Abstract
The aim of this study was to evaluate the removal of the smear layer by some commonly used (needle-and-syringe irrigation, sonic activation, ultrasonically activated irrigation) and new root canal irrigation strategies (negative pressure irrigation and polymer rotary file) using a novel approach by comparing pre- and post-experimental images. Prepared root canals (n = 50) were subjected to a split tooth model and divided into 5 groups (n = 10): (1) needle-and-syringe irrigation (control); (2) sonic activation (SA); (3) negative pressure irrigation with continuous warm activated irrigation and evacuation (CWA); (4) polymer finishing file (FF); (5) ultrasonically activated irrigation (UAI). Smear layer scores and percentage of open dentinal tubules (%ODT) were evaluated by 2 examiners before and after irrigation procedures, from the middle and apical thirds of the root canal, on scanning electron microscopic images. Data were analysed using Kruskal–Wallis and post hoc tests at P = 0.05. Needle-and-syringe irrigation (control) showed no significant difference (both smear score and %ODT) compared to the pre-experimental value (P > 0.05). All other groups showed lower smear scores and higher %ODT, compared to the control (P < 0.05). The lowest smear score and highest %ODT were observed in the CWA group, which was significantly different from all other groups (P < 0.05). SA group showed significantly higher smear scores and lower %ODT than FF or UAI (P < 0.05). CWA showed superior removal of smear layer in the middle and apical thirds of the root canal compared to the other irrigation strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Root canal instrumentation produces a layer of hard tissue debris on the root canal wall (i.e. smear layer), preventing the penetration of irrigants and intracanal medicaments into the dentinal tubules [1]. It may also reduce the adaptation of root filling materials to the root canal wall [2]. Removal of this accumulated hard tissue debris (AHTD) is a function of the irrigating solution and the delivery/agitation method. Conventionally, an irrigation regimen comprises sodium hypochlorite (NaOCl) followed by ethylene diamine tetraacetic acid (EDTA), both of which are delivered into the canal using a needle and syringe. From a chemical perspective, NaOCl dissolves the organic components while EDTA removes the inorganic components of the smear layer [3]. It has been reported that the clinical outcome of root canal treatment is improved when EDTA is used [4], which might be attributable to removal of the smear layer. A recent systematic review also concluded that smear layer removal improves the outcome of root canal treatment of primary teeth [5].
Irrigant delivery may be categorized into manual and mechanical techniques. Manual delivery involves injecting (positive pressure) irrigants with various needle designs, whereas mechanical techniques include the use of negative pressure or activation/agitation methods such as ultrasonic tip, sonic devices, brushes and polymer-based rotary files. Recently, an irrigant delivery system has been introduced (EndoIrrigator Plus™, Innovations Endo, Nasik, India) based on the concept of a continuous flow of heated sodium hypochlorite with negative pressure, hence also known as continuous warm activated irrigation and evacuation system (CWA). This device applies the principle of intracanal suction (via a single use 30G side-vented needle) and warm irrigant (50 °C). The heater can be switched off when the operator does not wish to use a warm irrigating solution. A recent study indicated that this method was able to clean the isthmus of mandibular molars significantly better than syringe irrigation, manual dynamic agitation and passive ultrasonic irrigation [6].
The endodontic literature is replete with studies of smear layer removal, often evaluated using a qualitative method. De-Deus et al. [7] commented that qualitative studies evaluating the smear layer after final irrigation, without taking the pre-treatment status into account should be considered invalid. The authors suggested co-site optical microscopy as a viable technique to evaluate the effect of different irrigating solutions on dentin. However, that technique will be unable to study the effect of irrigant activation. Qualitative studies of smear layer removal are considered less robust because of two reasons: (1) possible bias in image acquisition and interpretation, (2) lack of knowledge of the sclerotic dentin (due to unknown age of the teeth or possible pathological insults) in those teeth prior to the experiment [7, 8]. To overcome these problems, an experimental design whereby the tooth is examined by SEM prior to use of irrigating solution(s) and by evaluating the percentage of open dentinal tubules would be indicated.
