Abstract
Objectives
To determine demographic, socioeconomic, and clinical factors associated with being high-cost users (HCUs) in adult patients (≥ 18 years) who received acute care in Canada.
Research design
We conducted a retrospective study among adults who had at least one encounter with acute care facilities each year from 2011 to 2014 using national linked data sets. We defined HCUs as patients on the top 10% of the highest acute care cost users in the province, where the care was provided. Risk factors associated with being HCUs were identified using multilevel logistic regression. Provincial variations of identified risk factors were examined using logistic regression. Sensitivity analyses were also performed to investigate the influences of using different metrics and different thresholds to define high system users, missing data, and the inclusion of interaction terms on the study results.
Results
Between 2011 and 2014, a total of 3,891,410 patients with 6,017,430 hospitalizations were included. Patients who were male [odds ratio (OR), 1.60; 95% confidence interval (CI) 1.59–1.61], with low incomes [OR 1.42; 95% CI 1.41–1.43), with higher comorbidity score (OR 1.41; 95% CI 1.40–1.41] and older [OR 1.18; 95% CI 1.17–1.18] were more likely to be acute care HCUs. Significant interactions existed between comorbidity score and age/sex/income status. Across provinces, the associations between socioeconomic factors and being HCUs has the largest variation. When using various high system users (HSUs) definitions, the impacts of living in rural area and being visible minority on the odds of being HSUs differ.
Conclusions
A few demographic, socioeconomic, and clinical factors was associated with high acute care expenditures. The associations between included risk factors and being acute care HCUs vary across provinces and different definitions of high system users (HSUs).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Research showed that more than half of healthcare costs were spent on 5% of patients in developed countries or regions [1]. As for Canada, similar findings have been reported with 61% of hospital and community care expenditures in Ontario and 30% of physician services in British Columbia consumed by 5% of patients [2, 3]. These high system users (HSUs) are commonly defined using metrics, such as cumulative costs, the length of stay, the frequency of hospitalizations and the frequency of emergency department (ED) visits [4]. A recent study demonstrated that compared to non-high users, HSUs had substantially more hospital admissions (69.2 vs. 5.4%) and higher mortality (13.0 vs. 1.7%) [2]. In addition, increased use of ED services was associated with higher mortality among patients with mental disorders [5]. This contrast between higher healthcare resource inputs and poorer health gains in HSUs highlights the importance of understanding the utilization of healthcare resources by HSUs, a critical step to improving healthcare systems' efficiency and sustainability [3, 6].
Acute care includes health care services for individuals or populations who depend on time-sensitive and rapid interventions [7]. It involves a range of services including trauma care, acute care surgery, and inpatient care [7]. Studies have shown that acute care accounts for the largest share of health care expenditures (26.6%) in Canada in 2019 [8]. Acute care is also the largest source and driver of spending among high cost users (HCUs), who are HSUs defined using cumulative costs [8, 9]. Wodchis et al. found that acute care costs accounted for more than 30% of all healthcare expenditures among patients in the top decile of costs in Ontario, Canada [10]. In contrast, physician service, continuing care and other healthcare facilities (e.g., rehabilitation) each accounted for less than 20% of healthcare expenditures [10]. Furthermore, another study in Ontario, Canada showed that the total costs of HCUs in acute care were 6.5 times higher than that of HCUs in continuing care facilities and 11.5 times higher than that of rehabilitation services [3]. Therefore, HCUs in acute care have been the focus of most research and interventions. Previous research in Canada has identified a range of contributors to high acute care costs, including older age, socioeconomic disadvantages (e.g., personal or family low-income status) and medical complexity (e.g., a higher level of comorbidities) [1, 10,11,12,13,14]. However, few studies have adopted a national perspective and addressed the provincial variations in characteristics of acute care HCUs. Given the decentralized management of health care delivery in Canada and the variations in population demographic characteristics and patients' access and experience of health care services in different provinces, HCU characteristics might vary across provinces in Canada [15,16,17,18]. Furthermore, most studies were conducted based on health care administrative databases or health surveys, which limited their capacity to address individual socioeconomic characteristics that could be heterogeneous among clinically similar patients and amenable to interventions [10,11,12,13,14]. Thus, there is a lack of evidence on risk factors, especially socioeconomic factors, associated with being HCUs of acute care at the national level. It is unknown how these factors may vary across provinces. This study aimed to identify socioeconomic, demographic, and clinical factors associated with being HCUs of acute care in adult patients (≥ 18 years) in Canada and to examine how they vary across provinces.
