Abstract
Angiopoietin-like protein 2 (Angptl2) plays a key role in chronic inflammation and tissue remodeling. We evaluated whether serum Angptl2 is associated with interstitial lung disease (ILD) in primary Sjogren’s syndrome (pSS) patients. A total of 158 consecutive pSS patients and 25 normal healthy controls, which completed lung HRCT, were enrolled in our research. The levels of serum Angptl2 and TGF-β1 were measured by enzyme-linked immunosorbent assay. We investigated the correlation between the activity indexes of pSS-ILD patients and the serum Angptl2 levels. There were 71 of 158 (44.94%) patients interpreted pSS-ILD by radiologists at the initial presentation. The median interquartile range for serum Angptl2 was 16.55 ng/mL (range 10.82–41.07) in pSS patients, compared with 6.05 ng/mL (range 3.53–9.91) in normal healthy controls (P < 0.001). Importantly, differences between Angptl2 levels in pSS-ILD patients and pSS-N-ILD patients were also statistically significant [29.80 ng/mL (range 15.42–54.40), 14.75 ng/mL (range 9.85–40.48), P < 0.001]. A logistic regression analysis suggested that anti-Ro52, serum Angptl2 and DLCO were associated with pSS patients with interstitial lung disease, with aORs and 95% CIs of 2.06 (1.14–7.65), 4.13 (1.25–15.89) and 9.51 (2.10–37.74), respectively. Moreover, anti-Ro52 (rs = 0.48, P = 0.016) and TGF-β1 (rs = 0.64, P = 0.003) were significantly correlated with the serum Angptl2 in pSS-ILD patients. And, in pulmonary function tests, the serum Angptl2 was significantly correlated with DLCO (rs = − 0.40, P = 0.009) and FVC (rs = −0.37, P = 0.020). Serum Angptl2 may display a peculiar role in the pathogenesis of pSS-ILD and might be a potential biomarker.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary Sjogren’s syndrome (pSS) is a chronic systemic autoimmune disease which primarily affects the exocrine glands. But, interstitial lung disease (ILD) has been shown to be the most common involved in the damage of pulmonary in pSS patients [1,2,3,4]. The incidence estimates of pSS-ILD are dependent on screening methods and the selection of patient [3, 5, 6]. In Chinese population, our recent study found that the prevalence of pSS-ILD was 39.10% by HRCT [5]. ILD patients with poor prognosis: A recent registry data-based retrospective study showed that pSS-ILD patients had a fourfold higher risk of death than those without ILD [3]. Finding biomarkers related to pSS-ILD has novel clinical value.
Angiopoietin-like protein 2 (Angptl2), which functions in angiogenesis and tissue repair, belongs to the angiopoietin-like protein family. However, it has recently been shown that excessive Angptl2 signaling mediates chronic inflammation and subsequent pathological irreversible tissue remodeling. [7]. Transforming growth factor beta 1 (TGF-β1) plays an important role in tissue homeostasis and tissue remodeling during structurally related processes, including interstitial lung disease [8, 9]. It has been reported that mechanical stress induced by the expression of Angptl2 can promote the activation of TGF-β1/Smad signaling and increase the expression of TGF-β1 in the ligamental flavum tissue degeneration [10]. Meanwhile, Angptl2 is associated with liver fibrosis in hepatitis B patients [11].
Moreover, the level of Angptl2 in serum was higher in patients with NSCLC (non-small cell lung cancer) [12], whether the circulating concentration of Angtpl2 was increased in interstitial lung disease, particularly in primary Sjogren’s syndrome-related interstitial lung disease (pSS-ILD) patients was unknown. So, we hypothesized that Angptl2 participates in interstitial lung disease in pSS-ILD and would be a potential biomarker. In this research, we studied the correlation between the activity indexes of pSS-ILD patients and the serum Angptl2 levels.
