Abstract
Like many OECD countries, Germany is currently facing a shortage of long-term care (LTC) workers. This situation is concerning in the context of the ageing of the German population. A potential reason why Germany fails to recruit and retain LTC workers is that LTC jobs are particularly demanding (physical and psychological strain) which may be harmful to health. However, there is a lack of empirical evidence demonstrating this effect. This article fills the gap in the literature by exploring to what extent LTC jobs reduce workers’ health over time. We estimate a dynamic panel data model on the German Socio-Economic Panel (v.35; 1984–2018), which allows adressing selection issues into occupations. Our paper provides innovative findings on the impact of LTC occupations on workers’ health. We confirm that LTC jobs have a negative impact on self-reported health. Our results have strong policy implications: we emphasize the need to provide sufficient assistance to LTC workers, who are at risk of facing more health issues than other workers. This issue is key to increase the attractiveness of LTC jobs and reduce turnover in the LTC workforce.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 1995, Germany became one of the few countries to introduce a mandatory, universal long-term care (LTC) insurance system [1, 2]. However, this system has encouraged informal care arrangements [3], and compared to their peers in neighbouring countries such as the Netherlands, German elders rely more on informal care providers [4]. A large share of the LTC supply is provided through black-market arrangements [5], and the number of LTC workers per 100 people aged 65+ (5.1/100) is far below the supply observed in countries that have also implemented LTC insurance systems, such as the Netherlands (8.0/100), Sweden (12.4/100) and Norway (12.7/100) [6].
While the German system has held LTC spending under the OECD country average (1.5% vs. 1.7% of GDP), it is now facing important issues. The supply of informal care has decreased since 1995 due to several factors, including the ageing of the population, the increasing participation of women in the labour market, and changes in family structure, raising an urgent need to enhance the supply of formal care services [6]. Germany faced one of the largest increases in the demand for LTC services between 2007 and 2017 [6] and now ranks fourth among OECD countries with respect to the share of adults aged 65+ receiving LTC (15.6% in 2017). Half of these recipients are over 80 years of age, suggesting important needs.
Therefore, the German system is currently seeking to increase the supply of professional LTC workers. The professionals who provide these services, so-called LTC workers, are often nurses and personal care workers employed in home-based or institution-based settings [7]. While the 65+ population has increased in recent decades, the overall supply of LTC workers nurses has decreased, raising tensions between the supply of and demand for LTC services [8]. This situation has been exacerbated by the high turnover rate in LTC professions; for instance, rates of absenteeism due to sickness are higher among LTC workers than in other occupations [9].
One reason for the limited attractiveness of LTC jobs is that they are usually low-quality positions in the sense that they are low paid and mostly rely on part-time arrangements. For instance, half of LTC workers in Germany have a part-time contract [6]. Another potential explanation is that LTC jobs are also harmful, e.g., participating in the LTC workforce is hazardous to worker health. LTC workers often face workplace violence [10, 11], leading them to suffer from psychological strain, and exhibit increased burnout [11]. Moreover, LTC jobs frequently require workers to perform physical activities, such as carrying people, that can lead to back problems. Such stressful and physically demanding tasks could explain why LTC workers’ health worsen more rapidly over time compared to workers in other occupations.
From a theoretical perspective, the health capital accumulation model provides an interesting framework to anticipate the impact of LTC jobs on workers’ health [12]. According to this framework, health is a durable stock that depreciates over time at a given rate that can be reduced through health investment. The cost of investment in health services and prevention is higher for low-income than for high-income individuals, reducing the former’s capacity to invest in health care services; as a result, low-income individuals also face difficulties in compensating for the depreciation of their health capital over time. The Grossman model shows that human capital factors, such as education, also contribute to explaining health differences. A higher level of education increases one’s level of information about medical services, which increases the productivity of health investment. The low-skilled/low-pay nature of most LTC jobs and the lower education levels of LTC workers [6] could explain the higher rate of depreciation of their health status over time.
In addition, there is evidence that accidents at work are more frequent in the LTC sector than in the hospital sector and that work-related health issues and accidents at work are strongly correlated [13]. Specifically, nearly two thirds of LTC workers in OECD countries report exposure to physical risk factors, and almost half of LTC workers report exposure to mental well-being risk factors. Furthermore, the OECD identifies LTC jobs as low-quality jobs because of excessive regulatory constraints, insufficient investment to provide quality care, lack of supportive leadership, and difficulty of maintaining good work-life balance [13]. Prior work underlines that these job stressors can negatively impact workers’ quality of life [14]. All of these factors support the assumption that LTC jobs are more harmful to health than similar occupations.
Empirical studies also tend to corroborate the hypothesis that LTC jobs have a negative impact on workers’ health. Prior work suggests that contractual (such as flexible job arrangements) and working conditions affect worker health [15, 16]. More recently, empirical evidence [17] shows that in Germany, the health of workers involved in occupations that carry physical and psychosocial burdens (i.e., ‘blue-collar’ occupations) depreciates faster than that of workers with less physically demanding jobs (i.e., ‘white-collar’ occupations). LTC-related occupations fall in the ‘blue-collar’ occupation category, so one may assume that a similar conclusion may hold among the LTC worker population. Recent work [13] underlines that LTC jobs are low-quality jobs that are often associated with physical and psychological burdens. Because most tasks provided by LTC workers in Germany are physically demanding, one can assume that the detrimental effect of LTC jobs will be higher among older workers.
