Abstract
The aim of this in vitro study was to determine the influence of the order of composite layers’ stratification on resin composites color and appearance when restoring an anterior composite tooth on the 3D color coordinates L*a*b* by use of a spectrophotometer. A total of 192 discs samples made of two different commercial available composite materials (Miris 2 and HRI) of enamel (E) and dentin (D) shade, each with a 1 mm thickness, were divided into 6 configurations. The superposition of 4 samples for a total of 16 specimens per group determined the investigated configurations. All groups showed significant (p < 0.05) differences between them except groups E1DDE and EDDE1 which represent the same order of stratification, measured from the buccal side and from the palatal side. Perceptible differences were detected between all groups except for E1DDE, EDDE1 and EDDD, independent of the background (white or black). The realization of the palatal layer with dentin composite shade did not change the final outcome within the limit of a total 4 mm thickness in comparison to the palatal layer with enamel composite shade.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The importance of external appearances and the cosmetic parameters dictated by modern society have led to an increase in esthetic demands. Additionally, the development of composite restoration materials has broadened their indication in the field of esthetic restorative procedures.
Human teeth are multi-layered structures composed of dentin and enamel, both of which have differing optical characteristics. Enamel is more translucent but has a lower chroma, while dentin is opaque and more saturated [1]. To mimic these two natural substrates, two artificial restorative materials are available: Composite resins and ceramics. Composite resins are currently used to improve smile esthetics to achieve satisfactory results through a minimally invasive approach at relatively low cost and with a relatively high clinical performance [2, 3].
To enhance esthetics, composites can be applied following different incremental techniques to manage polymerization stresses and achieve a predictable esthetic outcome. Composite layering is often based on two different shades of the material, enamel and dentin, with different opacities and colors, with the goal to mimic the natural anatomy and appearance of a tooth. The restorative approach of layering, often called stratification, has been described as the “anatomic build-up technique” [1], the “trendy three-layer concept” [4] or the “natural layering concept” [5, 6].
Even if there is a general consensus regarding the necessity of a layering technique, there has been no study in the literature so far that evaluated the optical influence of each layer on the final outcome of the restoration. To perform an optical evaluation of the color of the entire restoration, two methods are possible: one based on a qualitative approach using human eyes but subject to bias due to perception limits and a quantitative method based on the use of quantitative instruments, such as a colorimeter or a spectrophotometer. The latter is preferred, as it is more precise due to a more accurate spectral analysis [7–10].
The aim of this in vitro study was to determine the influence of stratification of two brands of composite on the 3D color coordinates CIE L*a*b* [11] using a spectrophotometer. The CIE L*a*b* system defines a color space along two axes, a* from −a* (cyan) to +a* (magenta) and b* from −b* (blue) to +b* (yellow). L* stands for lightness ranging from 0 (black) to 100 (white).
The first null hypothesis was that the order of layers does not significantly influence the final L*a*b* values. The second null hypothesis was that the order of the layers does not influence the visual perception of the final optical result (ΔΕ ab < 1.1).
Materials and methods
Two micro hybrid resin composites (Table 1) were evaluated in this study: Miris 2 and HRI. In both materials, an enamel and a dentin shade were selected.
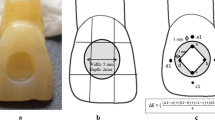
For each of the two resin composites evaluated, a total of 192 samples were readied. 48 samples of Miris 2 NR enamel, 48 samples of Miris 2 S3 dentin, 48 samples of HRI UE2 enamel and 48 samples of HRI UD3 dentin of 1 mm thickness each were divided into 6 configurations (groups) made out of the superposition of 4 samples (Fig. 1) for a total of 16 specimens per group. The different samples, unpolished to reflect the clinical situation of the internal layers, have been superposed each other without the interposition of any medium, avoiding any possible bias on the optical results. A slight notch done by means of a scalpel was made to be able to superimpose the samples according to the same orientation.
a 1 mm of enamel covering (E) layer, then 2 mm of dentin (D) and finally 1 mm of underlying enamel layer. b same configuration as 1 but measured from the side of the previous underlying layer. c 2 mm of dentin on the top and then 2 mm of enamel. d 2 mm of enamel on the top and then 2 mm of dentin. e 3 mm of enamel on the top and then 1 mm of dentin. f 1 mm of enamel on the top and then 3 mm of dentin
The configurations based on the enamel (E) and on the dentin (D) shade of two different composite brands were as follows:
-
EDDE (E1DDE and EDDE1) represented the gold standard stratification: one layer of palatal enamel (represented by one sample of enamel shade. “E”), the body of dentin (represented by 2 layers of dentin shade “DD”) and one layer of buccal enamel (represented by one sample of enamel shade “E”).
