Abstract
The aim of this study was to complete a full evaluation of the new EIZO RX850 liquid crystal display and compare it to two currently used medical displays in Australia (EIZO GS510 and Barco MDCG 5121). The American Association of Physicists in Medicine (AAPM) Task Group 18 Quality Control test pattern was used to assess the performance of three high-resolution primary medical displays: EIZO RX850, EIZO GS510, and Barco MDCG 5121. A Konica Minolta spectroradiometer (CS-2000) was used to assess luminance response, non-uniformity, veiling glare, and color uniformity. Qualitative evaluation of noise was also performed. Seven breast lesions were displayed on each monitor and photographed with a calibrated 5.5-MP Olympus E-1 digital SLR camera. ImageJ software was used to sample pixel information from each lesion and surrounding background to calculate their conspicuity index on each of the displays. All monitor fulfilled all AAPM acceptance criteria. The performance characteristics for EIZO RX850, Barco MDCG 5121, and EIZO GS510 respectively were as follows: maximum luminance (490, 500.5, and 413 cd/m2), minimum luminance (0.724, 1.170, and 0.92 cd/m2), contrast ratio (675:1, 428:1, 449:1), just-noticeable difference index (635, 622, 609), non-uniformity (20, 5.92, and 8.5 %), veiling glare (GR = 2465.6, 720.4, 1249.8), and color uniformity (Δu′v′ = +0.003, +0.002, +0.002). All monitors demonstrated low noise levels. The conspicuity index (χ) of the lesions was slightly higher in the EIZO RX850 display. All medical displays fulfilled AAPM performance criteria, and performance characteristics of EIZO RX850 are equal to or better than those of the Barco MDCG 5121 and EIZO GS510 displays.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The goal of medical imaging is to produce images for the purpose of screening and diagnosis of diseases. Medical imaging also plays a critical role in monitoring treatment interventions and staging of disease [1]. The ability of clinicians to recognize and discriminate abnormal features from normal areas on radiographic images depends in part on the monitor used to display the images. High quality image display is associated with more efficient search and diagnostic performance [2, 3]. Radiographic image quality is influenced by many factors along the imaging chain, from exposure parameters used for image acquisition and image receptor [4] to the monitor used to display the image, and can only be as good as the weakest link in the imaging chain [5]. In the digital era, image quality has significantly improved due to wide dynamic range of the detector, pre- and post-processing adjustment capabilities of digital systems, and improving digital display technology [6]. The monitor (display) is the last component of the imaging sequence and one of the key components that determine image quality [7]. However, even with advances in display technology, displays continue to be the weakest link in the imaging chain [5, 8].
Recent technological innovations such as direct digital radiography are aimed at maximizing the visualization of disease. However, to gain maximum benefits from these innovations, high quality image displays are needed [6, 7]. High quality displays with high luminance values, contrast ratio, resolution, and low veiling glare are particularly important in radiology where sufficient gray-level difference is required to render subtle lesions visible for interpretation. These requirements have led to replacement of cathode ray tubes (CRTs) with liquid crystal displays (LCDs) [9]. With LCDs, gray-level variation is achieved by conversion of the system’s digital driving levels (DDLs) to brightness levels that can be perceived by the average human observer. The amount of luminance change necessary to perceive difference in brightness of a target by the average human observer as change in shades of gray under a given viewing condition is known as just-noticeable difference (JND) [10, 11]. In order to standardize the appearance of medical images on displays, international standards for the calibration of monitors have been agreed. The Digital Imaging and Communication in Medicine (DICOM) Gray-scale Standard Display Function (GSDF) part 14 supports the calibration of displays to a standard mapping DDLs to JNDs [12, 13].