To the best of our knowledge, no article has isolated the impact of LTC jobs on workers’ health. The objective of this article is to test the hypothesis that LTC workforce participation has a negative impact on health. Following prior work [17], we explore this issue using a dynamic model estimated on the German Socio-Economic Panel (GSOEP). Our main findings show that while new LTC workers report on average a better health status than workers in similar occupations, participating in the LTC workforce in a given year has a negative impact on health in the following year. Moreover, this effect seems to be explained by the nature of LTC jobs, since LTC workers’ health is worse than that of hospital-based workers (in similar occupations), though the effect is not statistically significant at conventional thresholds. Finally, we do not find evidence that older LTC workers experience greater health depreciation compared to younger LTC workers.
The paper proceeds as follows. We first describe the GSOEP database. We then present the empirical strategy and sensitivity analyses, report the obtained results, and discuss our findings.
The German Socio-Economic Panel
We exploit the GSOEP (v35) over the period 1984-2018. It is a longitudinal household survey containing detailed information to analyse the relationship between work and health. Respondents are followed over multiple waves, but the panel is unbalanced because many respondents enter the sample after 1984 or leave the sample before 2018. Thus, if a maximum of 29 observations (waves) per individual is theoretically possible, respondents are actually observed across an average of 11 waves. We impose some restrictions on the sample. We first restrict our sample to 1995+ since the first German LTC reform was introduced in 1995, leading us to use 24 subsequent annual waves (from 1995 to 2018). We select individuals aged 16–64 years without missing values for health or the socio-demographic variables used in the analysis. Finally, to estimate panel data models that include a lagged dependent variable, we further restrict the sample to individuals observed at least twice during 1995–2018 period.
Construction of the LTC workforce participation variable
The database provides detailed information on employment status in the form of the International Standard Classification of Occupations (ISCO) and NACE codes. ISCO is a four-level classification of occupation groups managed by the International Labour Organisation (ILO). Its structure follows a grouping by education level. A total of 307 occupational titles are classified into nine major occupational groups ranked by the OECD classifications. The Statistical Classification of Economic Activities in the European Community, commonly referred to as NACE (“Nomenclature statistique des Activités économiques dans la Communauté Européenne”), is the industry standard classification system used in the European Union. Note that both classifications have evolved over time, with an amendment to the ISCO codes in 2008 (from ISCO88 to ISCO08), while the current NACE classification (NACE rev.2) officially entered into application in 2007. The change in the database was applied in 2013. By cross-referencing the two classifications, we recreate precise sets of jobs to compare. The LTC workforce follows the OECD’s definition and is composed of nurses and personal carers providing care and/or assistance to people limited in their daily activities.Footnote 1 We then create a second group that comprises all occupations considered similar to LTC jobs (according to the OECD classification), called “similar jobs”. Appendix A details the ISCO and NACE codes used to create the “similar jobs” category.
The three panels
We create three nested panels (A, B, and C) to explore our research question at three different level: First, are LTC jobs and similar care jobs more harmful than all other occupations (question explored in Panel A)? Second, are LTC jobs more harmful than similar services provided in different industries—e.g., childcare assistant—(question explored in Panel B)? Third, do we find differences between the LTC sector and the hospital sector when comparing similar occupations (question explored in Panel C)?
Panel A: LTC/similar workers vs. all other workers. Our first study sample—“panel A”—contrasts the workforce for LTC/similar jobs to that for all other jobs. This first sample includes 352,942 person-wave observations, with 70,159 different individuals and a median number of observations (per person) of 5. There are several rationales for gathering LTC and similar occupations together. First, these jobs require very similar skills, e.g., with an identical average level of education (see the “Descriptive statistics” section) and differ primarily in working environment. Second, both groups of jobs have tight labour markets. Thus, the two sectors are perpetually searching for workers, with many unfilled vacancies and high turnover of workers already hired. In our sample, 12% (resp. 22%) of LTC workers (similar workers) experience at least one transition period outside of their sub-group. Thus, we compare workers who switch occupations quite easily, for example, due to difficult working conditions. In our context, the similar workforce must be a pool of workers viewed as potentially attractive to fill the growing number of LTC job vacancies. Within the panel A, there were 3431 transitions from all other jobs to LTC/similar jobs, and 3280 transitions in the opposite direction.
Panel B: LTC workers vs. similar workers. Our second sample—“panel B”—is a sub-sample of panel A and distinguishes LTC workers from similar workers. This second sample contains 14,157 person-wave observations (10,185 person-wave observations for LTC jobs and 3972 person-wave observations for similar jobs), with 3760 different individuals and a median number of observations of 5. Within panel B, only 60 transitions from similar jobs to LTC jobs occured, while 204 LTC workers left the LTC sector to join a similar job in another sector. Our aim in analysing panel B is to investigate precisely the differential impact on health of joining the LTC workforce compared to joining another similar occupation.