-
The configuration EDDD replaced the palatal layer of enamel by a layer of dentin.
-
The configuration EEED mimicked the situation of the interproximal part and the incisal edge when the palatal part is replaced by a layer of dentin.
-
The configurations EEDD, DDEE completed the possible combinations.
The layer facing the measuring window of the spectrophotometer was defined as the covering (=vestibular) layer, while the layer in contact with the background was defined as the underlying (=oral) layer.
Each sample was a cylindrical composite disc with a diameter of 10 mm and 1.0 ± 0.05 mm thickness checked by means of a digital calliper, (digit-cal capaμsystem®, serial number 8R565806, TESA, Renens, Switzerland) that was obtained by pressing a defined amount of material between 2 microscope glass slides.
Every sample was light cured for 20 s using a 1100mW/cm2 LED light curing unit (Bluephase, serial no 1523817, Ivoclar Vivadent, Schaan, Liechtenstein), stored in artificial saliva and maintained for 7 days at constant temperature of 37 °C in an incubator (Memmert Universal, Wisconsin Oven Corporation, WI, USA) in the absence of light.
A calibrated reflectance spectrophotometer (SpectroShade Handy Dental Type 713000, serial no HDL2891, Medical High Technologies, Arbizzano di Negar, Italy) was used with the optical parameters of each specimen over a white (L* = 92.6, a* = −1.2, b* = 2.9) and black (L* = 1.6, a* = 1.2, b* = −1.0) background made of plasticized paper. L*, a* and b* are the three dimensions of color. The parameters taken into account, according to the official recommendations of the International Commission on Illumination of 1976, were L* (luminosity from 0 (black) to 100 (white); similar to value), a* (red-green axis from −300 to +299: positive value indicates red, negative indicates green) and b* (yellow-blue axis from −300 to +299: a positive value indicates yellow; negative indicates blue).
Thereafter, color differences between pairs of groups (Tables 2, 3, 4 and 5) were calculated according to the following formula: \(\Delta\text{E}_{\text{ab}}\,=\, \sqrt {({L_{1}-L_{2}})^2 + ({a_{1}-a_{2}})^2 + ({b_{1}-b_{2}})^2 }\) [2] where 1 and 2 represented the two groups. Table 6 gives the standard deviations of the laboratory measures. Concerning physiological perceptibility of differences in ΔΕ ab, values ranging from 0.0 to 1.1 were considered as not perceptible, between 1.1 and 3.3 as visually perceptible but clinically acceptable while all ΔΕ ab higher than 3.3 were considered as clearly visible and clinically disturbing [12–15].
In addition to the perceptibility evaluation, a first explorative analysis of the L*a*b* measures for the four composites and backgrounds (Miris black background, Miris white background, HRI black background, HRI white background) was performed. The 192 measures were plot in a two-dimensional plane resulting from Multidimensional Scaling (MDS).
To check the possible groups’ equivalence in terms of L*a*b*, a Kruskal–Wallis test was run.
Results
The ΔΕ ab results in the HRI groups ranged from 0.6 to 8.3 against a white background and from 0.6 to 8.8 against a black background (Tables 2 and 3). The ΔΕ ab results in the Miris 2 groups ranged from 0.2 to 9.3 against a white background and from 0.2 to 10.9 against a black background (Tables 4, and 5).
The result of the Multidimensional Scaling (MDS) is illustrated in Fig. 2. Each number represents one of the L*a*b* measures, the labels refers to the group the observations are part of and the ellipses represent the dispersion of data around the group centroid (group median of L*a*b*). The objective of MDS is to visualize the dissimilarities between the observations of a dataset in a low-dimensional space such that the distances correspond as close as possible to the dissimilarities. The distances among the observations plotted in Fig. 2 are representative of the actual ΔΕ ab measures.
As a matter of fact, the following result can be put in evidence:
-
Group 3 (DDEE) is always separate for the other groups.
-
Groups 1, 2 and 5 (E1DDE, EDDE1 and EDDD) are partially overlapping.
-
The observations per group are closer (i.e., there is less dispersion around the group median) for Miris rather than HRI composite.
Under the light of the MDS analyses and considering the ellipses overlapping, a Kruskal–Wallis test was run to test the following hypothesis:
-
Groups 1 and 2 (E1DDE, EDDE1) are equivalent: E1DDE = EDDE1.
-
Groups 1, 2 and 5 (E1DDE, EDDE1, EDDD) are equivalent: E1DDE = EDDE1 = EDDD.
-
Groups 4 and 6 (EEDD, EEED) are equivalent: EEDD = EEED.