Ultrasonically activated irrigation (UAI), sonic device (EndoActivator®; Dentsply Tulsa Dental Specialties, Tulsa, OK, USA) and EndoVac (Kerr Corporation, Oranga, California, USA) have all resulted in superior removal of smear layer in straight [9] and curved root canals [10] when compared to needle-and-syringe irrigation. Smear layer removal of the first two systems appeared to decline along the depth of the root canal system, whereas the EndoVac demonstrated significantly better results at locations closer to the apical foramen [9].
The efficacy of EndoIrrigator Plus on the removal of the smear layer has not yet been documented. The aim of this study was to compare the efficacy of smear layer removal by various irrigation strategies using an in vitro model that allows the preoperative evaluation of the dentin surface prior to SEM analysis. The null hypotheses were that (1) there was no significant difference in smear layer removal, and (2) in the percentage of open dentinal tubules, between different irrigation methods tested.
Materials and methods
Single-rooted mandibular first premolars (n = 50), extracted from patients in the age group of 13–18 for orthodontic reasons were collected after informed consent was obtained from the patients or their parents. Any root with caries, preexisting root canal treatment, fractures or cracks were discarded. Radiographs were taken in two directions to confirm the presence of a single root canal. The results of a pilot study allowed us to calculate that 10 specimens were needed per group to obtain results with a power of 80%.
Pre-operative evaluation
The split-tooth model used in this study was modified from that of Schmidt et al. [11]. Teeth were cleaved using a chisel and mallet. Longitudinal reference grooves of 0.5 mm depth were first made on root dentin near the root canal wall, to serve as a guide for indicating the standard locations where all microscopic assessments would be made later. The specimens were placed in an ultrasonic bath with 3% NaOCl for 5 min, followed by 17% EDTA for 2 min to dissolve the pulp tissues and to open up the dentinal tubules. The root canal wall at the location of the grooves marked earlier was examined using a low-vacuum environmental scanning electron microscope (eSEM; Quanta 650 FEG, FEI, Hillsboro, OR, USA).
The specific reason for using the eSEM is because no specimen preparation or sputter coating is required, and the samples can be reused for further analysis. This step was considered important as it ensures that the root canal walls had open dentinal tubules and hence the results obtained were not due to the presence of sclerotic dentin. This data was not used in the statistical analysis but only served to ensure homogeneity. The cleaved roots were reassembled using a light curing resin barrier (OpalDam, Ultradent Products, South Jordan, UT, USA). The root apex was covered with sticky wax and placed in a polyvinyl siloxane casing to simulate a closed apical system in vivo [12].
Root canal preparation
Root canals were prepared with MTwo rotary instruments (VDW GmBH, Munich, Germany) to an apical size of 35 and 0.04 taper and irrigated with 5 mL of 3% NaOCl (Parcan; Septodont, Saint-Maur-des-Fosses, France) through a 30G side-vented needle (NaviTip, Ultradent Products) placed passively to about 2 mm from the apical foramen without binding. Apical patency was maintained with #10 K-file. After instrumentation, canals were irrigated with 3 mL distilled water and dried with absorbent paper points.
The prepared specimens were randomly divided into 5 groups and examined again under the eSEM to confirm the presence of a smear layer. Photomicrographs at 500× and 1000× were graded using a method described below. The pre-experimental micrographs were taken to verify the extent of the smear layer formed, which in all groups was homogenously distributed. These values were labelled as “pre-experimental smear scores”.
Irrigation procedures and assessment of the smear layer
Specimens were reassembled and subject to one of the five irrigation protocols (n = 10 each).
Group 1 (needle-and-syringe irrigation)
A 30G needle (NaviTip, Ultradent) was used to deliver 10 mL of 3% NaOCl over a period of 90 s. This was followed by 3 mL of 17% EDTA, which was left within the root canal for 2 min. The root canals were then rinsed with 2 mL of distilled water for 1 min.
Group 2 (sonic activation)
The EndoActivator (Dentsply Sirona Endodontics, USA) was used with the red tip (25/0.04) at 10000 cycles/min. An activation cycle of 30 s was performed until 10 mL of 3% NaOCl was used. The total activation time was 90 s. Following this, 3 mL of 17% EDTA was activated for 60 s. A total contact time of 2 min was allowed for the EDTA solution. A final rinse of 2 mL distilled water was performed which was activated with the same tip for 1 min.