Patients and methods
The medical records of pSS patients admitted to the second hospital of Shanxi Medical University from March 2018 to February 2019 were retrospectively analyzed. Demographic characteristics, test data and clinical features were extracted from the database. This study was approved by the ethics committee of the second hospital of Shanxi Medical University, and the whole research process followed the principles of the Helsinki Declaration. The inclusion criteria for this study met the 2002 international classification criteria for Sjogren’s syndrome [13] or the 2016 ACR/EULAR classification criteria for Sjogren’s syndrome [14]. Exclusion criteria were pulmonary surgery, tumors, infectious diseases and overlap of other SS with other well-defined connective tissue diseases. All participants gave written informed consent.
All patients received HRCT scan of chest with 1–2-mm-thick incision. When inhaled in supine position, the scan was carried out. And images were evaluated blindly by two experienced radiologists [15]. All lung function test results are expressed as a percentage of the predicted value [16]. All patients completed pulmonary HRCT examination. The pSS patients were divided into ILD group (pSS-ILD) and non-ILD group (pSS-N-ILD) according to the HRCT manifestations. Serum of 71 patients with pSS-ILD and 87 patients with pSS-N-ILD was collected. Serum of the control group was taken from health staff of the second hospital of Shanxi Medical University (n = 25).
Measurement of serum Angptl2 and TGF-β1
The enzyme-linked immunosorbent assay (ELISA) kit (Catalog Number: CSB-E13881h and CSB-E04725h, CUSABIO, Beijing, China) was utilized to perform the manufacturer’s protocol for the determination of serum Angptl2 and TGF-β1 levels (capture antibody: murine monoclonal antibody; detection antibody: goat polyclonal antibody). The assay has high sensitivity and excellent specificity for detection of human Angptl2 and TGF-β1. No significant cross-reactivity or interference between human Angptl2 (or TGF-β1) and analogues was observed. All the blood samples obtained in the study were used to produce small aliquots, which were stored at −80 °C to ensure that all the samples underwent only one freeze–thaw cycle. We detected serum Angptl2 and TGF-β1 concentration in seventy-one patients with pSS-ILD, eighty-seven pSS-N-ILD patients and twenty-five healthy people as control.
Statistical analysis
Statistical analysis software (SPSS18.0, SPSS Inc, Chicago, IL, USA) was used for data analysis. Two-sided statistical analysis was carried out. P < 0.05 was considered statistically significant. Continuous variables were expressed as mean and standard deviation of normally distributed data or median values of non-normally distributed data (P25, P75), which were compared by Student’s t test or Mann–Whitney U test. The categorical variables were expressed as percentages and were compared using the Chi-square test. Logistic regression was used to compute the odds ratios of different variables for primary Sjogren’s syndrome patients with interstitial lung disease. Variables were included in the analysis using the backward likelihood ratio selection method. Pearson or Spearman’s rank correlation analysis was used to analyze the relationship between serum Angptl2 level and other variables.
Results
Serum Angptl2 and TGF-β1 levels were elevated in primary Sjogren’s syndrome-related interstitial lung disease patients.
Of the 158 patients, 71 were diagnosed as primary Sjogren’s syndrome-related interstitial lung disease (pSS-ILD) by radiologists at the first visit, with a prevalence of 44.94%. Clinical characteristics of pSS-ILD and pSS-N-ILD patients are shown in Table 1. Among the normal health controls (NHCs), 15 were women and 10 were men, 6 smokers all male. The age of the NHCs was 56.15 ± 12.61 years old. There were no significant differences between patients with pSS and NHCs in terms of age, proportion of female gender and smoke ever. Serum levels of angiopoietin-like protein 2 (Angptl2) and transforming growth factor β1 (TGF-β1) were detected by ELISA in 87 patients without interstitial lung disease (pSS-N-ILD), 71 pSS-ILD patients and 25 healthy controls (Table 2).