Monitors for primary interpretation of medical images are currently available from many manufacturers. Further to this, the American Association of Physicists in Medicine (AAPM) Task Group 18 (TG18) has detailed technical evaluations that should be carried out to assess the performance of calibrated display devices, and have set guidelines for their acceptance into clinical practice [11]. These guidelines are to ensure that images are displayed consistently for the purpose of medical decision-making and care. Monitors that do not meet these guidelines compromise image quality and reduce diagnostic performance [10]. It is therefore important that medical display devices have adequate display characteristics to show clinically relevant information and that new displays are characterized to ensure that they demonstrate performance that is at least equal to or better than currently existing displays before approval for clinical use.
The EIZO RX850 multimodality color monitor was recently introduced onto the market. Multimodality color monitors are capable of displaying monochrome and color images acquired by magnetic resonance imaging scanners, digital mammography, and ultrasound. Their color characteristics make them suitable for Doppler ultrasound and positron emission tomography/computed tomography (PET/CT) color image display and diagnosis [14]. As yet, the EIZO RX850 display has not been approved for mammography and general radiography in some countries including Australia; approval requires independent verification to ensure it is fit for purpose. To be considered fit for purpose for primary display of medical images, a monitor should have acceptable luminance, luminance ratio, and contrast conformance to the GSDF. Other requirements include high resolution, low levels of noise, veiling glare, and non-uniformity [11]. Therefore, this study aims to complete a full physical and psychophysical evaluation of the new EIZO RX850 primary medical-grade color display and to compare it to two other primary medical-grade monochrome displays currently used in Australia (EIZO GS510 and Barco MDCG 5121).
Materials and Methods
Three primary medical displays were evaluated: EIZO RX850 8-MP color display driven by an NVIDIA Quadrox FX 3450 Video Card (Beijing, China); EIZO GS510 5-MP monochrome display driven by an ATI FirePro V5800 Video Card (Sunnyvale, CA, USA); and Barco MDCG 5121 5-MP monochrome display with an ATI FirePro V5800 Video Card (Sunnyvale, CA, USA). All displays were evaluated using the American Association of Physicists in Medicine (AAPM) Task Group 18 (TG18) guidelines [11] in the Medical Image Optimisation and Perception Group (MIOPEG) laboratory of the Brain and Mind Research Centre at the University of Sydney, Australia. Prior to evaluation, the faceplates of the monitors were cleaned according to manufacturer’s recommendations, and display devices were warmed up for 30 min to allow for stabilization of their output. Manufacturers’ specifications for the displays are summarized in Table 1. Each monitor was then calibrated to DICOM GSDF part 14 [12, 13]. As EIZO RX850 and Barco MDCG5121 perform automatic self-calibration, the preset 256-point measurement was used to characterize their luminance response. However, luminance characterization of the EIZO GS510 was performed with the third party software (VeriLum® Plus Version 5.02.0006). The ambient light adjustment value for gamma LUT was 1.5 cd/m2. The number of luminance measurement for tracking was 17, and gamma correction 33. The calibration target was as follows: maximum luminance 500 cd/m2, minimum luminance 0.9 cd/m2, and DICOM GSDF part 14. The calibration software packages used compensate for additional luminance from ambient light. Thus, JND loss is distributed equally across the digital driving level (DDL) range.
Assessment of Monitors
AAPM TG18 test patterns were used for the assessment. Both qualitative and quantitative measurements were performed where necessary. All qualitative assessments were made from a distance of 30 cm. Quantitative measurement of luminance was performed using a calibrated spectroradiometer (CS-2000, Konica Minolta, Japan). All measurements were made with the front edge of the metal lens barrel at a distance of 50 cm from the display faceplate using a 0.2° aperture. For each parameter assessed, measurements were made four times and the mean value was used to represent performance of the display in terms of the parameter assessed. Although the display screen of EIZO RX850 is divided into two halves, each test pattern occupies the whole screen when activated. Therefore, the monitor was evaluated as a single screen. Quantitative measurements were made by one observer and qualitative assessments performed by two observers. Monitors were evaluated in the absence of ambient lighting at a viewing angle perpendicular to the display faceplate. Performance parameters assessed and test patterns used are described below.
