Abstract
This study aimed to analyse the effect of root-end resection on the sealing ability of orthograde apical plugs of three root-end filling materials (MTA Repair HP, Biodentine, MTA Plus) using the bacterial leakage method and compare it with the retrograde root-end filling technique. Eighty-four extracted mandibular premolar teeth with single root and single straight canals were selected and randomly divided into two main experimental groups (n = 36) depending on the apical plug placement technique and a control: Group I: orthograde technique, followed by root-end resection; Group II: retrograde root-end filling technique; one control Group III (n = 12): obturation with gutta-percha, followed by root-end resection. Experimental groups were further subdivided into three subgroups A, B, and C (n = 12) depending on the three different root-end filling materials used. An apical plug of 3 mm thickness was obtained in both the experimental groups. The apical sealing ability was evaluated with the dual-chamber bacterial leakage method. Statistical analysis was performed using the Kaplan–Meier survival analysis test. By the end of 30 days, the occurrence of turbidity indicating bacterial leakage was 75% in MTA Repair HP, 83.3% in Biodentine, and 91.7% in MTA Plus samples. This trend of turbidity was similar in both orthograde and retrograde technique. The control group showed turbidity in all the samples (100%). More MTA Repair HP samples (25%) survived the 30 days observation period with no bacterial leakage compared to Biodentine (16.7%) and MTA Plus (8.3%). The sealing ability of already set root-end filling materials placed through the orthograde technique did not deteriorate after root-end resection. Also among three root-end filling materials, MTA Repair HP presented the lowest bacterial microleakage followed by Biodentine and MTA Plus, respectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Microorganisms, along with their secondary products, have the potential to invade through the filled canals in the tooth and are detrimental to periradicular tissue [1]. These pertinacious microorganisms are predominantly accountable for the failure of root canal treatment [2]. In such cases, periradicular surgery is considered an alternative to facilitate healing. This procedure prevents bacterial leakage and further spread of infection in the root canal using root-end filling material [3].
The periradicular surgery includes thorough surgical debridement of pathological tissue existing in the periradicular area, resection of root apex, root-end cavity preparation, and placement of filling material at the root end to seal the apical aspect of the root canals [4]. Some of the challenges with the retrograde root-end filling technique are that during apical surgery, there might be a potential problem regarding contamination of root-end preparation by blood, medicaments, or saliva, which tends to wash off the root-end filling material. Also, this may affect the ability of a material to set correctly and, more importantly, maintain an adequate seal [2]. Also, root-end cavity preparation and restoration become difficult in cases with poor accessibility. Hence, an alternate method of orthograde placing of the root-end filling material can be adapted to overcome these problems.
In the orthograde technique, the need for root-end apical preparation and filling is eliminated, which makes the procedure more practical and systematic compared to the previous methods when a definitive need for periradicular surgery emerges. The orthograde technique simplifies the process wherein the clinician may resect the end portion of the root and expose the already set material rather than placing new root-end filling material through a retrograde approach [5]. This way, root-end cavity preparation is no longer required, so the chances of microcrack formation are also less in the orthograde technique than in the retrograde root-end filling technique. Another advantage of the orthograde technique is that it needs less vasoconstrictor local anaesthetics (which terminates bleeding during surgery to make it effortless to place root-end filling material), and therefore indicated in patients with vasoconstrictors contraindication [6].
The orthograde technique is an excellent substitute for the retrograde root-end filling technique in the case of periradicular surgeries because the orthograde method is more efficient, simplified, and performed faster. However, there are some concerns, one of which is an alteration of the seal of the previously set orthograde material at the time of root-end resection [1, 5].
In the present study, the bacterial leakage method was used to evaluate and compare the sealing ability, as it is considered most relevant biologically with maximum clinical simulation. It mimics the bacterial penetration through the entire portion of the root-end filling material, which is affected by many factors, including pH, temperature, etc.
Root-end resection following the orthograde filling might alter the apical seal and cause microleakage, leading to failure of root canal treatment. Microleakage after surgical endodontic treatment is a complex subject due to the influence of various components, which includes: techniques used for the root-end filling, the physical as well as the chemical properties of materials used, apical root-end resection, and thickness of the root-end cavity [7].