Methods
Data sources and study population
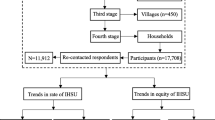
We conducted a retrospective cohort study using the HSUs linked to T1 Family File–Census of the Population Long-Form–National Household Survey (HSUS–T1FF–CENSUS–NHS, from now on referred to as “the linked data set”) [19]. The protocol for this study was published elsewhere with more details on the data sources and study population [20].
In the linked data set, the database HSUS provided the encrypted patient identification numbers and patients’ status of being HSUs or non-HSUs. It consisted of eight subset cohorts to reflect the definitions of HSUs regarding acute care cost, the total length of stay, the number of hospitalizations and the number of ED visits each year in adults (≥ 18 years) and children [21]. Our study focused on the adult acute care cost cohort, in which HCUs are defined as the top 10% of each province’s highest acute care cost adult users (≥ 18 years) each year from the fiscal year 2011/2012 to 2014/2015 [21]. Non-HCUs were patients randomly selected from the remaining 90% of adult patients in the same province each year with a sample ratio of 4:1. No matching between the HCU group and the non-HCU group was performed in the linked data set. The T1 Family File (T1FF) database, the 2006 Census of Population Long-Form (2006 Census 2B) and the 2011 National Household Survey (2011 NHS) complemented each other and provided socio-demographic and socioeconomic information about the included population. The linked data set also included the Discharge Abstract Database (DAD), which provided demographic, administrative, and clinical data on all discharges from acute inpatient facilities [22]. Using encrypted patient identity numbers in the HSUS, we merged databases at the individual level for our analysis (Supplemental file, Figure S1) [21].
Selected variables
Our primary outcome was whether a patient was an HCU or non-HCU of acute care. HCUs were patients within the top 10% of his/her province’s highest cumulative acute care cost in a specific fiscal year. Non-HCUs were patients randomly selected from the remaining 90% of that year’s adult acute care cohort. We selected a few demographic, socioeconomic and clinical factors as independent variables. We provided detailed descriptions and rationales of the selected variables in our protocol [20]. We made some changes to the variables included in the analysis. The income adequacy decile was excluded from the analysis due to its high proportion of missing values (29.5%). The admission category was excluded because of the potential endogeneity issue which occurs when the outcome variable could be the cause of a predictor variable [23]. Interaction terms were included based on consultation with experts in health economics and findings from a previous study which showed that the association between comorbidity level and healthcare costs was significantly modified by age, sex, and income level [24].