Panel C: LTC workers vs. hospital workers. Our third sample—“panel C”—is a sub-sample of panel B and distinguishes between LTC and hospital workers from 2013 to 2018. Indeed, the 2012 revision of the NACE nomenclature introduced a separate category for hospital workers, allowing us to compare personal care workers and nurses working in LTC from workers in the same occupations working in hospitals. This distinction could not be done before 2013, because both sectors were pooled in the broader “health services” category, and were thus indistinguishable. Therefore, under the NACE rev.2 nomenclature, we estimate the health effect of being an LTC worker in a home or residential facility (classified under codes 87 and 88, hereafter LTC workers) relative to personal care workers and nurses practising in hospitals (classified under code 86, hereafter hospital workers). This allows us to perfectly replicate the OECD’s definition (which excludes the hospital sector of LTC jobs) while comparing two jobs requiring exactly the same skills performed in different work environments. This second sample contains 3124 person-wave observations (1243 person-wave observations for LTC workers and 1881 person-wave observations for hospital workers), with 1202 different individuals and a median number of observations of 2. For the panel C, 129 transitions from hospital towards the LTC sector (home or institution) occurred, and 92 transitions were observed from the LTC sector towards the hospital sector.
Outcome variable
We use self-perceived health (SPH), measured on an integer scale from 0 to 10, as our health outcome variable. Although it is a subjective measure of health, a number of studies show that self-rated health is highly correlated with other objective measures and is a strong predictor of morbidity and mortality [18,19,20,21]. Because this study essentially focuses on individuals in the labour force (16–64 years), SPH is necessarily high. Appendix B shows that the SPH distributions are highly concentrated and quasi-similar for our six sub-samples, with on average 22% of each sub-population reporting a SPH less than or equal to five.
Empirical strategy
Econometric models
We use two main steps to better understand the effect of occupation (e.g., being an LTC worker) on SPH. First, we use an ordinary least squares (OLS) regression to model the correlation between occupation and SPH. This model allows us to control for time (age)-specific fixed effects, i.e., shocks for which the impact is restricted to a given time period, or temporal variations that cannot be controlled for by the variables included in the model. We use the following specification:
where \(h_{i,t}\) is the SPH for individual i at time t, \(O_{i,t-1}\) is a dummy variable denoting occupation in the previous year, \(\epsilon _{i,t}\) is an idiosyncratic error term that varies across subjects and over time, \(\alpha\) is the constant term, and \(x_{i,t}\) is a vector of control variables, including wave dummies and age group (9-year age bands, from ages 16–24 to ages 55–64) to control for (potentially non-linear) age effects and a common time trend.
Despite these controls, a selection problem may arise: \(O_{i,t-1}\) could be correlated with unobservable time-varying or time-invariant characteristics. This could happen if individuals self-select into LTC jobs earlier based on their better health, e.g., anticipating that they will be able to endure difficult working conditions. If these factors are not controlled for, then the OLS estimates will be biased, and \(\beta\) will not represent the causal effect of occupation on SPH. This potential estimation issue leads us to use another estimation strategy.
Second, following [17], we estimate a fixed effects (FE) dynamic panel data model allowing us to control for various sources of selection (time-varying and time-invariant) into occupation. Selections into LTC job occupations are likely to occur because of time-invariant characteristics (e.g., education) or time-varying factors (e.g., health). In the OLS specification, the impact of LTC jobs is embedded in the influence of the socioeconomic profile of LTC jobs candidates (e.g., lower levels of education). The dynamic FE specification allows netting out of the effects arising from differences in education levels (or initial health) in selecting an LTC job, thus addressing the endogenous nature of choosing a LTC job. After demeaning the covariates to eliminate time-invariant factors, the model is written as follows:
Using a within transformation of Eq. 1 allows us to remove the effect of any individual characteristics that are constant over time. Controlling for lagged health (\(h_{i,t-1}\)) makes it possible to purge the occupational effect from all time-varying unobserved shocks, to the extent to which their impacts decay exponentially at the same rate over time [17]. From a theoretical perspective, the lagged health effect is directly derived from Grossman’s model, which explores the health capital variations occurring between 2 periods of time. Introducing the lagged health variable thus allows us to follow Grossman’s theoretical framework. This variable captures the health capital depreciation rate over several periods—in our case, over a 2-year span—see [22]. In Eq. 2, \(\beta\) represents the net impact of entering occupation O in year \(t-1\) on health in year t. This model is estimated on our three panels A, B and C. The only difference is that occupation O differs in each panel.
Sensitivity analyses
Our dynamic FE model is estimated by OLS regressions applied to the time-centered variables. In this case, there is a potential correlation between the lagged dependent variable and the demeaning terms in the error. Importantly however, as showed by [23] and [24], the estimator is consistent for large T (in this case, the correlation between the mean of the errors term across the periods, \(\overline{\in _{i}}\) and \(y_{t-1}\) become small). While the GSOEP database allows observing individuals across a high number of waves (up to 24 waves), our panel A and B are limited to a median of 5 observations per individual—and only 2 for the panel C, which is not sufficient to satisfy this criterion.