Group 3 (CWA)
The EndoIrrigator Plus (Innovations Endo) device was used for this purpose. In the first step, 10 mL of 3% NaOCl was delivered over a period of 90 s with the “Warmer” mode on. This was followed by 3 mL of 17% EDTA solution delivered over a period of 1 min (with the warmer mode switched off), which was allowed to remain for 2 min in total. A final rinse of distilled water (2 mL) was delivered over a period of 1 min with the warmer mode switched off.
Group 4 (FF)
Finishing file (Engineered Endodontics, Menomonee Falls, WI, USA) size 20/0.04 taper was used at 900 rpm. The first activation cycle involved activation of 3% NaOCl in 30 s cycles until 10 mL of the solution was used. The total activation time was 90 s. This was followed by activation of 3 mL of 17% EDTA for 60 s with a total contact time of 2 min. A final rinse of 2 mL distilled water was performed which was activated with the same tip for 1 min.
Group 5 (UAI)
An IrriSafe tip (Satelec, Acteon Group, Merignac Cedex, France) was used in a Suprasson P5 Booster ultrasonic unit (Satelec) with a power setting of 3, as per the manufacturer’s instructions. The first step involved activation of 3% NaOCl in cycles of 30 s until 10 mL of the solution was used. The total activation time was 90 s. Following this, 3 mL of 17% EDTA was activated for 60 s with a total contact time of 2 min. A final rinse of 2 mL distilled water was performed which was activated with the same tip for 1 min.
Caution was exercised to standardise the volume, contact time and activation time of each of the irrigants in all the groups. The instrument tip in all the groups was placed 1 mm short of the working length (WL). The CWA was used with the “Warmer” mode on while delivering NaOCl while the warmer mode was switched off when delivering EDTA and distilled water. Canals were rinsed with distilled water and dried with paper points. Teeth were then coded for blinded evaluation by two calibrated examiners.
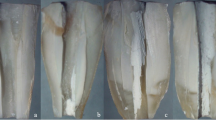
Each tooth was separated into their two halves along the cleavage created earlier and both the halves were processed for examination using SEM after gold sputtering. Micrographs obtained at 1000× were analysed using ImageJ software (1.48v, US National Institutes of Health, Bethesda, MA, USA) to determine the percentage area of open dentinal tubules in relation to the image area (%ODT). This was based on a robust methodology published earlier [11]. Furthermore, images taken at five random locations at the apical and middle thirds of the canal were graded based on the criteria proposed by Hülsmann et al. [13]: score 1—no smear layer, dentinal tubules open; score 2—small amount of smear layer, some dentinal tubules open; score 3—homogenous smear layer covering the root canal wall, only few dentinal tubules open; score 4—complete root canal wall covered by homogenous smear layer, no open dentinal tubules; score 5—heavy, non-homogenous smear layer covering the complete root canal wall. The scoring was performed independently by the 2 examiners and, in case of disagreement, the image was discussed to reach a consensus.
Data analysis
Intra- and inter-examiner reliability was verified (kappa test). The pre- and post-experimental smear were presented as mean ± standard deviation. Data were analysed using Kruskal–Wallis and Mann–Whitney U tests. Post hoc multiple comparisons were performed with Bonferroni test at a significance level of P = 0.05. The %ODT was calculated from both examiners and averaged, then analysed using the Kruskal–Wallis test, followed by non-parametric analysis of variance for multiple comparisons with Bonferroni correction to identify any differences.
Results
The pre-operative evaluation of all samples demonstrated a score of 1 (no smear layer, dentinal tubules open). After root canal preparation, there was no significant difference in the mean pre-experimental smear score and %ODT between groups (P > 0.05). There was excellent agreement between the two examiners (k = 0.90).