Data analysis
We used the data at patients’ first admissions in our analysis. We described the characteristics of HCUs and non-HCUs at the individual level using frequencies (percentages), means (standard deviations (SDs)) or medians (interquartile ranges (IQRs)) as appropriate. The number of hospitalizations within a year among HCUs and non-HCUs was also compared. To protect the confidentiality of respondents' personal information in the database, the individual-level census weights and subsequent rounding on the base of five were used to generate the descriptive statistics. In the primary analysis, we used the multilevel logistic regression with the province as a random effect to identify factors associated with the high acute care cost. Interactions between comorbidity score and age/sex/income status were explored. Provincial variations of risk factors associated with being acute care HCUs were examined using logistic regression models. The cutoff value of 10% was used to define HSUs across all cohorts. To assess the robustness of findings, sensitivity analyses were performed to (1) compare the results when missing data were handled using the complete case analysis vs. multiple imputations by the fully conditional specification algorithm [25]; (2) examine the variations of risk factors across alternative definitions for HSUs when HSUs are defined through different metrics (the length of stay, frequency of hospitalizations and frequency of emergency department visits) and HCUs are defined using different thresholds (5% and 1%); and 3) explore the impact of the inclusion of interaction terms on the coefficients of other variables. Since we did not have access to the raw costs data, we used the research intensity weights (RIWs) as a proxy to explore the impact of using the thresholds of 5% and 1% to define HCUs. RIWs are relative weights assigned to patients measuring the costs of an individual with certain clinical and demographic characteristics relative to the average typical inpatient case [26]. Only typical patients who have normal length of stay, relatively homogeneous resource use and no transfer were assigned RIWs and included in the analysis [27]. The unadjusted odds ratio (OR) and 95% confidence interval were estimated. The significance level of 0.05 was used for all statistical tests. All the data analyses were performed using R statistical software, version 4.0.1 [28]. This study was approved by the Social Sciences and Humanities Research Council (SSHRC) and granted a waiver of patient consent.
Results
Between April 1, 2011, and March 31, 2014, a total of 3,891,410 patients with 6,017,430 hospitalizations were included in our analysis. The percentage of patients with missing values was 2.13%. Table 1 presents the characteristics of included patients at the individual level. The HCUs and non-HCUs were similar with respect to their residential areas. However, the HCUs tended to be male, older, had lower work activity in the previous year, less educated and had more comorbidities. Similar results can be seen when summarizing patients’ clinical characteristics at the encounter level (Supplemental file, Table S1). In addition, the HCUs tended to have multiple admissions within a year (Table 2).
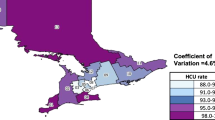
Table 3 presents the results of primary analysis. Compared to patients who are female, males (OR 1.60; 95% CI 1.59–1.61) were more likely to be HCUs. Compared to patients with higher income, low-income patients (OR 1.42; 95% CI 1.41–1.43) were more likely to be HCUs. Patients with higher comorbidity score (OR 1.41; 95% CI 1.40–1.41) and older age (OR 1.18; 95% CI 1.17–1.18) had higher odds of being HCUs. Compared to patients who did not work in the previous year, patients who worked had lower odds of being HCUs, especially for those with health occupations (OR 0.60; 95% CI 0.58–0.62). There were significant interactions between the Elixhauser comorbidity score and age/sex/income status. Figure 1 and Table S2 present the variation of risk factors in different provinces. The association between the underlying risk factors and the outcome varied substantially between provinces (Fig. 1). Among all the included factors, the association between socioeconomic factors and being HCUs has the largest variation across provinces, especially factors, such as immigrant status, visible minority, and some types of occupations.
Table 4 presents the sensitivity analysis results. When using the frequency of hospitalizations and frequency of ED visits to define HSUs and the thresholds of 5% and 1% to define HCUs, the associations between living in rural area and being visible minority and the status of being HSUs of acute care were distinct from the primary analysis. The impact of interaction terms was minimal on coefficients of variables except the comorbidity score. The impact of missing data on the analysis results was minimal.
Discussion
In the context of rising health care expenditures and limited resources, managing HSUs plays a critical role in improving the value and sustainability of health care [29]. In this population-based retrospective study, we used national linked data sets to identify demographic, socioeconomic, and clinical factors associated with high use of health care resources, with an exploration of provincial variations of these factors.
Our study has several important findings. Overall, a few risk factors including older age, being male, being low-income and being medically complex were identified to be associated with being acute care HCUs. We extended this analysis by adding socioeconomic predictors, such as work activity, occupation category and interaction terms between the comorbidity score and age/sex/income status. Higher work activity is associated with lower odds of being acute care HCUs. The impact of patients’ comorbidities could be modified by their age, sex, and income status. The significance of the selected predictors and their impact on the status of being acute care HCUs are different across provinces in Canada and different definitions of HSUs.