We decided to further explore the robustness of our results by running a different specification. First, we followed an approached defined by [25]: we estimated a non-dynamic FE model and compared the results with the dynamic model, which controlled for the lagged dependent variable. The results were robust to this alternative specification. Second, we estimated two additional models: a dynamic and a non-dynamic correlated random-effects model [26], which is not subject to the above-mentioned limitation (i.e., the correlation between \(\overline{\in _{i}}\) and \(y_{t-1}\)). Third, as recent work [27] underlines that the use of dynamic CRE estimations can be problematic in unbalanced panel, we also ran a non-dynamic CRE model and compared the results to the dynamic CRE model. Both models provided similar results. Fourth, we explored the robustness of our results using a slightly different declarative health scale in the data, i.e. the probability of reporting a poor health.
Finally, we checked whether our results hold across several sub-groups. We reproduced our main dynamic FE model stratifying according to level of education (years of education), sex, nationality and employment status (part-time vs. full-time) for panel A and panel B. Note that because its sample size was too small, we did not replicate the sensitivity analyses for panel C. We also tried a different specification to deal with the kurtosis of our dependent variable; we log-linearized SPH to smooth-out its distribution. The conclusions were similar (results not reported but available upon request).
Results
Descriptive statistics
Table 1 compares our two populations in panels A, B and C to assess whether there are significant differences in terms of self-perceived health (SPH) and socio-demographic characteristics. Only the differences that are significant at the 5% level are described below.
Panel A: LTC/similar jobs vs. all remaining jobs. The first sub-table summarizes the differences in observable characteristics for panel A, comparing LTC/similar jobs with all remaining jobs. Compared with workers in all remaining jobs, the LTC/similar workforce is on average younger (39.66 years vs. 41.03), mostly female (88.26% vs. 51.47%), and less likely to work full time (42.74% vs. 46.08). Moreover, the average low job tenureFootnote 2 (4.08 years) and the very low percentage of individuals remaining in the occupation for at least 4 years (37.93%) emphasize the very high turnover in occupations consistently in need of workers. On average, LTC/similar workers have better subjective health (SPH=7.06 vs. 6.93).
Panel B: LTC jobs vs. similar jobs. The second sub-table shows the differences in observable characteristics between LTC and similar workers. Regarding socio-demographics, the two groups are identical in terms of education and share of immigrants.Footnote 3 The proportion of men is very low in both groups, with only 12.27% (resp. 10.40%) of men in LTC jobs (resp. similar jobs). The average observed job tenure is very low for similar jobs (2.33 years) and LTC jobs (4.75 years) compared to all other jobs (at approximately 9 waves, see Panel A), consistent with the high turnover in both occupations.
Panel C: LTC vs. hospital workers. The third sub-table emphasizes differences between LTC and hospital workers. First, we observe that age and share of immigrants are higher compared to the other two panels. The two groups are not significantly different in terms of age, share of immigrants or job tenure. Compared to hospital workers, LTC workers are more likely to be female, have a lower level of education, and be part-time workers. Moreover, LTC workers’ health (6.63) is on average lower than hospital workers’ health (6.99).
Figure 1 compares the age distributions across our six analysed sub-groups. We note that each distribution is normal. This ensures that one, our results do not suffer from clustering, and two, heterogeneity in age is sufficient for a life-cycle analysis.
Age distributions of panels A, B and C. The two top graphs (panel A) show the self-perceived health distributions for our group of interest (left chart), composed of LTC and similar workers, and our first comparison group (right chart), composed of all remaining workers. The middle graphs (panel B) reproduce the distributions for LTC jobs (left chart) and for similar jobs (right chart). The bottom graphs (panel C) describe the distributions for the LTC workers (left chart) and for personal care workers and nurses practising in hospital settings (right chart). Source: GSOEP, v35 (1995–2018)
Results of econometric models
Panel A First, we estimate the impact of being an LTC/similar worker on health compared to all other jobs (Table 2). The OLS model in column 1 (Eq. 1) shows that, on average, the LTC/similar workforce report a higher SPH (\(\beta\) = 0.032*), which is significant at the 10% level. As stated in the previous section, this positive effect could be driven by health-related selection in LTC/similar jobs. The effect found through the FE dynamic panel data model (column 2; Eq. 2) highlights a significant negative effect of entering the job (\(\beta\) = − 0.060***).
To better understand the coefficients magnitude, we can represent the effect of entering to the LTC/similar workforce rather than all other jobs in terms of years of aging [17]. By calculating the average health deterioration of growing 1 year older (obtained from an individual fixed-effects regression of self-perceived health on age)—which corresponds to a coefficient of − 0.0539***—we find that joining the LTC/similar workforce translates into 13 months (\(-0.06 \times 12 / -0.0539\)) of aging. Column 3 uses the FE specification but adds an interaction term between job at t-1 and age group. The first coefficient (\(\beta\) = − 0.081) refers to the effect of job entry for age group 16–24 years (the reference level), and the other effects are interpreted as deviations from this effect for older cohorts. We find two main results. First, the youngest workers experience the largest depreciation in SPH (all the occupation \(\times\) age group effects are positive, though not statistically significant). Second, the overall effect of LTC occupation is negative across all age groups. Because none of the interaction terms were significant at the 5% level, we conclude that age of entry into the job does not seem to affect the average effect shown in column 2.
