Abstract
It is known that Streptococcus mutans (S. mutans) is the leading cariogenic pathogen. Recently, an increasing number of antimicrobial peptides (AMPs) have been brought into consideration as anti-caries agents. Here, we designed and synthesized an AMP derived from reutericin 6 and/or gassericin A, named LN-7, and explored its effect on biofilm of S. mutans UA159 in vitro and development of dental caries in vivo. Antibacterial assays showed that LN-7 was more active against S. mutans (3.2 μM) than many peptide-based agents, capable of killing other types of Streptococci in oral cavity. In addition, LN-7 presented fast killing kinetics, with more than 97% S. mutans killed within 5 min. The mechanism of the antimicrobial activity mainly lies on the disruption of bacterial membrane. Effects of LN-7 on the biofilm formation and the viability of preformed biofilm were quantified by crystal violet staining, which showed that LN-7 could effectively inhibit the biofilm accumulation of S. mutans. Moreover, the biofilm of S. mutans treated with LN-7 displayed notable changes in bacterial viability and morphology, observed by confocal laser scanning microscopy and scanning electron microscopy. In addition, topical oral treatment with LN-7 could suppress the development of dental caries in vivo, reducing the occurrence of severe dental lesion in a rodent model. These results reveal a new peptide-based agent as a topical treatment for dental caries, opening the door to clinical studies to explore its potential for caries prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dental caries is a prevalent chronic microbially mediated human disease worldwide, increasing global economic burden and causing common health concerns. Without appropriate prevention or treatment, it will eventually cause toothache pain and tooth loss, or even develop into maxillofacial infection. It is widely accepted that dental caries is primarily caused by the biofilm communities attached to the surface of the teeth, known as dental plaque [1].
Dental plaque is a complex biofilm system, consisting of a collection of microbial communities enclosed by a matrix of extracellular polymeric substance (EPS) and separated by a network of open water channel [2]. This kind of biofilm system is the prime cause for not only dental caries, but also other oral diseases, such as halitosis, peri-implantitis, periodontitis, and so on [3, 4]. Studies have shown that the regions of the oral cavity could harbor and create different micro-environments with the selection of several species [5]. For instance, in the sample of the tongue dorsum biofilm from halitosis-suffering patients, it was found that Streptococcus spp. seemed to be the most prevalent as early colonizers and F. nucleatum served as a bridge between early and late colonizers within the oral biofilm [2]. On the other hand, Streptococcus sanguinis was found to be the microorganism fundamental to the beginning of biofilm formation in patients with peri-implanting mucositis and peri-implantitis [5,6,7].
As for the natural teeth with dental caries, within the biofilm attached to its surface, Streptococcus mutans (S. mutans) was considered to be the main cariogenic bacteria because of its several cariogenic virulence properties, such as acidogenicity, acidurance, and the ability to interact with other microorganisms to build multispecies biofilm communities [1]. The particular condition of biofilm protects the microbes from environmental damage factors, including host immune cells and drug treatments, and also keeps the microenvironment stable at low pH, resulting in the demineralization of tooth enamel [4, 8]. Therefore, inhibiting the growth of S. mutans, blocking the formation of biofilm, and disrupting the preformed biofilm are the main strategies to prevent dental caries [9]. Traditional pharmacy approaches to prevent dental caries mainly include the use of antimicrobial agent, such as chlorhexidine (CHX), erythromycin, and fluoride-containing products [10, 11]. However, it has been proved that these methods could only exhibit a minimal inhibitory effect on biofilm-encased cells [12]. Furthermore, long-term use of chlorhexidine and fluoride-containing products have several adverse effects, including tooth staining, loss of taste perception, and rising incidence of dental and skeletal fluorosis [11, 13].
To address these concerns, more and more research emphasized the potential of antimicrobial peptides (AMPs) as potent alternatives to traditional antimicrobial agents recently. AMPs are short cationic host-defense molecules composed of 3–50 amino acids and play important modulatory roles in the immune system, effective at low micromolar concentrations against a broad range of microorganisms, including drug-resistant strains [14]. A growing body of evidence supports the notion that AMPs play an important part in maintaining the balance between health and disease in the complicated oral environment [15]. Currently, there are roughly 20 AMPs in different developmental phases, from preclinical to clinical phase Ill trials, four of which are applied to oral disease [16]. Moreover, many natural or synthetic AMPs were studied to assess the ability against cariogenic bacteria, such as α- and β-defensin [17], cathelicidin LL-37 [18], pleurocidin [19], chrysophsin-1 [20], histatin 5 [21], and Bac8c [22], yet no AMPs have been applied to clinical treatment for dental caries.
Reutericin 6 and gassericin A, circular bacteriocins produced by oral commensal bacteria Lactobacillus species, could inhibit the growth of S. mutans and its biofilm formation [23,24,25]. It is worth noticing that they were proved to be related to lower levels of dental plaque in vivo [24]. The sequences of them are identical (58 common amino acids), but the secondary structures are different [26]. However, because of their long circular structure, the synthesis of them is complicated and high-costing.
The objectives of this study were (1) to design and synthesize a novel short linear reutericin 6 and/or gassericin A-inspired peptide, (2) to subsequently demonstrate its activity against planktonic cultures and biofilms of S. mutans in vitro, also its killing kinetics and modes of action, and (3) to further explore its effect on the prevention of dental caries in vivo. Worth mentioning, to the best of our knowledge, this work is the first to observe anti-caries effects of a peptide derived from reutericin 6 and gassericin A in a rodent model of dental caries in vivo.