Luminance and Color Uniformity
Quantitative assessment of luminance was performed using TG18-LN test patterns. Measurement of maximum luminance was made in the center of the TG18-LN-18 pattern, and minimum luminance was measured at the center of the TG18-LN-01 pattern. Measurement of maximum luminance (L max) and minimum luminance (L min) were made in the absence of ambient lighting. This enabled the calculation of contrast ratio and achievable just-noticeable difference (L max − L min). Contrast ratio was calculated as shown below:
Color uniformity was assessed by measuring the u′v′ color coordinates at the center and four corners of the TG18-UNL80 test pattern.
Non-uniformity
Non-uniformity was assessed quantitatively using TG18-ULN10 test pattern. Luminance was measured at the four corners of the test pattern and at the center, and the maximum luminance deviation (L dev.) was calculated as shown below:
Noise
Qualitative assessment of display noise was performed using TG18-AFC test pattern [11]. Pattern was examined for visibility of targets; the number of targets visible in each quadrant was quantified and percentage of targets visualized was computed.
Veiling Glare
Qualitative assessment of veiling glare was performed by counting the number of objects visible at the center of the TG18-GV and TG18-GVN test patterns. Two observers independently performed qualitative assessment of veiling glare in the absence of ambient lighting. Observers wore non-reflective clothing, and assessed the test patterns at a distance of 30 cm from the display faceplate and a viewing angles perpendicular to the display faceplate. The consensus of the two observers was used for qualitative characterization of veiling glare. To avoid the effect of bright light on the eyes, the test was repeated with the bright field around the low luminance region in the TG18-GV masked before counting the number of objects visible within the low luminance area. Quantitative measurement of veiling glare was performed using TG18-GQ, TG18-GQB, and TG18-GQN. The spectroradiometer was used to measure luminance in the dark central region of TG18-GQ (L), central white region of TG18-GQN (Lb), and at the center of TG18-GQN (Ln). These were used to calculate glare ratio as follows:
Measurement of Lesion Conspicuity Index (χ) on Monitors
To assess the impact of the monitor characteristics on the human visual system, seven mammograms with obvious solid breast lesions were displayed on each of monitor and photographed with a 5.5-MP digital SLR camera (Olympus E-1, Zuiko Digital, Japan). The lens of the camera was calibrated to obtain the best possible focus using an EC-14 teleconverter. Calibration was done at three different adjustments: 12 − 60 + 4; 50 + 7, with EC-14 + 2; and 50 − 200 + 4, with EC-14 − 2. Ambient lighting was kept constant at 20 lux. Images were acquired from a distance of 50 cm and at an angle of 90° to the display faceplate. ImageJ software (National Institute of Health) [15] was used to sample pixel information from each displayed lesion and surrounding background and to calculate the index of conspicuity (χ) of the lesions as described by Manning et al. [16]. The border of each lesion was visually determined from the image by the observer, and four profiles were taken through the center of the lesion and extended beyond its opposite corners, at least 2 cm from the edge of the lesion to sample pixel information in its immediate background. The index of conspicuity (χ) for each lesion was calculated as follows:
where
- d :
-
is the longest dimension (cm) of the lesion along the profile line
- θ :
-
the maximum slope angle to the edge of the lesion profile in degrees
- ΔGL:
-
the gray-level difference (μ lesion − μ background)
- a :
-
the standard deviation of the gray levels of the lesion
- b :
-
the standard deviation of the gray levels of the background
Analysis of variance (ANOVA) was used to assess whether there were significant differences in the conspicuity index of the lesions between the displays.
Results
The performance characteristics of the displays are shown in Table 1. EIZO RX850 demonstrated calibrated maximum luminance (490 cd/m2), contrast ratio (675:1), just-noticeable difference (635), non-uniformity (20 %), low veiling glare (glare ratio = 2465.6), color uniformity (Δu′v′ = +0.003), and low noise levels (100 % visibility of targets in quadrants). The outputs of Barco MDCG and EIZO GS510 respectively were as follows: maximum luminance (500.5 and 413 cd/m2), minimum luminance (1.170 and 0.92 cd/m2), contrast ratio (428:1 and 449:1), just-noticeable difference (622 and 609), non-uniformity (5.92 and 8.5 %), veiling glare (GR = 720.4 and 1249.8), and color uniformity (Δu′v′ +0.002 and +0.002). The displays demonstrated noise levels well below acceptable limits.