The results of that Kruskal–Wallis test are given in Table 7. Therefore, it is possible to sustain that, except for E1DDE and EDDE1 that can be considered to be substantially equivalent (p values > 0.05), significant differences among all the other stratifications (p values < 0.001) have been detected.
Regarding the human eyes capacity, physiologically perceptible differences (ΔΕ ab > 1.1) [12] were detected between all groups, except for E1DDE, EDDE1 and EDDD for HRI and Miris 2 (ΔΕ ab < 1.1), independent of the considered background (Tables 2, 3, 4 and 5).
Discussion
There is a common trend among practitioners to layer enamel and dentin composite materials according to the actual thickness of the missing natural enamel and dentin. However, no composite behaves exactly as natural enamel or dentin and no single model has provided an exact solution to the problem of matching color of restorative materials to that of natural dentition so far.
Therefore, within the concept of stratification, the question of the importance of the order of placement of the different layers may arise. It is possible that the standard three-layer stratification may be replaced by a simplified two-layer stratification with the same quantity of enamel and dentin, respectively; additionally, the placement of one layer of enamel, instead of dentin, or vice versa might influence the final optical result. The standard 3-layer stratification requires time. This is why it is important to determine if a simplified technique of stratification could lead to similar outcomes.
In this study, color differences between six different composite stratifications were investigated to evaluate the influence of the layering technique. 4-mm thick specimens were tested, representing the average thickness of the central third of a central anterior tooth. It is known that in this specific tooth area, an equal thickness of enamel and dentin is present, which is approximately 1 mm palatal enamel, 2 mm body dentin and 1 mm buccal enamel [16].
Two possible approaches could have been possible: to stratify the different layers one on the top of the previous one or to build up separate samples and to superpose them. This latter methodology has been preferred to avoid the small variability of L*a*b* values which have been detected in a pre-study and to reduce the number of the samples. In this way, the same specimens have been used and their place changed within the sandwich design in order to simulate the different stratifications.
The composite resins shades employed in the present study were selected to mimic a tooth made out of A2 enamel and A3 dentin, according to the VITA classic shade guide. Two different resin composite systems, both of which propose the application of the natural layering technique [5] for esthetic restorations, were chosen. Manufacturers were asked to indicate the closest shade code to this clinical situation. For this reason, UD3/UE2 for HRI (Micerium Avegno, Italy) and S3/NR for Miris 2 (Coltène Whaledent, Altatätten, Switzerland) were chosen.
To closely mimic the final clinical situation, slight changes in the optical appearance, which take place during the first week after polymerization, were considered. This phenomenon is due to water sorption and the chemical reactions of tertiary amines and residual camphorquinone [17, 18]. Therefore, after polymerization of the samples, all resin discs were kept for one week in an incubator at 37 °C in the absence of light and immersed in artificial saliva before the spectrophotometric evaluation. The 7 days delay was chosen because water uptake and post-polymerization are completed after this time period [19–21].
The CIELAB system was chosen in this study because of its advantage to simply calculate the difference between two colors using the following formula: ΔΕ ab = √(ΔL*) + (Δa*) + (Δb*) [2] where ΔL*, Δa*, Δb* are the respective differences in the L*, a* and b* parameters between two colors.
A revised CIE L’a’b’ color space is recommended for calculating a color difference, called CIEDE2000. That new color difference formula (ΔΕ 00) proposed involves multiple conversions, averaging, and additional terms [22]. However, when comparing ΔΕ ab with ΔΕ 00, there was a significant correlation between them [23]. Furthermore, most color difference results reported in the current dental literature are based on the CIE L*a*b* system.
A lot of different techniques devoted to the analysis, communication and verification of dental shades exist. Shade determination has always been a challenge for esthetic dentistry. The visual method using a shade guide, most commonly the Vitapan Classical Shade guide (Vita Zahnfabrik, Bad Säckingen, Germany) is a subjective technique with a lot of bias. Even if the human eye can discern very small differences in color, the ability to communicate the degree and nature of these differences is lacking. To objectify the color evaluation, instrumental methods have been developed, such as colorimeter or spectrophotometer. In this study, a spectrophotometer was used for color evaluation to avoid bias due to subjective evaluation and to detect small differences that could be imperceptible to the human eye [8–10]. A spectrophotometer measures and records the amount of visible radiant energy reflected or transmitted by an object one wavelength at a time for each value, chroma and hue present in the entire visible spectrum [24]. The Spectro Shade system uses dual digital cameras linked through optic fibers to the spectrophotometer to measure the color of the tooth and allow readings of its translucency and reflectivity. Furthermore, this device has a build-in aiming routine that enables a reproducible positioning perpendicular to the specimens’ surface which ensures standardized measurement conditions for all specimens.