Materials and methods
Peptide design and synthesis
First, from the cationic α-helical region of reutericin 6 and/or gassericin A, a 13-residue linear peptide was truncated and named as LR-1. Then, the subsequent modification was based on the principle of amphipathicity and cationicity. Arginine residues were chosen to substitute the non-polar and negatively charged residues on the polar faces of LR-1 to increase its cationicity. Meanwhile, tryptophan and lysine residues were used to substitute the non-hydrophobic residues on the non-polar face to enhance the AMP’s antimicrobial activity [27,28,29]. Eventually, an AMP with increasing cationicity and hydrophobicity was obtained and named LN-7, with a sequence of LRRWLRWLLRWMR-NH2. The peptide was synthesized using standard 9-fluorenylmethoxycarbonyl (Fmoc) solid-phase protocols on Rink Amide MHBA resin (Nanjing Peptide Biotech Ltd, Nanjing, China). The C-terminal of the peptides was amidated to remove a negative charge at neutral pH. It was purified to >95% by RT-HPLC and their molecular weights were measured by mass spectrometry. Prior to assessing antimicrobial activities, the peptide was dissolved in sterile deionized water at a concentration of 5 mg/mL and stored at − 20 °C.
Strains and growth condition
Streptococcus mutans UA159 (S. mutans UA159), S. mutans ATCC25175 (S. mutans ATCC25175), Streptococcus gordonii ATCC10558 (S. gordonii ATCC10558), Streptococcus sobrinus ATCC33478 (S. sobrinus ATCC33478), and Enterococcus faecalis ATCC29212 (E. faecalis ATCC29212) were acquired from the Guangdong Microbial Culture Collection Centre (GDMCC; Guangdong, China). Brain–heart infusion (BHI) broth was used for anaerobic culture (10% CO2, 10% H2, 80% N2) at 37 °C.
Bacterial susceptibility assay
Minimal inhibitory concentrations (MIC) and minimum bactericidal concentrations (MBC) were measured by the standard broth microdilution method following the recommendations of the Clinical and Laboratory Standards Institute (CLSI) with some modifications [30]. Bacterial strains grown overnight at 37 °C were diluted to a final concentration of 1.0 × 106 CFU/mL and treated with LN-7, erythromycin (Sangon Biotech, Shanghai, China), or CHX (Sangon Biotech, Shanghai, China). The final test concentration for LN-7 ranged from 0.4 to 51.2 μM. Erythromycin and CHX were used as the positive controls ranging from 0.03 to 32.0 μM. Medium without bacteria served as the negative control. The experiments were performed in 96-well microtiter plates. The plates were incubated anaerobically at 37 °C for 1–2 days. MICs were determined as the lowest concentration of drugs that inhibited bacterial growth by visual inspection after 24 h of incubation. MBCs were defined as the lowest concentration resulting in no bacterial growth after 48 h of incubation with bacterial suspension spread on BHI.
Time-killing assay
The killing kinetics of the LN-7 against S. mutans UA159 were analyzed using a time-killing assay as previously described [31,32,33]. In brief, S. mutans was diluted to 1.0 × 106 CFU/mL in the BHI medium. Solutions of LN-7 at final concentrations of 6.4 and 12.8 μM (1× MBC and 2× MBC) were added to the bacterial suspension, with 19.8 μM (2× MBC) chlorhexidine and 2.7 μM (2× MBC) erythromycin as positive controls, and a non-treated group as the negative control. The cell survival was estimated by colony enumeration on BHI agar after treatment at 37 °C for 0, 0.5, 1, 1.5, 3, 5, 7, 9, 10, 15 and 30 min. The percent survival was determined by dividing the viable cell CFU/ml by the total CFU/ml in the untreated controls.
To further investigate the killing kinetics of the LN-7, optical density assays were performed as follows: S. mutans UA159 were cultured overnight, centrifuged at 1000 g for 10 min, and diluted to 1.0 × 106 CFU/ml with PBS after harvest. LN-7 at final concentrations of 6.4 and 12.8 μM was then added to the bacterial suspension for 0, 5, 15, 30, 60, 90, and 120 min at 37 °C. 3.5 μM melittin was used as a positive control. A non-treated group was used as a negative control. The mixture was filtered through a filter membrane (0.22 μm), and the optical density at 260 nm of the filtrates was measured by ultraviolet spectrophotometer (UV757CRT, Lengguang Tech., China).
In addition, to determine the antimicrobial effects of LN-7 on other types of Streptococci in oral cavity (S. sobrinus ATCC33478 and S. gordonii ATCC10558) at a cell density of 1 × 106 CFU/ml, bactericidal kinetics was also examined as described above, but only upon treatment with solution of LN-7 at final concentrations of 1 × MBC.
Biofilm susceptibility assays
Inhibition of S. mutans biofilm formation was examined using the crystal violet-based microtiter plate assay described originally by O’Toole and Kolter [34]. S. mutans UA159 was grown in BHI broth with 1% (w/v) sucrose (BHIS) and diluted to a final concentration of 1.0 × 106 CFU/mL, treated with LN-7, chlorhexidine, or erythromycin. The concentrations tested were 0.6×, 0.8×, 1×, 2×, 4× and 8× their respective MICs. After incubation at 37 °C for 24 h, the supernatant medium was removed, and all wells were washed three times with PBS. And then, 100 μL of methanol was added to fix adhered cells for 15 min. After the removal of methanol, 100 μL of 0.1% crystal violet was added for 5 min to stain adhered biomass. Excess dye was removed and rinsed with water, then the wells were air-dried for 1 h. To quantify the biomass, crystal violet stains were solubilized in 95% ethanol for 30 min and the optical densities were measured at the wavelength of 595 nm using a microplate reader. Biofilm formation was expressed as a ratio of crystal violet-stained biofilms relative to the untreated control. Biofilm was treated with chlorhexidine and erythromycin as positive controls.
Moreover, the antibiofilm activities of LN-7 were examined against preformed biofilm as described previously with a minor modification [10]. S. mutans UA159 was adjusted to 1 × 106 CFU/ml in BHIS and seeded on to 96-well polypropylene flat-bottomed plates. Biofilms were established anaerobically at 37 °C for 24 h. After incubation, non-adherent cells were removed carefully. Biofilms were then treated with LN-7, CHX, or erythromycin at final concentrations of 0, 1×, 2×, 4×, 8× and 10× their respective MICs in fresh BHIS for 24 h. To count the viable cells within treated biofilms, plates were sonicated for 5 s to dislodge the adherent bacteria. Then, the bacteria were removed mechanically from biofilms by scraping with pipette tips and rigorous vortex. The bacterial suspension was spread on BHI agar and incubated anaerobically at 37 °C for 2 days before colony enumeration.