Panel B Second, we study the effect of joining the LTC workforce on health compared to working in a similar job (Table 3). The OLS results in column 1 (Eq. 1) does not reveal a significant relationship between entering the LTC workforce (compared to a similar job) in the previous year and SPH values the next year (\(\beta\) = − 0.039). However, the effect obtained with the dynamic FE specification (column 2) is much stronger in absolute terms (\(\beta\) = − 0.198**) and significant at 5% level. By calculating the average health deterioration of growing 1 year older, we find that joining the LTC workforce translates into 45 months (\(-0.198 \times 12/-0.0528\)) of aging. Results obtained for the occupation \(\times\) age interactions (column 3) do not reveal any significant modifying effect due to age group. Note however that the age \(\times\) occupation interactions are all positive, which suggest that the negative health effect of entering the job at t-1 tends to be lower with older age. This could be explained by a selection effect where individuals joining the LTC workforce are relatively in better health.
Panel C Third, we estimate the impact of being an LTC worker on health relative to personal care/nurses employed at hospitals after 2012 (Table 4). The OLS model (column 1) shows a strong negative impact of working in the home or residential facilities on health (\(\beta\) = − 0.400***). By contrast, adding individual FE (column 2) reduces the effect (\(\beta\) = − 0.070), which is no longer statistically significant. By calculating the average health deterioration of growing 1 year older—which corresponds to a coefficient of − 0.0916***—we find that joining the LTC workforce at home/nursing home translates into 9 months (\(-0.07 \times 12/-0.0916\)) of aging. Finally, the column 3 highlights that the effect of job entry on health does not vary significantly according to age, though the effect tend to become more negative with age. Yet caution is needed in interpreting these results because of the low sample size (and limited number of transitions towards LTC workforce), which may explain that none of the effects were significant (Table 4).
Results of the sensitivity analyses
In sensitivity analyses, we first show that our results remain consistent using non-dynamic FE and CRE models (Appendix C: Tables 7, 8, and 9). We further explore the robustness of our results using the probability of reporting a poor health. Indeed, the GSOEP contains an alternative measure of health called self-assessed health (SAH)—derived from the question “How is your health in general?”—measured on an ordinal Likert scale with five answer categories: 1 (“Very good”), 2 (“Good”), 3 (“Satisfactory”), 4 (“Poor”), and 5 (“Bad”). We construct an outcome variable “Poor Health” (PH), which is a dummy that equals 1 if the individual reports that his or her health is “Poor” or “Bad” and 0 otherwise. We replicate the models estimated in Eq. 2 using an FE linear probability model (Appendix C: Table 10). Table 10 summarizes the results for each panel. We observe that joining the LTC/similar workforce increases the probability of being in poor health (β = 0.010*), while the differences are not significant in panel B (β = 0.031)—comparing LTC and similar workers—nor in panel C (β = 0.029*)—comparing home-based and hospital LTC workers. Again, note that the small sample sizes of panels B and C may explain the non-significant impact. Finally, we evaluate whether the negative effect of LTC occupations (and/or similar jobs) on health differs across various socio-demographic variables. We re-estimate our main dynamic FE model (Eq. 2) to show the effect of lagged occupation on health stratified according to specific characteristics such as education, employment status, sex and nationality. Appendix D (Tables 11, 12 and 13) reports the results of these sensitivity analyses for panel A, while Appendix E (Tables 15, 16 and 17) reports the results for panel B.Footnote 4
Effect by education (Panel B) We first estimate whether the negative impact of being an LTC worker differs by educational level. We cut off our sample at 11.5 years of education, based on the existing literature [28] and corresponding to the median education of our sample. Table 15 compares the impact of LTC jobs on less-educated (column 1) and more-educated (column 2) workers. We show that only the more-educated LTC workers experience a significant detrimental effect of their job on health (\(\beta\) = − 0.329**).
Effect by employment status (Panel B) Second, Table 16 contrasts full-time workers (column 1) and part-time workers (column 2). We highlight that the drudgery of the job is largely felt by part-time workers (\(\beta\) = − 0.409*** vs. \(\beta\) = 0.176 for full-time workers). Note that contrary to the other variables, employment status may be endogenous because reductions in working hours are likely to be health induced. According to previous work, temporary work may be damaging to health [29], such that individuals with lower health would select into the sub-group of part-time workers. Nevertheless, the use of dynamic FE specification may partly account for this selection effect provided that health does not varies significantly over two years.
Effect by time-invariant personal characteristics (Panel B) Third, we study whether gender or being a German citizen affects the results of the main estimation. Table 17 reports the estimates for the sub-sample of women (column 1) and for the sub-sample of German citizens (column 2). We show that the negative effect of working in an LTC occupation on health is stronger among women (β = − 0.215***), which suggests that woman’s health seems to be more affected by LTC jobs, while women represent a large share of the LTC workforce.