The conversion of spectrophotometric measurements to the three color parameters is described by the International Commission on Illumination (CIE). CIE describes a transformation of tristimulus values (properties that describe how the color of the object appears to the observer or how the color data would be reproduced on a device such as a computer monitor or printer in terms of coordinates/values) into the CIE L*a*b* color space.
The thickness of the specimens was kept constant and they were measured over two different backgrounds (white and black), as color perception is dependent on sample thickness [25–27], opacity [28] and background [29]. According to Ardu et al. [17], white background represents the clinical situation of a class III or class V restorations, where composite overlaps a residual part of natural enamel and, eventually, dentin. The black background mimics the reconstruction of an anterior incisal angle (class IV) without the presence of any residual tooth structure backing the composite restoration.
Neither optical nor statistical differences were detected between E1DDE and EDDE1. This is logical, as these groups represented the same configuration measured in opposite directions. However, a difference between the statistical approach and the optical evaluation appeared when the underlying (=oral) layer of enamel was substituted by a dentin layer, (EDDD). From a statistical point of view, difference was detected between EDDD and EDDE while from a visual point of view, no possible differences can be perceived by human eyes (ΔΕ ab < 1.1). The difference between the statistical approach and the optical evaluation is presented in Table 8 where each composite configuration is evaluated over a different background (HRI white background; HRI black background; Miris white background; Miris black background): different letters denote differences between groups while same letters mean that no statistical/visual differences are detected).
The use of a simplified stratification (EDDD) may allow for a faster realization of composite restorations, providing optically comparable results to the “state of the art” stratification.
A previous study [30] concluded that the optical properties of the cover material generally had a greater influence on color impression of layered samples than those of the underlying material. The influence of the cover layer in the total color perception increased distinctly with the layer thickness. The ratio of the layer thicknesses of the underlying and the cover material had an important influence on the total color impression of the sample [31].
The order of the placement of the layers is thus more important than the quantity of the material and the color of the cover material is primordial. The ΔΕ ab comparing the standard stratification with EEDD was considered acceptable (<3.3) but perceptible (>1.1) when compared to DDEE, where the difference was very high and unacceptable. These results are applicable over both white and black backgrounds and without differences between the two evaluated resin composites.
Caution has to be paid to the interpretation of these current results, which refers to the specific thickness of layers used in this study. When thickness varies, in fact, the thickness of the layers changes resulting in different color and appearance.
Additionally, these results are only valid for Miris 2 (Coltene-Whaledent, Altstätten, Switzerland) and HRI (Micerium, Avegno Genova, Itlay) and cannot be applied to other composites without further in vitro and in vivo studies. Furthermore, more studies regarding the clinical interpretation of these differences are needed to thoroughly investigate the clinical influence on visual perception.
Conclusions
The first null hypothesis which stated that the order of layers did not significantly influence the final L*a*b* values had to be rejected. Depending on the order of placement of the different layers, the results varied significantly.
The second null hypothesis was also rejected except for the comparison between the so-called natural layering concept (EDDE) and the simplified stratification (EDDD) within the limit of 4 mm thickness.
Within some approximation (ΔE ab), acceptable results for human perception were obtained with both stratification techniques: the so-called ≪natural layering concept≫ (EDDE) and the simplified layering technique (EDDD): Substitution of the underlying layer, within the limit of 4 mm total thickness, did not affect the final outcome.
Even though this study seems to show that some shortcuts are possible in composite stratification, layering remains important to handle polymerization contraction stress, provide a proper light-cure and to achieve a correct proximal contact point.
Further research is needed to investigate other thickness configurations, other composites as well as other stratification techniques. Additionally, more studies regarding the clinical interpretation of these differences are needed to thoroughly investigate the clinical influences on visual perception.
Références
Vanini L. Light and color in anterior composite restorations. Pract Periodontics Aesthet Dent. 1996;8:673–82.
Ardu S, Krejci I. Biomimetic direct composite stratification technique for the restoration of anterior teeth. Quintessence Int. 2006;37:167–74.
Dietschi D, Ardu S, Krejci I. A new shading concept based on natural tooth color applied to direct composite restorations. Quintessence Int. 2006;37:91–102.
Fahl JR. Achieving ultimate anterior esthetics with a new microhybrid composite. Compend Contin Educ Dent. 2000;26:4–13.
Dietschi D. Free-hand bonding in the esthetic treatment of anterior teeth: creating the illusion. J Esthet Dent. 1997;9:156–64.