Hence, the aim was to analyse the effect of root-end resection on the sealing ability of orthograde apical plugs of three root-end filling materials (MTA Plus, MTA Repair HP, and Biodentine) using the bacterial leakage method and compare it with the retrograde root-end filling technique.
Null hypothesis
There will be no difference in the marginal adaptation of orthograde apical plugs after root-end resection and retrogradely placed root-end filling material.
Materials and method
Eighty-four extracted mandibular premolar teeth with a single root, straight canals without cracks, caries, restoration, and resorption were selected for this in vitro study. Freshly extracted teeth were immersed in 0.5% sodium hypochlorite solution for about 1 h to eliminate organic materials from the root surfaces. Samples were then stored in physiologic saline to keep them moist before and during the experiment. Samples were randomly divided into two main experimental groups and one control group: Group I: orthograde technique, followed by root-end resection; Group II: retrograde technique; control Group III (n = 12): obturation with gutta-percha followed by root-end resection, depending on the methods of root-end filling. Experimental groups were further subdivided into three subgroups (n = 12) A: MTA Repair HP (Angelus Ltd. Brazil), B: Biodentine (Septodont Ltd, France), C: MTA Plus (Prevest Denpro Ltd. India), depending on the materials used (Fig. 1).
Sample preparation
The root length of each tooth was standardized to 15 ± 1 mm from the apex using a vernier calliper (Mitutoyo, Japan). It was decoronated using a diamond disc in a high-speed handpiece with water coolant. The standard access opening was prepared, and the working length was obtained by inserting #10K-file (Mani, India) into the canal until it was visible at the apical foramen and subtracting 1 mm from the respective value. The working length was confirmed using a digital radiograph. All samples were then instrumented to an ISO size of #40K-file (Mani, India) till working length, and the coronal portion was flared using #2 Gates–Glidden drills (Mani, India) till the coronal one-third of the root. Between instrumentation, irrigation was done using 1 mL of 5.25% sodium hypochlorite (Neelkanth, India), and the smear layer was removed with 1 mL of 17% EDTA (META BIOMED CO.Ltd, Korea), followed by 3 mL of sodium hypochlorite. Sterile paper point (Dentsply, USA) was used to dry the root canals after instrumentation.
For the orthograde technique
In experimental groups I.A., I.B., and I.C., the respective root-end filling materials were mixed as per the manufacturer’s instructions and placed into the canal from an orthograde approach using a messing gun (GDC, India). Materials were condensed with endodontic pluggers (GDC, India) to create a 5 ± 1 mm-thick apical plug. Void-free material placement and 5 mm apical plug thickness were ensured using digital radiographs. The rest of the canal space was left unfilled, and a moistened paper point was placed into it such that the paper point was in contact with the materials. Samples were stored in an incubator (Bioline, India) at 37 °C for 48 h to allow the material to set completely. All the samples of Group I (I.A., I.B., I.C.) were then subjected to root-end resection of 3 mm at approximately 90° to the long axis of the tooth using Endo-Z bur (Dentsply, USA), leaving a 3 mm apical plug of root-end filling materials.
For retrograde root-end filling technique
The apical 3 mm of the root apex of each sample from Group II (II.A, II.B, II.C) was resected at approximately 90° to the long axis of the tooth using Endo-Z bur (Dentsply, USA) and class I root-end cavities were prepared to a depth of 3 mm using an ultrasonic tip (ProUltra Surgical retro tips, Dentsply, USA) under 5× magnification. To facilitate proper placement of root-end filling materials, an intracanal plug of gutta-percha cone (Dentsply, USA) was placed as a matrix 3 mm away from the root apex against which root-end filling materials were condensed. This was later confirmed using a periodontal probe (GDC, India) and digital radiographs. Canals were dried with paper points before placement of root-end filling materials. Root-end filling materials were mixed as per the manufacturer’s instructions and placed into the root-end cavity with a messing gun (GDC, India). They were condensed with endodontic pluggers (GDC, India). The remaining canal space was left unfilled, and a moistened paper was placed inside it. The samples were then stored in an incubator at 37 °C for 48 h at 100% humidity to allow the material to set completely.
For control group
The root canal was obturated with gutta-percha (Dentsply, USA) point and A.H. Plus sealer (Dentsply India). After obturation, 3 mm of root apex was resected at approximately 90° to the long axis of the tooth using Endo-Z bur (Dentsply, USA), and gutta-percha was burnished.
