expiration duration ratio (pranayama yoga) as previously described [13]. Breathing technique was taught by a certified practitioner (AF) in a single 2-hour session. The session with the therapist was repeated at each follow-up visit after investigations.
None of the hypertensive participants in the study were on antihypertensive drug therapy. All subjects were instructed to repeat daily (at home) 30-min relaxation sessions in the supine position at least 3 hours after lunch and to record frequency and duration of home sessions on a diary card. Follow-up visits in laboratory were scheduled at 1, 4, and 8 week intervals. Measurements of BP and RRI, as well as assessments of HRV and BRS, were performed at baseline and at all follow-up visits. Compliance with interventions was monitored in both groups using participant diary cards.
Measured variables and autonomic assessment
Hemodynamic assessments
(a) Blood pressure and heart rate (HR) 24 h ambulatory BP was measured using validated devices (SpaceLabs 90207, Spacelabs Healthcare Co., Issaquah, WA) programmed to take measurements at 15 and 20 min intervals over the day and the night, respectively, as previously reported [13].
(b) Renal resistive index Two subgroups of subjects (10 in the intervention group and 10 in the control group, matched for age and gender) underwent assessment of RRI (at baseline and at follow-up visits) as previously reported [17]. Briefly, patients were placed in a supine position and the B-Mode and the Doppler measurements of RRI were performed using a Siemens G60S (Toshiba Aplio) machine with a 3.5-MHz sector transducer. The RRI was calculated in both kidneys according to the following formula: [(peak systolic velocity − minimum diastolic velocity)/peak systolic velocity] [17]. RRI values from the left and right sides were averaged for analysis. All measurements were taken in the late morning by the same examiner (MB).
Autonomic assessments
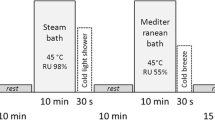
Subjects were examined in the late morning, under standardized conditions in a quiet room with at a comfortable temperature set to (25 °C). Participants were not permitted coffee or tea on the day of the study. After 30 min of quiet rest, subjects underwent continuous recordings of ECG, beat-to-beat non-invasive BP by Nexfin monitor (BMEYE B.V, Amsterdam, The Netherlands), and respiration rate during 10 min of spontaneous breathing and during 10 min of deep breathing defined as 6 cycles/min. The patient was then asked to stand up quickly within 3–4 s and ECG registration was continued over a period of 60 s. All recordings were made in a random order.
Offline, data were selected and exported on a personal computer for analysis of BRS and HRV
BRS assessments
Sequence method (time domain) The time series of RR interval and systolic BP (SBP) recorded during spontaneous breathing were scanned with software capable of identifying the sequence of at least three cardiac cycles in which both SBP and pulse interval are either steadily increasing (up) or decreasing (down); the variation threshold was fixed at 1 mmHg for SBP and 6 ms for pulse interval [18]. BRS values are expressed as combined values for up and down sequences. Separate values for up and down sequences were also calculated.
Spectral method (frequency domain) Time series of the tachogram and systogram were visually selected and used for analysis. The α-index (α) (the gain in the relationship between the RR period and SBP variability), was obtained by means of simultaneous spectral analysis of RR and SBP variability, with the calculation being made from the square root of the ratio between RR and SBP variability in the two major bands of LF (α-LF) and HF (α-HF). The values of the α-index were validated when the coherence between fluctuations in the RR interval and SBP was greater than 0.5 [19].
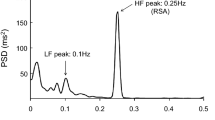
HRV assessments
HRV during inspiration and expiration (time domain) Measurements of HR response to deep breathing, the subject was placed in a seated position. Respiration rate for a period of 30 sec and baseline ECG recording were done. Then, subjects were asked to perform slow and deep inspiration followed by slow and deep expiration such that each breathing cycle lasted for 10 s, consisting of 6 breathing cycles/min. The difference between the highest HR recorded during deep inspiration and the lowest HR recorded during deep expiration was measured per cycle.
HR response to standing (time domain) For HR response to standing, an ECG was recorded in the supine position. The subject was instructed to stand up within 3 s. The ECG was continuously recorded during the procedure. The ratio between the RR interval of the 30th beat and the 15th beat (30:15 ratio) after standing was calculated. The average value of the two tests was then determined.