The post-irrigation examination showed that the needle-and-syringe group demonstrated a homogenous hard tissue debris covering the entire wall in the middle and apical third of the canal. The smear score and %ODT for this group was comparable to the pre-experimental smear scores (P > 0.05); the %ODT was 9 ± 1.1 and 3 ± 1.12 in the middle and apical root thirds, respectively. Canals irrigated with all other methods showed significantly lower smear scores in the middle and apical third, compared with their respective pre-experimental figures (P < 0.05). The mean of smear scores and average %ODT for all groups are summarised in Table 1.
Sonic activation showed patches of smear layer in the middle third, while the apical third was covered with a relatively homogenous smear layer with few open tubules (10 ± 1.21 %ODT). There was no significant difference between the FF and UAI group (P > 0.05), while they both had a smear score significantly lower than sonic activation (P < 0.05). Specimens irrigated with the CWA group showed no smear layer in the middle third in most of the samples, while the apical third had significantly less smear scores than all other groups (P < 0.05). Analysis of the SEM images revealed that the apical third of specimens irrigated using the CWA system showed no (score 1) (64%) or a small amount of hard tissue debris (score 2) (36%) in the apical third (Fig. 1).
There was a spatial difference in the %ODT along the root. It was noted that the middle third had significantly higher %ODT values in all groups, followed by the apical third. In the apical third, the CWA group showed the highest %ODT value followed by the finishing file (P < 0.05).
Discussion
The present study presented a novel approach to study the smear layer by comparing the pre- and post-irrigation images. A previous study by Schmidt et al. [11] employed a similar design but evaluated the smear layer only after root canal preparation. Our results indicated that the preoperative evaluation (baseline) showed no smear layer, with patent dentinal tubules, a result that is expected for non-instrumented root canal walls. Analysis of the specimens after root canal preparation, but prior to irrigant activation (pre-experimental smear score) showed that 38 samples demonstrated a score of 4 (complete root canal wall covered by homogenous smear layer with no open dentinal tubules) while 12 samples showed a score of 5 (heavy, non-homogenous smear layer covering completely the root canal walls), with no significant difference between the 5 groups prior to the different experimental irrigation regimens. This is reassuring, as all protocols were then tested on canals with hard tissue debris of similar extent. Furthermore, the teeth were extracted from young individuals and the presence of sclerotic dentin in the middle and apical third of these roots is highly unlikely [14]. The effect of this variable that might influence the result would be eliminated.
The ability of root canal irrigants to effectively reach anatomic spaces within the confines of the root canal system is essential to bring about tissue dissolution, biofilm destruction and removal of the smear layer [15, 16]. Several authors have recommended the removal of smear layer which may act as a substrate for bacteria [17], can prevent optimal diffusion of disinfecting agents [18], compromising the coronal [19] and apical seal [20], and may serve as an avenue for recontamination of the root canal system [21,22,23]. While the exact clinical relevance of smear layer in endodontics remains controversial, its removal may be considered as a parameter for which the effectiveness of irrigant delivery/activation systems may be compared. Since the apical portion of the canal is considered a critical area for root canal cleaning, only the middle and apical third were evaluated in this study.
A “closed” root canal system model was used to enhance the clinical relevance of this study [11, 24]. The presence of an entrapped air bubble (vapor lock) can impede effective irrigant exchange at the apical third of the root canal system [12]. Understandably, conventional needle-and-syringe irrigation was unable to remove the smear layer to any significant degree, in accordance with other reports [9, 10]. As there was significant difference between the irrigant activation methods in the removal of the smear layer, the first null hypothesis was rejected.
Irrigant activation enhances the kinetics and penetration, thereby increasing the efficiency [25, 26]. With the exception of needle-and-syringe irrigation, all other methods were able to remove the smear layer, leaving a canal wall with a good amount of open dentinal tubules. Therefore, the second null hypothesis had to be rejected too. This study tested, in addition to the conventional syringe delivery, four other irrigation protocols: sonic (SA), ultrasonic, polymer finishing file (FF) and a negative pressure delivery system. While the first three may be considered as activation/agitation systems, the fourth is a delivery system that draws irrigant by negative pressure via a needle placed near the apical third of the root canal system, which would eliminate the vapor lock [27].