Confocal laser scanning microscopy
S. mutans UA159 was cultured in BHIS for 24 h and diluted to a final concentration of 1.0 × 106 CFU/mL and then seeded in 6-well plates with coverslips in each well to establish biofilms. 1-day old S. mutans biofilms were treated with LN-7, CHX or erythromycin at the concentration of 10× MIC at 37 °C for 24 h. A no-treatment group was used as the negative control. After that, the biofilms on coverslips were rinsed thrice with PBS, followed then by labeling with 200 µl of the live/dead BacLight Bacterial Viability stain (L13152, Invitrogen, Carlsbad, CA, USA) and examined using an Olympus Fluoview FV10i confocal microscope (Olympus, Tokyo, Japan). Live cells were stained with SYTO 9 (green fluorescence), and dead cells were stained with propidium iodide (PI; red fluorescence).
Scanning electron microscopy
To observe the morphological change of planktonic bacteria in the presence of LN-7, we used the scanning electron microscope (SEM, Merlin, Zeiss, Oberkochen, Germany). Briefly, exponential-phase cultures of S. mutans UA159 (~108 CFU/ml) were treated with or without LN-7 at a final concentration of 2× MBC and incubated anaerobically for 24 h at 37 °C. Bacterial suspensions were centrifuged at 5000 g for 5 min, washed three times, and then resuspended in PBS. The subsequent procedures were performed as described previously [29].
Besides that, the effects of LN-7 on the morphology change of preformed biofilms were also observed. 1-day old S. mutans biofilms were preformed in BHIS broth and treated with drugs as described in the study of treatment of preformed biofilms but instead in 6-well plates with coverslips in each well.
The biofilms were then treated with LN-7, CHX, or erythromycin at 10× their respective MICs in BHIS broth. The preparation of biofilm samples for SEM observation was as described for the planktonic samples above. The samples were then observed by SEM.
PI uptake assay
To detect the ability of the peptide to break the bacterial membrane, propidium iodide (PI) was used as a fluorescence probe for its ability to cross the disrupted membrane and stain the nucleic acids of cells [35]. Mid-logarithmic phase S. mutans UA159 was adjusted to 1 × 106 CFU/ml. The cells were, respectively, treated with or without LN-7 dissolved in PBS at concentrations of 1× and 2× MBCs in centrifuge tubes. After 0, 5 and 10 min of incubation at 37 °C, the supernatants were removed and cells were washed twice with PBS. Then, 13.4 μM PI (Leagene, Beijing, China) was added to the cells and incubated for 30 min at room temperature. The cells were resuspended in 500 μl PBS after washing three times. The PI-positive cells were assessed by flow cytometry (FACSCanto II, BD, USA).
Circular dichroism (CD) spectroscopy
The CD spectra of the peptide solutions were recorded at room temperature using a CD spectrometer (ChirascanTM, Leatherhead, Surrey, UK) and a quartz cell with 0.5 cm path length. LN-7 was dissolved to a final concentration of 250.0 μg/ml with PBS (pH 7.4, mimicking an aqueous environment), or supplemented with 50% (v/v) TFE (mimicking the hydrophobic environment of the microbial membrane) [36]. Spectra were recorded by scanning wavelength from 190 to 250 nm at 20 nm min−1, and spectra averaged from four repeats. Spectra were analyzed using CDPro (http://lamar.colostate.edu/~sreeram/CDPro/main.html). Fractions of different types of secondary structure were calculated using three programs within the software (SELCON3, CONTINLL, and CDSSTR). The results of the three methods were averaged to give the final fractions.
In vivo animal study
To determine the effects of LN-7 on the development of dental caries in vivo, a total of 24 rats were purchased from the Animal Lab Center of Southern Medical University (Guangzhou, China). Animal experiments were performed on a well-established rodent model of dental caries disease as described previously [37,38,39]. Briefly, 24 weaned Sprague–Dawley rats, 21 days old, were fed with ampicillin sodium water (4000 U/ml) and a regular diet for 3 days to lower the microbial load. Oral swabs were plated on Mitis salivarius agar (Solarbio, Beijing, China) and cultured anaerobically at 37 °C to confirm the absence of endogenous S. mutans infection. The animals were then offered cariogenic diet 2000# ad libitum throughout the experiment to enhance the infection by S. mutans. At 24 days old, the animals were infected orally using an actively growing (mid-logarithmic) culture of S. mutans UA159 every day for five consecutive days to allow oral colonization, and their infection was checked via oral swabbing. Then, the infected animals were randomly placed into treatment groups (8 animals/group), and their teeth were treated topically twice daily with saturated cotton swabs containing treatment solutions wiped on the molars during a uniform operating time of approximately 1 min. The treatment groups included: (1) 32 μM LN-7 peptide solution, (2) 0.2% NaF (positive control), and (3) distilled deionized water (DDW; negative control).The experiment proceeded for 6 weeks; all animals were weighed weekly and their physical appearance was noted daily. At the end of the experimental period, the animals were sacrificed, and the jaws were surgically removed and aseptically dissected. All of the jaws were defleshed, molars of the animals were examined under a stereomicroscope and carious lesions were scored by the method of Keyes [40]. The determination of caries scores of the codified jaws was performed by a calibrated examiner.
Furthermore, the hemi-sectioned molars were prepared to be observed by the scanning electron microscope as described previously with a minor modification [41, 42]. First, the samples were fixed in 2.5% glutaraldehyde for 24 h and then washed in PBS to remove the fixative. After being dehydrated in increasing concentrations of ethanol, the samples were preserved at − 80 °C overnight and then dried in a lyophilizer. The subsequent procedures for SEM were performed as described previously [29].
Statistical analysis
All experiments were performed in triplicate, and the data are presented as mean ± standard deviation. Statistical analysis was carried out using GraphPad Prism version 7.0 software (GraphPad Software, Inc., La Jolla, CA, USA) via a one-way analysis of variance (ANOVA) or Kruskal–Wallis H test. Statistical significance was defined as P ≤ 0.05.