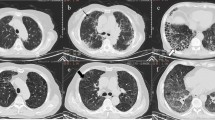
As shown in Fig. 1, the median interquartile range for serum Angptl2 was 16.55 ng/mL (range 10.82–41.07) in pSS patients, compared with 6.05 ng/mL (range 3.53–9.91) in normal healthy controls (P < 0.001). Importantly, differences between Angptl2 levels in pSS-ILD patients and pSS-N-ILD patients were also statistically significant [29.80 ng/mL (range 15.42–54.40), 14.75 ng/mL (range 9.85–40.48), P < 0.001]. Meanwhile, the median interquartile range for serum TGF-β1 was 11.70 ng/mL (range 6.40–17.75) in pSS patients, compared with 3.01 ng/mL (range 1.84–3.95) in normal healthy controls (P < 0.001). Differences between TGF-β1 levels in pSS-ILD patients and pSS-N-ILD patients were also statistically significant [16.50 ng/mL (range 10.12–22.85), 9.50 ng/mL (range 3.94–14.73), P < 0.001]. TGF-β1 plays an important role in structure-related processes in tissue homeostasis and tissue remodeling, including interstitial lung disease and pulmonary fibrosis. In pSS-ILD patients, serum TGF-β1 (rs = 0.64, P = 0.003, Table 3) was significantly correlated with the serum Angptl2. Those results revealed that serum Angptl2 levels may associated with interstitial lung disease.
Serum Angptl2 and TGF-β1 levels were elevated in primary Sjogren’s syndrome-related interstitial lung disease patients. Serum Angptl2 and TGF-β1 levels in 87 primary Sjogren’s syndrome patients without interstitial lung disease (pSS-N-ILD), 71 patients with interstitial lung disease (pSS-ILD) and 25 normal healthy controls (NHCs) are shown, as measured by enzyme-linked immunosorbent assay (*P < 0.05, **P < 0.01, ***P < 0.001)
Comparison of clinical manifestations between primary Sjogren’s syndrome patients without and with interstitial lung disease
We compared the clinical manifestations of primary Sjogren’s syndrome patients without and with interstitial lung disease (Table 1). Of the 158 pSS patients, 71 were diagnosed as pSS-ILD by HRCT at the first admission, and the prevalence of pSS-ILD in this study was 44.94%. In both pSS-ILD group and pSS-N-ILD group, no significant differences were observed in terms of age, sex and disease duration. The pSS-ILD group with smoking and dry cough was higher than compared with the pSS-N-ILD group (P < 0.01 and P < 0.001). However, there were no statistically significant differences between the two groups in dry mouth, dry eyes and arthritis.
Although there were no significant differences in serum globulin, IgA, IgM and IgG levels between groups, the data of the pSS-N-ILD group were lower than those of the pSS-ILD group. In our study, the RF titres, ESR and CRP were high and have no statistical differences. However, higher anti-Ro52 antibody positive rate was observed (P<0.01), indicating that anti-Ro52 antibody might have unique advantage to identify ILD in pSS patients.
No significant difference was found for pulmonary hypertension in echocardiography.
There was a significant difference in carbon monoxide diffusion capacity (DLCO) and forced vital capacity (FVC) between patients with pSS-ILD and those without ILD. Therefore, the patients with pSS-ILD were mainly characterized by diffuse dysfunction and restrictive ventilatory dysfunction. Significantly, both groups suffered from small airway disease, and the pSS-ILD group had a higher rate than the pSS-N-ILD group (64.79% vs. 14.94%, P < 0.001).
Predictors for primary Sjogren’s syndrome patients with interstitial lung disease.
Logistic regression was used to compute the odds ratios of different variables for primary Sjogren’s syndrome patients with interstitial lung disease. To develop a good-fit model, age, sex, disease duration, smoking, anti-Ro52 (+) and significant variables derived from univariate analyses were entered into the model. Logistic regression analysis suggested that anti-Ro52, serum Angptl2 and DLCO were associated with pSS patients with interstitial lung disease, with aORs and 95% CIs of 2.06 (1.14–7.65), 4.13 (1.25–15.89) and 9.51 (2.10–37.74), respectively.
Disease activity of pSS-ILD correlates with serum Angptl2 levels
TGF-β1 (rs = 0.64, P = 0.003) was significantly correlated with the serum Angptl2 in pSS-ILD patients. Meanwhile, anti-Ro52 (rs = 0.48, P = 0.016) significantly correlated with the serum Angptl2 in pSS-ILD patients. And, in pulmonary function tests, the serum Angptl2 was also significantly correlated with small airway involvement (rs = 0.52, P = 0.031), diffusion capacity of the lung for carbon monoxide (rs = − 0.40, P = 0.009) and forced vital capacity (rs = − 0.37, P = 0.020).