Discussion
Our paper provides innovative findings on the impact of LTC occupations on workers’ health. We confirm that LTC jobs have a negative impact on self-reported health, while their health is initially better than other workers (selection effect). We find three main results. First, we show that LTC jobs have a negative impact on health compared to other jobs (panel A)—corresponding to 13 months of aging. Second, we find that the effect is even stronger when comparing LTC jobs to similar occupations (panel B)—corresponding to 45 month of aging. Third, while not statistically significant (probably because of a sample size issue), our results suggest that nurses and personal care workers tend to report a lower health when they work in nursing homes or at home compared to when they work in a hospital (9 month of aging). In addition, we find heterogeneous effects according to age, education, employment status, gender and nationality.
Using more robust methodology, our study support previous results suggesting that LTC jobs may be harmful to one’s health [13]. Our empirical analysis, inspired by previous work [17], has several advantages. First, it builds on robust longitudinal German data using an objective classification of occupation. Second, our modelling framework is sufficiently robust to allow us to net out the effect of occupation on health arising from self-selection (e.g., individuals with lower education and/or initial better health self-selecting into more demanding jobs such as LTC jobs). Indeed, our preferred dynamic FE model accounts for three types of selection effects into occupation: (a) unobserved time-invariant variables (through the inclusion of individual FEs), (b) time-varying observed variables such as age and wave dummies, and (c) time-varying unobserved shocks that exponentially die out through the inclusion of the lagged dependent variable [17].
Comparing the results of OLS with those of the fixed-effects estimator (including a lagged dependent variable), therefore, provides a useful assessment of the importance of health-related selection into occupation. We find that failing to control for time-varying and time-invariant selection into occupation would not only bias the results but also lead to the opposite conclusions (i.e., LTC jobs increase health). This is explained by selection effects into LTC occupations, e.g., by the fact that those considering joining the LTC workforce are usually in good health.
Despite their strengths, our analyses face several limitations. First, our estimates can be interpreted as causal only under the stringent assumption that all switches between occupations are random, after conditioning on all time-invariant and time-varying (un)observed characteristics. In practice, as in previous applications of this model [17], we cannot exclude the possibility that unobserved time-varying shocks (e.g., changes in working conditions, family incidents) that are not sufficiently captured by lagged health simultaneously affect occupational switches and health. In the absence of a plausible instrument generating exogenous variation in occupational choice, any causal interpretation of our estimates should be made with caution. Moreover, it can be assumed that the effect of exposure to LTC jobs differs according to job tenure. Nevertheless, the lack of a convincing instrument to account for the endogeneity of job tenure (individuals remaining longer in a job are more likely to be in better health) and the limited number of waves observed (per person) among LTC workers do not allow us to rigorously test this assumption. In other words, our FE models only control for the effect of unobserved variables that do not vary over time. Therefore, it is possible that our regressions still face omitted variables issues. For instance, LTC workers face increased risk of accidents, violence or discrimination issues that are likely to influence both job participation and health [13].
Second, our estimations may suffer from a sample size issue. The results obtained through the dynamic FE model with interaction between profession and age group should be viewed with caution. Indeed, the low number of waves observed (on average) per person associated with an average age of approximately 40 years in our 3 panels may reduce the scope of our results. The interpretation of our coefficients in terms of aging may suffer from this limitation. In particular, we obtain a relatively large coefficient in panel B (although in absolute terms the size of the effect is moderate: − 0.198 point variation on a scale ranging between 0 and 10). We explored whether this difference with the coefficients obtained in Panels A and C could be explained by the fact that there has been a change in the ISCO and NACE nomenclatures in 2012. We explored the potential consequences of the nomenclature change in sensitivity analyses (Tables 14 and 18). We found that the increase in the coefficient magnitude obtained in Panel B seemed to be driven by observations collected after 2013: when restricting our analyses to the years before 2013, the coefficient size decreased and was similar to the one obtained in Panels A and C. To further explore that issue, we replicated our main analysis by using the ISCO-88 and NACE variables (which were provided for all years and did not change over time) and found similar effects. Therefore, we think that the larger coefficient obtained in Panel B is likely to be explained by the small number of transitions that occurred in the LTC workforce after 2012. Furthermore, the most convincing comparison (panel C, comparing LTC workers with hospital-based workers) is limited by the fact that we can only perform our analyses on a small subset of the data, as the NACE nomenclature change allowing that comparison was only introduced in 2012. As a consequence, very few individuals are observed two waves or more, only a few occupation switches could be observed. This could contribute to explain why the effect of LTC occupation is insignificant in Panel C.
Third, our analysis of the channels through which LTC jobs have detrimental effects on health is limited by the fact we lack access to occupational stressors data (e.g., physical strain, low job control, psychosocial workload). In line with the previous analyses [17], we assume that LTC workers are more exposed to these three occupational stressors, thus explaining the negative effect of LTC jobs on health. In addition, our analyses focus on professional LTC workers, but informal caregivers also play a central role in LTC provision. Further work is needed to explore whether providing assistance to dependent older people influences informal caregivers’ health in a similar way.