Nail varnish (Elite99, China) was applied to the sample’s surface in two layers except for the resected apex and access cavity. This was to prevent bacterial microleakage from the lateral canals.
Bacterial microleakage
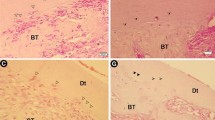
Dual-chamber anaerobic bacteria model was developed by modifying the technique introduced by Torabinejad et al. in 1990 to assess bacterial leakage [8]. The upper chamber was assembled by cutting the 5 mm tip of an Eppendorf tube (Sigma-Aldrich, India) and introducing samples inside the tubes until 2–3 mm of the roots protruded through the end. Sticky wax was used to seal the junction between the tube and root so that leakage other than the canal could be prevented. The assembled apparatus was gas sterilized using ethylene oxide for an 8-h cycle. The lower chamber of the bacterial leakage model comprised sterile disposable culture bottles containing 10 mL of sterile brain heart infusion (BHI) broth. The upper chamber was inserted into the culture tubes (lower chamber) under aseptic conditions such that a minimum of 2–3 mm of root apex was immersed in BHI broth. The junction between the Eppendorf tube and culture tubes was sealed with Parafilm tapes (Fig. 2). Two millimetres of BHI broth was inoculated with 9 × 108 CFU/mL (McFarland no. 3) of Enterococcus (E.) faecalis (ATCC 29212) to form a bacterial suspension. Two to three drops of this bacterial suspension were added to the upper chamber of the bacterial leakage model every second day. The lower chamber was observed for turbidity of the broth using McFarland standard set (Himedia Lab., India), which indicated bacterial growth. The day of McFarland no. 3 turbidity was recorded, and the experiment was conducted for 30 days. A sample was taken from the culture bottle and cultivated to confirm the purity of E. faecalis in BHI broth. The samples with no turbidity on the 30th day of the test were also cultivated to confirm the absence of microorganisms.
Statistical analysis of the data was accomplished using the Kaplan–Meier survival analysis test. A probability value of less than 0.05 was considered to be significant.
Results
By the end of 30 days, the occurrence of turbidity indicating bacterial leakage was 75% in MTA Repair HP, 83.3% in Biodentine, and 91.7% in MTA Plus samples. This trend of turbidity was similar in both orthograde and retrograde root-end filling techniques. The control group showed turbidity in all the samples (100%). More MTA Repair HP samples (25%) survived the 30 days observation period with no bacterial leakage compared to Biodentine (16.7%) and MTA Plus (8.3%) (Fig. 3).
The average time for bacterial leakage in different materials in orthograde and retrograde root-end filling techniques was compared using Kaplan–Meier survival analysis and survival plot. The log-rank estimation indicated that the time required for the turbidity to occur in both the orthograde and retrograde groups was statistically significantly different (X2 = 128.27.52, p < 0.001) compared to the control group (Table 1). Pairwise comparison of the average days for bacterial leakage between the orthograde and retrograde groups was made using a post hoc log-rank test. No statistically significant difference was observed between the experimental groups (p > 0.05) for all materials. MTA Repair HP in the orthograde techniques showed bacterial leakage in the median of 16th day compared to the median of 17th day by the retrograde root-end filling techniques (p > 0.05). Similarly, MTA Plus in the orthograde techniques showed bacterial leakage in the median of 8th day compared to a median of 7th day by the retrograde root-end filling techniques (p > 0.05). Biodentine showed bacterial leakage in the median of 8th day by both techniques (p > 0.05). Survival tests showed distributions of survival rates were the same in all experimental groups (Fig. 4).
Discussion
The success rate of root canal treatment is 53–98%, while it reduces in retreatment cases and cases exhibiting a periapical pathosis [9]. If periapical pathosis persists or non-surgical endodontic treatment is not successful or impractical, endodontic surgery is indicated. In the present study, an evaluation was performed to compare whether there would be any discrepancy in the apical seal when the root-end filling materials were placed through the orthograde or the retrograde approach during periradicular surgery using the bacterial leakage method.
The sealing ability of root-end filling materials is one of the crucial factors responsible for microleakage. Numerous in vitro types of research have been taken into consideration for the evaluation of the sealing ability of root-end filling materials, such as dye leakage method, scanning electron microscopy, electrochemical methods, fluid filtration techniques, radioisotopes, bacterial leakage method, and more recently micro-computed tomography analysis. Micro-computed tomography analysis is a non-invasive three-dimensional imaging technique used to measure the voids in apical plugs and assess the sealing ability of the root-end filling materials.