Dietschi D. Layering concepts in anterior composite restorations. J Adhes Dent. 2001;3:71–80.
Ardu S, Feilzer AJ, Braut V, Benbachir N, Rizcalla N, Mayoral JR, Krejci I. Pilot in vivo image spectro-photometric evaluation of optical properties of pure enamel and enamel-dentin complex. Dent Mater. 2010;26:e205–10.
Johnston WM, Kao EC. Assessment of appearance match by visual observation and clinical colorimetry. J Dent Res. 1989;68:819–22.
Liberman R, Combe EC, Piddock V, Pawson C, Watts DC. Development and assessment of an objective method of colour change measurement for acrylic denture base resins. J Oral Rehabil. 1995;22:445–9.
Brook AH, Smith RN, Lath DJ. The clinical measurement of tooth colour and stain. Int Dent J. 2006;57:324–30.
Commission International de l’eclairage (CIE) (1976) Technical Report, Colorimetry 2nd edn. CIE, Vienna.
Um CM, Ruyter IE. Staining of resin-based veneering materials with coffee and tea. Quintessence Int. 1991;22:377–86.
Ruyter IE, Nilner K, Moller B. Color stability of dental composite resin materials for crown and bridge veneers. Dent Mater. 1987;3:246–51.
Kuehni RG, Marcus RT. An experiment in visual scaling of small color differences. Color Res Appl. 1979;4:83–91.
Hunter R. The measurement of appearance. New York: Wiley; 1975. p. 77–80 (151–2,225,234).
Schillinghurgh JR, Grace CS. Thickness of enamel and dentin. J South Calif Dent Assoc. 1973;41:33–6.
Ardu S, Gutemberg D, Krejci I, Feilzer AJ, Di Bella E, Dietschi D. Influence of water sorption on resin composite color and color variation amongst various composite brands with identical shade code: an in vitro evaluation. J Dent. 2011;39(Suppl 1):e37–44.
Van Landuyt KL, Snauwaert J, De Munck J, Peumans M, Yoshida Y, Poitevin A, Coutinho E, Suzuki K, Lambrechts P, Van Meerbeek B. Systematic review of the chemical composition of contemporary dental adhesives. Biomaterials. 2007;28:3757–85.
Burtscher P. Stability of radicals in cured composite materials. Dent Mater. 1993;9:218–21.
De Pires Souza Fde C, Garcia Lda F, Hamida HM, Casemiro LA. Color stability of composites subjected to accelerated ageing after curing using either a halogen or a light emiting diode source. Braz Dent J. 2007;18:119–23.
Tyras M. Colour stability of composite resins: a clinical comparison. Aust Dent J. 1992;37:88–90.
Luo MR, Cui G, Rigg B. The development of the CIE 2000 colour-difference formula: CIEDE2000. Color research and application. 2001;26:340–50.
Lee YK, Powers JM. Comparaison of CIE lab, CIEDE 200 and DIN 99 color differences between various shades of resin composites. Int J Prosthodont. 2005;18:150–5.
Paul S, Peter A, Pietrobon N, Hammerle CH. Visual and spectrophotometric shade analysis of human teeth. J Dent Res. 2002;81:578–82.
Schmeling M, Meyer Filo A, De MA M, Baratieri LN. Chromatic influence of value resin composites. Oper Dent. 2010;35:44–9.
Friebel M, Pernell O, Cappuis HJ, Helfmann J, Meinke MC. Simulation of color perception of layered dental composites using optical properties to evaluate the benefit of esthetic layer preparation technique. Dent Mater. 2012;28:24–32.
Price RB, Murphy DG, Derand T. Light energy transmission through cured resin composite and human dentin. Quintessence Int. 2000;31:659–67.
Joiner A. Tooth colour: a review of the literature. J Dent. 2004;32(Suppl 1):3–12.
Ardu S, Braut V, Di Bella E, Lefever D. Influence of background on natural tooth colour coordinates: an in vivo evaluation. Odontology. 2013;11: ahead of print.
Lee YK, Powers JM. Calculation of colour resulting from composite/compomer layering techniques. J Oral Rehabil. 2004;31:1102–8.
Vichi A, Fraioli A, Davidson CL, Ferrari M. Influence of thickness on color in multi-layering technique. Dent Mater. 2007;23:1584–9.
Conflict of interest
Emilie Betrisey, Ivo Krejci, Enrico Di Bella, and Stefano Ardu declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Betrisey, E., Krejci, I., Di Bella, E. et al. The influence of stratification on color and appearance of resin composites. Odontology 104, 176–183 (2016). https://doi.org/10.1007/s10266-015-0197-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-015-0197-2