Results
Antimicrobial activity of LN-7
The cationic α-helical region of reutericin 6 and/or gassericin A was truncated and named LR-1. According to the principle of amphipathicity and cationicity of AMPs, we modified LR-1 into LN-7. To evaluate the antimicrobial potency of LN-7 against S. mutans UA159, we made a comparison among LN-7, LR-1 and several peptide-based antimicrobial agents with established effects against S. mutans (Table 1). It was observed that compared with LR-1, LN-7 exhibited obviously higher antimicrobial potency against S. mutans in the same condition with the MIC of 3.2 μM and MBC of 6.4 μM. In addition, the MICs of these known AMPs, except for LL-37, against S. mutans UA159 ranged from 4.6 to 100.4 μM, while LN-7 exhibited higher antimicrobial potency against S. mutans UA159 under the same test condition.
Besides, the effectiveness of LN-7 against other oral pathogenic bacteria was also tested. It turns out that LN-7 was effective against S. mutans, S. gordonii and S. sobrinus, but showed relatively low antimicrobial effect on E. faecalis; MIC of 3.3 μM and MBC values ranged from 6.5 to 13.1 μM (Table 2).
Killing kinetics of LN-7
To assess the killing kinetics of LN-7 against S. mutans, we performed a time-killing assay (Fig. 1). The results showed that LN-7 was more efficient in killing S. mutans than CHX and erythromycin. More than 97% of the planktonic bacteria were killed within 5 min after treating with LN-7, and all S. mutans were killed in 10 min, whereas after treating with CHX or erythromycin for 30 min, survival percent of S. mutans still remained 54.6 and 88.5%, respectively. In addition, the antimicrobial activity of LN-7 against planktonic S. mutans UA159 was dose- and time-dependent.
Next, we evaluated the killing kinetics of LN-7 against single-species planktonic cultures of S. mutans UA159 and two closely related oral Streptococci, S. sobrinus ATCC33478 and S. gordonii ATCC10558. It was shown that within 15 min, nearly 95% of S. gordonii were killed and all S. gordonii were killed in 30 min. However, the killing rate against S. sobrinus is rather slower, with only 52% of S. sobrinus killed within 30 min (Fig. S1).
In addition, the killing kinetics was further assessed by measuring the absorbance value at 260 nm with ultraviolet spectrophotometer as indicated in Fig. S2. After a different treatment, the leakage of nucleic acid of dead bacteria was monitored. Melittin was used as the positive control for its known ability to disrupt bacterial membrane. We can see that LN-7, CHX and melittin exerted relatively fast killing rate. On the contrary, the killing kinetics of erythromycin is rather slower. Furthermore, the killing kinetics of LN-7 against the other two types of Streptococci was consistent with the result of the colony-forming unit assay.
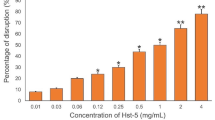
Effect of LN-7 on the formation and establishment of S. mutans biofilm
Given that the dental plaque formed by cariogenic bacterium is an important etiological factor for dental caries, we then tested the 50% minimum biofilm inhibitory concentration (MBIC50) of LN-7, CHX, and erythromycin, which indicated the activity against the formation of S. mutans biofilm. The biofilm biomass was quantified after staining with crystal violet for 24 h and the results are presented in Fig. 2. The reduction of S. mutans biofilm formation jumped from 60.2% at 0.6× MIC to over 99.5% at 2× MIC of LN-7, indicating that the MBIC50 of LN-7 was 0.6× MIC, and LN-7 could nearly inhibit the formation of biofilm of S. mutans completely at the concentration of 2× MIC, as the same as CHX. However, erythromycin was less effective at inhibiting biofilm formation and required 4× MIC to achieve complete inhibition.
Next, we assessed the effect of LN-7 on 1-d old S. mutans UA159 biofilm by quantifying the viable cells in the treated biofilm. We found that the ability of LN-7, CHX, and erythromycin to eradicate biofilms are dose-dependent (Fig. 3). At the concentration of 10 × MIC (32 µM), LN-7 could cause an overall 2.40-log10 reduction in the number of viable cells when compared with the untreated control. In contrast, CHX and erythromycin could only yielded a reduction in cell viability of 1.28- and 1.08-log10 at 10 × MIC, respectively.
Anti-biofilm activity of LN-7 against preformed S. mutans biofilms. 1-d old biofilms of S. mutans UA159 were treated with LN-7, CHX and erythromycin at final concentrations of 1 to ×10 their respective MICs in BHIS for 24 h. Viable cells within biofilms were obtained by colony enumeration on agar plates
Impairment of preformed biofilms visualized by confocal laser scanning microscopy (CLSM) and scanning electron microscopy (SEM)
After quantitative analysis, CLSM and SEM were used to reveal the changes of bacterial viability and morphology in the preformed biofilms treated with 10× MICs of LN-7. In the representative live/dead staining images (Figs. 4, 5), the green signal stands for vital bacteria with intact membranes, while the red signal stands for dead bacteria with destroyed membranes, and the yellow signal stands for the mixture. Biofilms incubated in the control group appeared dense and thick, with an average height of 21 µm, and no red signal was visualized. Conversely, the biofilm formed sparsely when added with LN-7 and CHX. It was obvious that the images of LN-7 showed thinner biofilms with an average height of 15 µm (Fig. 5) and more red signals when compared with the control group and erythromycin group (Fig. 4).
On the other hand, SEM depicted the impact of LN-7 on the structural integrity of preformed biofilm (Fig. 6b). After exposure to LN-7, an essentially disrupted cellular network and porous exopolysaccharide matrix were observed and the cell aggregates were hard to form. Whereas, the control group as shown in Fig. 6a showed apparent clumping of cells with a formation of chains embedded into the exopolysaccharide pool. Also, only a little change was observed in CHX- and erythromycin-treated biofilms compared to untreated biofilms (Fig. 6c, d).