A literature search showed that two negative pressure delivery devices have been studied in the past: EndoVac and Safety Irrigator (Vista Dental, Racine, WI, USA). The EndoVac has been reported to be superior to sonic and ultrasonic systems in removing the smear layer from apical third of root canals [27]. The CWA device (EndoIrrigator Plus), in principle, is similar to the EndoVac, but with an option to heat the irrigating solution. The smear scores in the apical third ranged between 1 and 2 when this device was used for irrigation. The superior efficiency of negative-pressure irrigation in debridement of the root canal systems may be attributed to an increase in the volume of solution delivered [28], and continuous replenishment of the solution [29]. Increased temperature of the irrigant and the ability to place the irrigating needle up to 1 mm short of the working length would also help [6]. Heated NaOCl, followed by EDTA, has been shown to be effective in removing smear layer than other irrigants [30]. This could be a reason behind the superior action of the CWA approach. Complete removal of smear layer occurs when the apical diameter is at least 0.30 in diameter [31]. In this study, all root canals were apically enlarged to a size of 0.35, which could account for the cleaner canals. Future studies should compare the two negative-pressure irrigant delivery systems (EndoVac and EndoIrrigator Plus).
UAI was able to remove significantly more smear layer and open up more dentinal tubules, compared to the sonic system in the present study. The endodontic literature is inconsistent with regard to the effects of ultrasonic and sonic activation on smear layer removal [9, 22, 23], probably due to the fact that there is no “ideal” recommended protocol for UAI [16]. Parameters for all the activation protocols were standardized in this study (time and volume of irrigating solution). Low frequency, low flow velocity and increased wall contact of the tip with the root canal walls (resulting in no cavitation effects) could have resulted in lesser efficiency of SA compared with UAI [27, 32,33,34,35].
This study seems to be the first to report on the efficacy of the finishing file in removing the AHTD. This single-use polymeric instrument has an offset flute design, tip size of 20 and taper of 0.04. This study indicated that FF is a superior method to remove smear layer than syringe irrigation or sonic agitation, producing a level of cleanliness comparable to UAI. Although the exact mechanism is not known, a similar plastic file (F-file, Plastic Endo, Buffalo Grove, IL) was reported to be able to remove debris from root canals and isthmus of mandibular molars to a similar extent as UI [36]. The main difference between the F-file and finishing file is the presence of a diamond coating on the F-file, which was speculated to induce the formation of a smear layer. Future studies should compare the F-file and finishing file.
In the present study, both the irrigating solutions and the final rinse with distilled water were agitated/delivered for all experimental groups. Thus far, only one study has performed this design [11]. This is important to note that loose debris generated by the irrigation/activation protocol may settle along the canal walls. To fully realize the target of smear layer removal to allow penetration of irrigants, intracanal medicaments and root filling materials, it is essential to remove the smear plug which may extend up to 40 µm into the dentinal tubules, to open up the dentinal tubules [37, 38]. The %ODT noticed in the apical third of specimens in this present study indicated the following order of effectiveness: CWA > finishing file > UAI > sonic activation > needle-and-syringe irrigation. In the middle third, however, there was no significant difference between the finishing file and UAI. It may be noted that the results of the percentage of open tubules correlated to the smear scores well, thereby increasing the validity of the study. Future studies should aim at evaluating the depth of cleanliness brought about by these systems.
Only teeth with straight root canals were used in this study. Future research should demonstrate the effectiveness of these strategies in canals with moderate to severe curvatures. This is especially important, considering that only one of the devices used in this study (EndoActivator) used a flexible polymeric tip. Another aspect to be taken into consideration is that we did not specifically measure the apical diameters of the root canals prior to root canal preparation. Given that the premolars were collected from relatively young patients, the apical sizes may be quite variable. However, it was our intention to focus on the irrigant activation strategies immaterial of the original apical sizes. Furthermore, when the roots were split, we observed that none of the roots had large apical diameters and all the roots split evenly, validating the methodology.
Conclusions
Conventional needle-and-syringe irrigation was unable to remove the smear layer from the middle and apical third of root canals. The CWA irrigation and evacuation system (EndoIrrigator Plus) was the most effective in reducing the smear layer, followed by the finishing file and UAI. Ultrasonic irrigation was more effective than sonic activation in removing the smear layer. The percentage of open dentinal tubules followed the same order as removal of the smear layer. Future studies should evaluate the effects of irrigating solution activation after delivery with negative pressure irrigation systems, and/or possibly compare the CWA to EndoVac.