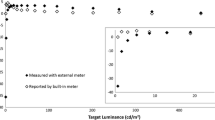
For each of the lesions assessed, the gray-level difference between the lesion and the background was slightly higher in the EIZO RX850 than in the Barco MDCG 5121 and EIZO GS510 displays. Similarly, the conspicuity index (χ) of each lesion was slightly higher in the EIZO RX850 display than in the other monitors assessed (Fig. 1). However, ANOVA showed no statistically significant differences in the conspicuity of the lesions on the three monitors (Barco MDCG 5121 vs. EIZO GS510: F = 0.008, p = 0.93; Barco MDCG 5121 vs. EIZO RX850: F = 0.017, p = 0.89; EIZO GS510 vs. EIZO RX850: F = 0.047, p = 0.83). Overall, differences in the conspicuity index of the lesions on all three monitors were non-significant (F value of 0.024, p = 0.98).
Discussion
Before new technologies are accepted into medical practice, a thorough evaluation is required to ensure that they are fit for a purpose. The current study evaluated the physical and psychophysical qualities of the new EIZO RX850 8-MP color display and compared it with EIZO GS510 and Barco MDCG 5121 5-MP displays which are currently used in Australia. The results show that all displays evaluated fulfilled the AAPM criteria (Table 2). EIZO RX850 demonstrated performance characteristics that are equal to or better than those of the EIZO GS510 and Barco MDCG 5121 monitors for the test performed. The Barco MDCG 5121 display demonstrated the highest maximum luminance; however, contrast ratio, just-noticeable-difference, and veiling glare were better in the EIZO RX850 display (Table 2). The findings also show that lesions are slightly more prominent in their background (higher index of lesion conspicuity) when displayed on EIZO RX850 than on EIZO GS510 and Barco MDCG 5121, but the differences were not statistically significant (p < 0.05).
The current study adopted quantitative approaches for luminance assessment. Although the EIZO GS510 was unable to achieve target calibration, it demonstrated a contrast ratio comparable to Barco MDCG 5121. We observed that the target maximum luminance for calibration of the EIZO GS510 display had decreased from 500 cd/m2 in 2012 to 421 cd/m2 in 2015, a 15.8 % reduction within a period of 3 years. Color displays generally demonstrate lower maximum luminance compared to monochrome due to the presence of filters that reduce backlight heating to avoid quick luminance deterioration [17]. High luminance positively impacts visual search [2]; however, optimum transfer of the visual information in a displayed image is attained when there is high difference in gray-levels within a field of view [8, 18]. High JND is associated with high gray-level difference which creates a pattern of contrast that allows distinction of lesions from their background [2].
It is imperative that the red, green, and blue (RGB) colors on monitors are adequately matched to create true chrominance for the display of grayscale or color images. Inadequate color matching will cause colors to appear differently on the display faceplate when the position of the monitor is changed [19, 20]. AAPM recommends a color uniformity (Δu′v′ ≤ +0.01) for primary displays, and all displays evaluated demonstrated a color mixture well below the limit (Table 2). Color has gained significance in medical imaging by enabling visualization of color information acquired by fusion-based modalities such as positron emission tomography/computed tomography (PET/CT). Infusion modalities use color for distinction of disease conditions, staging of cancer, and monitoring of response to therapy [14].