Mechanism of action of LN-7
It is acknowledged that disrupting membranes is one of the mechanisms of AMPs, which causes the lysis of microbial cells [43]. To explore the possible modes of action of LN-7 using PI as a labeling reagent, we employed flow cytometry to investigate the interactions between LN-7 and S. mutans. It was reported that PI is able to bind to double-stranded DNA by intercalating between base pairs, thus providing a rapid and reliable fluorescence method for monitoring dead bacterial cells injured by AMPs [33]. The observed red fluorescence stained by PI indicated that LN-7 was able to break down the cell membrane, which, as a result, can lead to the leakage of nucleic acid labeled with the PI dye. With a 5 min exposure to LN-7 at 12.8 µM, more than 96% of the S. mutans UA159 were stained with PI, which was in accordance with the result of the killing kinetics assays of LN-7 against planktonic S. mutans, and the proportion of the PI-positive cells were dose- and time-dependent.
Also, SEM was used to observe morphology changes of S. mutans UA159 after treated with LN-7. As shown in Fig. 7a, in the absence of the peptide, S. mutans showed a regular, smooth surface. When exposed to 2× MBC of LN-7, S. mutans obviously altered bacterial morphology: cells lost their original form (Fig. 7b), small holes and ruptures of membrane visible (Fig. 7c), and aggregates of cellular debris (Fig. 7d).
Secondary structure of LN-7
The secondary structures of LN-7 in water or 50% (v/v) TFE/water, which mimicked a hydrophobic membrane environment, were assessed using CD spectroscopy. As shown in Fig. 8, the CD spectrum of LN-7 in PBS and 50% TFE/water both exhibited two negative minimum peaks at 208 and 222 nm, indicating that the peptides adopted a well-defined α-helical structure. The calculated percentage of secondary structure elements for LN-7 was 98.85% α-helix and 5.98% β-turn in PBS, 99.60% α-helix and 5.30% β-turn in 50% TFE/water solution.
Prevention of dental caries in vivo
To assess whether LN-7 would exert effects in the complex oral environment in vivo, we then carried out an in vivo animal study. The experimental design and treatment regimen are illustrated in Fig. 9. It was observed that body weight was similar across all rats in three groups throughout the experiment, as shown in Fig. 10, and the rats remained apparently healthy and active. Moreover, no macroscopic tissue lesions or abnormalities were observed on the mucosa of the animals during the whole experiment, which proved the relative safeness of LN-7.
The carious lesions established on the occlusal surface were scored according to the penetration depth of murexide as enamel caries (E), slight dentinal caries (Ds), moderate dentinal caries (Dm) or external dentinal caries (Dx) [42], while lesions detected on smooth surface influenced only on enamel layer. All the scores were depicted in Table 3. In addition, representative images of carious lesions of three groups were obtained as shown in Fig. 11. Quantitative caries scoring analyses revealed that compared with the negative control, the LN-7 group presented significantly less overall carious lesions (P < 0.05). Also, LN-7 was highly effective in decreasing enamel and slight dentinal lesions in sulcal surfaces, similar to the effect of 0.2% NaF treatment (P > 0.05).
Representative images of molars of Sprague–Dawley rats after treatment of distilled and deionized water (DDW), 0.2% NaF, and 32 μM LN-7, respectively. In each group, images of occlusal surface (a–c), lingual surface (d–f), buccal surface (g–i) and hemi-sectioned teeth (j–l) were photographed. Arrows indicate the carious lesions
Moreover, we observed the characterization of the fissure caries with the scanning electronic microscope (Fig. 12). The murexide-negative fissures on the molar showed no cavitation on enamel. The uniform contrast of dentin underneath indicated no significant demineralization activity. The murexide-positive lesion located on the fissures on the molar, however, exhibited fissure caries with a different degree of severity. According to Fig. 12, we can see that the surface of the fissure on the molar in 0.2% NaF group was smooth and continuous (Fig. 12a), and we can clearly tell the enamel-dentinal junction as indicated by the hollow arrow. As for the LN-7 group (Fig. 12b), slight erosion on the enamel was observed, indicated by the solid arrow; however, the enamel-dentinal junction and dentin were intact. The defect was about 13 µm in depth. On the other hand, the surface of the fissure on the molar in DDW group was damaged heavily, which showed a cavitation about 65 µm in depth and had destroyed the enamel-dentinal junction (Fig. 12c).
Discussion
It is known that AMPs with cationicity can initially interact with cells through the attraction to the anionic electrostatic charge of biological membranes. In addition, amphipathicity is a prerequisite for α-helical AMP activity, which enables AMPs to bind to anionic phospholipid head groups of the exterior leaflet of bacterial membranes through electrostatic attraction and, thus, exhibit permeabilizing and/or disrupting activity [44, 45]. In our study, we first truncated the cationic α-helical region of reutericin 6 or gassericin A, named as LR-1, and then exploited existing design strategies [46] to modify it into a novel short linear peptide, LN-7. After the modification, the peptide showed perfect amphipathic arrangement and cationicity, which laid a foundation for the following experimental results that showed that compared with LR-1, LN-7 was more effective against S. mutans. Furthermore, confirmed by CDPro analysis, the secondary structure of LN-7 characterized by CD spectroscopy suggested that LN-7 adopted a helical structure in membrane-mimetic solvents (50% TFE), with a proportion of α- helical structure of 99.6%. The secondary structure of LN-7 characterized by CD spectroscopy suggested that LN-7 adopted a helical structure in membrane-mimetic solvents (50% TFE). It was proposed that percent helical composition >80% was correlated with antimicrobial potency [47]. The high percent helical composition of LN-7 suggested its well antimicrobial potency.