Consistent with findings of previous studies, older age and increasing comorbidity were associated with higher costs [3, 11, 13, 14, 30]. Older adults often have multiple chronic conditions, the financial burden of which tends to be high [31]. Based on estimates from the Public Health Agency of Canada, the annual direct healthcare costs of cancers, cardiovascular diseases, chronic lower respiratory diseases and diabetes were estimated to be $10.5 billion in Ontario [32]. Except for the above chronic illnesses, recent studies have found that patients with dementia and mental health conditions also incur high healthcare spendings [33,34,35]. The management of these chronic conditions could be prominent to reduce preventable healthcare costs. Joynt et al. found that 9.6% of Medicare HCUs’ inpatient costs were preventable [9]. Most of these preventable costs were related to congestive heart failure, bacterial pneumonia, chronic obstructive pulmonary disease, urinary tract infection and long-term diabetes complication [9]. Similarly, 9% of the acute care spending of HCUs with cancer in Ontario, Canada was potentially preventable [36]. In spite of the low percentage of preventable costs among HCUs, a recent study in Medicare beneficiaries has shown that 43.6% of total preventable spendings were used by high-cost frail elderly patients and related to urinary tract infections, dehydration, heart failure and bacterial pneumonia [37]. Further research is needed to investigate the degree and distribution of preventable healthcare costs among different groups of older patients to inform the design of strategies for cost prevention and reduction.
Previous HSU studies in Canada mainly focused on one province, such as Ontario, Alberta or British Columbia [2, 3, 6, 11, 35, 38]. Our study explored the risk factors of being acute care HCUs in all provinces in Canada and demonstrated that the association between predictors and the status of being HCUs varies across provinces, especially in Prince Edward Island (PE) and Northern Canada. Socioeconomic predictors tend to have more considerable provincial variations than comorbidity score. This might be related to the relatively small sample size of PE and Northern Canada in our analysis and their distinct population structures and social characteristics from other provinces [15, 17, 18]. For example, on July 1, 2012, residents in Nunavut, Northwest Territories and Yukon (three territories of Northern Canada) have a median age of 24.7, 32.1 and 39.4 years and a proportion of persons aged 65 and over of 3.3%, 6.2% and 9.4% [17]. On the contrary, residents in provinces other than Northern Canada have a median age from 36.1 to 44.2 years and a proportion of persons aged 65 and over from 11.1% to 17.2% [17]. The risk factors identified at the provincial level could potentially inform further research and interventions in different provinces. For example, the impact of being a visible minority on the odds of being HCUs varies across provinces. The reasons behind this could be associated with the varying levels of education and the unemployment rate of visible minorities in different provinces, which warrants further investigation and design of targeted interventions for this population, such as training programs to improve their employment opportunities [39].
Similar to the findings of Wick et al., we also observed that using different definitions of HSUs (cost, length of stay, frequency of discharges and frequency of ED visits) captures different populations [4]. While the independent factors identified using the length of stay to define HSUs are similar to the primary analysis in which HSUs are defined based on cost, factors identified using the frequency of hospitalizations and frequency of ED visits are distinct from the primary analysis. For example, when HSUs are defined based on the frequency of hospitalizations and frequency of ED visits, living in rural areas was associated with higher odds of being acute care HSUs. In contrast, living in rural areas was associated with lower odds of being HSUs in other HSU cohorts. These suggest that different HSU definitions are not interchangeable, and the selection of the most appropriate definition should depend on the research objective.