Although the AAPM TG-18 criteria recommend assessment of geometric distortion, it is only relevant for CRTs. In LCDs, the physical matching of pixel to their transistor and their discrete pixels offer very good resolution without geometric distortion [7]. Spatial resolution of LCDs is more appropriately related to pixel pitch rather than the Cx patterns indicated in the AAPM. The pixel pitch of all the monitors evaluated was less than or equal to 0.2 mm as specified by the manufacturers (Table 1). Therefore, geometric distortion and resolution were excluded from the evaluation of displays in the current study. Noise levels on all the monitors were low and well within acceptable limits. Also, all monitors evaluated demonstrated acceptable luminance non-uniformities. High non-uniformities cause pixel-by-pixel variations in the luminance of the display that are unrelated to patient anatomic information. Pixel variations across a display faceplate are associated with screen artifacts, perturbations, and spatial noise; these phenomena may interfere with subtle radiographic features or may be confused with clinically relevant image features [2, 18].
Another critical finding of the current study is that veiling glare is much lower in EIZO RX850 than the Barco MDCG 5121 and EIZO GS510 displays. Qualitatively, all targets on the TG18-GV test pattern were visible on the EIZO RX850 and EIZO GS510 monitors without masking, but none was visualized on the Barco MDCG 5121 monitor. Three targets became visible on Barco MDCG 5121 display when the surrounding high luminance region was masked with an opaque material. TG18-GQs allow for quantitative measurement of veiling glare, with high glare ratio indicating low veiling glare. LCDs are generally known for their low veiling glare compared to CRTs [21]. However, diffuse reflection from the display faceplate due to ambient lighting and specular reflection of light from bright objects may contribute to the measured veiling glare [21]. The glare ratio for EIZO RX580 was two and three times higher than those for EIZO GS510 and Barco MDCG 5121, respectively (Table 2), and may be due to its anti-reflective coating which reduces reflection caused by external light sources. Barco MDCG 5121 is fitted with a thick reflective protective front panel, and the reflectivity from this protective front panel may have contributed to its high veiling glare observed in the current study. This increased veiling glare is perhaps the reason why Barco released new products without the thick protective front panel. Whilst high veiling glare reduces observers’ performance [22], low glare has been shown to improve visualization of low contrast structures [10]. Assessment of veiling glare with AAPM guidelines is subject to different interpretations. Generally, masking of the high luminance region around the TG18-GV and TG18-GQ for qualitative and quantitative assessment respectively is recommended to reduce the effect of light reflection [19, 20, 23]. These recommendations were adopted in the current study; therefore, the glare ratio reported is the maximum achievable.
Clinical assessment of monitor performance is commonly done through radiologists’ subjective assessment of image quality [11]. However, subjective assessment is influenced by factors including observers’ adaptation to illumination, experience, and preference, and often causes variability in decisions on auditing [2, 3, 8]. This variability is not limited to technology assessment but also in diagnostic performance [24, 25]. To reduce subjectivity in the assessment of displays’ characteristics in clinical practice, a quantitative analysis of conspicuity index (CI) was performed. The result demonstrates that the index of conspicuity for all lesions was slightly higher in the EIZO RX850 than other monitors evaluated. However, the differences in conspicuity index between the monitors were not statistically significant (p > 0.05). CI refers to the prominence of a lesion on its background and takes into consideration the size of the lesion and the angle of the border profile to the background, as well as the complexity of the background structures when determining lesion visibility. These quantities are known to have the highest visual impact on the human visual system [16, 26].
Important differences between the 8- and 5-MP displays include that the 5-MP monitors (EIZO GS510 and Barco MDCG 5121) are monochrome and always used in pairs (side-by-side) while the 8-MP color display (EIZO RX850) is a single monitor divided into two halves. Thus, EIZO RX850 allows multiple images to be viewed side-by-side on the same monitor without an intervening bezel. It also enables multiple images of the same patient from different modalities as well as monochrome and color images to be displayed simultaneously on a single screen, thus improving work efficiency.