It is usually recommended that the duration of rinsing mouth and tooth brushing is about 3–5 min. Compared with the commonly used antimicrobial agents, chlorhexidine and erythromycin, LN-7 showed faster killing kinetics against planktonic S. mutans, which caused about 97% reduction in viability of S. mutans within 5 min at 12.5 μM, indicating its potential to be used in mouth rinses or toothpaste, assuming that its antimicrobial activity and stability in human saliva can be confirmed. In addition, given its shown effects against other types of Streptococci in the study, LN-7 may be a novel antimicrobial agent with relatively broad spectrum. Interestingly, our data have shown that the killing kinetics of LN-7 against S. mutans is about much faster than that against S. sorbrinus and S. gordonii in 5 min, which suggested that LN-7 may possess a selectively antimicrobial capability targeting S. mutans within a short time. It was demonstrated that selectively targeting of S. mutans biofilms is feasible and can effectively prevent dental caries without disturbing the overall oral microbiome [48], appealing further modification of LN-7. For example, combining LN-7 with the competence-stimulating peptide (CSP) [49], which is able to target S. mutans, may conduce to the selectivity of LN-7, but it requires further study.
Literatures have reported that biofilm-associated microorganisms behaved differently from their planktonic counterparts on their ability to resist drug treatment and host defenses [50]. A unique, highly protected phenotypic state adopted by the microorganisms in a biofilm, called persister cells, which were first identified by Joseph Bigger in 1944, contribute to the difference [51]. The persister cells are dormant and have little translation or topoisomerase activity, which enables resistance to killing by antibiotics. Reduced antimicrobial efficacy in biofilm-related disease results from the fact that almost all conventional antibiotics target the biosynthetic processes taking place in actively growing bacteria, including the biosynthesis of proteins, RNA, DNA, peptidoglycan and folic acid [52]. Therefore, conventional antibiotics show little efficacy in killing non-multiplying bacteria, in other words, persisters [53], and this is consistent with the result of our biofilm susceptibility assays, which showed that erythromycin exerted little inhibition of biofilm formation and preformed biofilm. However, biofilm susceptibility assays indicated that LN-7 could effectively inhibit the preformed biofilm of S. mutans at 10-fold MIC, and we further applied this concentration of LN-7 in the subsequent studies relevant to biofilm, including observation of the impairment of biofilm with CLSM and SEM, as well as the in vivo animal study [37, 54]. Results of the CLSM observation showed that compared with those in the control group and erythromycin group, the S. mutans biofilm in the LN-7 group appeared thinner and sparser, with more red signals in images, which indicated the effective antibacterial potency of LN-7, in agreement with those results of colony-forming count method. Furthermore, SEM images illustrated that biofilm treated with LN-7 was incompact and sparse, suggesting that combined with the use of mechanical cleaning, LN-7 may effectively eradicate biofilms.
The efficacy of LN-7 in inhibiting biofilm of S. mutans may be due to the mechanism of its antimicrobial activity. It was reported that AMPs function mainly based on the action on the bacterial membrane, which is different from the antimicrobial mechanism of conventional antibiotics [44], and may contribute to its rapid killing kinetics and less resistance selection, while other mechanisms of AMPs were also reported, such as intracellular targeting and activation of host cells immunomodulation [55]. We then preliminary explored the antibacterial mechanism of LN-7 and found that it was able to disrupt the membrane of bacteria, which was consistent with most peptides, especially those with fast killing kinetics [56]. However, further studies about the mechanism of the inhibition against the biofilm of S. mutans are needed, for example, the effect of LN-7 on extracellular polymeric substance, the matrix of biofilm.
To further assess the anti-caries effect of LN-7 in the complex oral environment, we used a well-established rodent model of dental caries [37,38,39]. Our findings corroborated that the LN-7 group performed significantly less enamel and slight dentinal lesions in the sulcal surface compared with the DDW group. Moreover, LN-7 groups also showed significantly less smooth surface lesions compared with the DDW group, even reaching the extent to NaF, which is considered as the gold standard in the prevention of caries [57]. In addition, it was reported that the accuracy of overall caries scores of rats can be enhanced by SEM images [42], and our results showed that SEM images could provide more detailed structure of the molars and exhibit the caries progression more clearly. The results of the animal study suggested that LN-7 may help to thwart the progression of dental caries in vivo. Notably, throughout the experiment, there were no signs of deleterious effects on the rats’ body weight or to the mucosa, suggesting the low local toxicity of LN-7. Nevertheless, full toxicity studies should be conducted to determine the long-term effects of daily topical applications of LN-7.
Dental caries is a multifactorial disease, whose progression is determined by a variety of factors, including the susceptible host, cariogenic microorganism, diet, and time. The key elements of anti-caries biological approaches lie in the use of remineralizing agents to the tooth structure and the regulation of cariogenic biofilms [58]. Our data supported that LN-7 exhibits certain capability of preventing dental caries, which may result from the anti-biofilm ability of LN-7 against S. mutans. However, the underlying mechanism requires further exploration.
In conclusion, this study clearly demonstrated the ability of a derivative of reutericin 6 and gassericin A to inhibit the biofilm of S. mutans UA159 and prevent dental caries in a rat model, justifying further studies under a broader range of cariogenic conditions, and the knowledge obtained in the study may provide a basis for the development of a feasible new anti-biofilm and anti-caries alternative product for therapeutic use.
References
Takahashi N, Nyvad B. The role of bacteria in the caries process: ecological perspectives[J]. J Dent Res. 2011;90(3):294–303.
Bernardi S, Continenza MA, Al-Ahmad A, et al. Streptococcus spp. and Fusobacterium nucleatum in tongue dorsum biofilm from halitosis patients: a fluorescence in situ hybridization (FISH) and confocal laser scanning microscopy (CLSM) study[J]. New Microbiol. 2019;42(2):108–13.
Bernardi S, Karygianni L, Filippi A, et al. Combining culture and culture-independent methods reveals new microbial composition of halitosis patients’ tongue biofilm[J]. Microbiologyopen. 2020;9(2):e958.
Bernardi S, Bianchi S, Botticelli G, et al. Scanning electron microscopy and microbiological approaches for the evaluation of salivary microorganisms behaviour on anatase titanium surfaces: in vitro study[J]. Morphologie. 2018;102(336):1–6.
Bernardi S, Bianchi S, Tomei AR, et al. Microbiological and SEM-EDS evaluation of titanium surfaces exposed to periodontal gel: in vitro study[J]. Materials. 2019;12(9):1448.