Spectral method (frequency domain) After 15 min of supine rest, and ECG was recorded for short-term HRV analysis following the procedures recommended by the Task Force [20]. The low-frequency and high-frequency components of HRV were assessed by frequency analysis of the sequential R wave to R intervals of the ECG obtained from short-term recordings of 5 min [20, 21]. LFRR and HFRR were expressed in normalized units, which represent the relative value of each power component in proportion to the total power minus the very low-frequency (VLF) component. The LFRR/HFRR ratio was then calculated.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD) when normally distributed. The predetermined sample size of groups was calculated for providing at least 80 % power (β) with p < 0.05 (α) based on previous results with home SBP measurements taking a 5-mmHg difference in population means with σ = 5.5 mmHg. Categorical variables were compared with Fisher’s exact test.
Factors associated with compliance to treatment with daily SB sessions (defined as subjects who completed the study in the intervention group) were preliminarily investigated by logistic regression analysis in the subgroup of subjects assigned to intervention. Age, gender, body mass index (BMI), smoking habit (yes or no), office SBP, diastolic BP (DBP), and HR were included as independent variables.
Statistical analysis was conducted on derived variables given by the difference between each measurement and the baseline values associated with each subject. A linear mixed-effect model was fitted by restricted maximum likelihood. Random effects were identified and repeated measurements were taken for these individuals, while fixed effects were specified for experimental conditions. A linear time trend was also included in the model terms. A further model was fitted allowing interaction terms between time and experimental conditions.
Multivariate linear regression was then used to identify variables independently associated with changes of 24 h SBP and RRI. The three measures of BRS sensitivity (sequence method in the time domain and α-indexes in the two major bands of LF, α-LF, and HF, α-HF) were found to be affected by serious multi-colinearity (variance inflation factor VIF >3). Independent variables included in the models were office SBP, BRS assessed by the sequence method (Seq), HRV during deep breathing (HRVdeep), HRV after standing (HRVortho), LFRR/HFRR ratio, with adjustment for age, HR, and breathing rate at rest.
Results are expressed as an odds ratio (OR) with 95 % confidence limits (95 % CI). A value of p < 0.05 was taken as the minimum level of statistical significance throughout the paper. Statistical analysis was performed using the Statistical Package for Social Science (SPSS, version 21.0, SPSS Inc., Chicago, IL) software package.
Results
From January 2009 to September 2010, 243 patients with essential hypertension were screened for enrollment in the study. From that group, 198 patients did not meet the inclusion criteria or met one or more of the exclusion criteria. Of the 30 patients assigned to the intervention SB group, 6 refused to continue the protocol and were excluded from the intervention group after their initial enrollment. Of the 15 patients assigned to the placebo SB (P-SB), two could not be reached at the time of follow-up. Therefore, 37 patients completed the protocol: 24 in the SB group and 13 in the P-SB group. Clinical characteristics were comparable between the two groups (Table 1). The main reasons for participant dropout were: family activity (n = 1), or work responsibility (n = 7). At logistic regression analysis, exclusion was not influenced by gender, age, smoking habit, baseline SBP or DBP, HR, or allocation to SB group. The 24 patients in the SB group self-reported a high compliance with daily slow-breathing treatment, with 6.6 ± 0.8 sessions of breathing exercises per week (range 5–7) during the first week of the study and 5.7 ± 0.9 sessions(range 4–7) during the last week. Diary cards revealed a similar compliance with listening to music in the control group.
Hemodynamic changes
Blood pressure Ambulatory recordings were of good technical quality in all participants. At the end of the study, the mean 24 h SBP and DBP were both significantly reduced compared to baseline values in the intervention group (120 ± 8 mmHg vs 129 ± 8; 77 ± 9 vs 82 ± 7; p < 0.001 for both). In the control group, no significant changes were observed at the 2 month follow up (128 ± 10 mmHg vs 128 ± 10; 84 ± 8 vs 85 ± 8; ns for both). A significant reduction in 24 h SBP in the intervention group was detectable at the 1-month follow-up visit (125 ± 7 mmHg; p < 0.05) (Table 2). Mixed model analysis of changes vs baseline revealed a significant time per group interaction on 24 h SBP (p < 0.01) (Fig. 1).