The study has a few limitations. First, clinical evaluation of image quality was not performed. Second, the date of manufacture of monitors differed (2014, 2012, and 2006 for EIZO RX850, Barco MDCG 5121, and EIZO GS510, respectively). However, Barco MDCG 5121 and EIZO GS510 were installed in 2012 and 2013, respectively. None of the monitors were used clinically; rather, they were used solely in the laboratory setting. The backlight hours, which included standby time, were 17,605 and 10,921 h for EIZO GS510 and Barco MDCG 5121, respectively. The time elapsed to last calibration was 2 years and 7 months for EIZO GS510 and 37 days for Barco MDGC 5121. Therefore, even though the monitors were not in regular use, the older ones may have suffered some luminance deterioration, as shown by the inability for EIZO GS510 to attain target calibration. Additionally, it would have been more reasonable to compare EIZO RX850 color display with others with comparable characteristics. A further limitation of the study is that most of the evaluation was performed by a single observer, and may be affected by subjectivity, which could lead to variability in the rating of the performance of monitors [27]. Also, although specular and diffuse reflectivity are not stated as compulsory acceptance test in the AAPM criteria, they are however relevant for viewing and should be considered in future work. Conversely, a major strength of the current study is the use of all AAPM recommended test patterns for evaluation of the displays. Additionally, luminance measurement was performed with a calibrated high-precision spectroradiometer (accuracy = ±2 %) capable of extremely low luminance measurement (0.003 cd/m2) that is independent of luminance and color space [28] and also independent of monitor manufacturers.
Conclusion
Qualitative and quantitative evaluations demonstrate that all monitors fulfill the criteria required of primary displays and that the EIZO RX850 display is equal to or better than the Barco MDCG 5121 and EIZO GS510 displays currently used for interpretation of mammographic images. Therefore, EIZO RX850 is fit for the purpose of primary display of mammography and general radiography images.
Abbreviations
- M5121:
-
Barco MDCG5121
- GS510:
-
EIZO GS510
- RX850:
-
EIZO RX850
- IPS:
-
In-plane switching
- TFT:
-
Thin-film transistor
- TFT AM LCD:
-
Thin-film transistor liquid crystal display
- CT:
-
Computed tomography
- MR:
-
Magnetic resonance
- US:
-
Ultrasound
- DR:
-
Digital radiography
- CR:
-
Computed radiography
- NM:
-
Nuclear medicine
- FDA:
-
Food and Drug Administration
- AAPM:
-
American Association of Physicists in Medicine
- TG18:
-
Task Group 18
- L max :
-
Maximum luminance
- L min :
-
Minimum luminance
- L amb :
-
Luminance in the presence of ambient lighting
- LR:
-
Luminance ratio
- CR:
-
Contrast ratio
- JND:
-
Just-noticeable difference
- GR:
-
Glare ratio
- Δu′v′:
-
Color uniformity
- L min + L amb :
-
Minimum luminance in the presence of ambient lighting
- ACR–AAPM–SIIM:
-
Technical Standard for Electronic Practice of Medical Imaging
References
Benveniste MF, Rosado-de-Christenson ML, Sabloff BS, et al: Role of imaging in the diagnosis, staging, and treatment of thymoma. Radiographics 31(7):1847–61, 2011. discussion 1861-3
Krupinski E, Roehrig H, Furukawa T: Influence of film and monitor display luminance on observer performance and visual search. Acad Radiol 6(7):411–8, 1999
Krupinski EA, Roehrig H: Pulmonary nodule detection and visual search: P45 and P104 monochrome versus color monitor displays. Acad Radiol 9(6):638–45, 2002
Ekpo EU, Hoban AC, McEntee MF: Optimisation of direct digital chest radiography using Cu filtration. Radiography 20(4):346–350, 2014
Krupinski EA, Williams MB, Andriole K, et al: Digital radiography image quality: image processing and display. J Am Coll Radiol 4(6):389–400, 2007
Samei E, Dobbins 3rd, JT, Lo JY, et al: A framework for optimising the radiographic technique in digital X-ray imaging. Radiat Prot Dosim 114:220–9, 2005
Saunders RS, Samei E, Baker J, et al: Comparison of LCD and CRT displays based on efficacy for digital mammography. Acad Radiol 13(11):1317–26, 2006
Krupinski EA, Roehrig H: The influence of a perceptually linearized display on observer performance and visual search. Acad Radiol 7(1):8–13, 2000
Badano A, Gagne RM, Jennings RJ, et al: Noise in flat-panel displays with subpixel structure. Med Phys 31(4):715–23, 2004
Lowe JM, Brennan PC, Evanoff MG, et al: Variations in performance of LCDs are still evident after DICOM gray-scale standard display calibration. AJR Am J Roentgenol 195(1):181–7, 2010
Samei E, Badano A, Chakraborty D, et al: Assessment of display performance for medical imaging systems: executive summary of AAPM TG18 report. Med Phys 32(4):1205–25, 2005
Fetterly KA, Blume HR, Flynn MJ, et al: Introduction to grayscale calibration and related aspects of medical imaging grade liquid crystal displays. J Digit Imaging 21(2):193–207, 2008
Kenneth S. Kump J.O., John French. Consistent image presentation implemented using DICOM grayscale standard display function. In: Medical Imaging. 2000. San Diego, CA: Proc. SPIE.