Patianna G, Valente NA, D’Addona A, et al. In vitro evaluation of controlled-release 14% doxycycline gel for decontamination of machined and sandblasted acid-etched implants[J]. J Periodontol. 2018;89(3):325–30.
Meza-Siccha AS, Aguilar-Luis MA, Silva-Caso W, et al. In vitro evaluation of bacterial adhesion and bacterial viability of Streptococcus mutans, Streptococcus sanguinis, and Porphyromonas gingivalis on the abutment surface of titanium and zirconium dental implants[J]. Int J Dent. 2019;2019:4292976.
Zijnge V, van Leeuwen MB, Degener JE, et al. Oral biofilm architecture on natural teeth[J]. PLoS One. 2010;5(2):e9321.
Kawada-Matsuo M, Komatsuzawa H. Role of Streptococcus mutans two-component systems in antimicrobial peptide resistance in the oral cavity[J]. Jpn Dent Sci Rev. 2017;53(3):86–94.
Min KR, Galvis A, Williams B, et al. Antibacterial and antibiofilm activities of a novel synthetic cyclic lipopeptide against cariogenic Streptococcus mutans UA159[J]. Antimicrob Agents Chemother. 2017;61(8):e00776-17.
Jiang W, Wang Y, Luo J, et al. Effects of antimicrobial peptide GH12 on the cariogenic properties and composition of a cariogenic multispecies biofilm[J]. Appl Environ Microbiol. 2018;84(24):e01423-18.
Guo L, McLean JS, Yang Y, et al. Precision-guided antimicrobial peptide as a targeted modulator of human microbial ecology[J]. Proc Natl Acad Sci USA. 2015;112(24):7569–74.
Zanatta FB, Antoniazzi RP, Rosing CK. Staining and calculus formation after 0.12% chlorhexidine rinses in plaque-free and plaque covered surfaces: a randomized trial[J]. J Appl Oral Sci. 2010;18(5):515–21.
McCormick TS, Weinberg A. Epithelial cell-derived antimicrobial peptides are multifunctional agents that bridge innate and adaptive immunity[J]. Periodontol 2000. 2010;54(1):195–206.
Guaní-Guerra E, Santos-Mendoza T, Lugo-Reyes SO, et al. Antimicrobial peptides: general overview and clinical implications in human health and disease[J]. Clin Immunol. 2010;135(1):1–11.
Sierra JM, Fuste E, Rabanal F, et al. An overview of antimicrobial peptides and the latest advances in their development[J]. Expert Opin Biol Ther. 2017;17(6):663–76.
Helmerhorst EJ, Hodgson R, Van‘t Hof W, et al. The effects of histatin-derived basic antimicrobial peptides on oral biofilms[J]. J Dent Res. 1999;78(6):1245–50.
Kreling PF, Aida KL, Massunari L, et al. Cytotoxicity and the effect of cationic peptide fragments against cariogenic bacteria under planktonic and biofilm conditions[J]. Biofouling. 2016;32(9):995–1006.
Tao R, Tong Z, Lin Y, et al. Antimicrobial and antibiofilm activity of pleurocidin against cariogenic microorganisms[J]. Peptides. 2011;32(8):1748–54.
Wang W, Tao R, Tong Z, et al. Effect of a novel antimicrobial peptide chrysophsin-1 on oral pathogens and Streptococcus mutans biofilms[J]. Peptides. 2012;33(2):212–9.
Maisetta G, Batoni G, Esin S, et al. Susceptibility of Streptococcus mutans and Actinobacillus actinomycetemcomitans to bactericidal activity of human beta-defensin 3 in biological fluids[J]. Antimicrob Agents Chemother. 2005;49(3):1245–8.
Ding Y, Wang W, Fan M, et al. Antimicrobial and anti-biofilm effect of Bac8c on major bacteria associated with dental caries and Streptococcus mutans biofilms[J]. Peptides. 2014;52:61–7.
Kang MS, Oh JS, Lee HC, et al. Inhibitory effect of Lactobacillus reuteri on periodontopathic and cariogenic bacteria[J]. J Microbiol. 2011;49(2):193–9.
Koll-Klais P, Mandar R, Leibur E, et al. Oral lactobacilli in chronic periodontitis and periodontal health: species composition and antimicrobial activity[J]. Oral Microbiol Immunol. 2005;20(6):354–61.
Soderling EM, Marttinen AM, Haukioja AL. Probiotic lactobacilli interfere with Streptococcus mutans biofilm formation in vitro[J]. Curr Microbiol. 2011;62(2):618–22.
Kawai Y, Ishii Y, Arakawa K, et al. Structural and functional differences in two cyclic bacteriocins with the same sequences produced by lactobacilli[J]. Appl Environ Microbiol. 2004;70(5):2906–11.
Torcato IM, Huang YH, Franquelim HG, et al. Design and characterization of novel antimicrobial peptides, R-BP100 and RW-BP100, with activity against Gram-negative and Gram-positive bacteria[J]. Biochim Biophys Acta. 2013;1828(3):944–55.
Won HS, Park SH, Kim HE, et al. Effects of a tryptophanyl substitution on the structure and antimicrobial activity of C-terminally truncated gaegurin 4[J]. Eur J Biochem. 2002;269(17):4367–74.
Zhu X, Zhang L, Wang J, et al. Characterization of antimicrobial activity and mechanisms of low amphipathic peptides with different alpha-helical propensity[J]. Acta Biomater. 2015;18:155–67.
Fang Y, Zhong W, Wang Y, et al. Tuning the antimicrobial pharmacophore to enable discovery of short lipopeptides with multiple modes of action[J]. Eur J Med Chem. 2014;83:36–44.
Eckert R, Qi F, Yarbrough DK, et al. Adding selectivity to antimicrobial peptides: rational design of a multidomain peptide against Pseudomonas spp[J]. Antimicrob Agents Chemother. 2006;50(4):1480–8.
Limsuwan S, Moosigapong K, Jarukitsakul S, et al. Lupinifolin from Albizia myriophylla wood: a study on its antibacterial mechanisms against cariogenic Streptococcus mutans[J]. Arch Oral Biol. 2018;93:195–202.