In the present study, the bacterial leakage method was used as it is clinically and biologically relevant [10]. Also, it helps in the exact measurement of bacterial penetration through the material and access the sealing ability of the entire portion. According to Barthel, different factors such as ion charge, pH, and temperature influence bacteria penetration through the material [11]. Hence, the bacterial leakage model was chosen for better simulation of the clinical condition.
The rationale for using E. faecalis is that these are most commonly isolated from secondary root canal infection. These bacteria are considered endodontic pathogens due to their high incidence in filled root canals and their resistance to various drugs [1, 3].
In the present study, a concentration of 0.5% sodium hypochlorite was used to clean the root surface of a freshly extracted sample tooth for its antibacterial and organic tissue disintegration properties. Studies have shown that a higher concentration of sodium hypochlorite would affect the physical and mechanical properties of the tooth. According to Sim et al., 5.25% of sodium hypochlorite reduces dentine's flexural strength and elastic modulus [12]. Hence, a lower concentration was used for its minimal effect on the physical property of the tooth and to achieve a desirable debridement effect.
Intracanal delivery technique for apical barrier placement plays a critical role in its sealing ability and the root-end filling material [13]. Thus, in the present study, for the retrograde root-end filling technique, root-end filling material was well condensed against a gutta-percha matrix which helps in better visualization and adaptation of the material. In the orthograde technique, samples were flared coronally to increase accessibility to the apical part, which will help to place the material in an appropriate place and condense it well, followed by root-end resection.
Canals were left unfilled in the experimental group, where apical plugs of root-end filling materials were placed. Gutta-percha root filling was not performed in these groups to avoid interfering with the sealing ability of the apical plugs and to accurately measure and compare the absolute microleakage through root-end filling materials. This technique is in concurrence with Hong et al. [14]. However, a moist paper point was kept inside the canals in contact with materials, as moisture is required to set mineral trioxide aggregate properly. In the control group, the canals were filled with gutta-percha, followed by root-end resection without any root-end filling to assess the sealing ability of gutta-percha as a material.
In the current research, 3 mm of root apex was resected in both techniques. Kim et al. stated that at least 3 mm resection of root apex would lead to a 98% reduction of apical ramification and 93% of lateral canals. Also, it will leave almost 7–9 mm of root length required for sufficient strength and stability to reduce the chance of reinfection [15]. Root-end resection was done at approximately 90° to the tooth’s long axis to minimize the root end’s beveling. The root-end resection is better to be done perpendicular to the long axis of the tooth from a biological perspective [16]. Minimal bevel (<10°) will lead to less exposure of dentine, require small osteotomy size, and minimal loss of buccal plate during microendodontic surgery. Also, it will have a lesser danger of periodontal communication and lingual perforation. In addition to the advantages mentioned above, it will also help quickly identify canals [15]. Microleakage increases with an increase in the slope angle due to more exposed dentinal tubules in the resected apical root [17].
The thickness of root-end filling material plays a vital role in its sealing ability. An apical plug thickness of 2–5 mm provides an effective apical seal [7, 18]. As the thickness increases, the resistance to leakage also increases [5]. In the present study, a 3 mm thickness of apical plug was selected since ultrasonic tips used for the root-end preparation were 3 mm in height, and the thickness was kept the same for both techniques to assimilate all the groups. A similar technique has been used by Moradi et al. [1].
In the present study, Pro Ultra Surgical ultrasonic retro tips (Dentsply, USA), zirconia-coated tips, were used for class I cavity preparation. Ultrasonic tips produce deeper and clean root-end cavities than burs and ultimately help in the retention of filling material and proper disinfection [19]. The class I cavity prepared with the ultrasonic tip is more centred in the canal, the operator has superior control, and there are reduced perforation chances [20]. Also, these tips are active and remove the intracanal filling material easily. The cavosurface produced by these tips is slightly rough, which helps better adherance to the root-end filling material. One of the advantages of zirconium-coated tips is its narrow diameter, as zirconium nitride is processed into the metal rather than adhered superficially over the tips [21].