Changes in 24h-ambulatory systolic blood pressure (24h SBP) a baroreflex sensitivity (sequence method) b low frequency component of heart rate variability (LFRR) c renal resistive index (RRI) d 30:15 ratio of HR response to standing (ms) (HRVorto) e and high frequency component of heart rate variability (HFRR) f from baseline to the end of the study in subjects assigned to intervention (black circle n=24) and controls (empty circles n=13).
Renal resistive index At the 2-month follow-up the RRI was reduced in the intervention group (0.54 ± 0.05 vs 0.63 ± 0.05; p < 0.001). The reduction vs baseline values was already significant at the 1-week visit (0.58 ± 0.06; p < 0.05). No significant changes were observed in the control group. The effect of the intervention on RRI was confirmed by mixed model analysis (time per group interaction, p = 0.003) (Fig. 1).
Autonomic cardiovascular regulation
BRS In the intervention group BRS at the 2-month follow-up increased compared to baseline for both the sequence method (12.17 ± 3.26 vs 8.84 ± 3.34 ms/mm Hg; p < 0.001) and spectral analysis (13.94 ± 4.25 vs 9.39 ± 3.61 for α-HF and 8.46 ± 3.44 vs 5.91 ± 3.51 for α-LF; p < 0.001 for both). Mixed model analysis revealed a significant time per group interaction for all methods of assessment (p < 0.05) (Table 3).
HRV Assessment of changes in HRV performed in the time domain (during standing and during deep breathing) revealed a significant effect of intervention even at the 1-week visit (p < 0.05), with the effect of intervention progressively increasing during follow-up (p < 0.001 for time per group interaction). In the frequency domain, subjects assigned to intervention showed a significant increase of the spectral HFRR band at 1 week (p = 0.03), a response which further increased at 1 month (p < 0.001). A significant decrease of the LFRR band was observed in the intervention group at the 2-month visit (p < 0.001). Overall whole a significant reduction of the LFRR/HFRR ratio was evident at the 1-month visit (p < 0.001) with a significant time per group interaction (p < 0.001). No changes were observed in the control group. The main results are shown in the Fig. 1.
Interaction between hemodynamic and autonomic changes
At multivariate linear regression 24 h SBP changes were found to be affected by changes in BRS (sequence method, β coefficient −0.180) and sympathetic tone (LFRR/HFRR ratio, β coefficient of 0.309, p < 0.001). Changes of RRI (1 unit) were mostly affected by changes in the sympathetic tone (LFRR/HFRR ratio with β coefficient of 0.322, p < 0.001; HRV after standing, β coefficient −0.279, p < 0.001; HRV during deep breathing, β coefficient −0.251, p < 0.003) (Table 4).
Discussion
According to our findings, the voluntary act of performing daily slow-breathing exercises induce stable changes in the autonomic cardiovascular control before the reduction of ambulatory BP. More precisely, the early enhancement of parasympathetic tone at 1 week is followed by an increase of BRS at the 1-month follow-up.
The voluntary reduction of breathing rate from 16 to less than 10 acts/minute for at least 2 min is consistently followed by an acute BP reduction [3, 5] associated with BRS increase [3, 4], enhanced parasympathetic and vagal tone, and/or reduction of sympathetic activation [2, 22]. In the absence of information regarding cardiovascular autonomic changes induced by repeated slow-breathing sessions, the possibility to move SB into the clinical environment was investigated using a device that is able to guide patients in reaching a SB rate. Based on the favorable results seen in office BP measurements during pre- and post-observational studies, in prospective matched case-control studies, and in randomized control trials, the device received FDA approval as an “adjunctive treatment to reduce BP” (http://www.resperate.com) [14, 23]. However, a recent meta-analysis of eight studies [24], although confirming a decrease in office SBP of 3.1 mm Hg (95 % CI 1.4–4.7) after 8 weeks [24], showed no effects when excluding sponsored studies [24]. When considering the effects on 24 h BP, conflicting results were reported because there was either a significant reduction after 8 weeks [7, 25] or no effects after 4 [26] or 8 weeks [27] of observation. However, the duration of daily sessions adopted in all studies is less than 15 min [14, 24]. The possibility to restore the BRS [28], to increase the participation of the vagal autonomic component in cardiac control [29], and to reduce BP [28], was demonstrated for physical training, but in all these studies the duration of the training sessions was consistently longer (45–60 min) [28, 29]. The duration of a session of physical activity should last more than 30 min according to current guidelines [14], a time duration which is also utilized in regular yoga regular practice [30]. Daily sessions of 30 min voluntary SB were adopted only in a single independent, controlled, randomized study [13] where a significant reduction of 24 h SBP at the 6 months’ follow-up was detected [13]. The duration of the SB session could thus be important for inducing favorable changes in cardiovascular autonomic control in the long term. term. In contrast to previous studies performed using a device [24], we integrated listening to music with additional instructions on how to perform SB. Therefore, we cannot exclude the possibility that the additional instructions given to patient may have potentiated the simple biofeedback provided by the device adopted in other studies [24]. The possibility that music-guided SB performed without the use of the device might have an effect is of potential practical use.