Our results have important policy implications. In the current context of constrained public budgets and dramatic increases in public LTC spending, it is crucial to prioritize governmental action and identify the most effective policies. To date, measures implemented in OECD countries to reduce turnover rates in the LTC workforce have focused on wage increases [30]. While evidence suggest that in the United States, these policies can be successful in the short term [31], they did not solve turnover issues. Germany introduced several Nursing Welfare Acts to improve the compensation of LTC workers, and the Federal Government is planning to introduce nationwide tariff agreements for elder care professions to guarantee better salaries for LTC staff. While these measures are likely to attract new workers to the LTC sector, our results suggest that the high turnover rate in the LTC workforce will persist due to the negative impact of LTC jobs on workers’ health. Indeed, our results show that while newly attracted workers are usually in better health than their counterparts in other sectors, their health status deteriorates quickly after one year in the profession. Therefore, priority should be given to measures improving working conditions.
The OECD advocates for measures targeting young people. The German LTC workforce is slowly ageing. The median age of LTC workers in Germany was 44 years old in 2016 and has been increasing in Germany as in most OECD countries over time. Empirical evidence in the United States and the United Kingdom shows that engagement in the LTC workforce varies across the life-cycle and follows a bell-shaped curve [13, 32]. The OECD recognizes that retaining workers over the age of 50 is very challenging because the bulk of LTC tasks in Germany are physically demanding tasks like transporting and moving elderly people [13]. For instance, the overall effect of joining the LTC workforce at 18 years of age is not negative because the detrimental impact of LTC jobs is smaller than the health selection effect associated with participation in LTC jobs. In other words, the marginal depreciation in health capital associated with participation in LTC jobs for younger workers is low relative to their overall health capital. By contrast, older workers who join the LTC workforce are rapidly impacted by the detrimental effect of these professions.
Finally, our results suggest the need to provide sufficient assistance to LTC workers, especially when they hold part-time jobs, because they face greater risks of enduring more health issues than other workers. Specifically, there is need to increase health care insurance access for LTC workers, especially when they are self-employed. Assistance is also needed in LTC job practices. New technologies (alarm button services, automated beds, telemedicine, etc.) could provide interesting solutions to assist LTC workers in providing surveillance for disabled elders, reducing reliance on LTC workers for difficult tasks, complementing their work, reducing stress, and improving coordination of care, which could ultimately reduce the burden associated with their work. To the best of our knowledge, no study has provided empirical evidence of a positive impact of these technologies on LTC workers’ health. Further work should explore this issue.
Notes
The OECD’s definition excludes the hospital sector of LTC jobs. Nevertheless, distinguishing between the hospital and residential/home sectors is only possible after 2012 using the revised NACE classification (see Table 6). To include as little noise as possible in our estimation, we include the hospital sector among LTC jobs before 2013 but differentiate the two sectors after this year. Panel C corrects this approach.
Duration (or job tenure) is defined here as the number of waves/years observed in the job.
Few immigrants (2% of our sub-sample) acquired German citizenship over the period considered. We only consider here responses in the first wave.
For parsimony, we comment on the results only for panel B, but the conclusions hold for panel A.
References
Campbell, J.C., Ikegami, N., Gibson, M.J.: Lessons from public long-term care insurance in Germany and Japan. Health Affairs 29(1), 87–95 (2010)
Harrington, C.A., Geraedts, M., Heller, G.V.: Germany’s long term care insurance model: lessons for the United States. J. Public Health Policy 23(1), 44–65 (2002)
Geyer, J., Korfhage, T.: Labor supply effects of long-term care reform in Germany. Health Econ. 27(9), 1328–1339 (2018)
Bakx, P., De Meijer, C., Schut, F., Van Doorslaer, E.: Going formal or informal, who cares? the influence of public long-term care insurance. Health Econ. 24(6), 631–643 (2015)
Nadash, P., Doty, P., Mahoney, K.J., Von Schwanenflugel, M.: European long-term care programs: lessons for community living assistance services and supports? Health Serv. Res. 47(1pt1), 309–328 (2012)
OECD: Health at a glance 2019. OECD publishing, Paris (2019)
Grabowski, D.: Long-term care—encyclopedia of health economics. Elsevier, Amsterdam (2014)
Kuhlmann, E., Larsen, C.: Long-term care in europe challenges and strategies in nursing staff management. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz 56(8), 1064–1071 (2013)