An observation period of 30 days was selected depending on the results of several similar studies where most samples showed microleakage in the first 5–10 days [1]. Montellano et al. also reported similar results over 30 days, where approximately all the samples showed microleakage in the first 3 days [2]. However, Al-Hezaimi et al. obturated the entire canal with root-end filling material, and microleakage was observed after 42 days. This may be due to the increased thickness of the material [22].
In the present study, the sealing ability of three root-end filling materials, MTA Plus (Prevest Denpro Ltd., India), MTA Repair HP (Angelus Ltd., Brazil), and Biodentine (Septodont Ltd., France), placed as an apical plug by both orthograde and retrograde root-end filling techniques was compared. A statistically significant difference was found between MTA Repair HP, Biodentine, and MTA Plus root-end filling material (p < 0.05); the MTA Repair HP showed the lowest bacterial leakage, followed by Biodentine and MTA Plus, respectively. High plasticity and the presence of calcium tungstate radio opacifier instead of bismuth oxide could be the attributing factor for better leakage resistance of MTA Repair HP. High plasticity improves its marginal adaptation to the root walls and decreases microleakage. Along with it, the higher release of calcium ions from the calcium tungstate during the initial stage promotes resistance of the material and prevents bacterial leakage [23].
This study showed no statistically significant difference between the sealing ability of both the techniques (p > 0.05) for all three root-end filling materials. Similar results were shown by many authors, including Moradi et al., who suggested no difference in the sealing ability of orthograde MTA and CEM plugs after root-end resection with retrograde MTA root-end filling [1].
Also, Andelin et al. declared that once MTA is set, root-end resection does not alter its sealing ability [24]. Similarly, Habibi et al., through their in vivo study on cats, showed no difference in the healing process of set and fresh MTA [6]. Hence, the results of this study showed that placing root-end filling material in an orthograde manner and then resecting the rigid material does not necessarily disturb the apical seal, in agreement with Yildirim et al. [7] and Milani et al. [25].
Conclusion
The study found that the sealing ability of already set root-end filling materials placed through the orthograde approach did not deteriorate after root-end resection. This suggests that the orthograde technique, which involves placing the apical plug from the coronal aspect of the tooth, can be regularly practised as it is a simplified technique compared to the retrograde root-end filling technique. Furthermore, the study compared the sealing abilities of three different root-end filling materials: MTA Repair HP, Biodentine, and MTA Plus. It was found that MTA Repair HP demonstrated the lowest bacterial microleakage, indicating that it provided a better seal compared to Biodentine and MTA Plus. This suggests that MTA Repair HP may be preferable for root-end filling due to its superior sealing properties.
Overall, the study’s findings support the use of the orthograde technique and highlight the importance of selecting an appropriate root-end filling material, with MTA Repair HP showing the best sealing ability among the three materials tested.
Data availability
The data supporting the findings of this study are available upon request from the corresponding author.
References
Moradi S, Disfani R, Ghazvini K, Lomee M. Sealing ability of orthograde MTA and CEM cement in apically resected roots using bacterial leakage method. Iran Endod J. 2013;8:109–13.
Montellano AM, Schwartz SA, Beeson TJ. Contamination of tooth-colored mineral trioxide aggregate used as a root-end filling material: a bacterial leakage study. J Endod. 2006;32:452–5.
Medeiros PL, Bernardineli N, Cavenago BC, Torres SA, Duarte M, Bramante CM, et al. Sealing ability of MTA, CPM, and MBPc as root-end filling materials: a bacterial leakage study. J Appl Oral Sci. 2016;24:148–52.
Gondim E, Zaia AA, Gomes BPFA, Ferraz CCR, Teixeira FB, Souza-Filho FJ. Investigation of the marginal adaptation of root-end filling materials in root-end cavities prepared with ultrasonic tips. Int Endod J. 2003;36:491–9.
Moradi S, Disfani R, Lomee M, Naghavi N. Effect of root resection on sealing ability of orthograde apical plugs of mineral trioxide aggregate and calcium-enriched mixture. J Dent (Tehran). 2014;11:447–54.
Habibi M, Ghoddusi J, Habibi A, Mohtasham N. Healing process following application of set or fresh mineral trioxide aggregate as a root-end filling material. Eur J Dent. 2011;5:19–23.