According to our study, BP changes parallel the enhancement in BRS in the time domain (sequence technique) and in the frequency domain (spectral analysis). In contrast to observations with physical exercise [28, 31], the restoration of BRS was not associated with baseline reductions of HR. The increase in BRS was, however, preceded by an enhancement of HFRR power reflecting an enhancement of parasympathetic tone [20] as also observed in healthy individuals assigned to physical training [32]. The early parasympathetic response was associated with a reduction in RRI, probably mediated by the parasympathetic modulation of renal sympathetic activity [33]. The renal response is indeed unlikely due to a direct parasympathetic effect on renal blood flow autoregulation, as there are no efferent renal vasomotor fibers present in the vagus nerve [34, 35]. It is unlikely that the significant RRI reduction observed at the first follow-up visit could be a result of structural changes in the blood vessel wall during the 2-month study period. RRI changes observed in the present study may thus reflect changes in vasomotor stimuli.
The present study is the first to provide evidence of stable modifications of cardiovascular control induced by the long-term practice of SB (pranayama yoga) in hypertensive subjects. Four months of respiratory training in pranayama yoga reduced the sympathovagal balance and the LF component of HRV in healthy elderly subjects [36], indicating a positive shift towards parasympathetic predominance. The reduced sympathovagal balance may be due to a central modulator regulatory effect, with an impact on BRS in our hypertensive patients. The activation of the Hering-Breuer reflex due to an increase in tidal volume during SB [5] might have also reduced chemoreflex sensitivity, thus ameliorating baroreflex function [5, 6]. Additionally, reducing the respiratory rate to six breaths per min induces R-R interval fluctuations, which when merged with the respiratory cycle, show a considerable increase in amplitude relative to BP changes. This may also lead to enhanced baroreflex efficiency [4].
Hypertensive patients included in our study had normal absolute values of RRI, normal renal function, and no microalbuminuria. Therefore, even minor absolute RRI changes could be appreciated. It is reasonable to expect that the improvement in BRS and the reduction of renal resistance may play a protective role in hypertensive patients.
The methods of assessing sympathetic and parasympathetic modulation in the present study are indirect, using HRV and the assessment of BRS involves only noninvasive measurements. Other more direct techniques such as microneurography or pharmacological challenges were not used. Although these invasive techniques are not feasible for routine clinical measurements, they may provide greater insight into the mechanisms underlying the autonomic changes investigated in this study [15]. A further limitation of the present study is the lack of serum catecholamine measurements. The use of more direct measures should be considered in future studies.
In conclusion, the antihypertensive effects of repeated 30 min daily sessions of music guided SB are associated with favorable changes in the autonomic nervous system and a reduction of RRI. Although this treatment method is effective, its time consuming nature may limit its use in the clinical setting. However, this limitation is shared by most non-pharmacological treatment and prevention strategies, such as physical exercise.