Discussion
Currently, research showed that Angptl2 is directly involved in disease-related pulmonary, kidney and liver fibrosis [11, 17,18,19]. However, the roles of Angptl2 in pSS-ILD patients are still unknown. To our knowledge, this is the first study to show a significant elevate in serum Angptl2 levels in patients with pSS, especially in patients with pSS-ILD.
In terms of connective tissue diseases, it has been reported that the concentration of Angptl2 in joint fluid of RA patients was significantly higher than that of osteoarthritis patients. In the proliferative rheumatoid synovium of RA patients, Angptl2 was expressed in large quantities, especially in fibroblast-like synovium cells and macrophage-like synovium cells [20]. Meanwhile, Angptl2 was abundant in keratinocytes from dermatomyositis patients’ skin eruptions [21], and treatment of keratinocytes with exogenous Angptl2 could increase the expression of IL-1β and IL-6 by activating the NF-kB inflammatory signaling pathway. Surprisingly, our study found that serum Angptl2 level in pSS patients was significantly higher than that in the normal healthy control group.
Recent studies have shown that excessive Angptl2 signaling could mediate chronic inflammation and subsequent pathological irreversible tissue remodeling [7]. TGF-β1 plays a key role in tissue homeostasis and tissue remodeling during structurally related processes, including interstitial lung disease [8, 9]. In murine models of pulmonary fibrosis, inflammatory response and fibrosis were improved in Angptl2 (−/−) mice by decreasing pulmonary TGF-β1 expressions [18]. Angptl2 may be mediated by alpha5beta1 integrin-mediated activation of extracellular signal-regulated kinases to increase TGF-β1 expression [17]. Studies have shown that the expression of Angptl2 induced by mechanical stress could increase the expression of TGF-β1 in the ligamental flavum tissue and promote the activation of TGF-β1/Smad signaling [10]. In our research, the average level of serum Angptl2 and TGF-β1 in pSS-ILD patients was significantly higher than that of the pSS-N-ILD patients. And in pSS-ILD patients, serum TGF-β1 was significantly correlated with the serum Angptl2. Logistic regression analysis suggested that not only anti-Ro52 and DLCO, but also serum Angptl2 was associated with pSS patients with interstitial lung disease. Those results revealed that serum Angptl2 may display a peculiar role in the pathogenesis of pSS-ILD.
Studies have reported that the anti-Ro52/60 antibody has unpredictable value in predicting the occurrence of pSS-ILD [2, 22]. Higher anti-Ro52 antibody positive rate was observed in pSS-ILD patients [3]. Consistent with previous research, in this study, the number of anti-Ro52 antibodies was significantly increased in pSS-ILD patients compared with pSS-N-ILD patients. Those results indicating that anti-Ro52 antibody might have unique advantage to identify ILD in pSS patients. And anti-Ro52 antibody, which was associated with the TH17 pathway [23], regulated the activity of IL-23. This may be related to the involvement of anti-Ro52 antibodies in the pathogenesis of pSS-ILD. Meanwhile, serum Angptl2 was significantly positively correlated with anti-Ro52. The interaction between Angptl2 and anti-Ro52 deserves further investigation.
PFTs are sensitive but non-specific. Kelly et al. found that DLCO was significantly reduced in both limited and extensive interstitial lung disease [24]. DLCO was reported to be a highly sensitive screening test for the presence of interstitial lung disease. There were significant differences in forced vital capacity (FVC) and carbon monoxide diffusion capacity (DLCO) between patients with pSS-ILD and those without ILD. Therefore, patients with pSS-ILD were mainly characterized by diffuse dysfunction and restrictive ventilatory dysfunction. It is worth noting that the two groups of patients we studied were suffered from small airway diseases, and the pSS-ILD group had a higher rate, which may be related to inflammatory lymphocytic infiltration or airway mucosal interstitial lesion itself. Moreover, serum Angptl2 levels were significantly negatively correlated with FVC and DLCO. Given the current evidences and our results, we suggest that serum Angptl2 not only may display a peculiar role in the pathogenesis of pSS-ILD, but also might be a potential biomarker. However, due to multiple limitations, further research must be required.