References
Wang Z, Shen Y, Haapasalo M. Effect of smear layer against disinfection protocols on Enterococcus faecalis-infected dentin. J Endod. 2013;39:1395–400.
Violich DR, Chandler NP. The smear layer in endodontics—a review. Int Endod J. 2010;43:2–15.
Carvalho AS, Camargo CH, Valera MC, Camargo SE, Mancini MN. Smear layer removal by auxiliary chemical substances in biomechanical preparation: a scanning electron microscope study. J Endod. 2008;34:1396–400.
Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J. 2011;44:583–609.
Pintor AV, Dos Santos MR, Ferreira DM, Barcelos R, Primo LG, Maia LC. Does smear layer removal influence root canal therapy outcome? A systematic review. J Clin Pediatr Dent. 2016;40:1–7.
Neelakantan P, Devaraj S, Jagannathan N. Histologic assessment of debridement of the root canal isthmus of mandibular molars by irrigant activation techniques ex vivo. J Endod. 2016;42:1268–72.
De-Deus G, Reis C, Paciornik S. Critical appraisal of published smear layer-removal studies: methodological issues. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:531–43.
Lottanti S, Gautschi H, Sener B, Zehnder M. Effects of ethylenediaminetetraacetic, etidronic and peracetic acid irrigation on human root dentin and the smear layer. Int Endod J. 2009;42:335–43.
Mancini M, Cerroni L, Iorio L, Armellin E, Conte G, Cianconi L. Smear layer removal and canal cleanliness using different irrigation systems (EndoActivator, EndoVac, and passive ultrasonic irrigation): field emission scanning electron microscopic evaluation in an in vitro study. J Endod. 2013;39:1456–60.
Blank-Goncalves LM, Nabeshima CK, Martins GH, Machado ME. Qualitative analysis of the removal of the smear layer in the apical third of curved roots: conventional irrigation versus activation systems. J Endod. 2011;37:1268–71.
Schmidt TF, Teixeira CS, Felippe MC, Felippe WT, Pashley DH, Bortoluzzi EA. Effect of ultrasonic activation of irrigants on smear layer removal. J Endod. 2015;41:1359–63.
Tay FR, Gu LS, Schoeffel GJ, Wimmer C, Susin L, Zhang K, Arun SN, Kim J, Looney SW, Pashley DH. Effect of vapor lock on root canal debridement by using a side-vented needle for positive-pressure irrigant delivery. J Endod. 2010;36:745–50.
Hulsmann M, Rummelin C, Schafers F. Root canal cleanliness after preparation with different endodontic handpieces and hand instruments: a comparative SEM investigation. J Endod. 1997;23:301–6.
Vasiliadis L, Darling AI, Levers BG. The amount and distribution of sclerotic human root dentin. Arch Oral Biol. 1983;28:645–9.
Basmadjian-Charles CL, Farge P, Bourgeois DM, Lebrun T. Factors influencing the long-term results of endodontic treatment: a review of the literature. Int Dent J. 2002;52:81–6.
Gu LS, Kim JR, Ling J, Choi KK, Pashley DH, Tay FR. Review of contemporary irrigant agitation techniques and devices. J Endod. 2009;35:791–804.
George S, Kishen A, Song KP. The role of environmental changes on monospecies biofilm formation on root canal wall by Enterococcus faecalis. J Endod. 2005;31:867–72.
Baumgartner JC, Mader CL. A scanning electron microscopic evaluation of four root canal irrigation regimens. J Endod. 1987;13:147–57.
Saunders WP, Saunders EM. The effect of smear layer upon the coronal leakage of gutta-percha fillings and a glass ionomer sealer. Int Endod J. 1992;25:245–9.
Yang SE, Bae KS. Scanning electron microscopy study of the adhesion of Prevotella nigrescens to the dentin of prepared root canals. J Endod. 2002;28:433–7.