References
Pal GK, Adithan C, Ananthanarayanan PH, Pal P, Nanda N, Thiyagarajan D, Syamsunderkiran AN, Lalitha V, Dutta TK (2013) Association of sympathovagal imbalance with cardiovascular risks in young prehypertensives. Am J Cardiol 112(11):1757–1762
Gallagher D, Terenzi T, de Meersman R (1992) Heart rate variability in smokers, sedentary and aerobically fit individuals. Clin Auton Res 2(6):383–387
Joseph CN, Porta C, Casucci G, Casiraghi N, Maffeis M, Rossi M, Bernardi L (2005) Slow breathing improves arterial baroreflex sensitivity and decreases blood pressure in essential hypertension. Hypertension 46(4):714–718
Bernardi L, Porta C, Spicuzza L, Bellwon J, Spadacini G, Frey AW, Yeung LY, Sanderson JE, Pedretti R, Tramarin R (2002) Slow breathing increases arterial baroreflex sensitivity in patients with chronic heart failure. Circulation 105(2):143–145
Bernardi L, Gabutti A, Porta C, Spicuzza L (2001) Slow breathing reduces chemoreflex response to hypoxia and hypercapnia, and increases baroreflex sensitivity. J Hypertens 19(12):2221–2229
Spicuzza L, Gabutti A, Porta C, Montano N, Bernardi L (2000) Yoga and chemoreflex response to hypoxia and hypercapnia. Lancet 356(9240):1495–1496
Rosenthal T, Alter A, Peleg E, Gavish B (2001) Device-guided breathing exercises reduce blood pressure: ambulatory and home measurements. Am J Hypertens 14(1):74–76
Grossman E, Grossman A, Schein MH, Zimlichman R, Gavish B (2001) Breathing-control lowers blood pressure. J Hum Hypertens 15(4):263–269
Schein MH, Gavish B, Herz M, Rosner-Kahana D, Naveh P, Knishkowy B, Zlotnikov E, Ben-Zvi N, Melmed RN (2001) Treating hypertension with a device that slows and regularises breathing: a randomised, double-blind controlled study. J Hum Hypertens 15(4):271–278
Viskoper R, Shapira I, Priluck R, Mindlin R, Chornia L, Laszt A, Dicker D, Gavish B, Alter A (2003) Nonpharmacologic treatment of resistant hypertensives by device-guided slow breathing exercises. Am J Hypertens 16(6):484–487
Meles E, Giannattasio C, Failla M, Gentile G, Capra A, Mancia G (2004) Nonpharmacologic treatment of hypertension by respiratory exercise in the home setting. Am J Hypertens 17(4):370–374
Elliot WJ, Izzo JL Jr, White WB, Rosing DR, Snyder CS, Alter A, Gavish B, Black HR (2004) Graded blood pressure reduction in hypertensive outpatients associated with use of a device to assist with slow breathing. J Clin Hypertens (Greenwich) 6(10):553–559
Modesti PA, Ferrari A, Bazzini C, Costanzo G, Simonetti I, Taddei S, Biggeri A, Parati G, Gensini GF, Sirigatti S (2010) Psychological predictors of the antihypertensive effects of music-guided slow breathing. J Hypertens 28(5):1097–1103
Brook RD, Appel LJ, Rubenfire M, Ogedegbe G, Bisognano JD, Elliott WJ, Fuchs FD, Hughes JW, Lackland DT, Staffileno BA, Townsend RR, Rajagopalan S, American Heart Association Professional Education Committee of the Council for High Blood Pressure Research CoC, Stroke Nursing CoE, Prevention, Council on Nutrition PA (2013) Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the american heart association. Hypertension 61(6):1360–1383
Limberg JK, Morgan BJ, Schrage WG, Dempsey JA (2013) Respiratory influences on muscle sympathetic nerve activity and vascular conductance in the steady state. Am J Physiol Heart Circ Physiol 304(12):H1615–H1623
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F (2013) 2013 ESH/ESC Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 31(7):1281–1357
Boddi M, Sacchi S, Lammel RM, Mohseni R, Serneri GG (1996) Age-related and vasomotor stimuli-induced changes in renal vascular resistance detected by Doppler ultrasound. Am J Hypertens 9(5):461–466
Parati G, Di Rienzo M, Bertinieri G, Pomidossi G, Casadei R, Groppelli A, Pedotti A, Zanchetti A, Mancia G (1988) Evaluation of the baroreceptor-heart rate reflex by 24-hour intra-arterial blood pressure monitoring in humans. Hypertension 12(2):214–222