This research dose has some inevitable limitations. Firstly, this is a retrospective study. Secondly, owing to the study’s design and enroll patients in a single medical care center, it is difficult to establish the exact causal relationships. Thirdly, to validate serum Angptl2 as a useful biomarker, more comprehensive and detailed follow-up studies must be conducted.
In conclusion, the serum Angptl2 was significantly higher in pSS-ILD patients. Logistic regression analysis suggested that anti-Ro52, serum Angptl2 and DLCO were associated with pSS patients with interstitial lung disease. Anti-Ro52 and TGF-β1 were significantly correlated with the serum Angptl2. Moreover, the serum Angptl2 was also significantly correlated with DLCO. Serum Angptl2 may display a peculiar role in the pathogenesis of pSS-ILD and might be a potential biomarker.
References
Flament T, Bigot A, Chaigne B, Henique H, Diot E, Marchand-Adam S. Pulmonary manifestations of Sjogren’s syndrome. Eur Respir Rev. 2016;25(140):110–23. https://doi.org/10.1183/16000617.0011-2016.
Sebastian A, Misterska-Skora M, Silicki J, Sebastian M, Wiland P. Chest HRCT findings in patients with primary Sjogren’s syndrome. Adv Clin Exp Med. 2017;26(7):1101–6. https://doi.org/10.17219/acem/68978.
Palm O, Garen T, Berge Enger T, Jensen JL, Lund MB, Aalokken TM, et al. Clinical pulmonary involvement in primary Sjogren’s syndrome: prevalence, quality of life and mortality—a retrospective study based on registry data. Rheumatology (Oxford). 2013;52(1):173–9. https://doi.org/10.1093/rheumatology/kes311.
Sisto M, Lorusso L, Lisi S. TLR2 signals via NF-kappaB to drive IL-15 production in salivary gland epithelial cells derived from patients with primary Sjogren’s syndrome. Clin Exp Med. 2017;17(3):341–50. https://doi.org/10.1007/s10238-016-0429-y.
Dong X, Zhou J, Guo X, Li Y, Xu Y, Fu Q, et al. A retrospective analysis of distinguishing features of chest HRCT and clinical manifestation in primary Sjogren’s syndrome-related interstitial lung disease in a Chinese population. Clin Rheumatol. 2018;37(11):2981–8. https://doi.org/10.1007/s10067-018-4289-6.
Bergantini L, Cameli P, d’Alessandro M, Vagaggini C, Refini RM, Landi C, et al. NK and NKT-like cells in granulomatous and fibrotic lung diseases. Clin Exp Med. 2019;19(4):487–94. https://doi.org/10.1007/s10238-019-00578-3.
Kadomatsu T, Endo M, Miyata K, Oike Y. Diverse roles of ANGPTL2 in physiology and pathophysiology. Trends Endocrinol Metab. 2014;25(5):245–54. https://doi.org/10.1016/j.tem.2014.03.012.
Bagnato G, Harari S. Cellular interactions in the pathogenesis of interstitial lung diseases. Eur Respir Rev. 2015;24(135):102–14. https://doi.org/10.1183/09059180.00003214.
Richeldi L, Collard HR, Jones MG. Idiopathic pulmonary fibrosis. Lancet. 2017;389(10082):1941–52. https://doi.org/10.1016/s0140-6736(17)30866-8.
Nakamura T, Okada T, Endo M, Kadomatsu T, Taniwaki T, Sei A, et al. Angiopoietin-like protein 2 induced by mechanical stress accelerates degeneration and hypertrophy of the ligamentum flavum in lumbar spinal canal stenosis. PLoS ONE. 2014;9(1):e85542. https://doi.org/10.1371/journal.pone.0085542.
Deng Y, Zhao H, Zhou J, Yan L, Wang G. Angiopoietin-like protein as a novel marker for liver fibrosis in chronic hepatitis B patients with normal to minimally raised ALT. BMC Infect Dis. 2017;17(1):650. https://doi.org/10.1186/s12879-017-2728-7.