Cameron JA. The use of ultrasound for the removal of the smear layer. The effect of sodium hypochlorite concentration; SEM study. Aust Dent J. 1988;33:193–200.
Rodig T, Dollmann S, Konietschke F, Drebenstedt S, Hulsmann M. Effectiveness of different irrigant agitation techniques on debris and smear layer removal in curved root canals: a scanning electron microscopy study. J Endod. 2010;36:1983–7.
Prado M, Gusman H, Gomes BP, Simao RA. Scanning electron microscopic investigation of the effectiveness of phosphoric acid in smear layer removal when compared with EDTA and citric acid. J Endod. 2011;37:255–8.
de Gregorio C, Estevez R, Cisneros R, Paranjpe A, Cohenca N. Efficacy of different irrigation and activation systems on the penetration of sodium hypochlorite into simulated lateral canals and up to working length: an in vitro study. J Endod. 2010;36:1216–21.
Haapasalo M, Shen Y, Wang Z, Gao Y. Irrigation in endodontics. Br Dent J. 2014;216:299–303.
Mozo S, Llena C, Forner L. Review of ultrasonic irrigation in endodontics: increasing action of irrigating solutions. Med Oral Patol Oral Cir Bucal. 2012;17:e512-6.
Jiang LM, Verhaagen B, Versluis M, van der Sluis LW. Evaluation of a sonic device designed to activate irrigant in the root canal. J Endod. 2010;36:143–6.
Moorer WR, Wesselink PR. Factors promoting the tissue dissolving capability of sodium hypochlorite. Int Endod J. 1982;15:187–96.
Saber Sel D, Hashem AA. Efficacy of different final irrigation activation techniques on smear layer removal. J Endod. 2011;37:1272–5.
Wu L, Mu Y, Deng X, Zhang S, Zhou D. Comparison of the effect of four decalcifying agents combined with 60 °C 3% sodium hypochlorite on smear layer removal. J Endod. 2012;38:381–4.
Khademi A, Yazdizadeh M, Feizianfard M. Determination of the minimum instrumentation size for penetration of irrigants to the apical third of root canal systems. J Endod. 2006;32:417–20.
Lee SJ, Wu MK, Wesselink PR. The efficacy of ultrasonic irrigation to remove artificially placed dentin debris from different-sized simulated plastic root canals. Int Endod J. 2004;37:607–12.
Capar ID, Aydinbelge HA. Effectiveness of various irrigation activation protocols and the self-adjusting file system on smear layer and debris removal. Scanning. 2014;36:640–7.
Malki M, Verhaagen B, Jiang LM, Nehme W, Naaman A, Versluis M, Wesselink P, van der Sluis L. Irrigant flow beyond the insertion depth of an ultrasonically oscillating file in straight and curved root canals: visualization and cleaning efficacy. J Endod. 2012;38:657–61.
Sabins RA, Johnson JD, Hellstein JW. A comparison of the cleaning efficacy of short-term sonic and ultrasonic passive irrigation after hand instrumentation in molar root canals. J Endod. 2003;29:674–8.
Klyn SL, Kirkpatrick TC, Rutledge RE. In vitro comparisons of debris removal of the EndoActivator system, the F file, ultrasonic irrigation, and NaOCl irrigation alone after hand-rotary instrumentation in human mandibular molars. J Endod. 2010;36:1367–71.
Mader CL, Baumgartner JC, Peters DD. Scanning electron microscopic investigation of the smeared layer on root canal walls. J Endod. 1984;10:477–83.
White RR, Goldman M, Lin PS. The influence of the smeared layer upon dentinal tubule penetration by endodontic filling materials. Part II. J Endod. 1987;13:369–74.
Acknowledgements
The authors sincerely thank Ms. Samantha Kar Yan Li, Centralized Research Laboratories, Faculty of Dentistry, The University of Hong Kong for the data analysis.
Funding
This study did not receive any funding from internal or external sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Neelakantan, P., Ounsi, H.F., Devaraj, S. et al. Effectiveness of irrigation strategies on the removal of the smear layer from root canal dentin. Odontology 107, 142–149 (2019). https://doi.org/10.1007/s10266-018-0373-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-018-0373-2