Kliner, K., Rennert, D., Richter, M.: Gesundheit und Arbeit-Blickpunkt Gesundheitswesen: BKK Gesundheitsatlas 2017. MWV Medizinisch Wissenschaftliche Verlagsgesellschaft (2017)
Franz, S., Zeh, A., Schablon, A., Kuhnert, S., Nienhaus, A.: Aggression and violence against health care workers in Germany-a cross sectional retrospective survey. BMC Health Serv. Res. 10(1), 51 (2010)
Hanson, G.C., Perrin, N.A., Moss, H., Laharnar, N., Glass, N.: Workplace violence against homecare workers and its relationship with workers health outcomes: a cross-sectional study. BMC Public Health 15(1), 11 (2015)
Grossman, M.: On the concept of health capital and the demand for health. J. Polit. Econ. 80(2), 223–255 (1972)
OECD: Who Cares? Attracting and retaining care workers for the elderly. OECD publishing, Paris. (2020). https://doi.org/10.1787/92c0ef68-en
Liang, Y.W., Hsieh, Y., Lin, Y.H., Chen, W.Y.: The impact of job stressors on health-related quality of life of nursing assistants in long-term care settings. Geriatr. Nurs. 35(2), 114–119 (2014)
Joyce, K., Pabayo, R., Critchley, J.A., Bambra, C.: Flexible working conditions and their effects on employee health and wellbeing. Cochrane Database Syst. Rev. (2010). https://doi.org/10.1002/14651858.CD008009.pub2
Robone, S., Jones, A.M., Rice, N.: Contractual conditions, working conditions and their impact on health and well-being. Eur. J. Health Econ. 12(5), 429–444 (2011)
Ravesteijn, B., Hv, Kippersluis, Ev, Doorslaer: The wear and tear on health: what is the role of occupation? Health Econ. 27(2), e69–e86 (2018)
Franks, P., Gold, M.R., Fiscella, K.: Sociodemographics, self-rated health, and mortality in the us. Soc. Sci. Med. 56(12), 2505–2514 (2003)
Idler, E.L., Benyamini, Y.: Self-rated health and mortality: a review of twenty-seven community studies. J. Health Soc. Behav. 38, 21–37 (1997)
McCallum, J., Shadbolt, B., Wang, D.: Self-rated health and survival: a 7-year follow-up study of Australian elderly. Am. J. Public Health 84(7), 1100–1105 (1994)
Van Beveren, J.: Does health care for knowledge management? J. Knowl. Manage. (2003). https://doi.org/10.1108/13673270310463644
Wagstaff, A.: The demand for health: an empirical reformulation of the grossman model. Health Econ. 2(2), 189–198 (1993)
Nickell, S.: Biases in dynamic models with fixed effects. Econometrica J. Econometr. Soc. 49, 1417–1426 (1981)
Bond, S.R.: Dynamic panel data models: a guide to micro data methods and practice. Portuguese Econ. J. 1(2), 141–162 (2002)
Angrist, J.D., Pischke, J.S.: Mostly harmless econometrics: an empiricist’s companion. Princeton University Press, Princeton (2008)
Mundlak, Y.: On the pooling of time series and cross section data. Econometrica J. Econometr. Soc. 46, 69–85 (1978)
Wooldridge, J.M.: Correlated random effects models with unbalanced panels. J Econometrics. 211 (1), 137–150 (2019)
Dauth, C., Lang, J.: Can the unemployed be trained to care for the elderly? the effects of subsidized training in elderly care. Health Econ. 28(4), 543–555 (2019)
Pirani, E., Salvini, S.: Is temporary employment damaging to health? a longitudinal study on Italian workers. Soc. Sci. Med. 124, 121–131 (2015)
Columbo, et al.: Help wanted? Providing and paying for long-term care. OECD Publishing (2011)
Baughman, R.A., Smith, K.E.: Labor mobility of the direct care workforce: implications for the provision of long-term care. Health Econ. 21(12), 1402–1415 (2012)
Rapp, T., Sicsic, J.: The contribution of the immigrant population to the us long-term care workforce. Soc. Sci. Med. 263, 113305 (2020)
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix A
Detail description of similar jobs
Appendix B
Self-perceived health for panels A, B and C
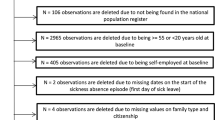
See Fig. 2.
Self-perceived health distributions of panels A, B and C. The two top graphs (panel A) show the self-perceived health distributions for our group of interest (left chart), composed of long-term care and similar workers, and our first comparison group (right chart), composed of all remaining workers. The middle graphs (panel B) reproduce the distributions for long-term care jobs (left chart) and for similar jobs (right chart). The bottom graphs (panel C) describe the distributions for the LTC workers (left chart) and for personal care workers and nurses practising in hospital settings (right chart). Source: GSOEP, v35 (1995–2018). Skewness (S) and Kurtosis (K) descriptives, with Kolmogorov-Smirnov (KS) tests: Panel A: (a): S = − .80; K= 3.42 ; KS test = 0.0940*** (b): S = − .77; K=3.31 ; KS test = 0.0881***; Panel B: (c): S = − .83; K= 3.46 ; KS test = 0.0832*** (d): S = − .75; K = 3.25 ; KS test = 0.0901***; Panel C: (e): S= − .80; K = 3.35 ; KS test = 0.0833*** - (f): S = − .57; K = 2.94 ; KS test = 0.0787***
Appendix C
Sensitivity analyses
Appendix D
Stratified analyses—Panel A
Appendix E
Stratified analyses—Panel B
See Tables 15, 16, 17, and 18.
Rights and permissions
About this article
Cite this article
Rapp, T., Ronchetti, J. & Sicsic, J. Are long-term care jobs harmful? Evidence from Germany. Eur J Health Econ 22, 749–771 (2021). https://doi.org/10.1007/s10198-021-01288-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-021-01288-y