One major strength of this study is that the linked data set used in our study allows us to analyze a broad range of demographic, socioeconomic and clinical factors potentially associated with the high use of healthcare resources at the national level and to explore provincial variations of these factors. The HCU risk factors identified at the national level provide a full picture of characteristics of acute care HCUs in Canada. Another strength is that we investigated the variations of patient characteristics across different definitions of HSUs in Canada, which advances our understanding of the heterogeneity in HSUs. However, our study also has limitations. First, the information for each patient is retrieved from different databases with different data collection times. There is a time lag between the demographic and socioeconomic information collected within the Census 2006/NHS 2011 and patients’ status of being high system users or non-high system users from 2011 to 2014. We addressed this problem by setting priorities of using data from different databases to ensure the data we used for the analysis is as up-to-date as possible [20]. For example, the order of using information for socioeconomic factors in our study was T1FF 2011–2014, NHS 2011 and then Census 2006. Second, the risk factors identified when the thresholds of 5% and 1% were used to define HCUs should be interpreted with caution as we used RIW as a proxy for costs and only typical patients with RIWs were included in these analyses. This may leave some high cost but atypical patients excluded from the analysis. Third, the identified risk factors only reflected the characteristic differences between acute care HSUs and non-HSUs when the threshold of 10% was used to define HSUs. When using different thresholds, the association between the risk factors and being HSUs varies. Finally, it is important to note that the relationship between the identified risk factors and the status of being acute care HSUs was associational rather than causal and that the analysis was limited to the health care setting of acute care.
Conclusions
A few demographic, socioeconomic, and clinical factors were associated with high use of acute care expenditures. The associations between included risk factors and being acute care HCUs vary across provinces and different definitions of high system users (HSUs).
Availability of data, material, and code
The data used in this study are confidential and requires application to the Statistics Canada for access. The study protocol, analytic code and other materials are available from the corresponding author on reasonable request.
References
Wammes, J.J.G., van der Wees, P.J., Tanke, M.A.C., Westert, G.P., Jeurissen, P.P.T.: Systematic review of high-cost patients’ characteristics and healthcare utilisation. BMJ Open 8, e023113 (2018)
Reid, R., Evans, R., Barer, M., Sheps, S., Kerluke, K., McGrail, K., Hertzman, C., Pagliccia, N.: Conspicuous consumption: characterizing high users of physician services in one Canadian province. J. Health Serv. Res. Policy 8, 215–224 (2003)
Rais, S., Nazerian, A., Ardal, S., Chechulin, Y., Bains, N., Malikov, K.: High-cost users of Ontario’s healthcare services. Heal Policy 9, 44–51 (2013)
Wick, J., Hemmelgarn, B., Manns, B., Tonelli, M., Quan, H., Lewanczuk, R., Ronksley, P.: Comparison of methods to define high use of inpatient services using population-based data. J. Hosp. Med. 12, 596–602 (2017)
Urbanoski, K., Cheng, J., Rehm, J., Kurdyak, P.: Frequent use of emergency departments for mental and substance use disorders. Emerg. Med. J. EMJ 35, 220–225 (2018)
Chechulin, Y., Nazerian, A., Rais, S., Malikov, K.: Predicting patients with high risk of becoming high-cost healthcare users in Ontario (Canada). Heal Policy 9, 68–79 (2014)