Chen Z, Yang G, Lu S, et al. Design and antimicrobial activities of LL-37 derivatives inhibiting the formation of Streptococcus mutans biofilm[J]. Chem Biol Drug Des. 2019;93(6):1175–85.
O’Toole GA, Kolter R. Initiation of biofilm formation in Pseudomonas fluorescens WCS365 proceeds via multiple, convergent signalling pathways: a genetic analysis[J]. Mol Microbiol. 1998;28(3):449–61.
Chatterjee A, Perevedentseva E, Jani M, et al. Antibacterial effect of ultrafine nanodiamond against Gram-negative bacteria Escherichia coli[J]. J Biomed Opt. 2015;20(5):51014.
Tu H, Fan Y, Lv X, et al. Activity of synthetic antimicrobial peptide GH12 against oral Streptococci[J]. Caries Res. 2016;50(1):48–61.
Kim D, Liu Y, Benhamou RI, et al. Bacterial-derived exopolysaccharides enhance antifungal drug tolerance in a cross-kingdom oral biofilm[J]. ISME J. 2018;12(6):1427–42.
Naha PC, Liu Y, Hwang G, et al. Dextran-coated iron oxide nanoparticles as biomimetic catalysts for localized and pH-activated biofilm disruption[J]. ACS Nano. 2019;13(5):4960–71.
Bowen WH. Rodent model in caries research[J]. Odontology. 2013;101(1):9–14.
Keyes PH. Dental caries in the molar teeth of rats. II. A method for diagnosing and scoring several types of lesions simultaneously[J]. J Dent Res. 1958;37(6):1088–99.
Naylor F, Aranha ACC, Eduardo CDP, et al. Micromorphological analysis of dentinal structure after irradiation with Nd:YAG laser and immersion in acidic beverages[J]. Photomed Laser Surg. 2006;24(6):745.
Yucesoy DT, Fong H, Gresswell C, et al. Early caries in an in vivo model: structural and nanomechanical characterization[J]. J Dent Res. 2018;97(13):1452–9.
Brogden KA. Antimicrobial peptides: pore formers or metabolic inhibitors in bacteria?[J]. Nat Rev Microbiol. 2005;3(3):238–50.
Takahashi D, Shukla SK, Prakash O, et al. Structural determinants of host defense peptides for antimicrobial activity and target cell selectivity[J]. Biochimie. 2010;92(9):1236–41.
Wiradharma N, Sng MY, Khan M, et al. Rationally designed alpha-helical broad-spectrum antimicrobial peptides with idealized facial amphiphilicity[J]. Macromol Rapid Commun. 2013;34(1):74–80.
Liang D, Li H, Xu X, et al. Rational design of peptides with enhanced antimicrobial and anti-biofilm activities against cariogenic bacterium Streptococcus mutans[J]. Chem Biol Drug Des. 2019;94:1768–81.
Deslouches B, Phadke SM, Lazarevic V, et al. De novo generation of cationic antimicrobial peptides: influence of length and tryptophan substitution on antimicrobial activity[J]. Antimicrob Agents Chemother. 2005;49(1):316–22.
Garcia SS, Blackledge MS, Michalek S, et al. Targeting of Streptococcus mutans biofilms by a novel small molecule prevents dental caries and preserves the oral microbiome[J]. J Dent Res. 2017;96(7):807–14.
Kaplan CW, Sim JH, Shah KR, et al. Selective membrane disruption: mode of action of C16G2, a specifically targeted antimicrobial peptide[J]. Antimicrob Agents Chemother. 2011;55(7):3446–52.
Fux CA, Costerton JW, Stewart PS, et al. Survival strategies of infectious biofilms[J]. Trends Microbiol. 2005;13(1):34–40.
Del PJ. Biofilm-related disease[J]. Expert Rev Anti Infect Ther. 2018;16(1):51–65.
Hurdle JG, O’Neill AJ, Chopra I, et al. Targeting bacterial membrane function: an underexploited mechanism for treating persistent infections[J]. Nat Rev Microbiol. 2011;9(1):62–75.
Coates AR, Hu Y. Targeting non-multiplying organisms as a way to develop novel antimicrobials[J]. Trends Pharmacol Sci. 2008;29(3):143–50.
Bueno-Silva B, Koo H, Falsetta ML, et al. Effect of neovestitol-vestitol containing Brazilian red propolis on accumulation of biofilm in vitro and development of dental caries in vivo[J]. Biofouling. 2013;29(10):1233–42.
Mai S, Mauger MT, Niu L, et al. Potential applications of antimicrobial peptides and their mimics in combating caries and pulpal infections[J]. Acta Biomater. 2017;49:16–35.
de Breij A, Riool M, Cordfunke RA, et al. The antimicrobial peptide SAAP-148 combats drug-resistant bacteria and biofilms[J]. Sci Transl Med. 2018;10(423):eaan4044.
Clarkson JJ, McLoughlin J. Role of fluoride in oral health promotion[J]. Int Dent J. 2000;50(3):119–28.
Baptista A, Kato IT, Prates RA, et al. Antimicrobial photodynamic therapy as a strategy to arrest enamel demineralization: a short-term study on incipient caries in a rat model[J]. Photochem Photobiol. 2012;88(3):584–9.
Acknowledgements
The work was supported by the Science and Technology Department of Guangdong Province of China (2018B030311047) and the Science and Technology Program of Guangzhou, China (201804010419).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10266_2020_529_MOESM1_ESM.docx
Fig. S1 Killing kinetics of LN-7 against S. mutans UA159, S. sobrinus ATCC33478 and S. gordonii ATCC10558. (DOCX 119 kb)
Rights and permissions
About this article
Cite this article
Liang, J., Liang, D., Liang, Y. et al. Effects of a derivative of reutericin 6 and gassericin A on the biofilm of Streptococcus mutans in vitro and caries prevention in vivo. Odontology 109, 53–66 (2021). https://doi.org/10.1007/s10266-020-00529-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-020-00529-5