Pagani M, Somers V, Furlan R, Dell’Orto S, Conway J, Baselli G, Cerutti S, Sleight P, Malliani A (1988) Changes in autonomic regulation induced by physical training in mild hypertension. Hypertension 12(6):600–610
Camm AJ, Malik M, Bigger JT, Breithardt G, Cerutti S, Cohen RJ, Coumel P, Fallen EL, Kennedy HL, Kleiger RE, Lombardi F, Malliani A, Moss AJ, Rottman JN, Schmidt G, Schwartz PJ, Singer DH (1996) Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Eur Heart J 17(3):354–381
Malliani A, Pagani M, Lombardi F, Cerutti S (1991) Cardiovascular neural regulation explored in the frequency domain. Circulation 84(2):482–492
Mori H, Yamamoto H, Kuwashima M, Saito S, Ukai H, Hirao K, Yamauchi M, Umemura S (2005) How does deep breathing affect office blood pressure and pulse rate? Hypertens Res 28(6):499–504
(2007) Resperate for hypertension. Med Lett Drugs Ther 49(1264):55–56
Mahtani KR, Nunan D, Heneghan CJ (2012) Device-guided breathing exercises in the control of human blood pressure: systematic review and meta-analysis. J Hypertens 30(5):852–860
Howorka K, Pumprla J, Tamm J, Schabmann A, Klomfar S, Kostineak E, Howorka N, Sovova E (2013) Effects of guided breathing on blood pressure and heart rate variability in hypertensive diabetic patients. Auton Neurosci 179(1–2):131–137
Anderson DE, McNeely JD, Windham BG (2010) Regular slow-breathing exercise effects on blood pressure and breathing patterns at rest. J Hum Hypertens 24(12):807–813
Hering D, Kucharska W, Kara T, Somers VK, Parati G, Narkiewicz K (2013) Effects of acute and long-term slow breathing exercise on muscle sympathetic nerve activity in untreated male patients with hypertension. J Hypertens 31(4):739–746
Laterza MC, de Matos LD, Trombetta IC, Braga AM, Roveda F, Alves MJ, Krieger EM, Negrao CE, Rondon MU (2007) Exercise training restores baroreflex sensitivity in never-treated hypertensive patients. Hypertension 49(6):1298–1306
Cozza IC, Di Sacco THR, Mazon JH, Salgado MCO, Dutra SGV, Cesarino EJ, Souza HCD (2012) Physical exercise improves cardiac autonomic modulation in hypertensive patients independently of angiotensin-converting enzyme inhibitor treatment. Hypertens Res 35(1):82–87
Wang J, Xiong X, Liu W (2013) Yoga for essential hypertension: a systematic review. PLoS ONE 8(10):e76357
Somers VK, Conway J, Johnston J, Sleight P (1991) Effects of endurance training on baroreflex sensitivity and blood-pressure in borderline hypertension. Lancet 337(8754):1363–1368
Sandercock GRH, Bromley PD, Brodie DA (2005) Effects of exercise on heart rate variability: inferences from meta-analysis. Med Sci Sports Exerc 37(3):433–439
Miki K, Hayashida Y, Shiraki K (1993) Cardiac-renal-neural reflex plays a major role in natriuresis induced by left atrial distension. Am J Physiol 264(2 Pt 2):R369–R375
Majid DS, Karim F (1995) Primary neural involvement in renal haemodynamic and functional responses to prolonged stimulation of atrial receptors in anaesthetized dogs. Exp Physiol 80(4):631–644
Fater DC, Schultz HD, Sundet WD, Mapes JS, Goetz KL (1982) Effects of left atrial stretch in cardiac-denervated and intact conscious dogs. Am J Physiol 242(6):H1056–H1064
Santaella DF, Devesa CR, Rojo MR, Amato MB, Drager LF, Casali KR, Montano N, Lorenzi-Filho G (2011) Yoga respiratory training improves respiratory function and cardiac sympathovagal balance in elderly subjects: a randomised controlled trial. BMJ Open 1(1):e000085
Acknowledgments
This study was supported by a grant from the University of Florence (progetti di ricerca d’ateneo ex 60 % 2010/2011), and Regione Toscana (PMI 2009 POR CReO FESR 2007–2013-linea d’intervento 1.1.c, D.D. n. 1942 del 10.04.2009).
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Modesti, P.A., Ferrari, A., Bazzini, C. et al. Time sequence of autonomic changes induced by daily slow-breathing sessions. Clin Auton Res 25, 95–104 (2015). https://doi.org/10.1007/s10286-014-0255-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-014-0255-9