Hirshon, J.M., Risko, N., Calvello, E.J., Stewart de Ramirez, S., Narayan, M., Theodosis, C., O’Neill, J.: Health systems and services: the role of acute care. Bull. World Health Organ. 91, 386–388 (2013)
Canadian Institute for Health Information. National Health Expenditure Trends, 1975 to 2019 CIHI. https://www.cihi.ca/en/national-health-expenditure-trends-1975-to-2019 (2019). Accessed 25 Nov 2020
Joynt, K.E., Gawande, A.A., Orav, E.J., Jha, A.K.: Contribution of preventable acute care spending to total spending for high-cost Medicare patients. JAMA 309, 2572–2578 (2013)
Wodchis, W.P., Austin, P.C., Henry, D.A.: A 3-year study of high-cost users of health care. CMAJ 188, 182–188 (2016)
Ronksley, P.E., Kobewka, D.M., McKay, J.A., Rothwell, D.M., Mulpuru, S., Forster, A.J.: Clinical characteristics and preventable acute care spending among a high cost inpatient population. BMC Health Serv. Res. 16, 165 (2016)
Fitzpatrick, T., Rosella, L.C., Calzavara, A., Petch, J., Pinto, A.D., Manson, H., Goel, V., Wodchis, W.P.: Looking beyond income and education: socioeconomic status gradients among future high-cost users of health Care. Am. J. Prev. Med. 49, 161–171 (2015)
Rashidi, B., Kobewka, D.M., Campbell, D.J.T., Forster, A.J., Ronksley, P.E.: Clinical factors contributing to high cost hospitalizations in a Canadian tertiary care centre. BMC Health Serv. Res. 17, 777 (2017)
Singer, A., Kosowan, L., Katz, A., Ronksley, P., McBrien, K., Halas, G., Williamson, T.: Characterizing patients with high use of the primary and tertiary care systems: a retrospective cohort study. Health Policy Amst. Neth. 124, 291–297 (2020)
Government of Canada. Canada’s Health Care System. https://www.canada.ca/en/health-canada/services/health-care-system/reports-publications/health-care-system/canada.html (2019). Accessed 19 Jun 2020
Marchildon, G.: Health systems in transition: Canada, 2nd edn. University of Toronto Press, Canada (2013)
Statistics Canada Annual Demographic Estimates: Canada, Provinces and Territories: Section 2: Population by age and sex. https://www150-statcan-gc-ca.libaccess.lib.mcmaster.ca/n1/pub/91-215-x/2012000/part-partie2-eng.htm. (2020). Accessed 19 Jun 2020
Health Council of Canada. Where You Live Matters: Canadian Views On Health Care Quality. Results from the 2013 Commonwealth Fund International Health Policy Survey of the General Public. Canadian Health Care Matters, Bulletin 8. Toronto, ON: Health Council of Canada. https://healthcouncilcanada.ca/806/ (2014). Accessed 20 Jun 2020
Canadian Research Data Centre Network. HSUS-T1FF-CENSUS-NHS (high system users linked to T1 Family File-census of the population long-Form-national household survey). https://crdcn.org/taxonomy/term/4530 (2019). Accessed 16 Jul 2019
Zhang, M., Ma, J., Xie, F., Thabane, L.: Identifying factors associated with high use of acute care in Canada: protocol of a population-based retrospective cohort study. BMJ Open 10, e038008 (2020)
Canadian Institute of Health Research. Dynamic Cohort of Complex, High System Users—2011–2015. http://www.cihr-irsc.gc.ca/e/50129.html#section_3_3 (2019). Accessed 16 Jul 2019
Canadian Institute for Health Information. Discharge Abstract Database Metadata (DAD). https://www.cihi.ca/en/discharge-abstract-database-metadata (2019). Accessed 16 Jul 2019
Lynch, S., Brown, J. Endogeneity—an overview | ScienceDirect Topics. https://www.sciencedirect.com/topics/psychology/endogeneity (2011). Accessed 8 Nov 2022
Thavorn, K., Maxwell, C.J., Gruneir, A., Bronskill, S.E., Bai, Y., Pefoyo, A.J.K., Petrosyan, Y., Wodchis, W.P.: Effect of socio-demographic factors on the association between multimorbidity and healthcare costs: a population-based, retrospective cohort study. BMJ Open 7, e017264 (2017)