Chen Y, Jiang H, Zhu L, Wang P, Liu S, Xiao X, et al. Diagnostic and prognostic value of serum angiopoietin-like protein 2 in patients with non-small cell lung cancer. Clin Lab. 2017;63(1):59–65. https://doi.org/10.7754/Clin.Lab.2016.160528.
Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, et al. Classification criteria for Sjogren’s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis. 2002;61(6):554–8.
Shiboski CH, Shiboski SC, Seror R, Criswell LA, Labetoulle M, Lietman TM, et al. 2016 American College of Rheumatology/European League against rheumatism classification criteria for primary Sjogren’s syndrome: a consensus and data-driven methodology involving three international patient cohorts. Arthritis Rheumatol. 2017;69(1):35–45. https://doi.org/10.1002/art.39859.
Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183(6):788–824. https://doi.org/10.1164/rccm.2009-040GL.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–38. https://doi.org/10.1183/09031936.05.00034805.
Morinaga J, Kadomatsu T, Miyata K, Endo M, Terada K, Tian Z, et al. Angiopoietin-like protein 2 increases renal fibrosis by accelerating transforming growth factor-beta signaling in chronic kidney disease. Kidney Int. 2016;89(2):327–41. https://doi.org/10.1016/j.kint.2015.12.021.
Yang W, Liu W, Yu W, Fei D, Meng X, Yang S, et al. Angptl2 deficiency attenuates paraquat (PQ)-induced lung injury in mice by altering inflammation, oxidative stress and fibrosis through NF-kappaB pathway. Biochem Biophys Res Commun. 2018;503(1):94–101. https://doi.org/10.1016/j.bbrc.2018.05.186.
Motokawa I, Endo M, Terada K, Horiguchi H, Miyata K, Kadomatsu T, et al. Interstitial pneumonia induced by bleomycin treatment is exacerbated in Angptl2-deficient mice. Am J Physiol Lung Cell Mol Physiol. 2016;311(4):L704–13. https://doi.org/10.1152/ajplung.00005.2016.
Okada T, Tsukano H, Endo M, Tabata M, Miyata K, Kadomatsu T, et al. Synoviocyte-derived angiopoietin-like protein 2 contributes to synovial chronic inflammation in rheumatoid arthritis. Am J Pathol. 2010;176(5):2309–19. https://doi.org/10.2353/ajpath.2010.090865.
Ogata A, Endo M, Aoi J, Takahashi O, Kadomatsu T, Miyata K, et al. The role of angiopoietin-like protein 2 in pathogenesis of dermatomyositis. Biochem Biophys Res Commun. 2012;418(3):494–9. https://doi.org/10.1016/j.bbrc.2012.01.052.
Li X, Xu B, Ma Y, Li X, Cheng Q, Wang X, et al. Clinical and laboratory profiles of primary Sjogren’s syndrome in a Chinese population: a retrospective analysis of 315 patients. Int J Rheum Dis. 2015;18(4):439–46. https://doi.org/10.1111/1756-185X.12583.
Espinosa A, Dardalhon V, Brauner S, Ambrosi A, Higgs R, Quintana FJ, et al. Loss of the lupus autoantigen Ro52/Trim21 induces tissue inflammation and systemic autoimmunity by disregulating the IL-23-Th17 pathway. J Exp Med. 2009;206(8):1661–71. https://doi.org/10.1084/jem.20090585.
Kelly CA, Saravanan V, Nisar M, Arthanari S, Woodhead FA, Price-Forbes AN, et al. Rheumatoid arthritis-related interstitial lung disease: associations, prognostic factors and physiological and radiological characteristics—a large multicentre UK study. Rheumatology (Oxford). 2014;53(9):1676–82. https://doi.org/10.1093/rheumatology/keu165.
Funding
No funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
This study was approved by the ethics committee of the second hospital of Shanxi Medical University, and the whole research process followed the principles of the Helsinki Declaration.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shi, L., Fu, Q., Chen, N. et al. Angiopoietin-like protein 2 as a novel marker for patients with primary Sjogren’s syndrome-related interstitial lung disease. Clin Exp Med 20, 393–399 (2020). https://doi.org/10.1007/s10238-020-00623-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-020-00623-6