von Schulthess GK, Steinert HC, Hany TF: Integrated PET/CT: current applications and future directions. Radiology 238(2):405–22, 2006
Schneider CA, Rasband WS, Eliceiri KW: NIH Image to ImageJ: 25 years of image analysis. Nat Methods 9(7):671–5, 2012
Manning DJ, Ethell SC, Donovan T: Detection or decision errors? Missed lung cancer from the posteroanterior chest radiograph. Br J Radiol 77(915):231–5, 2004
Sabnis RW: Color filter technology for liquid crystal displays. Displays 20(3):119–129, 1999
Kimpe T, Xthona A, Matthijs P, et al: Solution for nonuniformities and spatial noise in medical LCD displays by using pixel-based correction. J Digit Imaging 18(3):209–18, 2005
Crespi A, Bonsignore F, et al: Acceptance tests of diagnostic displays in a PACS system according to AAPM TG18. Phys Med 22(1):17–24, 2006
Crespi A, Bonsignore F, Paruccini N, et al: Grayscale calibration and quality assurance of diagnostic monitors in a PACS system. Radiol Med 111(6):863–75, 2006
Jerrold T, Bushberg AS, Leidholdt EM, Boone JM: The essential physics of medical imaging. 3rd edition. Lippincott Williams and Wilkins, 2012
Krupinski EA, Lubin J, Roehrig H, et al: Using a human visual system model to optimize soft-copy mammography display: influence of veiling glare. Acad Radiol 13(3):289–95, 2006
Jung H, Kim HJ, Kang WS, et al: Assessment of flat panel LCD primary class display performance based on AAPM TG 18 acceptance protocol. Med Phys 31(7):2155–64, 2004
Zhao B, Tan Y, Bell DJ, et al: Exploring intra- and inter-reader variability in uni-dimensional, bi-dimensional, and volumetric measurements of solid tumors on CT scans reconstructed at different slice intervals. Eur J Radiol 82(6):959–68, 2013
Ekpo EU, McEntee MF: Measurement of breast density with digital breast tomosynthesis—a systematic review. Br J Radiol 20140460,2014
Manning D. S., Ethell Lesion conspicuity and AFROC performance in pulmonary nodule detection. Progress in Biomedical Optics and Imaging: Medical Imaging. 3(24),2002,300-311
Hartling L, Hamm M, Milne A, et al: Validity and Inter-Rater Reliability Testing of Quality Assessment Instruments. Rockville MD, 2012
Majumder A, Stevens R: Color nonuniformity in projection-based displays: analysis and solutions. IEEE Trans Vis Comput Graph 10(2):177–88, 2004
Acknowledgments
The authors of this research would like to thank Professor Patrick Brennan for providing the spectroradiometer and digital camera used for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Ekpo, E.U., McEntee, M.F. An Evaluation of Performance Characteristics of Primary Display Devices. J Digit Imaging 29, 175–182 (2016). https://doi.org/10.1007/s10278-015-9831-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10278-015-9831-3