van Buuren, S.: Multiple imputation of discrete and continuous data by fully conditional specification. Stat. Methods Med. Res. 16, 219–242 (2007)
Manitoba Center for Health Policy. Term: Resource Intensity Weights (RIWTM). http://mchp-appserv.cpe.umanitoba.ca/viewDefinition.php?printer=Y&definitionID=103807 (2009). Accessed 19 Apr 2022
University of Manitoba, MCHP concept dictionary and glossary for population-based research. Term: Typical Patient. http://mchp-appserv.cpe.umanitoba.ca/viewDefinition.php?definitionID=103699 (2022). Accessed 16 Nov 2022
R Core Team. R: A language and environment for statistical computing (2020)
Austin, P., Newman, A., Corallo, A., Henry, D.: The Concentration of Health Care Spending: Little Ado (yet) About Much (Money). http://www.longwoods.com/blog/the-concentration-of-health-care-spending-little-ado-yet-about-much-money/ (2013). Accessed 20 Mar 2020
Ronksley, P.E., Hemmelgarn, B.R., Manns, B.J., Wick, J., James, M.T., Ravani, P., Quinn, R.R., Scott-Douglas, N., Lewanczuk, R., Tonelli, M.: Potentially preventable hospitalization among patients with CKD and high inpatient use. Clin. J. Am. Soc. Nephrol. CJASN 11, 2022–2031 (2016)
Suzman, R., Beard, J.R., Boerma, T., Chatterji, S.: Health in an ageing world–what do we know? Lancet Lond. Engl. 385, 484–486 (2015)
Public Health Agency of Canada. Economic Burden of Illness in Canada, 2010. https://www.canada.ca/en/public-health/services/chronic-diseases/chronic-disease-knowledge-development-exchange/economic-burden-illness-canada.html (2018). Accessed 17 Nov 2022
de Oliveira, C., Cheng, J., Vigod, S., Rehm, J., Kurdyak, P.: Patients with high mental health costs incur over 30 percent more costs than other high-cost patients. Health Aff. Proj. Hope 35, 36–43 (2016)
Wick, J., Campbell, D.J.T., McAlister, F.A., Manns, B.J., Tonelli, M., Beall, R.F., Hemmelgarn, B.R., Stewart, A., Ronksley, P.E.: Identifying subgroups of adult high-cost health care users: a retrospective analysis. CMAJ Open 10, E390–E399 (2022)
de Oliveira, C., Cheng, J., Rehm, J., Kurdyak, P.: The role of mental health and addiction among high-cost patients: a population-based study. J. Med. Econ. 21, 348–355 (2018)
de Oliveira, C., Cheng, J., Chan, K., Earle, C.C., Krahn, M., Mittmann, N.: High-cost patients and preventable spending: a population-based study. J Natl. Compr. Canc. Netw. 18, 23–31 (2020)
Figueroa, J.F., Joynt Maddox, K.E., Beaulieu, N., Wild, R.C., Jha, A.K.: Concentration of potentially preventable spending among high-cost medicare subpopulations: an observational study. Ann. Intern. Med. 167, 706–713 (2017)
Ronksley, P.E., McKay, J.A., Kobewka, D.M., Mulpuru, S., Forster, A.J.: Patterns of health care use in a high-cost inpatient population in Ottawa, Ontario: a retrospective observational study. CMAJ Open 3, E111-118 (2015)
Government of Canada. Visible minorities in Canada-ARCHIVED. http://www150.statcan.gc.ca/n1/pub/85f0033m/85f0033m2001009-eng.pdf (2020). Accessed 27 Nov 2020
Funding
This study has received no funding.
Author information
Authors and Affiliations
Contributions
MZ, and LT conceptualized and designed this study. MZ statistically analyzed the data and wrote the draft manuscript. JM, FX and LT critically revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors have completed the ICMJE uniform disclosure form and confirmed that there was no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
All authors read and approved the final manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, M., Ma, J., Xie, F. et al. Identifying factors associated with high use of acute care in Canada: a population-based retrospective study. Eur J Health Econ 24, 1505–1515 (2023). https://doi.org/10.1007/s10198-022-01558-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-022-01558-3