Yildirim T, Er K, Taşdemir T, Tahan E, Buruk K, Serper A. Effect of smear layer and root-end cavity thickness on apical sealing ability of MTA as a root-end filling material: a bacterial leakage study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:67–72.
Torabinejad M, Ung B, Kettering JD. In vitro bacterial penetration of coronally unsealed endodontically treated teeth. J Endod. 1990;16:566–9.
Gorni FG, Gagliani MM. The outcome of endodontic retreatment: a 2-year follow-up. J Endod. 2004;30:1–4.
Timpawat S, Amornchat C, Trisuwan WR. Bacterial coronal leakage after obturation with three root canal sealers. J Endod. 2001;27:36–9.
Barthel CR, Moshonov J, Shuping G, Orstavik D. Bacterial leakage versus dye leakage in obturated root canals. Int Endod J. 1999;32:370–5.
Sim TP, Knowles JC, Ng YL, Shelton J, Gulabivala K. Effect of sodium hypochlorite on mechanical properties of dentine and tooth surface strain. Int Endod J. 2001;34(2):120–32.
Hachmeister DR, Schindler WG, Walker WA 3rd, Thomas DD. The sealing ability and retention characteristics of mineral trioxide aggregate in a model of apexification. J Endod. 2002;28:386–90.
Hong ST, Bae KS, Baek SH, Kum KY, Lee W. Microleakage of accelerated mineral trioxide aggregate and Portland cement in an in vitro apexification model. J Endod. 2008;34:56–8.
Kim S, Kratchman J. Modern endodontic surgery concepts and practice: a review. J Endod. 2006;32:601–23.
Post LK, Xavier CB, Demarco FF. Sealing ability of MTA and amalgam in different root-end preparations and resection bevel angles: an in vitro evaluation using marginal dye leakage. Braz Dent J. 2010;21:416–9.
Peter AG, Figdor D, Martin J. Apical dentin permeability and microleakage associated with root end resection and retrograde filling. J Endod. 1994;20:22–6.
Lamb EL, Loushine RJ, Weller N, Kimborugh WF, Pashley DH. Effect of root resection on the apical sealing ability of mineral trioxide aggregate. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:732–5.
Wuchenich G, Meadows D, Torabinejad M. A comparison between two root endpreparation techniques in human cadavers. J Endod. 1994;20:279–82.
Engel TK, Steiman HR. Preliminary investigation of ultrasonic root-end preparation. J Endod. 1995;21:443–8.
Navarre SW, Steiman R. Root-end fracture during retropreparation: a comparison between zirconium nitride-coated and stainless steel microsurgical ultrasonic instruments. J Endod. 2002;28:330–2.
Al-Hezaimi K, Naghshbandi J, Oglesby S, Simon JH, Rotstein I. Human saliva penetration of root canals obturated with two types of mineral trioxide aggregate cements. J Endod. 2005;31:453–6.
Tavares L, Cintra A, Benetti F, Olinta I, Queiroz DA, Maria J, et al. Cytoxicity, biocompatibility, and biomineralization of the new high-plasticity MTA material. J Endod. 2017;18:1–5.
Andelin WE, Browning DF, Hsu GR, Roland DD, Torabinejad M. Microleakage of resected MTA. J Endod. 2002;28:573–4.
Milani AS, Sahar S, Borna Z. Evaluating the effect of resection on the sealing ability of MTA and CEM cement. Iran Endod J. 2012;7:134–8.
Acknowledgements
We would like to offer our sincere thanks to Dr. Sandesh N for his assistance with the statistics used in the research.
Author information
Authors and Affiliations
Contributions
Chhaya Harinkhere: conceptualization, methodology, visualization. Pallav Mahesh Patni: data curation, supervision, validation. Pradeep Jain: methodology, visualization, reviewing. Swadhin Raghuwanshi: supervision, writing—editing. Sanket Hans Pandey: software, validation, writing—reviewing. Sakshi Bilaiya: supervision, validation, writing—reviewing and editing.
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Harinkhere, C., Patni, P.M., Jain, P. et al. Comparison of the sealing ability amongst orthograde apical plugs of mineral trioxide aggregate plus, mineral trioxide aggregate repair HP, and Biodentine after root resection: a bacterial leakage study. Odontology 112, 364–371 (2024). https://doi.org/10.1007/s10266-023-00847-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-023-00847-4